Kinetics of Lower Limb Prosthesis: Automated Detection of Vertical Loading Rate
Abstract
:1. Introduction
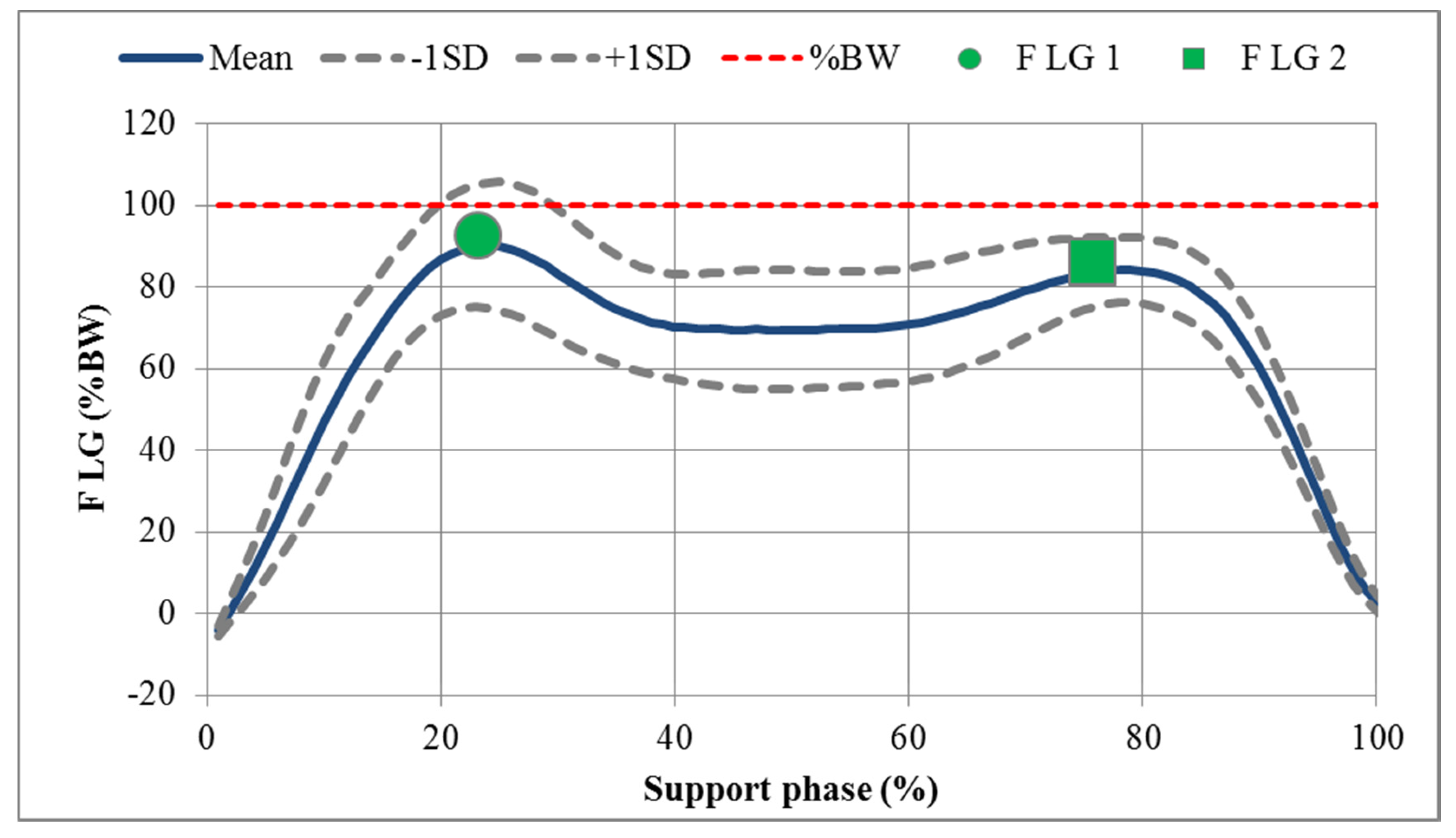
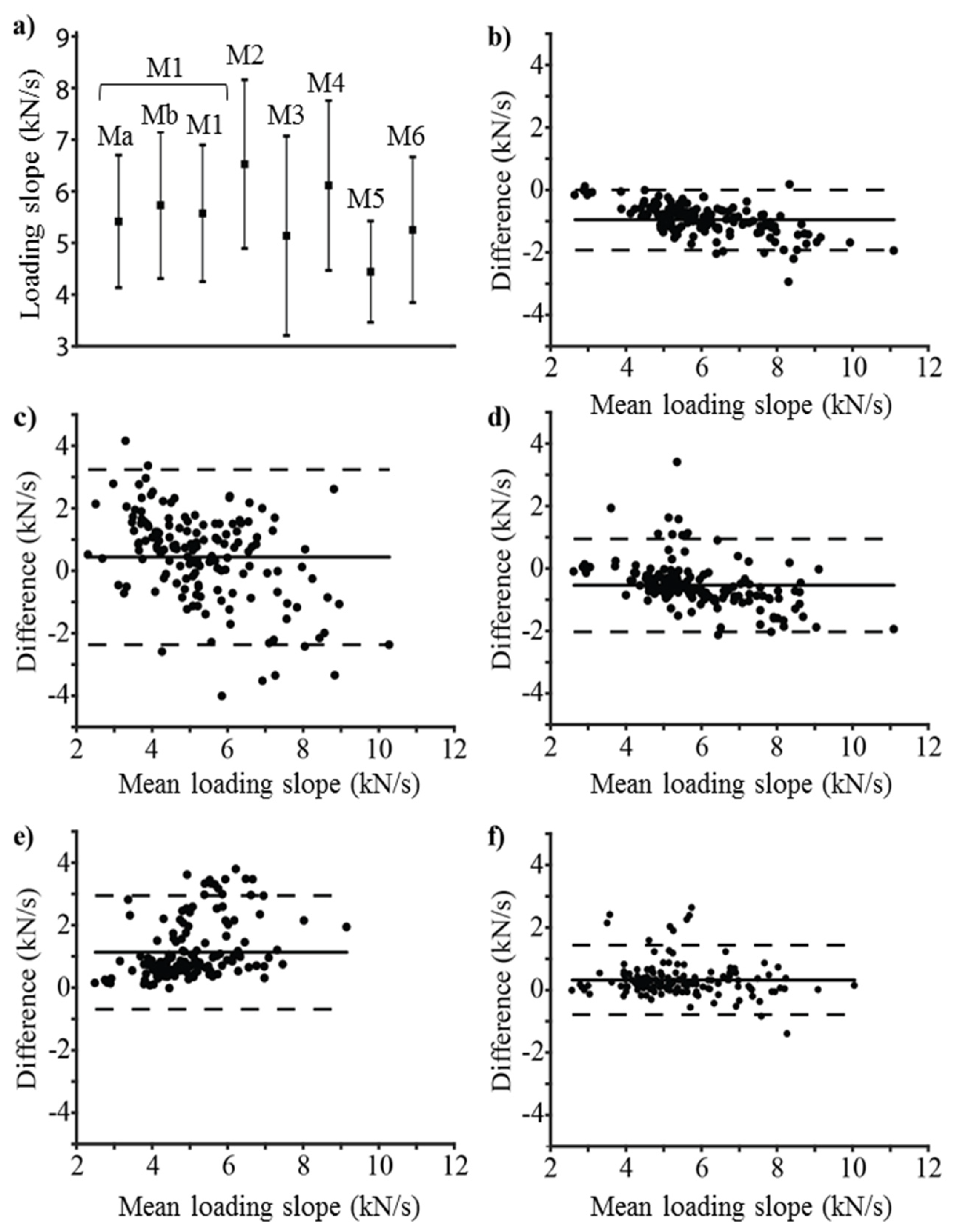
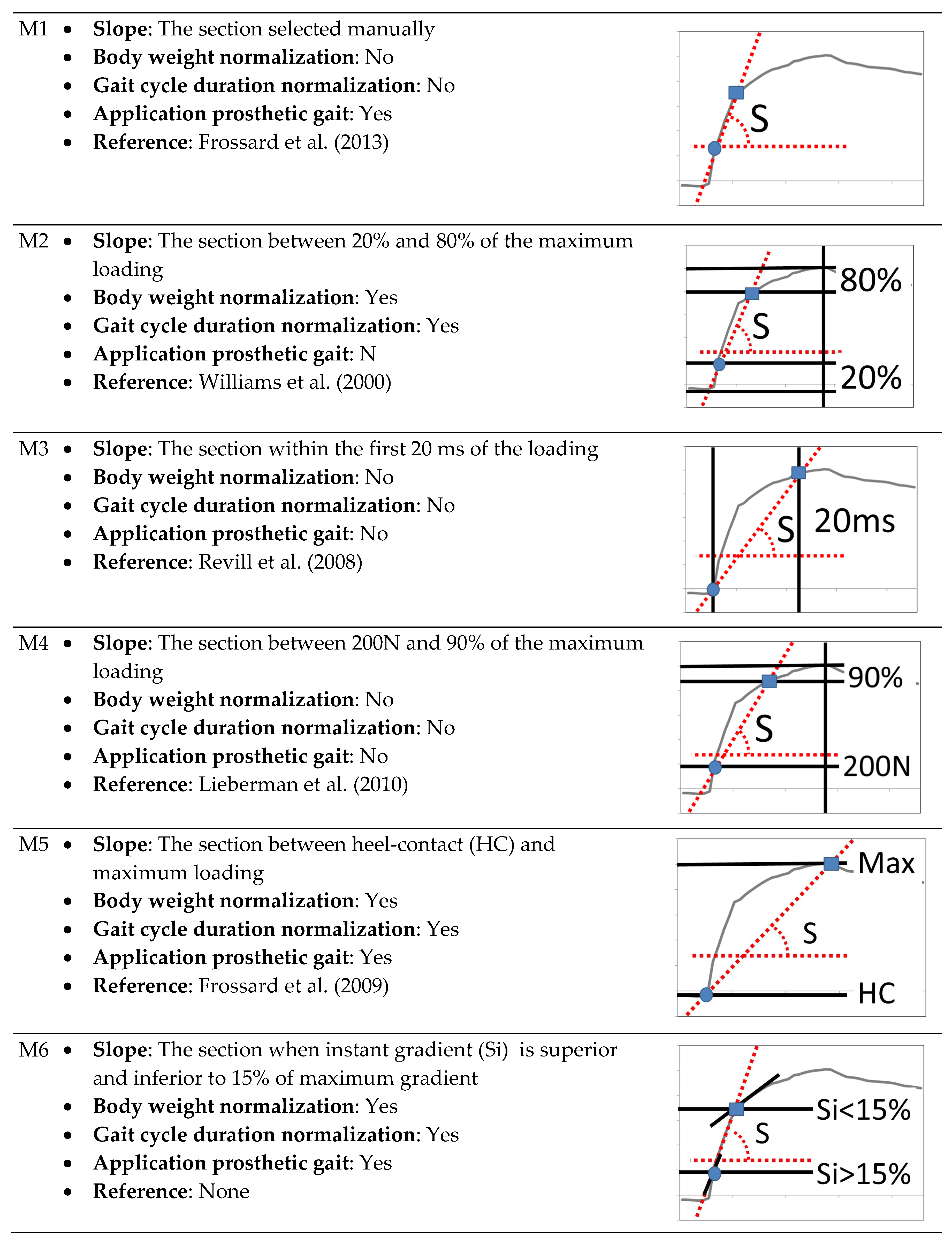
2. Results
3. Discussion
3.1. Limitations
3.2. Interpretation
3.3. Generalizability
3.4. Future Studies
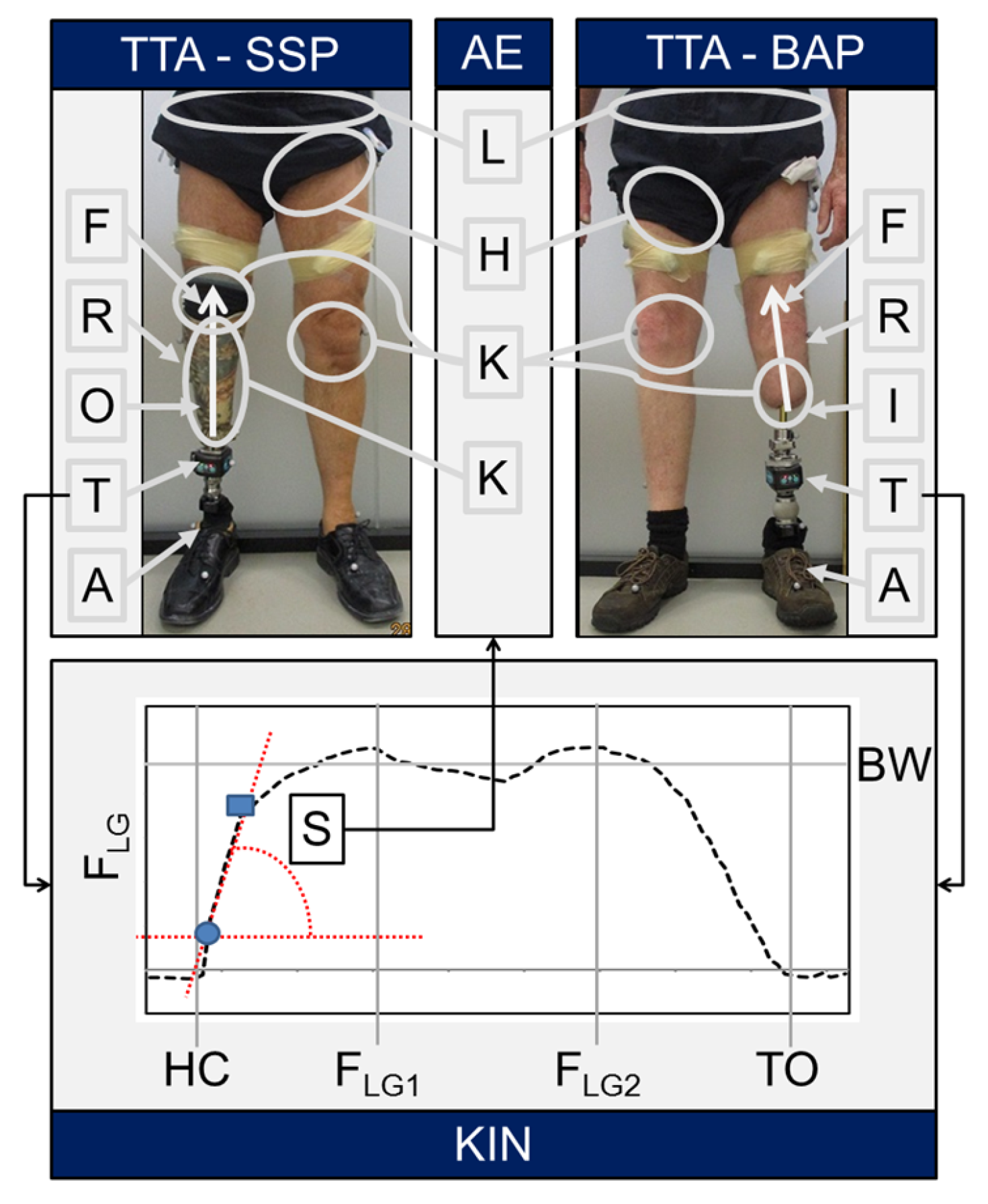
4. Materials and Methods
4.1. Participants
4.2. Apparatus
4.3. Processing
4.4. Analysis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| %GC | Unit of time expressed in percentage of gait cycle |
| %BW | Unit of vertical force (FLG) expressed in percentage of body weight |
| CI | Confidence interval |
| FLG | Force applied on the long axis of the leg |
| FLG1 | First loading peak during the first half of the support phase |
| GC | Gait cycle |
| HC | Heel contact |
| Ma | Slope selected by expert a |
| Mb | Slope selected by expert b |
| Mi | Method i (M1–M6) of automated detection of vertical loading rate |
| S | Vertical loading slope |
| Si | Instantaneous vertical loading slope |
| TO | Toe-off |
References
- Portnoy, S.; Yizhar, Z.; Shabshin, N.; Itzchak, Y.; Kristal, A.; Dotan-Marom, Y.; Siev-Ner, I.; Gefen, A. Internal mechanical conditions in the soft tissues of a residual limb of a trans-tibial amputee. J. Biomech. 2008, 41, 1897–1909. [Google Scholar] [CrossRef] [PubMed]
- Sartori, M.; Llyod, D.G.; Farina, D. Neural data-driven musculoskeletal modeling for personalized neurorehabilitation technologies. IEEE Trans. Biomed. Eng. 2016, 63, 879–893. [Google Scholar] [CrossRef] [PubMed]
- Besier, T.F.; Fredericson, M.; Gold, G.E.; Beaupre, G.S.; Delp, S.L. Knee muscle forces during walking and running in patellofemoral pain patients and pain-free controls. J. Biomech. 2009, 42, 898–905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pather, S.; Vertriest, S.; Sondergeld, P.; Ramis, M.A.; Frossard, L. Load characteristics following transfemoral amputation in individuals fitted with bone-anchored prostheses: A scoping review protocol. JBI Database System. Rev. Implement. Rep. 2018, 16, 1286–1310. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, J.; Zhang, J.; Heidlauf, T.; Sartori, M.; Besier, T.; Röhrle, O.; Lloyd, D. Multiscale musculoskeletal modelling, data–model fusion and electromyography-informed modelling. Interface Focus 2016, 6. [Google Scholar] [CrossRef]
