Abstract
Background: A timely diagnostic colonoscopy (DC) after a positive FIT result is crucial for effective colorectal cancer (CRC) screening. In the Flemish CRC screening program (CRC-SP), 17% of FIT-positive participants had no DC in 2020. This study explores self-reported barriers, experiences, and perceptions about DC in FIT-positive participants. Methods: An online survey combining qualitative and quantitative approaches was sent by email to FIT-positive participants (November 2019–September 2020). Results: Out of 5134 invitees, 1597 respondents (31.1%) completed the survey. Among them, 77.5% had undergone/planned a DC, while 22.5% were unwilling to undergo a DC. DC perceptions, expectations, and experiences differed among groups; 57% of the ‘DC-performed’ group reported better-than-expected experiences. A substantial portion of the ‘DC-naïve’ group anticipated pain (42%) and embarrassment (30%), while the actual experience in the ‘DC-performed’ group was much lower (6.4% and 3.2%, respectively). GP advice, support from close contacts, and colonoscopy experiencers trigger DC planning, whereas lack of symptoms, false-positive perception, fears, and embarrassment were identified as barriers to DC. Conclusions: The study reveals barriers/facilitators for a DC in the Flemish CRC-SP. The findings inform targeted interventions for improved DC completion and its impact, including patient navigation and testimonial videos of ‘colonoscopy experiencers’ to address DC misperceptions.
1. Introduction
In Flanders, the population-based colorectal cancer screening program (CRC-SP), coordinated by the Centre for Cancer Detection (CCD), employs a centralized invitation process to send invitations, along with information leaflets and fecal immunochemical test (FIT), by mail to eligible individuals. Participation in the program is cost free for the target population, and individuals are re-invited every 24 months following their last screening or last invitation for non-participants [1]. Diagnostic colonoscopies (DC) (colonoscopies performed after a positive FIT result) are mainly covered by the Belgian healthcare system, with participants bearing approximately 13% (mean average of EUR 85) [2]. In 2021, the screening uptake was 52.5% [3], yielding a FIT positivity rate of 5.9%, which led to 26,931 participants being advised to undergo DC. Maintaining adequate compliance with DC following a positive FIT is crucial for reducing CRC incidence and mortality. Notably, in 2021, 17% (4578) did not proceed with DC after their positive FIT in Flanders (within 12 months after the positive FIT), and 11.3% (1422) received no follow-up at all (incomplete data) [3]. Although the DC completion of 83% in Flanders aligns with international averages of approximately 80% [4,5], it falls short of the EU guidelines’ acceptable rate of 90% [6].
A timely DC after a positive FIT is clinically important, as a delayed DC may contribute to the diagnosis of more advanced-stage CRC and an increase in CRC mortality risks [7,8]. Analysis of Flemish data from 2013 to 2017 reveals that CRCs identified in FIT-positive patients without a following DC within 12 months are notably more frequently diagnosed at stage III (19.7%) and stage IV (12.2%) compared to cases where FIT-positive patients underwent a DC within the same time frame (9.4% and 2.0%, respectively) [9]. In Flanders, the five-year relative survival rate for CRC between 2014 and 2018) is 74.9%, with stage I demonstrating a significantly higher survival rate of 97.6%, in contrast to the survival rate of 18.7% in stage IV [9]. Although the COVID-19 pandemic had minimal impact on uptake and screening intervals [10], it did influence FIT-positive participants’ willingness to undergo a DC, leading to extended time intervals between a positive FIT and DC [11]. In February and October 2021, the CCD conducted an online survey among FIT-positive participants in the Flemish CRC-SP who did not undergo a follow-up DC. This study aimed to examine the effects of the COVID-19 pandemic on FIT-positive individuals’ decision not to undergo a follow-up DC (results recently published) [11]. Furthermore, the study aimed to explore perceptions and experiences regarding DC after a positive FIT. This study presents the self-reported barriers, experiences, and perceptions surrounding DC after a positive FIT among participants in the Flemish CRC-SP. An in-depth understanding of the reasons behind the non-completion of (timely) DC after a positive FIT is crucial for maximizing DC adherence.
2. Results
2.1. Characteristics of Study Population and Survey Response Rate
A total of 1597 individuals, constituting 31.1% of the 5134 invitees, participated in the online survey, with 875 (17.5%) responding after receiving the reminder email. Table 1 presents the characteristics of the study population. Notably, a higher percentage of eligible screening individuals with an available email address (thus, receiving the online survey) was observed among younger individuals (85.6% in the 50–54 years group, in contrast to only 63.7% in the 70+ years group, p < 0.001), and among men (78.7%) relative to women (70.8%, p < 0.001). The response rate in men and women was quite similar (both around 31%). Among the five included age groups, the oldest group (70+ years) had the lowest response rate to the survey (only 23.4%).

Table 1.
Distribution of study population by sex and age (presented in absolute numbers and percentages).
