Sound Environment during Dental Treatment in Relation to COVID-19 Pandemic
Abstract
:1. Introduction
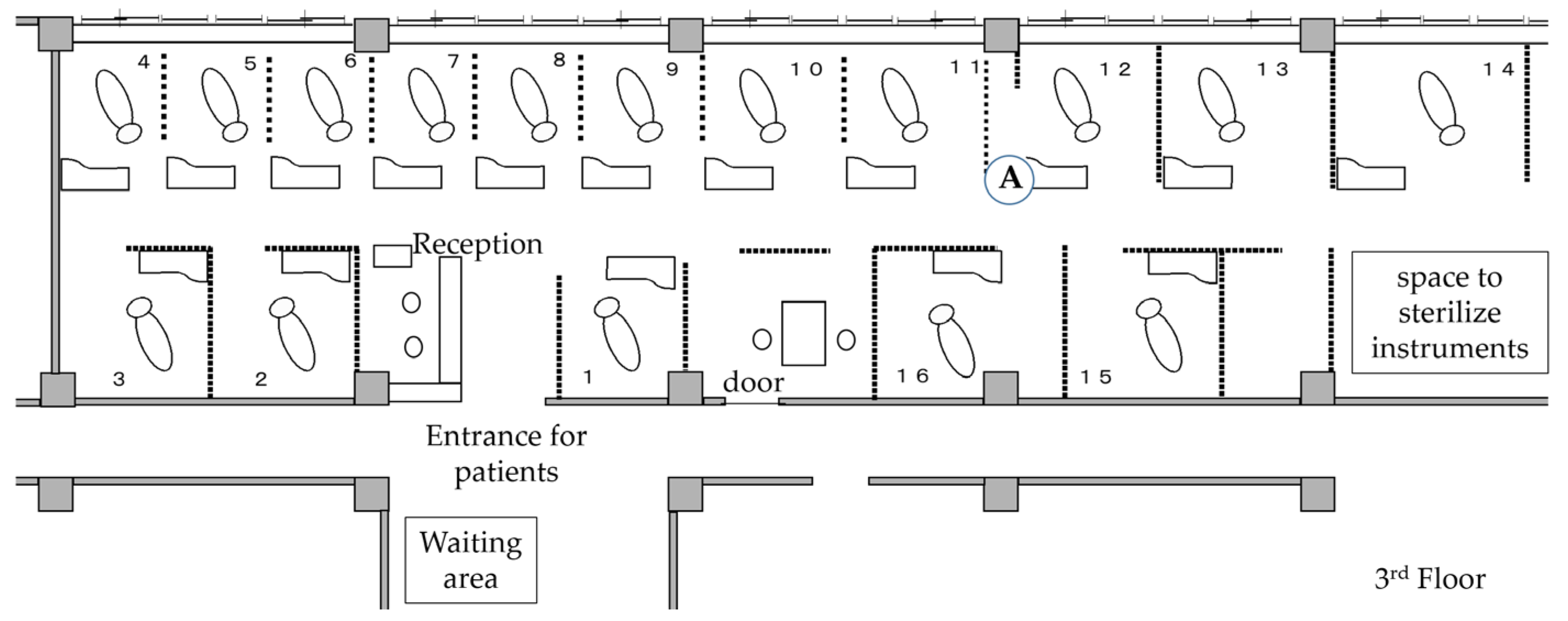
2. Materials and Methods
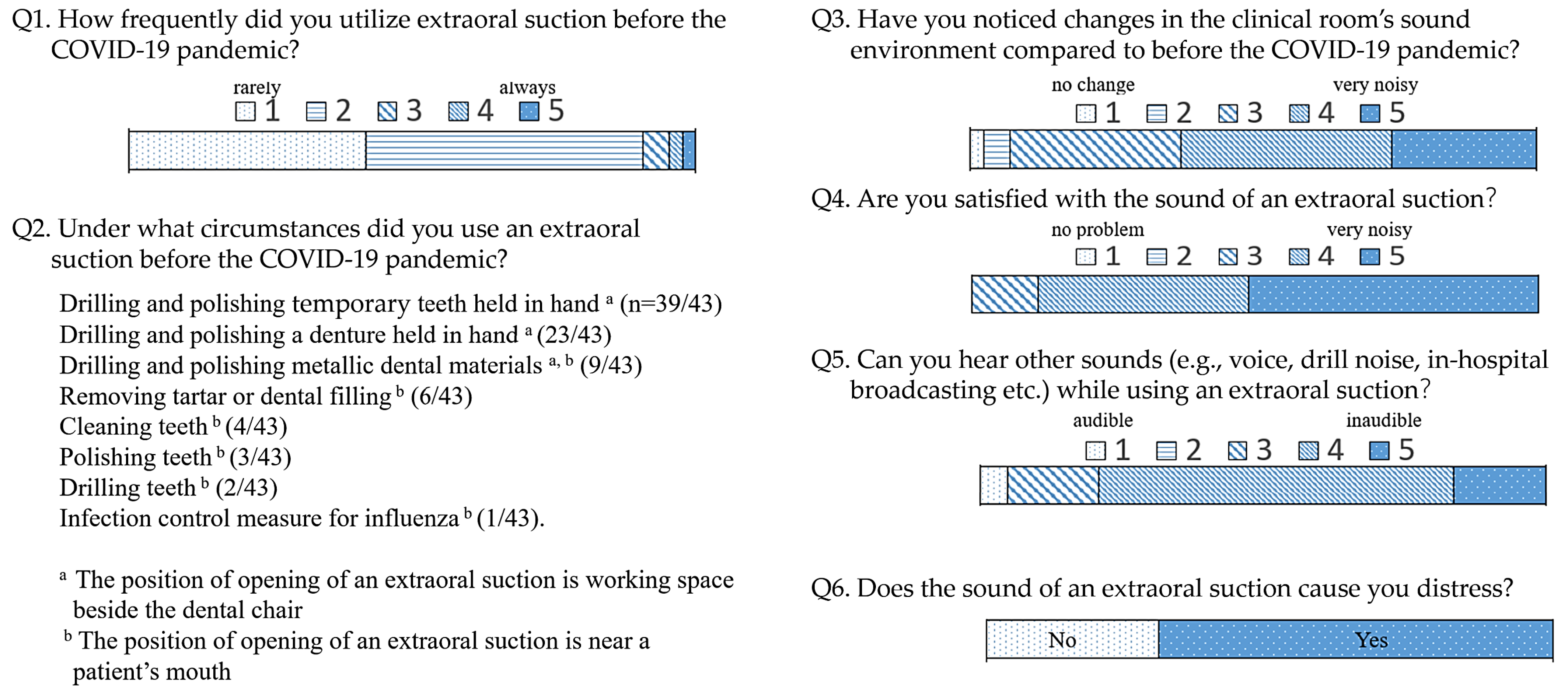
2.1. Questionnaire Survey
- “How frequently did you utilize extraoral suction before the COVID-19 pandemic?”
- “Under what circumstances did you use it before the COVID-19 pandemic?”
- “Have you noticed changes in the clinical room’s sound environment compared to before the COVID-19 pandemic?”
- “Are you satisfied with the sound produced by the extraoral suction?”
- “Can you hear other sounds (e.g., voices, drill noise, music, in-hospital broadcasts, telephone, etc.) while using extraoral suction?”
- “Does the sound emitted by the extraoral suction cause you distress?”
