Osseodensification Drilling vs. Standard Protocol of Implant Site Preparation: An In Vitro Study on Polyurethane Foam Sheets
Abstract
:1. Introduction
2. Results
3. Discussion
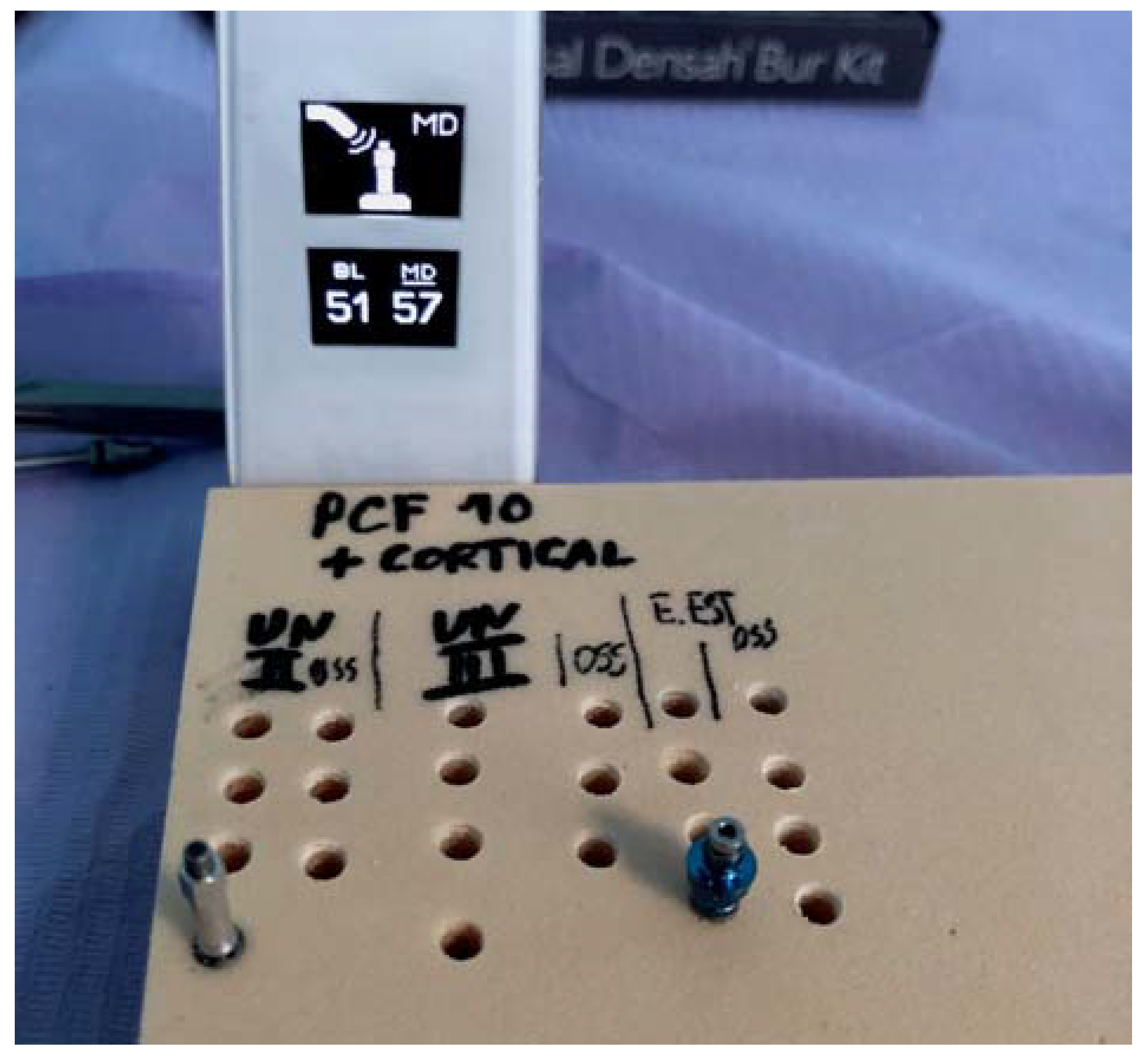
4. Materials and Methods
4.1. Implants
4.2. Polyurethane Sheets Foam
4.3. Experimental Design and Sample Size
4.4. Osseodensification Drilling Protocol
4.5. Stability Measurement
4.6. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Degidi, M.; Daprile, G.; Piattelli, A. Primary stability determination by means of insertion torque and RFA in a sample of 4135 implants. Clin. Implant Dent. Relat. Res. 2012, 14, 501–507. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Romanos, G.E. The role of primary stability for successful immediate loading of dental implants. A literature review. J. Dent. 2010, 38, 612–620. [Google Scholar] [CrossRef] [PubMed]
- Gehrke, S.A.; Tumedei, M.; Aramburú Júnior, J.; Treichel, T.L.E.; Kolerman, R.; Lepore, S.; Piattelli, A.; Iezzi, G. Histological and Histomorphometrical Evaluation of a New Implant Macrogeometry. A Sheep Study. Int. J. Environm. Res. Public Health 2020, 17, 3477. [Google Scholar] [CrossRef]
- Tumedei, M.; Piattelli, A.; Degidi, M.; Mangano, C.; Iezzi, G. A Narrative Review of the Histological and Histomorphometrical Evaluation of the Peri-Implant Bone in Loaded and Unloaded Dental Implants. A 30-Year Experience (1988–2018). Int. J. Environ. Res. Public Health 2020, 17, 2088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scarano, A.; Crocetta, E.; Quaranta, A.; Lorusso, F. Influence of the Thermal Treatment to Address a Better Osseointegration of Ti6Al4V Dental Implants: Histological and Histomorphometrical Study in a Rabbit Model. Biomed. Res. Int. 2018, 2018, 2349698. [Google Scholar] [CrossRef] [Green Version]