Participants were classified into three groups based on their self-reported DC status: those who had already undergone a DC (72.4%), those who indicated having scheduled a DC appointment (5.1%), and those who had neither undergone nor planned a DC at the time of the survey (22.4%) (see Figure 1 below).
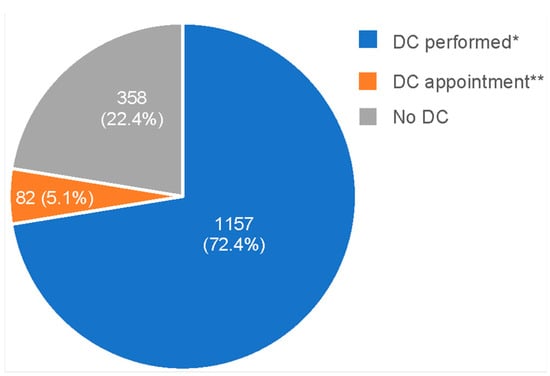
Figure 1.
Participants’ self-reported diagnostic colonoscopy (DC) status at the time of the survey, presented in absolute numbers and percentages. * DC performed: although a DC was not registered at the Centre for Cancer Detection when the survey was sent, participants indicated that they had already undergone a DC by the time they responded to the survey. ** No DC performed, but an appointment scheduled: participants reported having made an appointment for DC despite not yet undergoing the procedure. DC, diagnostic colonoscopy.
2.2. Survey Question Results
Table 2 shows the survey question results for all respondents about perceptions and experiences with DC after a FIT+ result. In the ‘no DC’ group, 21.5% had ever undergone a colonoscopy, compared with more than 35% in the ‘DC’ and ‘DC appointment’ groups. Almost 70% of respondents in the ‘no DC’ group indicated the positive result letter did not make them feel anxious, compared to more than 45% in the ‘DC’ and ‘DC appointment’ groups. Regarding communication with their GPs about the positive result letter, more than a quarter (26.8%) of the ‘no DC’ group did not have such discussions, compared to about 20% in the ‘DC’ and ‘DC appointment’ groups. In all three groups, the majority of the respondents took the initiative to talk with the GP about the matter.

Table 2.
Perceptions and experiences with DC after a FIT+ result: findings based on multiple choice questions (DC-performed, DC appointment, and no DC groups included). DC: diagnostic colonoscopy.
Only 3.9% in the ‘no DC’ groups estimated the risk of having CRC as high to very high, compared to about 13.5% in the ‘DC’ and ‘DC appointment’ groups. In the ‘DC’ group, more than 80% of respondents knew someone who had had a colonoscopy, compared to about 70% in the ‘no DC’ and ‘DC appointment’ groups. In the ‘no DC’ group, almost 20% indicated that the experiences of others influenced their decision whether to have a DC, compared to only 11.6% and 13.6% in the ‘DC’ and ‘DC appointment’ groups, respectively. Less than 40% in the ‘no DC’ group reported receiving advice from others to undergo a DC, compared to 47% and 49% in the ‘DC’ and ‘DC appointment’ group. Notably, in all three groups, it was mainly the GP or specialist who provided such advice.
In addition to multiple choice questions, this study explored perceptions and experiences (only in the ‘DC-performed’ and ‘no DC’ groups) based on fixed statements (Table 3), which were divided into six subthemes. In the ‘no DC’ group, only 55.6% agreed with the statement that their doctor wanted them to undergo a DC, and 55.3% agreed that it was important to undergo a DC after a positive FIT result based on their loved ones’ opinions (compared to over 90% in the DC group).

Table 3.
Perceptions and experiences about a DC: findings based on fixed statements (‘DC-performed’ and ‘no DC’ groups included). DC, diagnostic colonoscopy; CRC, colorectal cancer.
Regarding the different aspects of DC, bowel preparation was perceived as annoying by 53.5% in the ‘DC-performed’ group and 61.4% in the ‘no DC’ group. Less than 5% of the ‘DC-performed’ group reported discomfort with the DC itself annoying (compared to 57.6% in the ‘no DC’ group), the subsequent side effects (compared to 45.8% in the no DC group), or the sedation-induced side effects (compared to 38.8% in the no DC group). While 26.5% of the ‘DC-performed’ group expected the DC to be very painful (compared to 42% in the ‘no DC’ group), only 6.4% of the ‘DC-performed’ group indicated the DC was actually very painful.
In the ‘no DC’ group, fear of DC and DC results was explored through fixed statements: 45.2% agreed with the statement ‘I’m very anxious about having a colonoscopy’, and 34.1% with the statement ‘I’m afraid of possible complications that can occur during a colonoscopy’. While more than 30% of the ‘no DC’ group agreed with the statement ‘I would feel embarrassed during colonoscopy’, only 3.2% of the ‘DC-performed’ group actually felt embarrassed. More than one fifth (21.8%) of the ‘no DC’ group agreed that a colonoscopy affected their personal integrity.
