Characterising Residual Limb Morphology and Prosthetic Socket Design Based on Expert Clinician Practice
Abstract
1. Introduction
1.1. Current Clinical Practice in Residual Limb Shape Capture and Prosthetic Socket Design
1.2. Towards More Evidence-Based Prosthetic Socket Design
1.3. Machine Learning
1.4. Understanding Population and Design Variation in Current Prosthetics Workflows
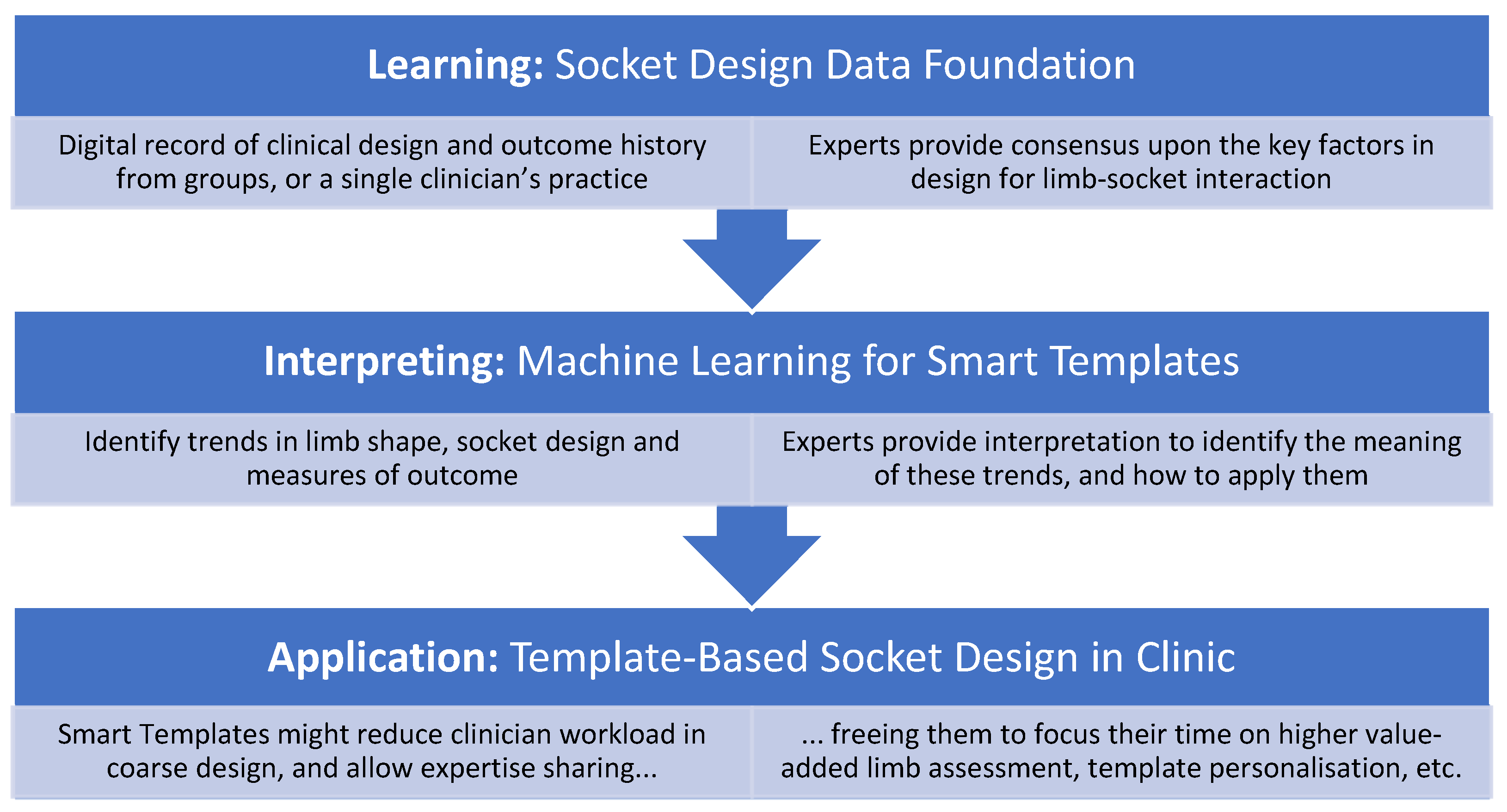
1.5. Motivation
1.6. Objectives
- The first objective was to investigate how population-based models of the residual limb anatomic shape and the prosthetic socket design might be built, the key requirements for each, and whether separate shape and design models might provide higher resolution for machine learning than a combined shape and design model. This compared methods of PCA (Section 2.2) and k-means clustering to identify local rectifications separately (Section 2.3).
- The second objective was to inspect the data to characterise expert socket design following PTB and TSB approaches, and identify any general trends in socket design for particular residual limb shapes by descriptive statistics. Null hypotheses assumed that there was no difference between the limb shapes of individuals given PTB or TSB sockets, and that rectifications were more pronounced in PTB than TSB sockets.