- Huwais, S.; Meyer, E.G. A Novel Osseous Densification Approach in Implant Osteotomy Preparation to Increase Biomechanical Primary Stability, Bone Mineral Density, and Bone-to-Implant Contact. Int. J. Oral Maxillofac. Implants 2017, 32, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Möhlhenrich, S.C.; Heussen, N.; Elvers, D.; Steiner, T.; Hölzle, F.; Modabber, A. Compensating for poor primary implant stability in different bone densities by varying implant geometry: A laboratory study. Int. J. Oral Maxillofac. Surg. 2015, 44, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Javed, F.; Almas, K.; Crespi, R.; Romanos, G.E. Implant surface morphology and primary stability: Is there a connection? Implant Dent. 2011, 20, 40–46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Misch, C.E.; Judy, K.W. Classification of partially edentulous arches for implant dentistry. Int. J. Oral Implantol. 1987, 4, 7–13. [Google Scholar] [PubMed]
- Degidi, M.; Daprile, G.; Piattelli, A. Influence of underpreparation on primary stability of implants inserted in poor quality bone sites: An in vitro study. J. Oral Maxillofac. Surg. 2015, 73, 1084–1088. [Google Scholar] [CrossRef]
- Degidi, M.; Perrotti, V.; Shibli, J.A.; Mortellaro, C.; Piattelli, A.; Iezzi, G. Evaluation of the peri-implant bone around parallel-walled dental implants with a condensing thread macrodesign and a self-tapping apex: A 10-year retrospective histological analysis. J. Craniofac. Surg. 2014, 25, 840–842. [Google Scholar] [CrossRef] [PubMed]
- Alam, K.; Muhammad, R.; Shamsuzzoha, A.; AlYahmadi, A.; Ahmed, N. Quantitative analysis of force and torque in bone drilling. J. Eng. Res. [TJER] 2017, 14, 39–48. [Google Scholar] [CrossRef] [Green Version]