Furthermore, in the ‘no DC’ group, several statements about the perception of false positive FIT and/or the belief that DC was not needed were questioned: 55.1% agreed with the statement ‘I have no complaints and thus believe a colonoscopy is not needed’, and about 40% agreed with the statement ‘I doubt whether the result of the stool test is correct’ and ‘If I had CRC I would have complaints’. One third agreed that ‘other medical issues had priority’, and 7% agreed with the statement ‘I believe the personal amount I need to pay for a colonoscopy is too high’ (Table 3).
A total of 308 persons had questions about the positive result letter. These open answers were categorized into 19 themes and later grouped into 4 subthemes and 1 rest-category (see Figure 2 below). About one third of the questions were related to the colonoscopy procedure itself, more than one fifth about the accuracy and reliability of the FIT, one fifth about the odds of having CRC, and almost one fifth about the causes of the positive FIT.
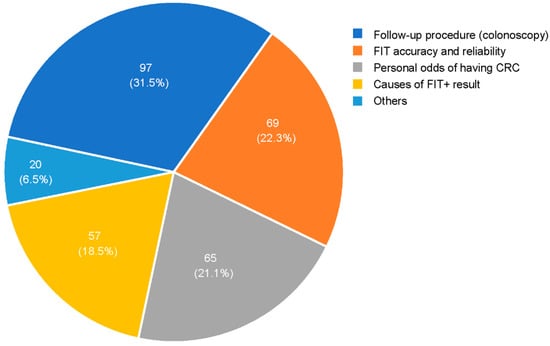
Figure 2.
Questions about the positive result letter (‘DC-performed’, ‘DC-appointment’, and no ‘DC groups’, n = 308). DC, diagnostic colonoscopy.
Table 4 presents the results of the survey questions about having had (‘DC-performed’ group) or planned (‘DC-appointment’ group) a DC after a positive FIT result. The open question ‘Why did you undergo or plan a DC after the FIT positive letter?’ was recoded into 17 categories, grouped into 3 subthemes and 1 ‘rest-category’. The main reason respondents cited for undergoing DC was the advice by the CCD itself (46.1%), often accompanied by advice from others (10.4%). For 30.6% of respondents, the first motivation for planning a DC was to be informed about the cause of the positive FIT. About 8% indicated an increased risk (e.g., symptoms or familial risk) as the main motivation to undergo a DC. More than half (57.2%) indicated the DC went better or much better than expected. The majority of respondents discussed the DC with someone (96.6%) and expressed willingness to undergo a DC again (99.1%) if needed.

Table 4.
Having or planning a DC after a FIT+ result: reasons, experiences, and future intention. DC, diagnostic colonoscopy; CCD, Centre for Cancer Detection; CRC, colorectal cancer.
In the ‘no DC’ group, insights were gathered from the open question ‘Why did you not plan a DC?’. The responses were coded into 9 subthemes and 1 ‘rest category’ (see Table 5 below). The primary reasons for not planning a DC (aside from the impact of the COVID-19 pandemic (see the related publication [11]), were ‘second stool test was negative’ (18.2%) and ‘perception of false positive FIT’ (17.9%). The majority of the respondents indicated themselves as the key decision-maker in choosing not to undergo a DC (71.5%). A small portion of 5.9% was discouraged by others from proceeding with a DC. Around one fifth of respondents opted for a second stool test by the GP instead of a DC.

Table 5.
Decision not to have a DC after a FIT+ result: reasons, decision-making process, and potential motivations (no DC group, n = 358).
Potential motivations/triggers for considering a DC were explored through self-reported answers (open questions) and fixed statements. Over 20% of respondents indicated that a second positive stool test result would convince them to do a DC. Additionally, 14% expressed their willingness to undergo a DC if insisted by a doctor, while 7.5% answered that nothing would persuade them to plan a DC after the positive FIT. Based on the fixed statement, potential triggers to plan a DC were the advice of a GP (72.1%), the availability of an appointment included in the positive result letter (39.7%), the inclusion of a leaflet containing additional information about the DC along with the positive result letter (38.5%), and an educational video about DC on the website (37.4%). For all the other statements, more than 25% either partially or completely agreed with the indicated triggers to plan a DC.
3. Discussion
In Flanders, approximately 83% of FIT-positive participants completed a DC (<1 year after the FIT+), which is in line with findings from international studies [4,5]. The absence of (timely) DC after a positive FIT isconcerning due to the associated heightened risk of CRC, a greater probability of advanced-stage disease at the time of diagnosis, and an elevated mortality rate associated with CRC [7,8,12]. Therefore, understanding the reasons behind the lack of follow-up and developing strategies to mitigate this issue is crucial [13,14]. An overview of perceptions and expectations concerning DC is needed to maximize DC completion rates among FIT-positive individuals. Previous Flemish research on FIT-positive individuals (limited to those without a DC) revealed the main barriers to DC, including the belief that the FIT result was a false positive one, lack of symptoms, competing medical priorities, fear of a colonoscopy, and GP advice not to plan a DC [9].