2. Materials and Methods
2.1. Study Design, Approval and Raw Data
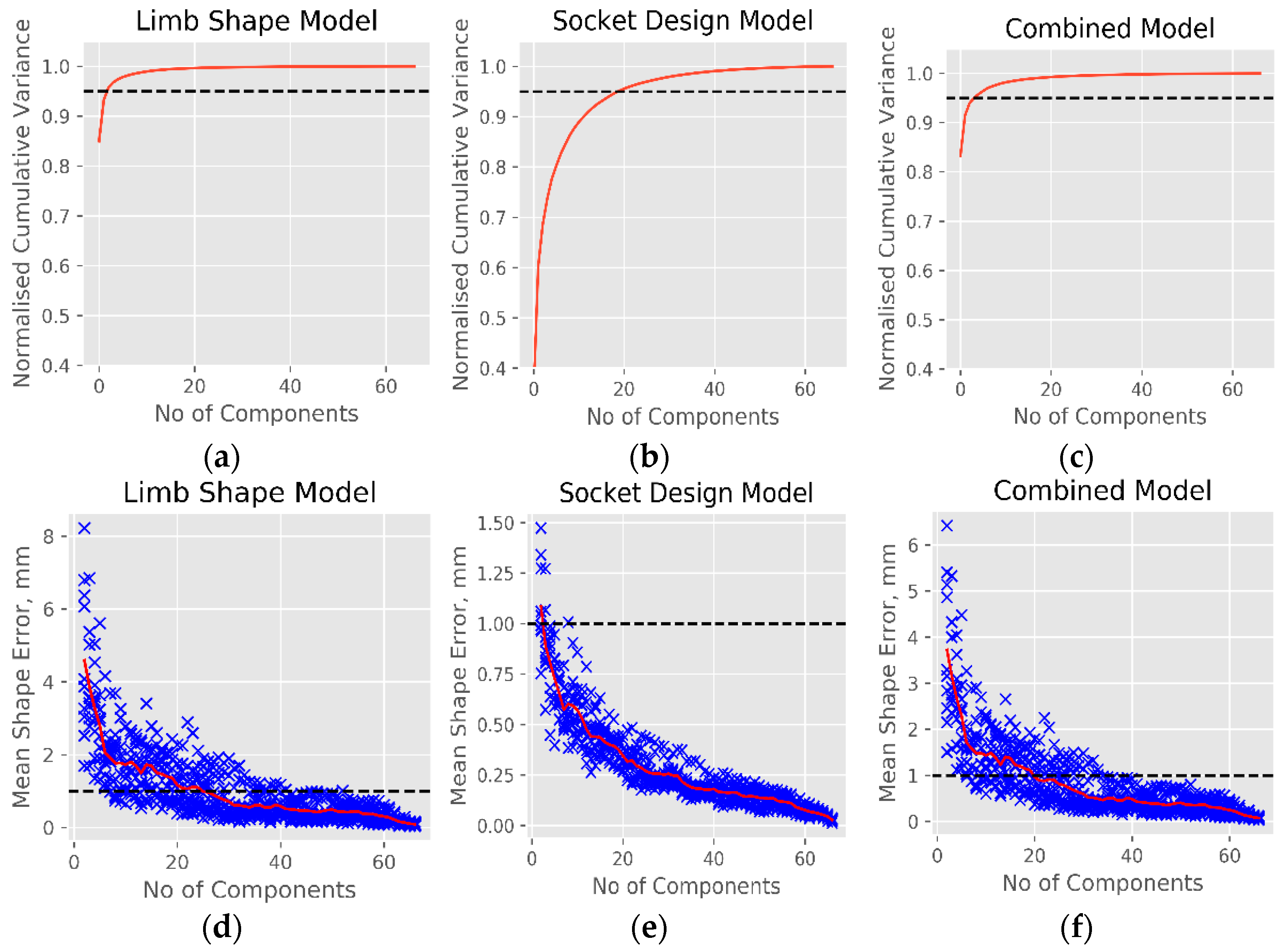
2.2. PCA for Statistical Shape and Design Models
- Right-sided shapes were mirrored.
- The full set of socket shapes were aligned. A vertical superior–inferior translation was applied so that each shape’s patella tendon rectification was located at z = 0, and the shapes’ centroids at the patella tendon level were aligned in the medial–lateral and anterior–posterior axes (x = 0, y = 0). An internal–external rotation was applied so that the posterior trimline lay parallel with the coronal plane. The sockets’ abduction–adduction and flexion–extension were not changed from the CAD file.
- Each limb shape was aligned with its corresponding socket. Shapes were aligned first by their centroids, then by automatic iterative-closest-point surface matching. Where the limb and socket scan shapes deviated considerably, manual alignment adjustments were made and checked by two experienced observers (Diment, Dickinson) to ensure prioritised medial–lateral, anterior–posterior and abduction–adduction alignment at the knee, flexion–extension and internal–external rotation alignment at the anterior tibia. Superior–inferior alignment referenced the anterior tibia and patella.
- An HC Laplacian smoothing algorithm was applied to remove noise while preserving volume, and the socket shapes were cut at an approximated trimline.
- A ~30,000 node mesh was registered onto each of the limb and socket meshes using elastic matching, to allow direct comparison in location of corresponding vertices.