- Zizzari, V.L.; Berardi, D.; Congedi, F.; Tumedei, M.; Cataldi, A.; Perfetti, G. Morphological Aspect and iNOS and Bax Expression Modification in Bone Tissue Around Dental Implants Positioned Using Piezoelectric Bone Surgery Versus Conventional Drill Technique. J. Craniofac. Surg. 2015, 26, 741–744. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Lorusso, F.; Noumbissi, S. Infrared Thermographic Evaluation of Temperature Modifications Induced during Implant Site Preparation with Steel vs. Zirconia Implant Drill. J. Clin. Med. 2020, 9, 148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scarano, A.; Petrini, M.; Mastrangelo, F.; Noumbissi, S.; Lorusso, F. The Effects of Liquid Disinfection and Heat Sterilization Processes on Implant Drill Roughness: Energy Dispersion X-ray Microanalysis and Infrared Thermography. J. Clin. Med. 2020, 9, 1019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Degidi, M.; Daprile, G.; Piattelli, A.; Iezzi, G. Development of a new implant primary stability parameter: Insertion torque revisited. Clin. Implant Dent. Relat. Res. 2013, 15, 637–644. [Google Scholar] [CrossRef]
- Padhye, N.M.; Padhye, A.M.; Bhatavadekar, N.B. Osseodensification—A systematic review and qualitative analysis of published literature. J. Oral Biol. Craniofac. Res. 2020, 10, 375–380. [Google Scholar] [CrossRef]
- Lahens, B.; Neiva, R.; Tovar, N.; Alifarag, A.M.; Jimbo, R.; Bonfante, E.A.; Bowers, M.M.; Cuppini, M.; Freitas, H.; Witek, L.; et al. Biomechanical and histologic basis of osseodensification drilling for endosteal implant placement in low density bone. An experimental study in sheep. J. Mech. Behav. Biomed. Mater. 2016, 63, 56–65. [Google Scholar] [CrossRef]
- Comuzzi, L.; Iezzi, G.; Piattelli, A.; Tumedei, M. An In Vitro Evaluation, on Polyurethane Foam Sheets, of the Insertion Torque (IT) Values, Pull-Out Torque Values, and Resonance Frequency Analysis (RFA) of NanoShort Dental Implants. Polymers 2019, 11, 1020. [Google Scholar] [CrossRef] [Green Version]