- Sooriakumaran, S.; Uden, M.; Mulroy, S.; Ewins, D.; Collins, T. The impact a surgeon has on primary amputee prosthetic rehabilitation: A survey of residual lower limb quality. Prosthet. Orthot. Int. 2018, 42, 428–436. [Google Scholar] [CrossRef]
- Besier, T.F.; Draper, C.E.; Gold, G.E.; Beaupre, G.S.; Delp, S.L. Patellofemoral joint contact area increases with knee flexion and weight-bearing. J. Orthop. Res. 2005, 23, 345–350. [Google Scholar] [CrossRef]
- Besier, T.F.; Gold, G.E.; Delp, S.L.; Fredericson, M.; Beaupre, G.S. The influence of femoral internal and external rotation on cartilage stresses within the patellofemoral joint. J. Orthop. Res. 2008, 26, 1627–1635. [Google Scholar] [CrossRef] [Green Version]
- Boone, D.A.; Kobayashi, T.; Chou, T.G.; Arabian, A.K.; Coleman, K.L.; Orendurff, M.S.; Zhang, M. Influence of malalignment on socket reaction moments during gait in amputees with transtibial prostheses. Gait Posture 2013, 37, 620–626. [Google Scholar] [CrossRef]
- Kobayashi, T.; Arabian, A.K.; Orendurff, M.S.; Rosenbaum-Chou, T.G.; Boone, D.A. Effect of alignment changes on socket reaction moments while walking in transtibial prostheses with energy storage and return feet. Clin. Biomech. (Bristol Avon) 2014, 29, 47–56. [Google Scholar] [CrossRef]
- Kobayashi, T.; Orendurff, M.S.; Zhang, M.; Boone, D.A. Individual responses to alignment perturbations in socket reaction moments while walking in transtibial prostheses. Clin. Biomech. (Bristol Avon) 2014, 29, 590–594. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Orendurff, M.S.; Arabian, A.K.; Rosenbaum-Chou, T.G.; Boone, D.A. Effect of prosthetic alignment changes on socket reaction moment impulse during walking in transtibial amputees. J. Biomech. 2014, 47, 1315–1323. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Orendurff, M.S.; Zhang, M.; Boone, D.A. Socket reaction moments in transtibial prostheses during walking at clinically perceived optimal alignment. Prosthet. Orthot. Int. 2015, 40, 503–508. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paterno, L.; Ibrahimi, M.; Gruppioni, E.; Menciassi, A.; Ricotti, L. Sockets for limb prostheses: A review of existing technologies and open challenges. IEEE Trans. Biomed. Eng. 2018, 65, 1996–2010. [Google Scholar] [CrossRef] [PubMed]
- Vertriest, S.; Pather, S.; Sondergeld, P.; Frossard, L. Rehabilitation programs after the implantation of transfemoral osseointegrated fixations for bone-anchored prostheses: A scoping review protocol. JBI Database System. Rev. Implement. Rep. 2017, 15, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Vertriest, S.; Coorevits, P.; Hagberg, K.; Branemark, R.; Haggstrom, E.E.; Vanderstraeten, G.; Frossard, L.A. Static load bearing exercises of individuals with transfemoral amputation fitted with an osseointegrated implant: Loading compliance. Prosthet. Orthot. Int. 2017, 41, 393–401. [Google Scholar] [CrossRef]
- Vertriest, S.; Coorevits, P.; Hagberg, K.; Branemark, R.; Haggstrom, E.; Vanderstraeten, G.; Frossard, L. Static load bearing exercises of individuals with transfemoral amputation fitted with an osseointegrated implant: Reliability of kinetic data. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 423–430. [Google Scholar] [CrossRef]
- Frossard, L.; Cheze, L.; Dumas, R. Dynamic input to determine hip joint moments, power and work on the prosthetic limb of transfemoral amputees: Ground reaction vs knee reaction. Prosthet. Orthot. Int. 2011, 35, 140–149. [Google Scholar] [CrossRef]
- Dumas, R.; Branemark, R.; Frossard, L. Gait analysis of transfemoral amputees: Errors in inverse dynamics are substantial and depend on prosthetic design. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 679–685. [Google Scholar] [CrossRef]
- Dumas, R.; Cheze, L.; Frossard, L. Loading applied on prosthetic knee of transfemoral amputee: Comparison of inverse dynamics and direct measurements. Gait Posture 2009, 30, 560–562. [Google Scholar] [CrossRef] [Green Version]