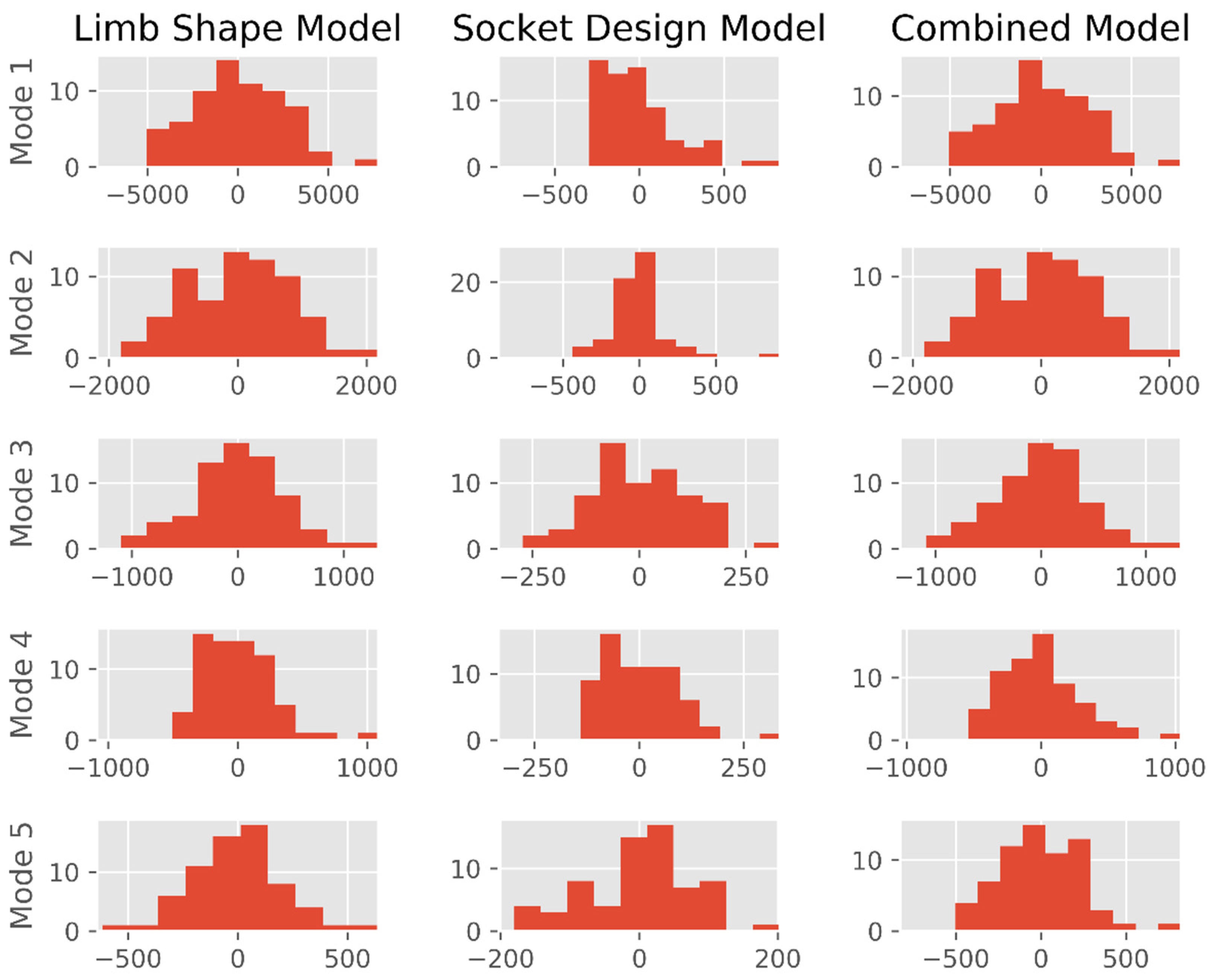
- A statistical limb shape model (SLM) using the limb scans as a training dataset was produced by principal component analysis (PCA) using the scikit-learn toolbox [36]. The mesh files were each represented as a column vector:where represents the number of nodes in the baseline mesh and , and are the vertex coordinates. A vector describing the mean limb shape was calculated by:where represents the number of limbs in the training dataset. PCA by mean-centred Singular Value Decomposition allowed each limb shape to be described by:where are eigenvectors corresponding to the principal components (PC) or ‘modes’ of the population’s shape variation, and is a vector of weighting coefficients associated with the eigenvectors to describe each shape’s deviation from mean.
- A statistical design model (SDM) was produced in the same way, but using a column vector containing the socket–limb rectification values at each vertex:
- Finally, a statistical limb shape and design model (SLDM) was produced in the same way, using a column vector of the limb shape and socket–limb rectification values:
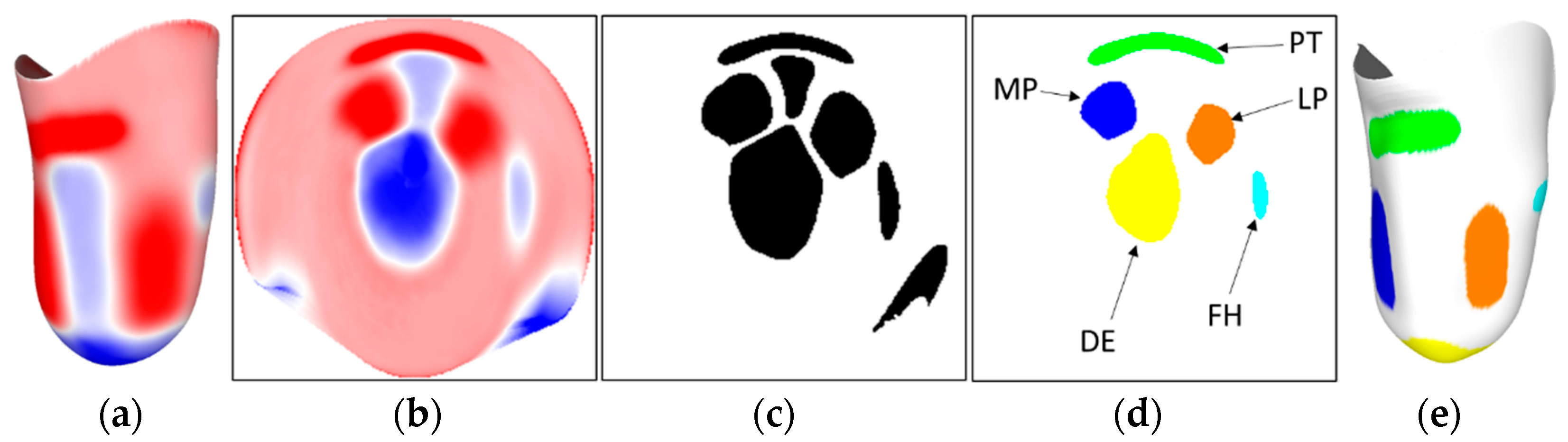
2.3. K-Means Cluster Analysis of Localised Rectifications
- Segmentation: fields of rectification, curvature, and combined rectification and curvature from the 67 training datasets (Figure 3a) were mapped onto 224 × 224-pixel 2D images (Figure 3b). K-means clustering was applied across all the images to generate up to 90 binarised pixel regions per image (Figure 3c).