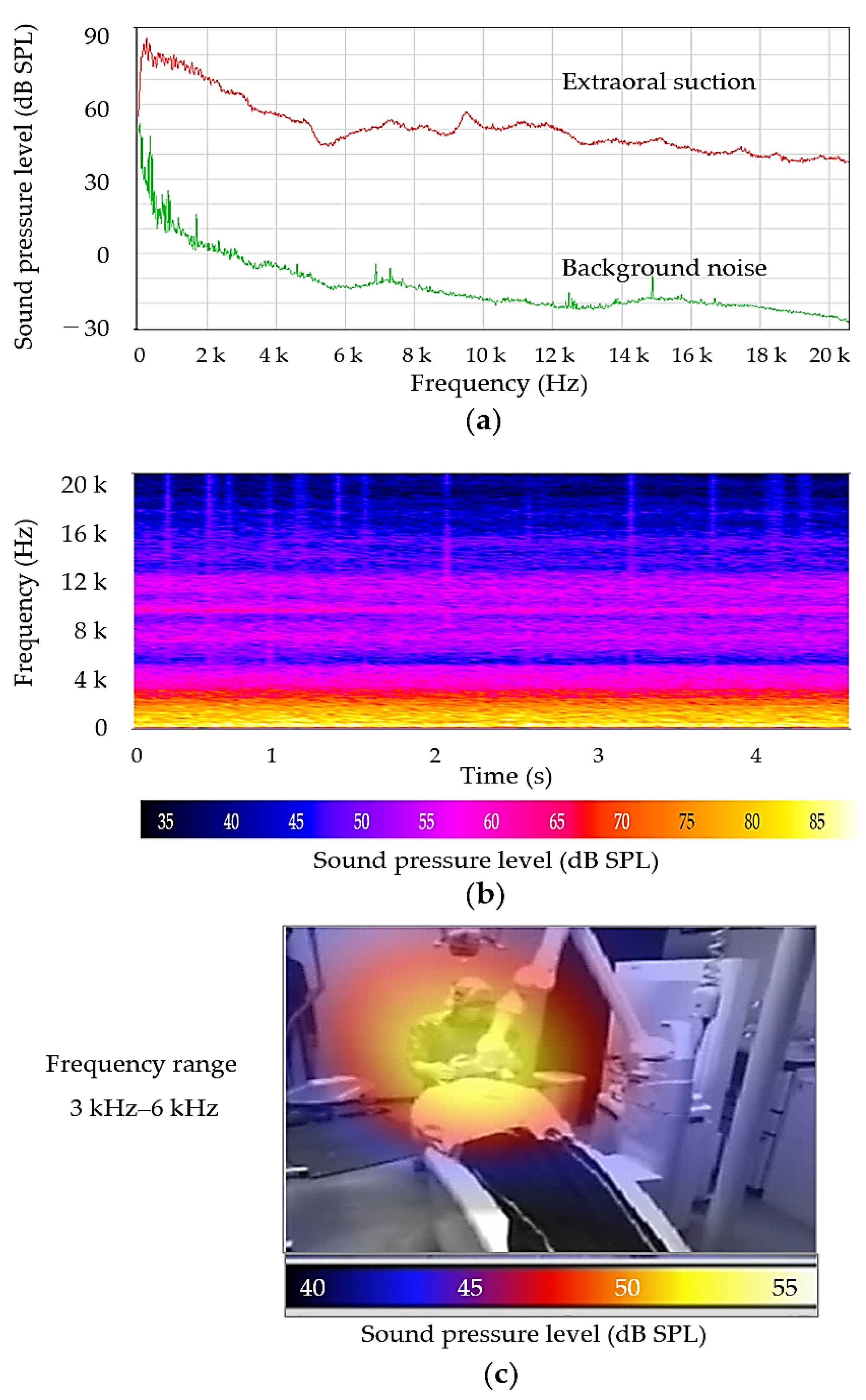
2.2. Measurement of Sound Levels at Extraoral Suction Openings
2.3. Visualization of Extraoral Suction Sound with Actual Usage Condition
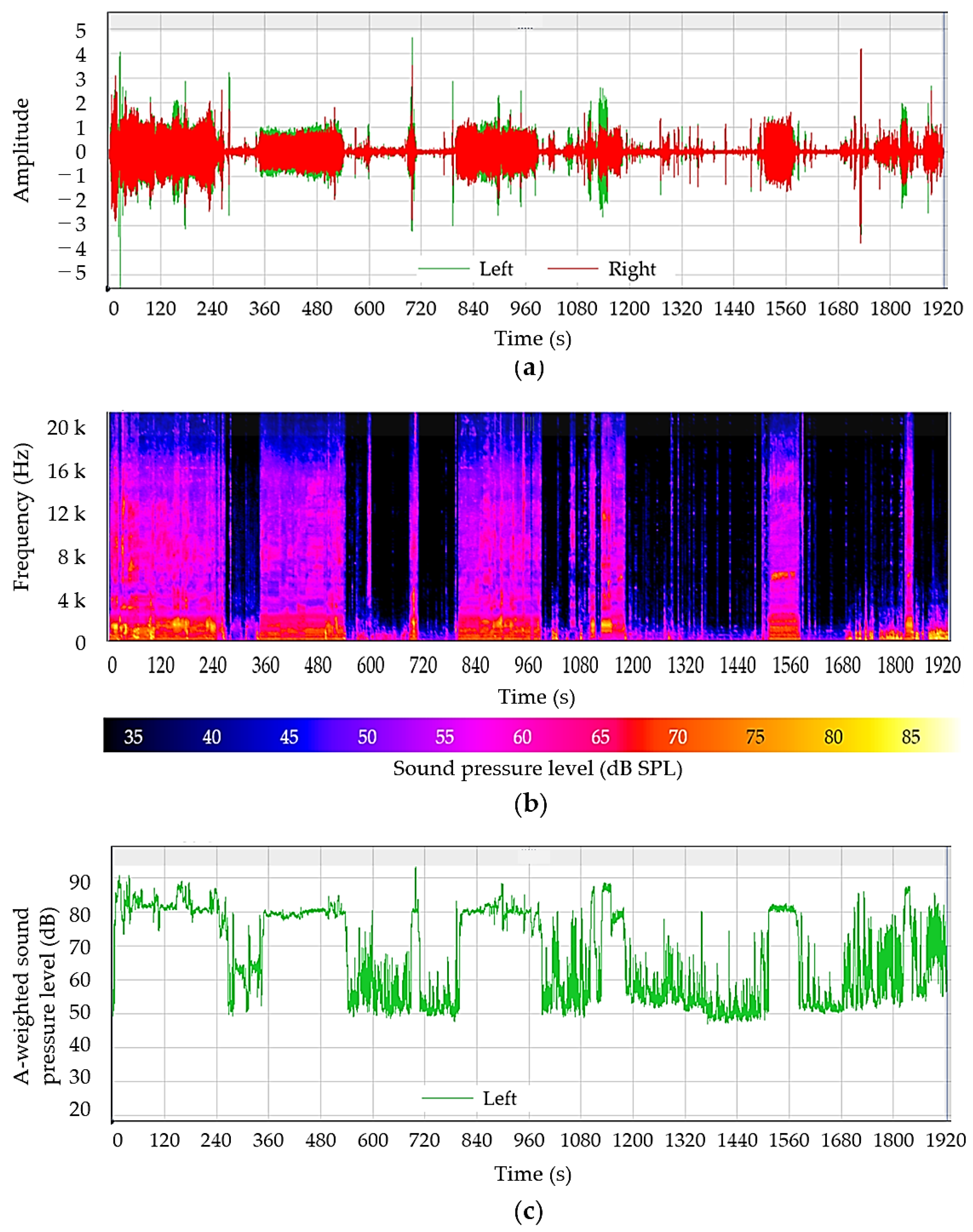
2.4. Sound Levels Heard by the Dentist during Dental Clinical Treatment with Aerosol Control
2.5. Measurement of Sound Levels in the Clinical Room
3. Results
3.1. Questionnaire Survey
3.2. Measurement of Sound Levels at the Position of the Opening of Extraoral Suctions
3.3. Acoustic Imaging of Extraoral Suction Sound with Actual Usage Condition
3.4. Sound Quantity and Quality of Noise Heard by the Dentist during Clinical Treatment
3.5. Sound Levels and Sound Sources in the Clinical Room
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Occupational Safety and Health Administration (OSHA). OSHA Technical Manual (OMC), Chapter 5; US Department of Labor: Washington, DC, USA, 2013. Available online: https://www.osha.gov/otm/section-3-health-hazards/chapter-5 (accessed on 10 October 2023).