- Neumann, E.; Frossard, L.; Ramos, M.; Bidwell, K. Prosthesis: Load cell applicability to outcome measurement—Chapter 6. In Advances in Medicine and Biology; Berhardt, L.V., Ed.; Nova Science Publishers: New York, NY, USA, 2017; pp. 133–172. [Google Scholar]
- Stephenson, P.; Seedhom, B.B. Estimation of forces at the interface between an artificial limb and an implant directly fixed into the femur in above-knee amputees. J. Orthop. Sci. 2002, 7, 192–297. [Google Scholar] [CrossRef] [PubMed]
- Dumas, R.; Cheze, L.; Frossard, L. Load during prosthetic gait: Is direct measurement better than inverse dynamics? Gait Posture 2009, 30, S86–S87. [Google Scholar] [CrossRef] [Green Version]
- Koehler, S.R.; Dhaher, Y.Y.; Hansen, A.H. Cross-validation of a portable, six-degree-of-freedom load cell for use in lower-limb prosthetics research. J. Biomech. 2014, 47, 1542–1547. [Google Scholar] [CrossRef] [PubMed]
- Thesleff, A.; Ludvigsson, S.; Ohr, E.; Ortiz-Catalan, M. Load exposure of osseointegrated implants for transfemoral limb prosthesis during running. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2018, 1743–1746. [Google Scholar] [CrossRef]
- Frossard, L.; Stevenson, N.; Sullivan, J.; Uden, M.; Pearcy, M. Categorization of activities of daily living of lower limb amputees during short-term use of a portable kinetic recording system: A preliminary study. J. Prosthet. Orthot. 2011, 23, 2–11. [Google Scholar] [CrossRef]
- Frossard, L.; Stevenson, N.; Smeathers, J.; Haggstrom, E.; Hagberg, K.; Sullivan, J.; Ewins, D.; Lee Gow, D.; Gray, S.; Branemark, R. Monitoring of the load regime applied on the osseointegrated fixation of a trans-femoral amputee: A tool for evidence-based practice. Prosthet. Orthot. Int. 2008, 32, 68–78. [Google Scholar] [CrossRef]
- Futamure, S.; Bonnet, V.; Dumas, R.; Venture, G. A sensitivity analysis method for the body segment inertial parameters based on ground reaction and joint moment regressor matrices. J. Biomech. 2017, 64, 85–92. [Google Scholar] [CrossRef]
- Narang, Y.S.; Arelekatti, V.N.; Winter, A.G. The effects of prosthesis inertial properties on prosthetic knee moment and hip energetics required to achieve able-bodied kinematics. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 754–763. [Google Scholar] [CrossRef]