- Feature Extraction: The shape of each region was quantified using Histogram of Oriented Gradients (HOG) to detect the edges, followed by PCA to reduce the problem dimensionality, with the first 25 components retained (>95% of explained variance). In parallel, the location of each region was quantified by dividing the original region into a 7 × 7 grid, with the number of pixels for each region in each grid square calculated. Finally, the total pixel count was included. This resulted in 75 features for each region which were used for classification.
- Classification: the features were fed into a second k-means clustering algorithm, which groups the regions generated from the image segmentation. To ensure all groups represented the same features, erroneous clustering was identified through comparison to the average of each cluster. Outliers were identified based upon pixel overlap with the average cluster. Any outlier regions were then moved to the cluster where they were closest to the average. The clustered groups were then visually inspected and related to rectifications of interest, for example, a group which contains the patella tendon bars across all input sockets (Figure 3d). The classified cluster images were then mapped back onto the corresponding 3D shape (Figure 3e).
2.4. Data Analysis
3. Results
3.1. Objective 1: Population Models of Residual Limb Anatomic Shape and Prosthetic Socket Design
3.2. Objective 2: Characterising Residual Limb Anatomic Shape and Prosthetic Socket Design Practice
4. Discussion
4.1. Observations
4.2. Limitations
4.3. Implications and Use
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Correlations Between SLM Modes and Participant Metadata | ||||||
|---|---|---|---|---|---|---|
| Mode | 1 | 2 | 3 | 4 | 5 | |
| Gross Size: Large to Small | Soft Tissue: Bulky to Slender | Knee Angle: Adducted to Abducted | Sag. Profile: Conical to Bulbous | Cor. Profile: Conical to Bulbous | ||
| Time Since Amputation | r | 0.10 | 0.23 | 0.02 | 0.05 | 0.28 |
| p | 0.433 | 0.065 | 0.865 | 0.702 | 0.026 * | |
References
- Safari, R. Lower limb prosthetic interfaces: Clinical and technological advancement and potential future direction. Prosthet. Orthot. Int. 2020, 44, 384–401. [Google Scholar] [CrossRef] [PubMed]
- Pezzin, L.E.; Dillingham, T.R.; MacKenzie, E.J.; Ephraim, P.; Rossbach, P. Use and satisfaction with prosthetic limb devices and related services. Arch. Phys. Med. Rehabil. 2004, 85, 723–729. [Google Scholar] [CrossRef] [PubMed]
- Haggstrom, E.E.; Hansson, E.; Hagberg, K. Comparison of prosthetic costs and service between osseointegrated and conventional suspended transfemoral prostheses. Prosthet. Orthot. Int. 2013, 37, 152–160. [Google Scholar] [CrossRef] [PubMed]
- Suyi Yang, E.; Aslani, N.; McGarry, A. Influences and trends of various shape-capture methods on outcomes in trans-tibial prosthetics: A systematic review. Prosthet. Orthot. Int. 2019, 43, 540–555. [Google Scholar] [CrossRef]
- Foort, J. The Patellar-Tendon-Bearing Prosthesis for below-knee amputees, a review of technique and criteria. Artif Limbs 1965, 13, 4–13. [Google Scholar]
- Staats, T.B.; Lundt, J. The UCLA Total Surface Bearing Suction Below-Knee Prosthesis. Clin. Prosthet. Orthot. 1987, 11, 118–130. [Google Scholar]