- Sampaio Fernandes, J.C.; Carvalho, A.P.; Gallas, M.; Vaz, P.; Matos, P.A. Noise levels in dental schools. Eur. J. Dent. Educ. 2006, 10, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Setcos, J.C.; Mahyuddin, A. Noise levels encountered in dental clinical and laboratory practice. Int. J. Prosthodont. 1998, 11, 150–157. [Google Scholar] [PubMed]
- Dierickx, M.; Verschraegen, S.; Wierinck, E.; Willems, G.; van Wieringen, A. Noise Disturbance and Potential Hearing Loss Due to Exposure of Dental Equipment in Flemish Dentists. Int. J. Environ. Res. Public Health 2021, 18, 5617. [Google Scholar] [CrossRef] [PubMed]
- Baseer, M.A.; Al Saffan, A.; AlMasoud, S.M.; Dahy, W.T.; Aldali, H.W.; Walid Bachat, A.M.; Walid Bachat, R.M.; AlMugeiren, O.M. Noise levels encountered in university dental clinics during different specialty treatments. J. Fam. Med. Prim. Care 2021, 10, 2987–2992. [Google Scholar] [CrossRef]
- da Cunha, K.F.; Dos Santos, R.B.; Klien Júnior, C.A. Assessment of noise intensity in a dental teaching clinic. BDJ Open 2017, 3, 17010. [Google Scholar] [CrossRef]
- Goswami, M.; Singh, D.; Vashist, B.; Marwaha, S. Noise levels and sound pollution associated with various operative procedures and equipment in a pediatric dental environment—A clinical study. J. Oral Biol. Craniofac. Res. 2017, 7, 182–187. [Google Scholar] [CrossRef]
- Lehto, T. Dentists’ hearing and exposure to high speed turbine dental drill noise. Proc. Finn. Dent. Soc. 1990, 86, 115–125. [Google Scholar]
- Jiang, P.; Atherton, M.A.; Millar, B.J. A Passive Noise Attenuation Earplug Designed to Minimise Unwanted Air Turbine Driven High-Speed Dental Drill Noise. Eur. J. Prosthodont. Restor. Dent. 2023, 31, 262–277. [Google Scholar]
- Wilson, C.E.; Vaidyanathan, T.K.; Cinotti, W.R.; Cohen, S.M.; Wang, S.J. Hearing-damage Risk and Communication Interference in Dental Practice. J. Dent. Res. 1990, 69, 489–493. [Google Scholar] [CrossRef]
- Yamada, T.; Ebisu, S.; Kuwano, S. A questionnaire survey on the effect of the sound of dental drills on the feeling of patients in dental clinics. Acoust. Sci. Technol. 2006, 27, 305–308. [Google Scholar] [CrossRef]
- Yamada, T.; Kuwano, S.; Ebisu, S.; Hayashi, M. Effect of processing of dental drill noise on subjective impression. Appl. Acoust. 2021, 177, 107895. [Google Scholar] [CrossRef]
- Yamada, T.; Kuwano, S.; Ebisu, S.; Hayashi, M. Statistical analysis for subjective and objective evaluations of dental drill sounds. PLoS ONE 2016, 11, e0159926. [Google Scholar] [CrossRef]
- ISO 14457; Dentistry—Handpieces and Motors. International Organization for Standardization: Geneve, Switzerland, 2017.