- Chia Bejarano, N.; Ambrosini, E.; Pedrocchi, A.; Ferrigno, G.; Monticone, M.; Ferrante, S. A novel adaptive, real-time algorithm to detect gait events from wearable sensors. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 413–422. [Google Scholar] [CrossRef]
- Crea, S.; Cipriani, C.; Donati, M.; Carrozza, M.C.; Vitiello, N. Providing time-discrete gait information by wearable feedback apparatus for lower-limb amputees: Usability and functional validation. IEEE Trans. Neural Syst. Rehabil. Eng. 2015, 23, 250–257. [Google Scholar] [CrossRef]
- Khandelwal, S.; Wickstrom, N. Gait event detection in real-world environment for long-term applications: incorporating domain knowledge into time-frequency analysis. IEEE Trans. Neural Syst. Rehabil. Eng. 2016, 24, 1363–1372. [Google Scholar] [CrossRef] [PubMed]
- Maqbool, H.F.; Husman, M.A.B.; Awad, M.I.; Abouhossein, A.; Iqbal, N.; Dehghani-Sanij, A.A. A real-time gait event detection for lower limb prosthesis control and evaluation. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 1500–1509. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; D’Andrea, S.E.; Nunnery, M.J.; Kay, S.M.; Huang, H. Towards design of a stumble detection system for artificial legs. IEEE Trans. Neural Syst. Rehabil. Eng. 2011, 19, 567–577. [Google Scholar] [CrossRef] [PubMed]
- Frossard, L.; Beck, J.; Dillon, M.; Chappell, M.; Evans, J.H. Development and preliminary testing of a device for the direct measurement of forces and moments in the prosthetic limb of transfemoral amputees during activities of daily living. J. Prosthet. Orthot. 2003, 15, 135–142. [Google Scholar] [CrossRef]
- Neumann, E.S.; Brink, J.; Yalamanchili, K.; Lee, J.S. Regression estimates of pressure on transtibial residual limbs using load cell measurements of the forces and moments occurring at the base of the socket. JPO J. Prosthet. Orthot. 2013, 25, 1–12. [Google Scholar] [CrossRef]
- Neumann, E.S.; Brink, J.; Yalamanchili, K.; Lee, J.S. Use of a load cell and force-moment analysis to examine transtibial prosthesis foot rollover kinetics for anterior-posterior alignment perturbations. JPO J. Prosthet. Orthot. 2012, 24, 160–174. [Google Scholar] [CrossRef]