The current study delved deeper into the perceptions and expectations surrounding DC within both the ‘no DC’ and the ‘DC’ groups. The online survey engaged a total of 1597 FIT-positive participants from the Flemish CRC-SP, covering three categories: 73% had had a DC performed, 5% had scheduled a DC appointment, and 22% had no DC performed or planned at the time they responded to the survey. The lack of symptoms and the belief that the FIT result was a false positive once again emerged as barriers to DC planning, in alignment with previous research [9,11,15,16,17]. These findings underline a critical misunderstanding of the purpose of screening. As highlighted by Amlani (2020), over half of the colonoscopy-naïve respondents were unaware of the preventive nature of colonoscopies [16]. One third of the respondents agreed that other medical issues took priority, consistent with the existing literature [11,14,15].
Almost half of the ‘no DC’ group agreed with the statement that colonoscopy made them feel very anxious and more than one-third stated being afraid of possible complications during a DC. Fear of pain, discomfort, and potential complications during DC have been documented in prior studies [14,15,17,18,19,20]. Individuals undergoing CRC screening experience elevated levels of anxiety due to screening participation, especially those who undergo colonoscopy as a follow-up diagnostic procedure subsequent to a positive FIT outcome, as opposed to using it as the primary screening method [21,22]. Bynum et al. [23] found that fear and lack of trust in medical procedures influenced individuals’ readiness to participate in CRC screening. One third of the ‘no DC’ group expressed discomfort about potential embarrassment during a DC, a concern that has also been highlighted in previous studies [17,24].
This study demonstrates that individuals who have already undergone a DC generally find the experience much less unpleasant, compared to the colonoscopy-naïve group. Among the different aspects of DC, participants mainly perceived bowel preparation as bothersome. This aligns with findings from Issaka et al. (2021), who associated lower DC completion rates with bowel preparation (survey among primary care providers—PCPs) [20]. Vemulapalli et al. (2023), in a study involving colonoscopy experiences, also emphasized that bowel preparation was considered the least favorable aspect of colonoscopy, and was a significant deterrent to a future colonoscopy [25]. Similarly, Amlani et al. (2020) found that respondents with colonoscopy experience exhibited a greater aversion to bowel preparation compared to those who were colonoscopy naïve (47% vs. 26%) [16]. A systematic review by Decruz (2021) further supported that the bowel preparation, including the use of laxatives, was regarded as ‘repulsive’ and ‘abusive’ even, compared to the actual colonoscopy procedure, which was viewed as relatively straightforward [24].
Our study demonstrates remarkable differences in perceptions about a DC between the ‘DC-performed’ group and the ‘no DC’ group in Flanders. Less than 5% of the ‘DC-performed’ group perceived the DC itself as annoying, in contrast to almost 60% in the ‘no DC’ group. Additionally, only a minority within the ‘DC-performed’ group indicated significant pain during the DC, while over 40% of the ‘no DC’ group anticipated experiencing substantial pain during the procedure. More than 30% of the ‘no DC’ group expressed concerns about potential embarrassment during a DC, and more than one fifth (22%) of the ‘no DC’ group believed that undergoing a DC would impact their personal integrity. In contrast, only 3.2% of the ‘’DC-performed’ group reported feeling embarrassed. In fact, individuals without prior experience with colonoscopy often overestimate the likelihood of experiencing pain during the procedure, overemphasize its negative aspects, and underestimate the challenges of bowel preparation [16]. This perspective was supported by Flugelman (2019), who suggested that the discomfort linked to bowel preparation may be underestimated by colonoscopy-naïve respondents [26]. A significant proportion of the ‘no DC’ group (45%) also exhibited anxiety about undergoing a DC. Over half of the ‘DC-performed’ group reported that their DC experience went better than expected, and an overwhelming 99% expressed willingness to undergo a DC again if needed, which is in line with the literature that suggests previous colonoscopy experience encourages repeat participation [19].
Perceived susceptibility, a fundamental construct within the Health Belief Model as outlined by Hochbaum, Rosenstock, & Kegels in 1952/2016 [27], is characterized by the belief that an individual is susceptible to contracting a disease and this belief significantly shapes their screening behavior. The ‘no DC’ group estimated a significantly lower risk of having CRC compared to both the ‘DC-performed’ and ‘DC appointment’ groups. More than half of the ‘DC-performed’ or ‘DC appointment’ group individuals indicated that the positive result letter made them feel anxious, in contrast to only one third in the ‘no DC’ group. This highlights the link between individuals’ assessment of their susceptibility to CRC and the perceived severity of the disease with their likelihood of opting for a colonoscopy [18,19].
The recommendation from the CCD to undergo a DC in the positive result letter and the (supplementary) advice from GPs emerged as the main triggers for planning a DC. Approximately half of the ‘DC-performed’ and ‘DC appointment’ groups received advice from others (mainly GPs) to plan a DC, while this was less than 40% in the ‘no DC’ group. The advice from a GP emerged as a motivating factor to plan a DC. While a substantial majority (over 90%) of the ‘DC-performed’ group agreed with the statement that their doctor advocated for a DC and that their loved ones believed a DC was important, only around half of the ‘no DC’ group shared these viewpoints.