- Comuzzi, L.; Tumedei, M.; Piattelli, A.; Iezzi, G. Short vs. Standard Length Cone Morse Connection Implants: An In Vitro Pilot Study in Low Density Polyurethane Foam. Symmetry 2019, 11, 1349. [Google Scholar] [CrossRef] [Green Version]
- Di Stefano, D.A.; Arosio, P.; Gastaldi, G.; Gherlone, E. The insertion torque-depth curve integral as a measure of implant primary stability: An in vitro study on polyurethane foam blocks. J. Prosthet Dent. 2018, 120, 706–714. [Google Scholar] [CrossRef]
- Tumedei, M.; Savadori, P.; Del Fabbro, M. Synthetic Blocks for Bone Regeneration: A Systematic Review and Meta-Analysis. Int. J. Mol. Sci. 2019, 20, 4221. [Google Scholar] [CrossRef] [Green Version]
- Gehrke, S.A.; Mazón, P.; Del Fabbro, M.; Tumedei, M.; Aramburú Júnior, J.; Pérez-Díaz, L.; De Aza, P.N. Histological and Histomorphometric Analyses of Two Bovine Bone Blocks Implanted in Rabbit Calvaria. Symmetry 2019, 11, 641. [Google Scholar]
- Araújo, M.G.; Silva, C.O.; Misawa, M.; Sukekava, F. Alveolar socket healing: What can we learn? Periodontol. 2000 2015, 68, 122–134. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Piattelli, A.; Assenza, B.; Carinci, F.; Di Donato, L.; Romani, G.L.; Merla, A. Infrared thermographic evaluation of temperature modifications induced during implant site preparation with cylindrical versus conical drills. Clin. Implant Dent. Relat. Res. 2011, 13, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Carinci, F.; Lorusso, F.; Festa, F.; Bevilacqua, L.; Santos de Oliveira, P.; Maglione, M. Ultrasonic vs Drill Implant Site Preparation: Post-Operative Pain Measurement Through VAS, Swelling and Crestal Bone Remodeling: A Randomized Clinical Study. Materials (Basel) 2018, 11, 2516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Falco, A.; Berardini, M.; Trisi, P. Correlation