- Lee, W.; Frossard, L.; Hagberg, K.; Haggstrom, E.; Brånemark, R. Kinetics analysis of transfemoral amputees fitted with osseointegrated fixation performing common activities of daily living. Clin. Biomech. 2007, 22, 665–673. [Google Scholar] [CrossRef]
- Lee, W.; Frossard, L.; Hagberg, K.; Haggstrom, E.; Lee Gow, D.; Gray, S.; Branemark, R. Magnitude and variability of loading on the osseointegrated implant of transfemoral amputees during walking. Med. Eng. Phys. 2008, 30, 825–833. [Google Scholar] [CrossRef] [Green Version]
- Frossard, L.; Hagberg, K.; Haggstrom, E.; Branemark, R. Load-relief of walking aids on osseointegrated fixation: Instrument for evidence-based practice. IEEE Trans. Neural Syst. Rehabil. Eng. 2009, 17, 9–14. [Google Scholar] [CrossRef]
- Frossard, L.; Tranberg, R.; Haggstrom, E.; Pearcy, M.; Branemark, R. Fall of a transfemoral amputee fitted with osseointegrated fixation: Loading impact on residuum. Gait Posture 2009, 30, S151–S152. [Google Scholar] [CrossRef] [Green Version]
- Frossard, L.; Gow, D.L.; Hagberg, K.; Cairns, N.; Contoyannis, B.; Gray, S.; Branemark, R.; Pearcy, M. Apparatus for monitoring load bearing rehabilitation exercises of a transfemoral amputee fitted with an osseointegrated fixation: A proof-of-concept study. Gait Posture 2010, 31, 223–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frossard, L.; Hagberg, K.; Häggström, E.; Gow, D.L.; Brånemark, R.; Pearcy, M. Functional outcome of transfemoral amputees fitted with an osseointegrated fixation: Temporal gait characteristics. J. Prosthet. Orthot. 2010, 22, 11–20. [Google Scholar] [CrossRef]
- Frossard, L.A. Load on osseointegrated fixation of a transfemoral amputee during a fall: Determination of the time and duration of descent. Prosthet. Orthot. Int. 2010, 34, 472–487. [Google Scholar] [CrossRef] [PubMed]
- Frossard, L.A.; Tranberg, R.; Haggstrom, E.; Pearcy, M.; Branemark, R. Load on osseointegrated fixation of a transfemoral amputee during a fall: Loading, descent, impact and recovery analysis. Prosthet. Orthot. Int. 2010, 34, 85–97. [Google Scholar] [CrossRef] [PubMed]