External influences, particularly the experiences of others, appeared to shape DC’s planning decision. The ‘no DC’ group had significantly fewer acquaintances who had undergone a colonoscopy, and when they did, these experiences tended to be more negative. The impact of negative experiences from others appeared to be more pronounced in the ‘no DC’ group. One fifth of the ‘no DC’ group participants indicated that the experiences of others played a role in their decision to consider a DC. The majority (96.6%) of the ‘DC-performed’ group engaged in post-DC discussions with others. The support, encouragement, and companionship of family members emerged as crucial factors motivating individuals to undergo a DC [28]. This is confirmed by the findings from the EU survey by Amlani et al. (2020), which indicated that talking with individuals who have previously undergone a colonoscopy was an important trigger. The interaction with colonoscopy experiencers often eliminates the misconception of excessive pain during the procedure. Instead, colonoscopy-experienced respondents often indicated that the process was less intimidating than anticipated [16]. These results suggest that testimonials from those with DC experience can have a positive impact on motivating potential DC candidates. In the fixed statements, participants from the ‘no DC’ group also expressed the desire to have a conversation with someone who has already undergone a DC, potentially providing them with a sense of reassurance.
An additional leaflet offering more information and an educational video about DC on the screening program’s website were identified through fixed statements as potential triggers for motivating DC planning. Patient navigation emerged as a promising strategy to enhance DC completion [29,30]. Navigated patients showed a 1.5 times higher likelihood of completing screening colonoscopy compared to those receiving standard care [30]. To mitigate potential fears and anxieties, it is recommended to create a comprehensive video that covers details about bowel preparation, the colonoscopy procedure, and post-procedural care, supplemented by guidance that encourages individuals to plan for a DC [28]. The utilization of instructional aids and graphics (e.g., a preparatory video [31]) has shown effectiveness in decreasing pre-procedure anxiety. Parker [32] demonstrated the success of a web-based multimedia patient navigation tool in reducing patient anxiety and increasing knowledge regarding colonoscopy. Additionally, establishing easily accessible helplines for patients with uncertainties about a DC could be beneficial in addressing misconceptions prior to DC planning [24].
Previous research in Flanders has emphasized the important role of GPs in advocating for CRC screening and promoting adherence to screening recommendations [9,11]. Within the current study, a quarter of respondents did not undergo a DC due to the belief that ‘it was not necessary according to their GP’ and a DC would be planned only if a second stool test was also positive. The advice of a GP has been reported as an important trigger for DC planning [15,16,17,33], while the inability to discuss the necessity of a DC with a healthcare provider has posed a significant obstacle [17]. An EU survey demonstrated that over 70% of individuals without prior colonoscopy experience expressed willingness to undergo the procedure if recommended by their GP [16]. Furthermore, healthcare providers might underestimate the probability that a positive FIT result indicates the presence of CRC or advanced adenoma (AA), leading to a diminished sense of urgency for DC planning [18]. Similar underestimations of AA and CRC probabilities after a positive FIT result were noted among GPs in a Dutch study. Upon being informed of the actual probabilities, some GPs acknowledged the potential for this knowledge to reshape their approach towards communicating with patients [18].
Decisions surrounding DC completion were occasionally the outcome of negotiations between FIT-positive individuals and their GPs. Despite receiving initial recommendations from PCPs to undergo a DC, a subset of patients was determined to stick to their decision, either believing the positive FIT result was a false positive or feeling afraid of the DC procedure. These FIT-positive patients frequently negotiated alternative follow-up measures, including repeating the FIT [15]. In certain cases, GPs could potentially have offered more extensive counseling to the FIT-positive individuals. The decision not to plan a DC might also be attributed to PCPs’ lack of knowledge of the relevant guidelines [34]. While the implementation of a failsafe mechanism is crucial, the knowledge of the guidelines remains critical to ensure satisfactory DC completion rates. Screening programs could optimize follow-up procedures by limiting the utilization of repeat FITs [15]. Once again, this study underscores the potential influence of GPs on guiding appropriate follow-up after a positive FIT result in the CRC-SP. An online survey was conducted in March 2023 among GPs to explore the potential motivations of GPs and patients for not opting for a DC.
This study has certain limitations. Firstly, the online survey was restricted to individuals with a valid email address registered in the database of the CCD, potentially resulting in the underrepresentation of older age groups and those with a non-Belgian nationality at birth (due to a lower provision of email addresses). Men appeared to be overrepresented in the survey. This skewed representation can be attributed to the significantly higher FIT positivity rate and lower DC compliance among men in Flanders [1,3], which led to a higher proportion of men in this study. Respondents with a lower education level were significantly more prevalent in the ‘no DC’ group. Secondly, there is a possibility of selection bias influencing the willingness to respond to the online survey, as individuals who participated might have been more driven to express their motivations (or lack thereof) to plan a DC. Interestingly, a portion of individuals in the ‘no DC’ category conveyed their intentions to schedule a DC post-COVID-19 pandemic. Nevertheless, due to the anonymity of the survey, we were unable to verify whether those who intended to undergo a DC actually followed through. Thus, it is noteworthy that some of the respondents’ answers might be influenced by socially desirable responses.