- Fillauer, C.E.; Pritham, C.H.; Fillauer, K.D. Evolution and development of the silicone suction socket (3S) for below-knee prostheses. J. Prosthet. Orthot. 1989, 1, 92–103. [Google Scholar] [CrossRef]
- Kristinsson, O. The ICEROSS concept: A discussion of a philosophy. Prosthet. Orthot. Int. 1993, 17, 49–55. [Google Scholar] [CrossRef]
- Murdoch, G. The “Dundee” Socket—A Total Contact Socket for the Below-Knee Amputation. Orthop. Prosthet. Appl. J. 1965, 19, 231–234. [Google Scholar]
- Wu, Y.; Casanova, H.; Smith, W.K.; Edwards, M.; Childress, D.S. CIR sand casting system for trans-tibial socket. Prosthet. Orthot. Int. 2003, 27, 146–152. [Google Scholar] [CrossRef]
- Wu, Y.; Casanova, H.R.; Reisinger, K.I.M.D.; Smith, W.K.; Childress, D.S. CIR casting system for making transtibial sockets. Prosthet. Orthot. Int. 2009, 33, 1–9. [Google Scholar] [CrossRef]
- ISPO. International Society for Prosthetics and Orthotics ISPO Biennium Report 2017–2019; ISPO: Brussels, Belgium, 2019. [Google Scholar]
- Al-Fakih, E.A.; Abu Osman, N.A.; Mahmad Adikan, F.R. Techniques for interface stress measurements within prosthetic sockets of transtibial amputees: A review of the past 50 years of research. Sensors 2016, 16, 1119. [Google Scholar] [CrossRef] [PubMed]
- Sewell, P.; Noroozi, S.; Vinney, J.; Amali, R.; Andrews, S. Static and dynamic pressure prediction for prosthetic socket fitting assessment utilising an inverse problem approach. Artif. Intell. Med. 2012, 54, 29–41. [Google Scholar] [CrossRef]
- Krouskop, T.A.; Muilenberg, A.L.; Doughtery, D.R.; Winningham, D.J. Computer-aided design of a prosthetic socket for an above-knee amputee. J. Rehabil. Res. Dev. 1987, 24, 31–38. [Google Scholar] [PubMed]
- Dickinson, A.S.; Steer, J.W.; Worsley, P.R. Finite element analysis of the amputated lower limb: A systematic review and recommendations. Med. Eng. Phys. 2017, 43, 1–18. [Google Scholar] [CrossRef]
- Sewell, P.; Noroozi, S.; Vinney, J.; Andrews, S. Developments in the trans-tibial prosthetic socket fitting process: A review of past and present research. Prosthet. Orthot. Int. 2000, 24, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Mak, A.F.T.; Zhang, M.; Boone, D.A. State-of-the-art research in lower-limb prosthetic biomechanics-socket interface: A review. J. Rehabil. Res. Dev. 2001, 38, 161–173. [Google Scholar] [PubMed]
- Colombo, G.; Facoetti, G.; Rizzi, C. Automatic Below-Knee Prosthesis Socket Design: A Preliminary Approach. In Proceedings of the 7th International Conference, DHM 2016, Held as Part of HCI International 2016, Toronto, ON, Canada, 17–22 July 2016. [Google Scholar]
- Saverio Frillici, F.; Rotini, F. Prosthesis socket design through shape optimization. Comput. Aided. Des. Appl. 2013, 10, 863–876. [Google Scholar] [CrossRef]
- Steer, J.W.; Grudniewski, P.A.; Browne, M.; Worsley, P.R.; Sobey, A.J.; Dickinson, A.S. Predictive prosthetic socket design: Part 2—generating person-specific candidate designs using multi-objective genetic algorithms. Biomech. Model. Mechanobiol. 2020, 19, 1347–1360. [Google Scholar] [CrossRef]
- Ballit, A.; Mougharbel, I.; Ghaziri, H.; Dao, T.T. Computer-aided parametric prosthetic socket design based on real-time soft tissue deformation and an inverse approach. Vis. Comput. 2021, 37, 1–19. [Google Scholar] [CrossRef]