- Froum, S.H.; Froum, S.J. Incidence of COVID-19 Virus Transmission in Three Dental Offices: A 6-Month Retrospective Study. Int. J. Periodontics Restor. Dent. 2020, 40, 853–859. [Google Scholar] [CrossRef]
- Wong, C.K.; Tsang, D.N.C.; Chan, R.C.W.; Lam, E.T.K.; Jong, K.K. Infection risks faced by public health laboratory Services Teams when handling specimens associated with coronavirus Disease 2019 (COVID-19). Saf. Health Work 2020, 11, 372–377. [Google Scholar] [CrossRef] [PubMed]
- Kranz, A.M.; Chen, A.; Gahlon, G.; Stein, B.D. 2020 trends in dental office visits during the COVID-19 pandemic. J. Am. Dent. Assoc. 2021, 152, 535–541. [Google Scholar] [CrossRef]
- Iwasaki, S.; Fujisawa, S.; Nakakubo, S.; Kamada, K.; Yamashita, Y.; Fukumoto, T.; Sato, K.; Oguri, S.; Taki, K.; Senjo, H.; et al. Comparison of SARS-CoV-2 detection in nasopharyngeal swab and saliva. J. Infect. 2020, 81, e145–e147. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). 3. Setting-Specific Considerations, Dental Facilities, Interim Infection Prevention and Control Recommendations for Healthcare Personnel during the Coronavirus Disease 2019 (COVID-19) Pandemic; US Department of Health & Human Services: Washington, DC, USA, 2023. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html (accessed on 27 September 2023).
- Japan Dental Association (JDA). Guidelines for Dental Practice Based on New Infectious Diseases, first edition. J. Jpn. Dent. Assoc. 2020, 73, 807–818. (In Japanese) [Google Scholar]
- Osaka University Dental Hospital: Osaka, Japan. Available online: https://hospital.dent.osaka-u.ac.jp/index-e.html (accessed on 27 September 2023).
- Nambu, E.; Nozaki, K.; Tsubokura, M.; Hayashi, M. Numerical simulation of air age in dental offices. Sci. Rep. 2022, 12, 14120. [Google Scholar] [CrossRef]
- Ono Sokki LA-7000, Sound Level Meter. Available online: https://www.onosokki.co.jp/English/hp_e/products/keisoku/s_v/la7000.htm (accessed on 27 September 2023).
- CAE Software und Systems GmbH SoundCam 2.0. Available online: https://soundcam.com/ (accessed on 27 September 2023).
- Matys, J.; Grzech-Leśniak, K. Dental Aerosol as a Hazard Risk for Dental Workers. Materials 2020, 13, 5109. [Google Scholar] [CrossRef]
- Head Acoustics BHS II (Code 3322) Binaural Headset for Aurally Accurate Recording and (with SQobold). Available online: https://cdn.head-acoustics.com/fileadmin/data/en/Data-Sheets/AH-BR/BHS-II-Binaural-Headset-3322-Data-Sheet.pdf (accessed on 27 September 2023).
- Watanabe, J.; Iwamatsu-Kobayashi, Y.; Kikuchi, K.; Kajita, T.; Morishima, H.; Yamauchi, K.; Yashiro, W.; Nishimura, H.; Kanetaka, H.; Egusa, H. Visualization of droplets and aerosols in simulated dental treatments to clarify the effectiveness of oral suction devices. J. Prosthodont. Res. 2023. [Google Scholar] [CrossRef]
- Chavis, S.E.; Hines, S.E.; Dyalram, D.; Wilken, N.C.; Dalby, R.N. Can extraoral suction units minimize droplet spatter during a simulated dental procedure? J. Am. Dent. Assoc. 2021, 152, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Barrett, B.; McGovern, J.; Catanzaro, W.; Coble, S.; Redden, D.; Fouad, A.F. Clinical Efficacy of an Extraoral Dental Evacuation Device in Aerosol Elimination During Endodontic Access Preparation. J. Endodont. 2022, 48, 1468–1475. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health, Labour and Welfare. Guidelines for Preventing Hearing Impairment Due to Noise in Working Space; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2020. Available online: https://www.mhlw.go.jp/content/000628106.pdf (accessed on 27 September 2023). (In Japanese)
- National Institute for Occupational Safety and Health (NIOSH). Criteria for a Recommended Standard: Occupational Exposure to Noise; Revised Criteria; US Department of Health and Human Services: Washington, DC, USA, 1998.