To our knowledge, this is the first study to explore beliefs and perceived barriers regarding DC after a positive FIT result among different groups within the screening population in Flanders. This study reveals substantial differences in DC perceptions between the ‘DC-performed/planned’ and ‘no DC’ groups. While previous work by Decruz (2021) has delved into the perceptions of unscreened populations and medical personnel, there remains a need for research that gathers insights from the screened individuals who have directly experienced colonoscopy. Such firsthand perspectives are crucial for providing accurate and practical information about the procedure and addressing any negative connotations, contributing to an improved understanding of the factors influencing colonoscopy experiences [24]. Qualitative studies on DC barriers and perceptions are currently scarce [15], and little has been known about DC perceptions within the Flemish CRC-SP. Additionally, significant discrepancies in the perception of barriers to colonoscopy exist between PCPs and the general population. The only barrier that PCPs agreed on was the absence of a physician’s recommendation [35]. Moreover, the considerable variations in colonoscopy perceptions among EU countries and regions highlight the need for regional studies, such as this one, to inform localized policy recommendations [16].
To facilitate timely DC after a positive FIT, multiple interventions are needed. CRC-SPs incorporating patient navigators and provider reminders report higher rates of DC completion [5]. In Flanders, a comprehensive approach has been developed, which involves patient-level interventions (e.g., notifying patients of test results and fail-safe mechanism), provider-level strategies (e.g., notifying GPs of test results and fail-safe mechanism, along with providing a yearly overview of patients without DC), and system-level measures (e.g., establishing a registry to track FIT-positive patients). Since March 2019, a fail-safe mechanism has been implemented, where a reminder recommendation for DC is issued to participants and GPs 24 months after a positive FIT if a DC (or virtual colonoscopy) has not occurred. Sending the reminder letter shortly after a positive FIT outcome is not feasible because of administrative delays in registering colonoscopies (attributed to the lack of a centralized colonoscopy register). Starting in 2022, GPs receive an annual report comparing the DC rate in their practice with regional and Flemish averages, with a list of patients lacking (correct) follow-up, allowing GPs to motivate patients if necessary.
Additional interventions are needed to ensure that participants with positive FIT results are thoroughly informed about DC, thereby alleviating fears, reducing anxiety, and addressing DC myths and misperceptions. The CCD plans to develop a patient education leaflet aimed at rectifying misperceptions about DC (including information about perceived pain, discomfort, and sedation) and emphasizing the importance of the procedure. In Flanders, it is imperative that FIT-positive patients receive comprehensive information about DC to reduce fear and anxiety and address misconceptions to improve DC uptake. Leveraging the experiences of individuals who have already undergone a DC could serve to ‘reassure’ DC-naïve patients. The importance of early CRC detection, especially among asymptomatic individuals, is consistently emphasized in the informational materials and the leaflet accompanying the invitation letter. This study suggests incorporating this information into the positive result letter, along with featuring it in a testimonial (through a video on the screening program’s website accessible via a QR code within the positive result letter).
Although a limited number of respondents agreed that a pre-scheduled appointment for DC in the positive FIT letter might prompt action, it is worth noting that this singular approach has not successfully resolved the non-completion rate of 11–14% for DC in the Dutch CRC-SP [18]. Furthermore, due to the lack of a centralized colonoscopy register and the authorization of all gastroenterologists to perform a DC in the Flemish CRC-SP, implementing such a strategy is challenging. After all, a colonoscopy remains the gold standard after a positive FIT. The quest for a more acceptable and well-tolerated bowel preparation still represents an unmet need within the field of colonoscopy [25]. It is possible that non-DC compliers might be willing to undergo a CTC. Despite its limited use in Flanders, possibly due to low public awareness, CTC holds potential as an alternative to DC, with fewer barriers to overcome.
4. Material and Methods
Study Design—Online Survey
The current cross-sectional study integrates both a qualitative component, involving categorized open-ended questions, and a quantitative component, involving fixed statements and closed questions within an online survey. The survey was disseminated via email to the Flemish CRC-SP participants who received a positive FIT result between 1 November 2019 and 30 September 2020, and had not undergone a follow-up DC by the time of the survey, conducted on 12 February 2021 and 19 October 2021, respectively. A reminder mailing was sent to the entire study population four weeks after the first mailing, maintaining our anonymous approach. The survey was developed based on insights from prior research and the existing literature, and it was piloted before implementation among the eligible population. Candidate selection was based on the administrative databases of the CCD. The online survey was sent to individuals in the eligible population who had filled in the participation form with a valid email address (accompanying the stool sample) during their participation in the CRC-SP.