- Frossard, L.; Haggstrom, E.; Hagberg, K.; Branemark, P. Load applied on a bone-anchored transfemoral prosthesis: Characterisation of prosthetic components—A case study. J. Rehabil. Res. Dev. 2013, 50, 619–634. [Google Scholar] [CrossRef]
- Neumann, E.S.; Yalamanchili, K.; Brink, J.; Lee, J.S. Transducer-based comparisons of the prosthetic feet used by transtibial amputees for different walking activities: A pilot study. Prosthet. Orthot. Int. 2012, 36, 203–216. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.C.; Doocey, J.M.; Branemark, R.; Adam, C.J.; Evans, J.H.; Pearcy, M.J.; Frossard, L.A. FE stress analysis of the interface between the bone and an osseointegrated implant for amputees--implications to refine the rehabilitation program. Clin. Biomech. (Bristol Avon) 2008, 23, 1243–1250. [Google Scholar] [CrossRef]
- Helgason, B.; Palsson, H.; Runarsson, T.P.; Frossard, L.; Viceconti, M. Risk of failure during gait for direct skeletal attachment of a femoral prosthesis: A finite element study. Med. Eng. Phys. 2009, 31, 595–600. [Google Scholar] [CrossRef] [Green Version]
- Frossard, L. Loading characteristics data applied on osseointegrated implant by transfemoral bone-anchored prostheses fitted with basic components during daily activities. Data Br. 2019, 26, 104492. [Google Scholar] [CrossRef]
- Lieberman, D.E.; Venkadesan, M.; Werbel, W.A.; Dauod, A.I.; D’Andrea, S.; Davis, I.S.; Mang’Eni, R.O.; Pitsiladis, Y. Foot strike patterns and collison forces in habitually barefoot versus shod runners. Nature 2010, 463, 531–535. [Google Scholar] [CrossRef]
- Revill, A.L.; Perry, S.D.; Michelle Edwards, A.; Dickey, J.P. Variability of the impact transient during repeated barefoot walking trials. J. Biomech. 2008, 41, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Williams III, D.S.; McClay, I.S.; Manal, K.T. Lower extremity mechanics in runners with a converted forefoot strike pattern. J. Appl. Biomech. 2000, 16, 210–218. [Google Scholar] [CrossRef]
- An, W.; Rainbow, M.J.; Cheung, R.T. Effects of surface inclination on the vertical loading rates and landing pattern during the first attempt of barefoot running in habitual shod runners. Biomed. Res. Int. 2015, 2015, 240153. [Google Scholar] [CrossRef] [PubMed]