- Al-Rawi, N.H.; Al Nuaimi, A.S.; Sadiqi, A.; Azaiah, E.; Ezzeddine, D.; Ghunaim, Q.; Abbas, Z. Occupational noise-induced hearing loss among dental professionals. Quintessence Int. 2019, 50, 245–250. [Google Scholar]
- Al-Omoush, S.A.; Abdul-Baqi, K.J.; Zuriekat, M.; Alsoleihat, F.; Elmanaseer, W.R.; Jamani, K.D. Assessment of occupational noise-related hearing impairment among dental health personnel. J. Occup. Health. 2020, 62, e12093. [Google Scholar] [CrossRef] [PubMed]
- Mohan, K.M.; Chopra, A.; Guddattu, V.; Singh, S.; Upasana, K. Should Dentists Mandatorily Wear Ear Protection Device to Prevent Occupational Noise-induced Hearing Loss? A Randomized Case-Control Study. J. Int. Soc. Prev. Community Dent. 2022, 12, 513–523. [Google Scholar] [PubMed]
- Henneberry, K.; Hilland, S.; Haslam, S.K. Are dental hygienists at risk for noise-induced hearing loss? A literature review. Can. J. Dent. Hyg. 2021, 55, 110–119. [Google Scholar]
- Myers, J.; John, A.B.; Kimball, S.; Fruits, T. Prevalence of tinnitus and noise-induced hearing loss in dentists. Noise Health 2016, 18, 347–354. [Google Scholar]
- Wilson, J.D.; Darby, M.L.; Tolle, S.L.; Sever, J.C., Jr. Effects of occupational ultrasonic noise exposure on hearing of dental hygienists: A pilot study. J. Dent. Hyg. 2002, 76, 262–269. [Google Scholar]
- Münzel, T.; Gori, T.; Babisch, W.; Basner, M. Cardiovascular effects of environmental noise exposure. Eur. Heart J. 2014, 35, 829–836. [Google Scholar] [CrossRef]