The online survey had two primary objectives: (1) to examine the potential effects of the COVID-19 pandemic on DC (results recently published) [11] and (2) to explore the barriers, perceptions, and experiences of a DC after a positive FIT (the current study). Inform consent is indicated by respondents’ completion of the online survey. Ethical approval was not required. Throughout this study, the anonymity of the survey respondents was rigorously maintained. No incentives were given for participation. IBM SPSS statistics software (version 27.0 for Windows) was used for the analyses of the collected survey data. Possible statistically significant associations were investigated with the Chi-square test (p-values < 0.05). Analysis of responses to the open-ended survey questions involved open coding, followed by recategorization. Categories with fewer than 20 answers were omitted from the analyses.
5. Conclusions
In the online survey, over 77.5% of respondents either underwent or scheduled a DC after a positive FIT result, while 22.5% were not willing to proceed with a DC. The main reasons behind this reluctance included a lack of symptoms, concerns about false positives, and feelings of fear and embarrassment. Potential triggers for DC included GPs’ advice, support from close contacts, additional leaflets, and educational videos about DC. Notably, perceptions of DC differ significantly between ‘DC-experienced’ and ‘no DC’ groups within the Flemish population. The ‘DC-experienced’ group found the procedure much less unpleasant than anticipated. For the Flemish CRC-SP to reach its full potential impact, ensuring all FIT positives are followed by a DC is imperative. The CCD has already implemented targeted actions to increase DC compliance in FIT-positive participants, but further strategies such as patient navigation and/or testimonial videos of ‘colonoscopy experiencers’ could be useful in addressing misperceptions about DC and enhancing DC adherence.
Author Contributions
Conceptualization, S.H.; writing—original draft preparation, S.H.; writing—review and editing, S.H. and T.N.T.; statistical analysis, S.H.; visualization, S.H. and T.N.T.; supervision, S.H. All authors have read and agreed to the published version of the manuscript.
Funding
The Flemish CRC-SP is funded exclusively by the Agency for Care and Health, part of the Flemish Ministry of Welfare, Public Health and Family (https://www.vlaanderen.be/en, accessed on 28 September 2023). The Flemish Ministry was not involved in any phase of this study (design, data collection, analysis, interpretation, and writing the manuscript).
Institutional Review Board Statement
The secondary use and linkage of the databases involved were approved on 17 September 2013 (updated on 20 March 2018), with reference number 13/091, and on 6 July 2021, with reference number 21/118, by the Information Security Committee (formerly the Committee for the Protection of Privacy). Approval of an ethical committee was not necessary given the fact that this retrospective study does not fall under the Belgian legislation for ethical committee approval (Law of 7 May 2004 regarding experiments on human persons (art. 3, Section 2)). Only pseudonymised data were used for this study, and results are reported in an aggregated way. The study protocol conforms to the principles of the 1964 Helsinki Declaration and its later amendments and to the applicable national guidelines.
Informed Consent Statement
When participating in the Flemish CRC-SP, all participants filled out a written informed consent explaining that personal information can be used for scientific research and evaluation to improve the CRC-SP.
Data Availability Statement
Data on screening uptake, gender, and age-specific proportions of the target screening population can be requested by contacting the Centre for Cancer Detection in Flanders at https://www.bevolkingsonderzoek.be. Data on DC compliance, gender, and age-specific proportions of DC compliance can be requested by contacting the Belgian Cancer Registry (BCR) at https://kankerregister.org/ (accessed both links on 28 September 2023).
Acknowledgments
We acknowledge the Flemish Colorectal Cancer Screening Task Force for functioning as a sounding board.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Hoeck, S.; van de Veerdonk, W.; De Brabander, I. Do socioeconomic factors play a role in nonadherence to follow-up colonoscopy after a positive faecal immunochemical test in the Flemish colorectal cancer screening programme? Eur. J. Cancer Prev. 2020, 29, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Meeus, A.; Demyttenaere, B. Study Colonoscopy [Studie Colonoscopie]; Nationaal Verbond van Socialistische Mutualiteiten: Brussel, Belgium, 2020. [Google Scholar]
- Centre for Cancer Detection & Belgian Cancer Registry. Monitoring Report of the Flemish Colorectal Cancer Screening Programme. 2021. Available online: https://dikkedarmkanker.bevolkingsonderzoek.be/sites/default/files/2022-03/Jaarrapport%202021%20BVO%20naar%20kanker_0.pdf (accessed on 23 May 2023).