between Implant Geometry, Implant Surface, Insertion Torque, and Primary Stability: In Vitro Biomechanical Analysis. Int. J. Oral Maxillofac. Implants 2018, 33, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Di Stefano, D.A.; Arosio, P.; Perrotti, V.; Iezzi, G.; Scarano, A.; Piattelli, A. Correlation between Implant Geometry, Bone Density, and the Insertion Torque/Depth Integral: A Study on Bovine Ribs. Dent. J. (Basel) 2019, 7, 25. [Google Scholar] [CrossRef] [Green Version]
- Almutairi, A.S.; Walid, M.A.; Alkhodary, M.A. The effect of osseodensification and different thread designs on the dental implant primary stability. F1000Res 2018, 7, 1898. [Google Scholar] [CrossRef] [Green Version]
- Maglione, M.; Bevilacqua, L.; Dotto, F.; Costantinides, F.; Lorusso, F.; Scarano, A. Observational Study on the Preparation of the Implant Site with Piezosurgery vs. Drill: Comparison between the Two Methods in terms of Postoperative Pain, Surgical Times, and Operational Advantages. BioMed Res. Inter. 2019, 8483658, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Di Fiore, A.; Sivolella, S.; Stocco, E.; Favero, V.; Stellini, E. Experimental Analysis of Temperature Differences during Implant Site Preparation: Continuous Drilling Technique Versus Intermittent Drilling Technique. J. Oral Implantol. 2018, 44, 46–50. [Google Scholar] [CrossRef] [PubMed]
- Bacci, C.; Lucchiari, N.; Frigo, A.C.; Stecco, C.; Zanette, G.; Dotto, V.; Sivolella, S. Temperatures generated during implant site preparation with conventional drilling versus single-drill method: An ex-vivo human mandible study. Minerva Stomatol. 2019, 68, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Scarano, A.; Piattelli, A.; Murmura, G.; Iezzi, G.; Assenza, B.; Mancino, C. Delayed expansion of the atrophic mandible by ultrasonic surgery: A clinical and histologic case series. Int. J. Oral Maxillofac. Implants 2015, 30, 144–149. [Google Scholar] [CrossRef] [Green Version]