- Orendurff, M.S. Literature review of published research investigating microprocessor-controlled prosthetic knees: 2010–2012. JPO J. Prosthet. Orthot. 2013, 25, P41–P46. [Google Scholar] [CrossRef]
- Copay, A.G.; Subach, B.R.; Glassman, S.D.; Polly, D.W., Jr.; Schuler, T.C. Understanding the minimum clinically important difference: A review of concepts and methods. Spine J. 2007, 7, 541–546. [Google Scholar] [CrossRef]
- Hansen, M.; Haugland, M.K.; Sinkjaer, T. Evaluating robustness of gait event detection based on machine learning and natural sensors. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 81–88. [Google Scholar] [CrossRef]
- Pitkin, M.; Cassidy, C.; Muppavarapu, R.; Edell, D. Recording of electric signal passage trough a pylon in direct skeletal attachment of leg prostheses. IEEE Trans. Biomed. Eng. 2012, 59, 1349–1353. [Google Scholar] [CrossRef]
- Douglas, T.; Solomonidis, S.; Sandham, W.; Spence, W. Ultrasound imaging in lower limb prosthetics. IEEE Trans. Neural Syst. Rehabil. Eng. 2002, 10, 11–21. [Google Scholar] [CrossRef]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frossard, L.; Jones, M.W.M.; Stewart, I.; Leggat, P.A.; Schuetz, M.; Langton, C. Kinetics of Lower Limb Prosthesis: Automated Detection of Vertical Loading Rate. Prosthesis 2019, 1, 16-28. https://doi.org/10.3390/prosthesis1010004
Frossard L, Jones MWM, Stewart I, Leggat PA, Schuetz M, Langton C. Kinetics of Lower Limb Prosthesis: Automated Detection of Vertical Loading Rate. Prosthesis. 2019; 1(1):16-28. https://doi.org/10.3390/prosthesis1010004
Chicago/Turabian StyleFrossard, Laurent, Michael W. M. Jones, Ian Stewart, Peter A. Leggat, Michael Schuetz, and Christian Langton. 2019. "Kinetics of Lower Limb Prosthesis: Automated Detection of Vertical Loading Rate" Prosthesis 1, no. 1: 16-28. https://doi.org/10.3390/prosthesis1010004
APA StyleFrossard, L., Jones, M. W. M., Stewart, I., Leggat, P. A., Schuetz, M., & Langton, C. (2019). Kinetics of Lower Limb Prosthesis: Automated Detection of Vertical Loading Rate. Prosthesis, 1(1), 16-28. https://doi.org/10.3390/prosthesis1010004