- Li, S.; Lan, H.; Luo, X.; Lv, Y.; Gao, L.; Yu, H. Quantitative compensation design for prosthetic socket based on eigenvector algorithm method. Rev. Sci. Instrum. 2019, 90, 104101. [Google Scholar] [CrossRef]
- Karamousadakis, M.; Porichis, A.; Ottikkutti, S.; Chen, D.; Vartholomeos, P. A Sensor-Based Decision Support System for Transfemoral Socket Rectification. Sensors 2021, 21, 3743. [Google Scholar] [CrossRef] [PubMed]
- Sanz-Pena, I.; Arachchi, S.; Halwala-Vithanage, D.; Mallikarachchi, S.; Kirumbara-Liyanage, J.; McGregor, A.; Silva, P.; Newell, N. Characterising the mould rectification process for designing scoliosis braces: Towards automated digital design of 3d-printed braces. Appl. Sci. 2021, 11, 4665. [Google Scholar] [CrossRef]
- Lemaire, E.D.; Johnson, F. A Quantitative Method for Comparing and Evaluating Manual Prosthetic Socket Modifications. IEEE Trans. Rehabil. Eng. 1996, 4, 303–309. [Google Scholar] [CrossRef]
- Torres-Moreno, R.; Foort, J.; Morrison, J.B.; Saunders, C.G. A reference shape library for computer aided socket design in above-knee prostheses. Prosthet. Orthot. Int. 1989, 13, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Lemaire, E.D.; Bexiga, P.; Johnson, F.; Solomonidis, S.E.; Paul, J.P. Validation of a quantitative method for defining CAD/CAM socket modifications. Prosthet. Orthot. Int. 1999, 23, 30–44. [Google Scholar] [CrossRef]
- Fatone, S.; Johnson, W.B.; Tran, L.; Tucker, K.; Mowrer, C.; Caldwell, R. Quantification of rectifications for the Northwestern University Flexible Sub-Ischial Vacuum Socket. Prosthet. Orthot. Int. 2017, 41, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Saxby, D.J.; Killen, B.A.; Pizzolato, C.; Carty, C.P.; Diamond, L.E.; Modenese, L.; Fernandez, J.; Davico, G.; Barzan, M.; Lenton, G.; et al. Machine learning methods to support personalized neuromusculoskeletal modelling. Biomech. Model. Mechanobiol. 2020, 19, 1169–1185. [Google Scholar] [CrossRef]
- Cook, D.D.; Robertson, D.J. The generic modeling fallacy: Average biomechanical models often produce non-average results! J. Biomech. 2016, 49, 3609–3615. [Google Scholar] [CrossRef]
- Worsley, P.R.; Steer, J.W.; Woods, C.J.; Dickinson, A.S. Classifying residual limb shape in transtibial amputees. Prosthet. Orthot. Int. 2015, 39, 414. [Google Scholar] [CrossRef][Green Version]
- Steer, J.W.; Worsley, P.R.; Browne, M.; Dickinson, A.S. Predictive prosthetic socket design: Part 1—population-based evaluation of transtibial prosthetic sockets by FEA-driven surrogate modelling. Biomech. Model. Mechanobiol. 2020, 19, 1331–1346. [Google Scholar] [CrossRef] [PubMed]
- Steer, J.; Stocks, O.; Parsons, J.; Worsley, P.; Dickinson, A. Ampscan: A lightweight Python package for shape analysis of prosthetics and orthotics. J. Open Source Softw. 2020, 5, 2060. [Google Scholar] [CrossRef]
- Dickinson, A.S.; Steer, J.W.; Woods, C.J.; Worsley, P.R. Registering a methodology for imaging and analysis of residual-limb shape after transtibial amputation. J. Rehabil. Res. Dev. 2016, 53, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-Learn: Machine Learning in Python. J. Mach. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Convery, P.P.; Buis, A.W.P.; Wilkie, R.; Sockalingam, S.; Blair, A.; McHugh, B. Measurement of the consistency of patellar-tendon-bearing cast rectification. Prosthet. Orthot. Int. 2003, 27, 207–213. [Google Scholar] [CrossRef]