- Díaz-Castro, M.-C.; Falcao, A.; López-Jarana, P.; Falcao, C.; Ríos-Santos, J.-V.; Fernández-Palacín, A.; Herrero-Climent, M. Repeatability of the resonance frequency analysis values in implants with a new technology. Med. Oral Patol. Oral Cir. Bucal 2019, 24, e636–e642. [Google Scholar] [CrossRef]
- López-Jarana, P.; Díaz-Castro, C.M.; Falcão, A.; Falcão, C.; Ríos-Santos, J.V.; Herrero-Climent, M. Thickness of the buccal bone wall and root angulation in the maxilla and mandible: An approach to cone beam computed tomography. BMC Oral Health 2018, 18, 194. [Google Scholar] [CrossRef]
- Andrés-García, R.; Vives, N.G.; Climent, F.H.; Palacín, A.F.; Santos, V.R.; Climent, M.H.; Bullón, P. In vitro evaluation of the influence of the cortical bone on the primary stability of two implant systems. Med. Oral Patol. Oral Cir. Bucal 2009, 14, E93–E97. [Google Scholar]
- Herrero-Climent, M.; Albertini, M.; Rios-Santos, J.-V.; Lázaro-Calvo, P.; Fernández-Palacín, A.; Bullon, P. Resonance frequency analysis-reliability in third generation instruments: Osstell mentor®. Med. Oral Patol. Oral Cir. Bucal 2012, 17, e801–e806. [Google Scholar] [CrossRef] [Green Version]
- Ríos-Santos, J.V.; Menjívar-Galán, A.M.; Herrero-Climent, M.; Ríos-Carrasco, B.; Fernández-Palacín, A.; Perez, R.A.; Gil, F.J. Unravelling the effect of macro and microscopic design of dental implants on osseointegration: A randomised clinical study in minipigs. J. Mater. Sci. Mater. Med. 2018, 29, 99. [Google Scholar] [CrossRef]
- Lahens, B.; Lopez, C.D.; Neiva, R.F.; Bowers, M.M.; Jimbo, R.; Bonfante, E.A.; Morcos, J.; Witek, L.; Tovar, N.; Coelho, P.G. The effect of osseodensification drilling for endosteal implants with different surface treatments: A study in sheep. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 615–623. [Google Scholar] [CrossRef]