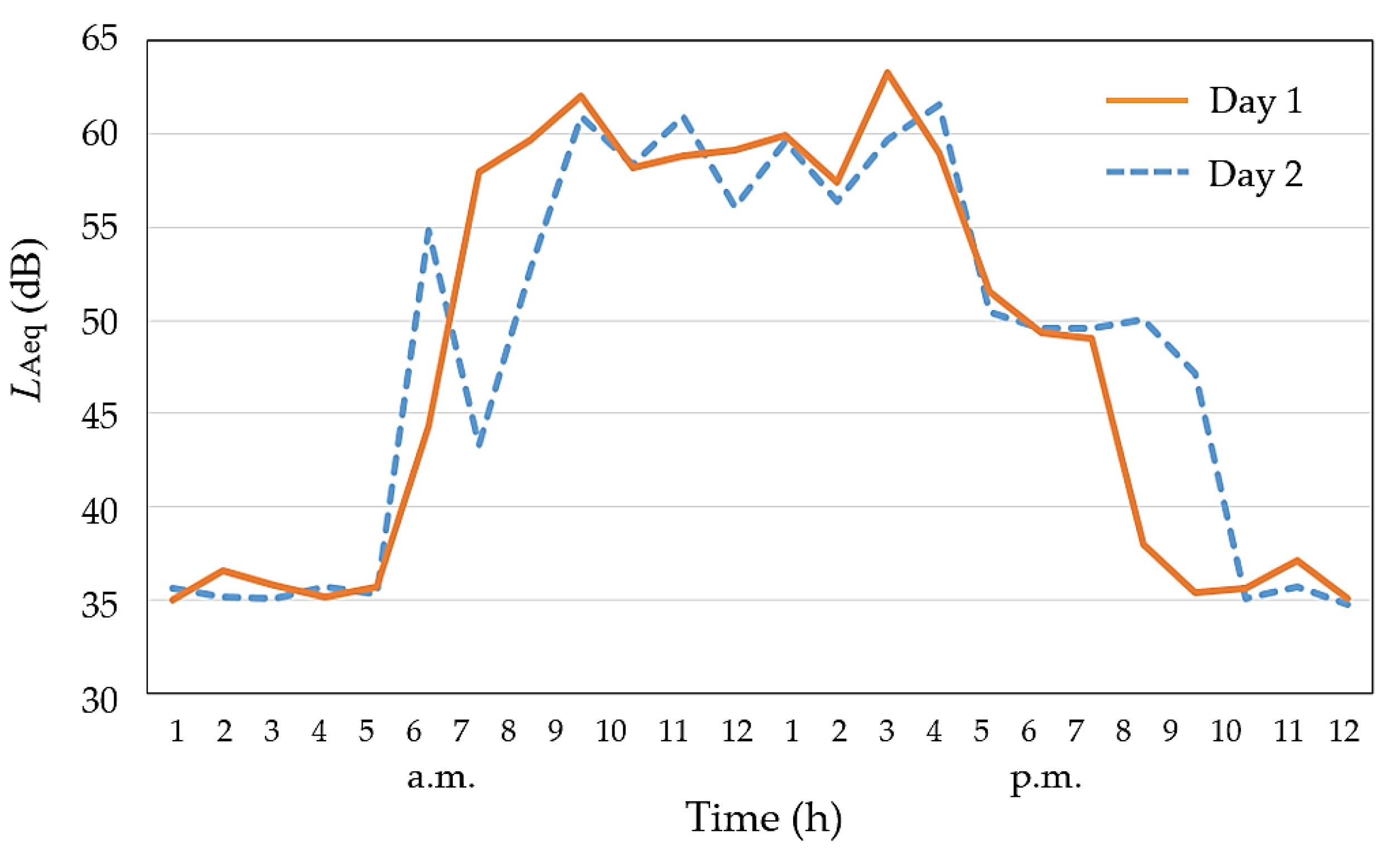
| Day 1 | Day 2 | Activity |
|---|---|---|
| 7 a.m. | 6 a.m. | Floor cleaning by cleaning staff |
| 8:30 a.m. | Opening of the clinic for patients Preparation for dental treatment | |
| 9 a.m. | Music broadcast start | |
| 9 a.m.–4 p.m. | Dental examination and treatment | |
| 4:30 p.m. | Music off/clean-up Maintenance of dental chairs and materials | |
| 5 p.m. | Training/discussion for students and dentists | |
| 7 p.m. | 8 p.m. | Close/automatic maintenance |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yamada, T.; Nozaki, K.; Hayashi, M.; Kuwano, S. Sound Environment during Dental Treatment in Relation to COVID-19 Pandemic. Acoustics 2023, 5, 987-998. https://doi.org/10.3390/acoustics5040056
Yamada T, Nozaki K, Hayashi M, Kuwano S. Sound Environment during Dental Treatment in Relation to COVID-19 Pandemic. Acoustics. 2023; 5(4):987-998. https://doi.org/10.3390/acoustics5040056
Chicago/Turabian StyleYamada, Tomomi, Kazunori Nozaki, Mikako Hayashi, and Sonoko Kuwano. 2023. "Sound Environment during Dental Treatment in Relation to COVID-19 Pandemic" Acoustics 5, no. 4: 987-998. https://doi.org/10.3390/acoustics5040056
APA StyleYamada, T., Nozaki, K., Hayashi, M., & Kuwano, S. (2023). Sound Environment during Dental Treatment in Relation to COVID-19 Pandemic. Acoustics, 5(4), 987-998. https://doi.org/10.3390/acoustics5040056