- Dickinson, A.; Donovan-Hall, M.; Kheng, S.; Bou, K.; Tech, A.; Steer, J.; Metcalf, C.; Worsley, P. Selecting Appropriate 3D Scanning Technologies for Prosthetic Socket Design and Transtibial Residual Limb Shape Characterisation. J. Prosthet. Orthot. 2020. [Google Scholar] [CrossRef]
- Safari, M.R.; Meier, M.R. Systematic review of effects of current transtibial prosthetic socket designs—Part 1: Qualitative outcomes. J. Rehabil. Res. Dev. 2015, 52, 491–508. [Google Scholar] [CrossRef]
- Stevens, P.M.; Depalma, R.R.; Wurdeman, S.R. Transtibial socket design, interface, and suspension: A clinical practice guideline. J. Prosthet. Orthot. 2019, 31, 172–178. [Google Scholar] [CrossRef]
- Yiǧiter, K.; Şener, G.; Bayar, K. Comparison of the effects of patellar tendon bearing and total surface bearing sockets on prosthetic fitting and rehabilitation. Prosthet. Orthot. Int. 2002, 26, 206–212. [Google Scholar] [CrossRef]
- Laing, S.; Lee, P.V.; Goh, J.C. Engineering a trans-tibial prosthetic socket for the lower limb amputee. Ann. Acad. Med. Singap. 2011, 40, 252–259. [Google Scholar]
- Hachisuka, K.; Dozono, K.; Ogata, H.; Ohmine, S.; Shitama, H.; Shinkoda, K. Total surface bearing below-knee prosthesis: Advantages, disadvantages, and clinical implications. Arch. Phys. Med. Rehabil. 1998, 79, 783–789. [Google Scholar] [CrossRef]
- Chan, R.B.; Rovick, J.S.; Childress, D.S. Surface curvature analysis for enhanced computer-aided-design of prosthetic sockets. In Proceedings of the 15th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 31 October 1993; pp. 1292–1293. [Google Scholar] [CrossRef]
- Chahande, A.I.; Billakanti, S.R. Identification of load bearing areas for prosthetic limbs in a below-the-knee amputee using neural networks. In Proceedings of the 15th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Diego, CA, USA, 31 October 1993; pp. 1284–1285. [Google Scholar] [CrossRef]
- Sanders, R. The Pareto principle: Its use and abuse. J. Serv. Mark. 1987, 1, 37–40. [Google Scholar] [CrossRef]
- Silver-Thorn, M.B.; Childress, D.S. Parametric analysis using the finite element method to investigate prosthetic interface stresses for persons with trans-tibial amputation. J. Rehabil. Res. Dev. 1996, 33, 227–238. [Google Scholar] [PubMed]
- Silver-Thorn, M.B.; Childress, D.S. Generic, geometric finite element analysis of the transtibial residual limb and prosthetic socket. J. Rehabil. Res. Dev. 1997, 34, 171–186. [Google Scholar]


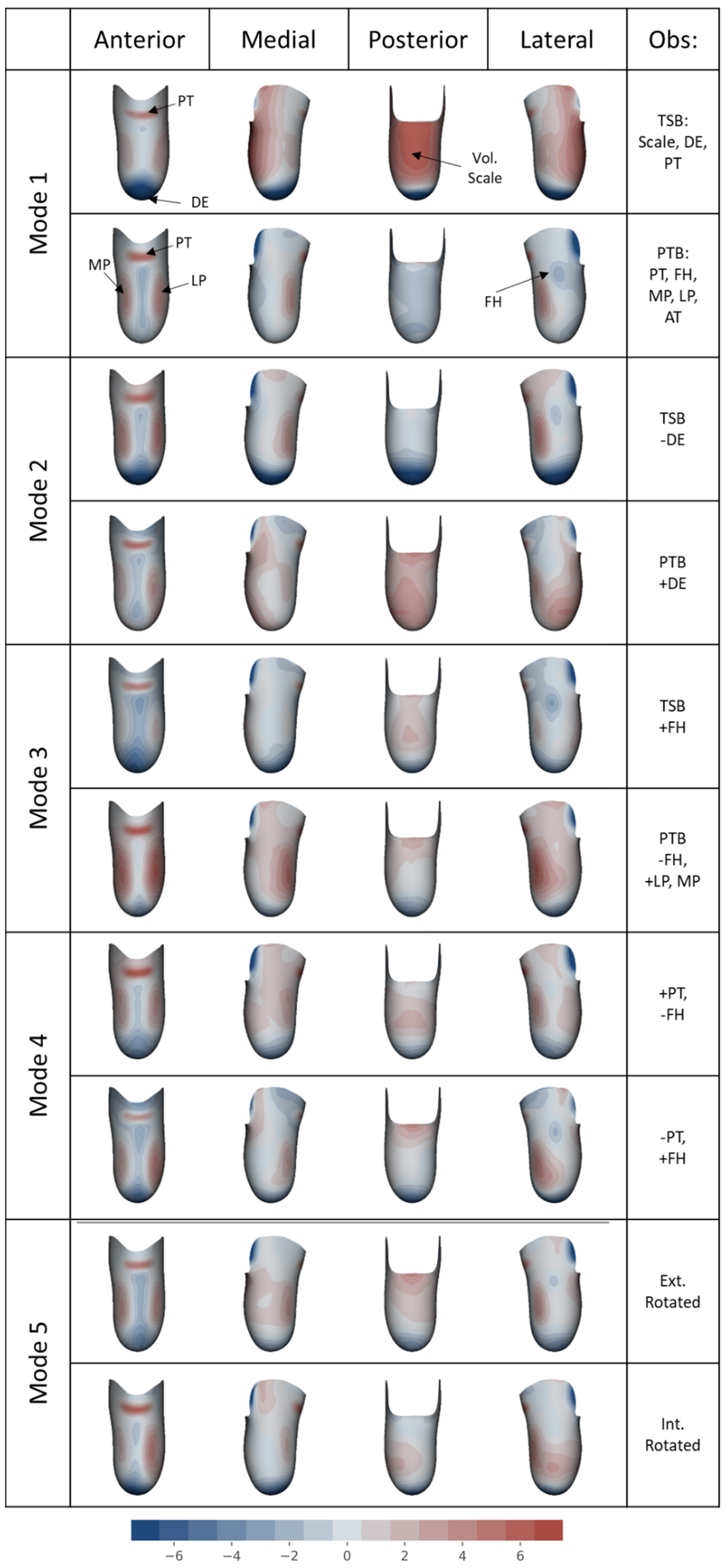

| Mode No. | Mode Variance and Description for Each Statistical Model | ||
|---|---|---|---|
| Limb Shape (SLM) | Socket Design (SDM) | Limb Shape and Socket Design (SSDM) | |
| 1 | (85%) Size and length: long/large to small/short | (35%) PTB to TSB with distal tip space | (83%) Large and PTB to small and TSB |
| 2 | (8.3%) Bulky to slender soft tissue | (25%) PTB with distal tip space to TSB | (8.2%) Bulky and PTB to slender and TSB |