- Açil, Y.; Sievers, J.; Gülses, A.; Ayna, M.; Wiltfang, J.; Terheyden, H. Correlation between resonance frequency, insertion torque and bone-implant contact in self-cutting threaded implants. Odontology 2017, 105, 347–353. [Google Scholar] [CrossRef]
- O’Sullivan, D.; Sennerby, L.; Meredith, N. Measurements comparing the initial stability of five designs of dental implants: A human cadaver study. Clin. Implant Dent. Relat. Res. 2000, 2, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Trisi, P.; Berardini, M.; Falco, A.; Podaliri Vulpiani, M. New Osseodensification Implant Site Preparation Method to Increase Bone Density in Low-Density Bone: In Vivo Evaluation in Sheep. Implant Dent. 2016, 25, 24–31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chávarri-Prado, D.; Brizuela-Velasco, A.; Diéguez-Pereira, M.; Pérez-Pevida, E.; Jiménez-Garrudo, A.; Viteri-Agustín, I.; Estrada-Martínez, A.; Montalbán-Vadillo, O. Influence of cortical bone and implant design in the primary stability of dental implants measured by two different devices of resonance frequency analysis: An in vitro study. J. Clin. Exp. Dent. 2020, 12, e242–e248. [Google Scholar] [CrossRef] [PubMed]
- Comuzzi, L.; Tumedei, M.; Pontes, A.E.; Piattelli, A.; Iezzi, G. Primary Stability of Dental Implants in Low-Density (10 and 20 pcf) Polyurethane Foam Blocks: Conical vs Cylindrical Implants. Int. J. Environ. Res. Public Health 2020, 17, 2617. [Google Scholar] [CrossRef] [PubMed] [Green Version]
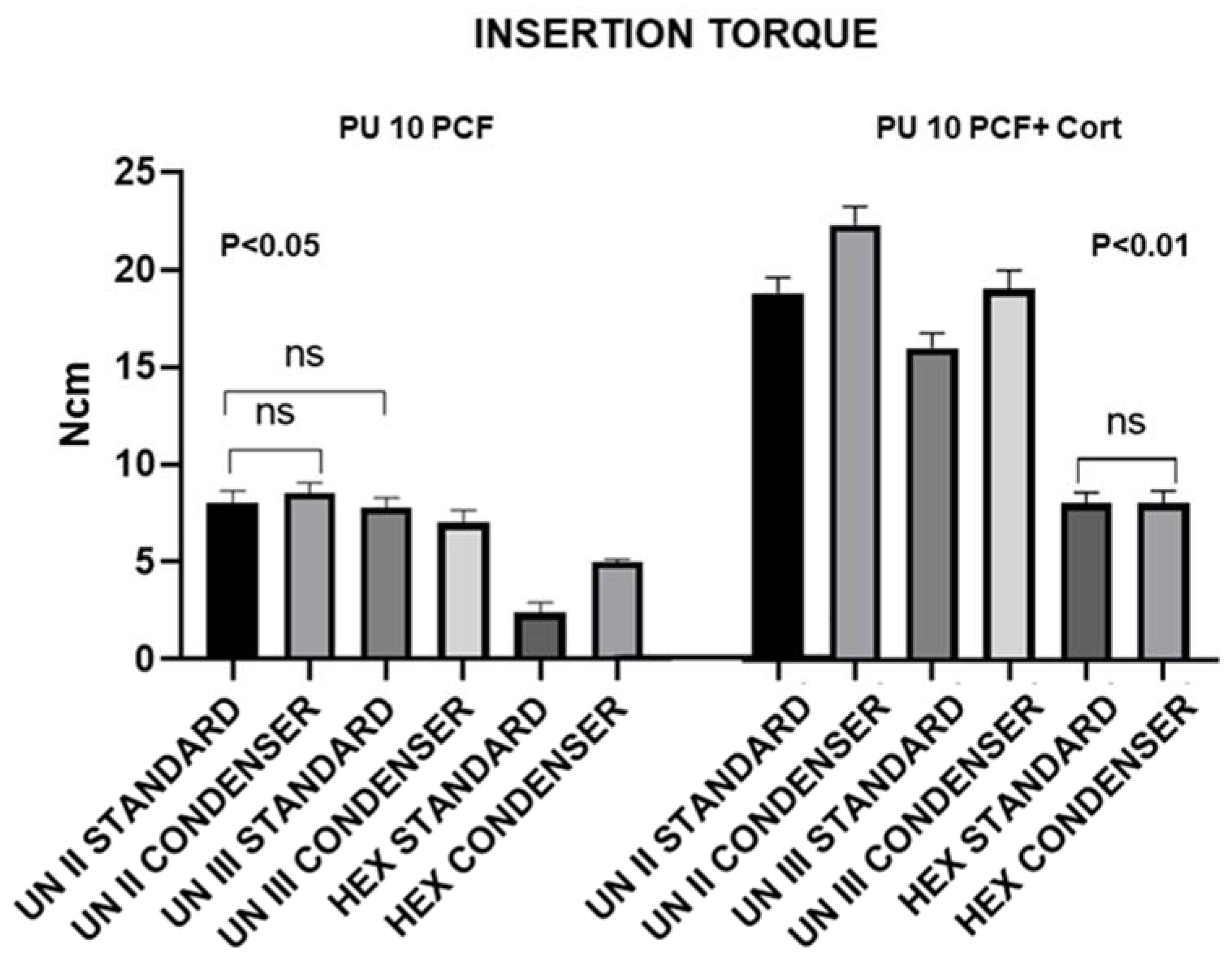
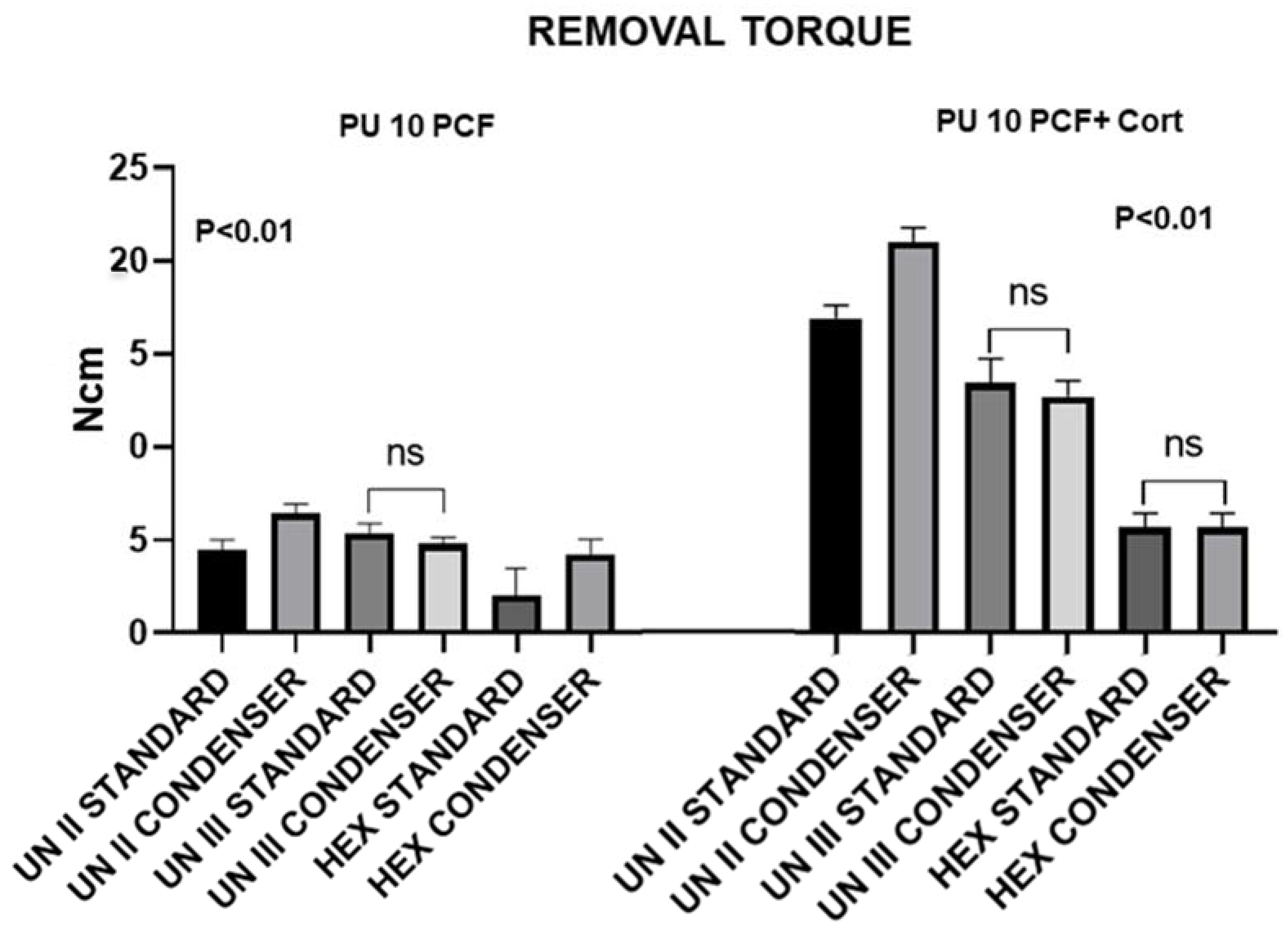
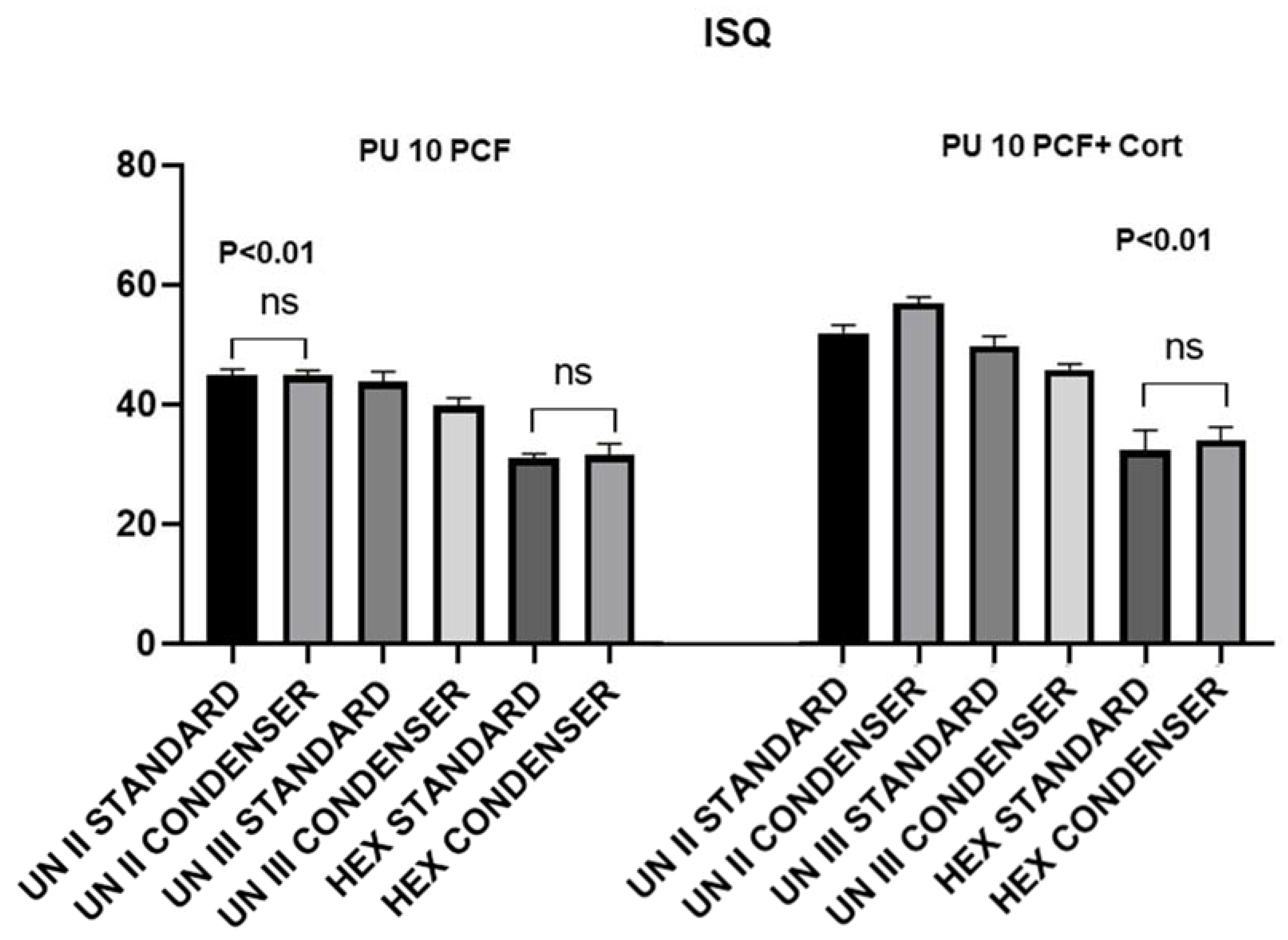