| 3 | (2.5%) Angle of knee, abducted to adducted | (8.5%) PTB to TSB with fibula head rectns. | (2.5%) Abducted to adducted knee |
| 4 | (1.1%) Sagittal profile, conical to bulbous | (5.1%) PTB to TSB with patella tendon and anterior tibia rectns. | (1.1%) Profile: conical PTB to bulbous TSB |
| 5 | (0.6%) Coronal profile, conical to bulbous | (3.9%) Internal–external rotation of tibia | (0.7%) Profile: bulbous PTB to conical TSB |
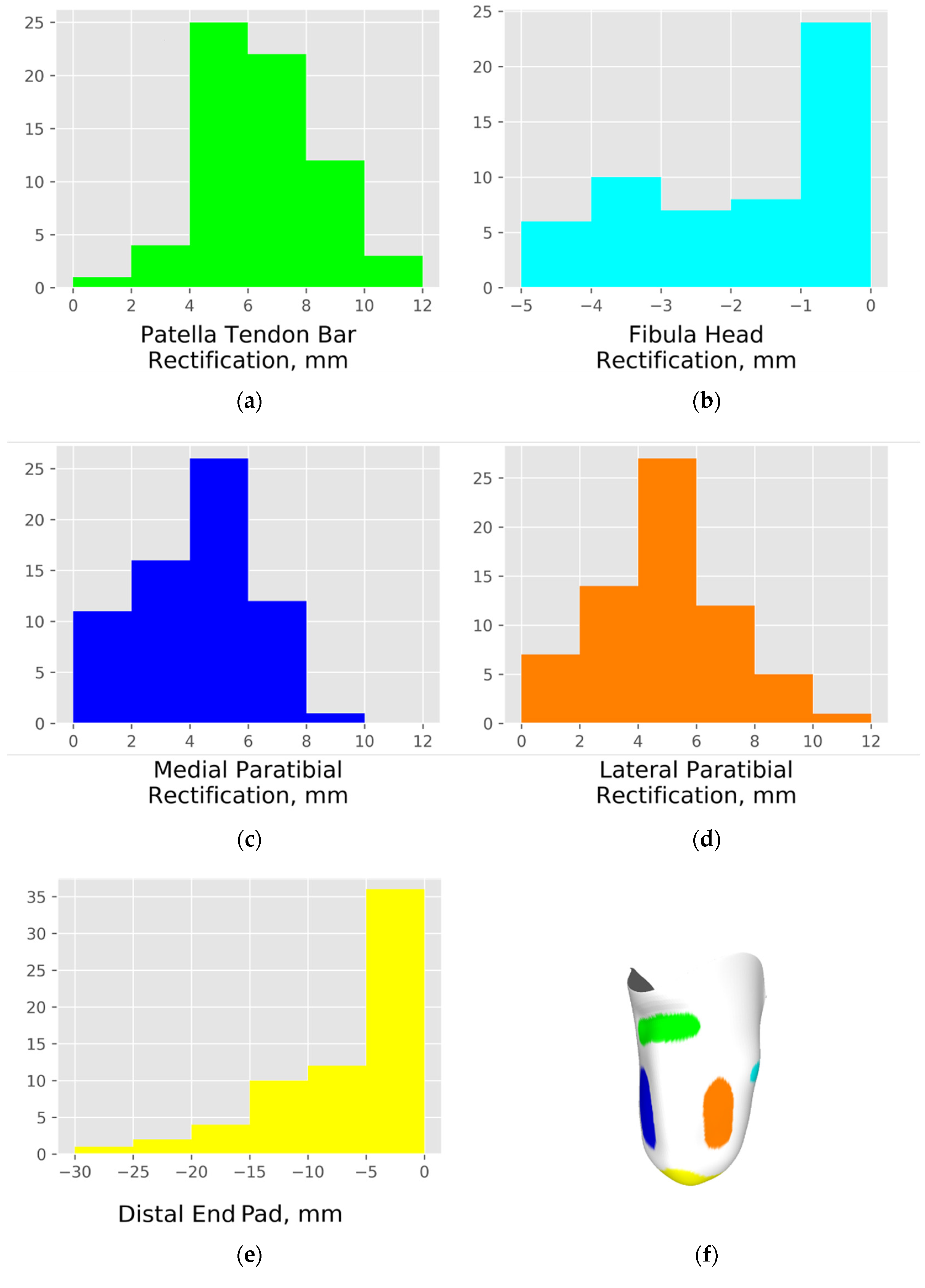
| Rectification | PT | FH | MP | LP | DE |
|---|---|---|---|---|---|
| Prevalence, % | 100 | 82 | 94 | 97 | 91 |
| Classification, % | 100 | 93 | 99 | 96 | 100 |
| Measure | Whole Group (n = 67) | PTB Group (n = 55) | TSB Group (n = 12) |
|---|---|---|---|
| Residual Limb Anatomy: normally distributed: mean (s.d.) | |||
| Limb length, mm | 156 (29) | 157 (29) | 153 (31) |
| Perimeter at patella tendon, mm | 383 (40) | 383 (42) | 385 (34) |
| Perimeter at ½ limb length, mm | 366 (51) | 358 (55) | 355 (30) |
| Perimeter at ¾ limb length, mm | 327 (48) | 329 (52) | 315 (24) |
| Profile ratio at ½ limb length 1 | 0.95 (0.06) | 0.96 (0.06) | 0.92 (0.05) |
| Profile ratio at ¾ limb length 1 | 0.85 (0.07) | 0.86 (0.07) | 0.82 (0.04) |
| Abduction/adduction angle, ° | 0.7 (1.9) | 0.7 (2.0) | 0.5 (1.6) |
| Gross Socket Sizing: normally distributed: mean (s.d.) | |||
| Overall volume reduction, % | −1.9 (4.3) | −1.6 (4.4) | −3.1 (3.7) |
| Area reduction at patella tendon, % | −4.1 (5.7) | −3.8 (5.6) | −5.6 (5.8) |
| Area reduction at ½ limb length, % | −6.0 (4.5) | −5.7 (4.2) | −7.7 (5.4) |
| Area reduction at ¾ limb length, % | −1.9 (5.8) | −1.6 (5.8) | −3.7 (5.5) |
| Local Socket Rectifications: non-normally distributed: median (10th–90th percentile range) | |||
| Patella tendon rect. depth, mm | 6.7 (4.2–9.0) | 6.7 (4.2–9.1) | 6.6 (3.8 –8.6) |
| Fibula head rect. height, mm | −1.0 (−4.2–0.4) | −1.6 (−4.4–0.4) * | 0.0 (−3.0–0.4) * |
| Medial paratibial rect. depth, mm | 4.3 (0.9–6.9) | 4.5 (1.2–6.9) | 3.8 (0.0–7.2) |
| Lateral paratibial rect. depth, mm | 4.9 (1.5–7.8) | 4.9 (2.8–7.9) | 3.5 (−0.2–8.7) |
| Distal end rect. height, mm | −4.2 (−15.4–0.0) | −4.1 (−14.4–0.0) | −5.2 (−21.0–0.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dickinson, A.; Diment, L.; Morris, R.; Pearson, E.; Hannett, D.; Steer, J. Characterising Residual Limb Morphology and Prosthetic Socket Design Based on Expert Clinician Practice. Prosthesis 2021, 3, 280-299. https://doi.org/10.3390/prosthesis3040027
Dickinson A, Diment L, Morris R, Pearson E, Hannett D, Steer J. Characterising Residual Limb Morphology and Prosthetic Socket Design Based on Expert Clinician Practice. Prosthesis. 2021; 3(4):280-299. https://doi.org/10.3390/prosthesis3040027
Chicago/Turabian StyleDickinson, Alexander, Laura Diment, Robin Morris, Emily Pearson, Dominic Hannett, and Joshua Steer. 2021. "Characterising Residual Limb Morphology and Prosthetic Socket Design Based on Expert Clinician Practice" Prosthesis 3, no. 4: 280-299. https://doi.org/10.3390/prosthesis3040027
APA StyleDickinson, A., Diment, L., Morris, R., Pearson, E., Hannett, D., & Steer, J. (2021). Characterising Residual Limb Morphology and Prosthetic Socket Design Based on Expert Clinician Practice. Prosthesis, 3(4), 280-299. https://doi.org/10.3390/prosthesis3040027