| 10 PCF | 10 PCF/Cort | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| UN II Stand | UN II Cond | UN III Stand | UN III Cond | HEX Stand | HEX Cond | UN II Stand | UN II Cond | UN III Stand | UN III Cond | HEX Stand | HEX Cond | ||
| IT | Mean | 8.00 | 8.53 | 7.78 | 6.99 | 2.41 | 5.01 | 18.8 | 22.3 | 15.96 | 18.99 | 8.02 | 8.02 |
| SD | 0.62 | 0.52 | 0.48 | 0.62 | 0.50 | 0.12 | 0.79 | 0.95 | 0.77 | 0.97 | 0.53 | 0.62 | |
| RT | Mean | 4.5 | 6.4 | 5.4 | 4.8 | 2.01 | 4.26 | 16 | 19.9 | 12.7 | 12 | 5.4 | 5.4 |
| SD | 0.52 | 0.51 | 0.51 | 0.34 | 0.62 | 0.79 | 0.66 | 0.73 | 1.25 | 0.82 | 0.66 | 0.66 | |
| ISQ | Mean | 44.85 | 44.85 | 43.8 | 39.75 | 31 | 31.55 | 52 | 57 | 49.85 | 45.9 | 32.45 | 34.1 |
| SD | 1.06 | 0.85 | 1.67 | 1.32 | 0.78 | 1.86 | 1.37 | 1.05 | 1.67 | 0.94 | 3.34 | 2.21 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Comuzzi, L.; Tumedei, M.; Piattelli, A.; Iezzi, G. Osseodensification Drilling vs. Standard Protocol of Implant Site Preparation: An In Vitro Study on Polyurethane Foam Sheets. Prosthesis 2020, 2, 76-86. https://doi.org/10.3390/prosthesis2020008
Comuzzi L, Tumedei M, Piattelli A, Iezzi G. Osseodensification Drilling vs. Standard Protocol of Implant Site Preparation: An In Vitro Study on Polyurethane Foam Sheets. Prosthesis. 2020; 2(2):76-86. https://doi.org/10.3390/prosthesis2020008
Chicago/Turabian StyleComuzzi, Luca, Margherita Tumedei, Adriano Piattelli, and Giovanna Iezzi. 2020. "Osseodensification Drilling vs. Standard Protocol of Implant Site Preparation: An In Vitro Study on Polyurethane Foam Sheets" Prosthesis 2, no. 2: 76-86. https://doi.org/10.3390/prosthesis2020008
APA StyleComuzzi, L., Tumedei, M., Piattelli, A., & Iezzi, G. (2020). Osseodensification Drilling vs. Standard Protocol of Implant Site Preparation: An In Vitro Study on Polyurethane Foam Sheets. Prosthesis, 2(2), 76-86. https://doi.org/10.3390/prosthesis2020008