- Gingold-Belfer, R.; Leibovitzh, H.; Boltin, D.; Issa, N.; Tsadok Perets, T.; Dickman, R.; Niv, Y. The compliance rate for the second diagnostic evaluation after a positive fecal occult blood test: A systematic review and meta-analysis. United Eur. Gastroenterol. J. 2019, 7, 424–448. [Google Scholar] [CrossRef] [PubMed]
- Selby, K.; Senore, C.; Wong, M.; May, F.P.; Gupta, S.; Liang, P.S. Interventions to ensure follow-up of positive fecal immunochemical tests: An international survey of screening programs. J. Med. Screen. 2021, 28, 51–53. [Google Scholar] [CrossRef]
- Segnan, N.; Patnick, J.; von Karsa, L. (Eds.) European Guidelines for Quality Assurance in Colorectal Cancer Screening and Diagnosis, 1st ed.; Publications Office of the European Union: Luxembourg, 2010. [Google Scholar]
- Corley, D.A.; Jensen, C.D.; Quinn, V.P.; Doubeni, C.A.; Zauber, A.G.; Lee, J.K.; Schottinger, J.E.; Marks, A.R.; Zhao, W.K.; Ghai, N.R.; et al. Association Between Time to Colonoscopy After a Positive Fecal Test Result and Risk of Colorectal Cancer and Cancer Stage at Diagnosis. JAMA 2017, 317, 1631–1641. [Google Scholar] [CrossRef] [PubMed]
- Zorzi, M.; Battagello, J.; Selby, K.; Capodaglio, G.; Baracco, S.; Rizzato, S.; Chinellato, E.; Guzzinati, S.; Rugge, M. Non-compliance with colonoscopy after a positive faecal immunochemical test doubles the risk of dying from colorectal cancer. Gut 2022, 71, 561–567. [Google Scholar] [CrossRef]
- Hoeck, S.; De Schutter, H.; Van Hal, G. Why do participants in the Flemish colorectal cancer screening program not undergo a diagnostic colonoscopy after a positive fecal immunochemical test? Acta Clin. Belg. 2022, 77, 760–766. [Google Scholar] [CrossRef]
- Jidkova, S.; Hoeck, S.; Kellen, E.; le Cessie, S.; Goossens, M.C. Flemish population-based cancer screening programs: Impact of COVID-19 related shutdown on short-term key performance indicators. BMC Cancer 2022, 22, 183. [Google Scholar] [CrossRef]
- Hoeck, S.; Janssens, S.; Van Hal, G.; Van Herck, K. Self-Reported and Objective Impact of the COVID-19 Pandemic on Planning, Compliance and Timeliness of a Diagnostic Colonoscopy after a Positive FIT Screening Result in the Flemish Colorectal Cancer Screening Program. Gastrointest. Disord. 2022, 4, 129–140. [Google Scholar] [CrossRef]
- Mutneja, H.R.; Bhurwal, A.; Arora, S.; Vohra, I.; Attar, B.M. A delay in colonoscopy after positive fecal tests leads to higher incidence of colorectal cancer: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2021, 36, 1479–1486. [Google Scholar] [CrossRef]
- Dalton, A.R.H. Incomplete diagnostic follow-up after a positive colorectal cancer screening test: A systematic review. J. Public Health 2018, 40, e46–e58. [Google Scholar] [CrossRef]
- Kerrison, R.S.; Travis, E.; Dobson, C.; Whitaker, K.L.; Rees, C.J.; Duffy, S.W.; von Wagner, C. Barriers and facilitators to colonoscopy following fecal immunochemical test screening for colorectal cancer: A key informant interview study. Patient Educ. Couns. 2022, 105, 1652–1662. [Google Scholar] [CrossRef] [PubMed]
- Llovet, D.; Serenity, M.; Conn, L.G.; Bravo, C.A.; McCurdy, B.R.; Dube, C.; Baxter, N.N.; Paszat, L.; Rabeneck, L.; Peters, A.; et al. Reasons For Lack of Follow-up Colonoscopy Among Persons With A Positive Fecal Occult Blood Test Result: A Qualitative Study. Am. J. Gastroenterol. 2018, 113, 1872–1880. [Google Scholar] [CrossRef] [PubMed]
- Amlani, B.; Radaelli, F.; Bhandari, P. A survey on colonoscopy shows poor understanding of its protective value and widespread misconceptions across Europe. PLoS ONE 2020, 15, e0233490. [Google Scholar] [CrossRef] [PubMed]
- Mog, A.C.; Liang, P.S.; Donovan, L.M.; Sayre, G.G.; Shaukat, A.; May, F.P.; Glorioso, T.J.; Jorgenson, M.A.; Wood, G.B.; Mueller, C.; et al. Timely Colonoscopy After Positive Fecal Immunochemical Tests in the Veterans Health Administration: A Qualitative Assessment of Current Practice and Perceived Barriers. Clin. Transl. Gastroenterol. 2022, 13, e00438. [Google Scholar] [CrossRef] [PubMed]
- Bertels, L.; Lucassen, P.; van Asselt, K.; Dekker, E.; van Weert, H.; Knottnerus, B. Motives for non-adherence to colonoscopy advice after a positive colorectal cancer screening test result: A qualitative study. Scand. J. Prim. Health Care 2020, 38, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Olchowska-Kotala, A.; Bajcar, B. Predictors of Undergoing Colonoscopy, Does Time Horizon Matter? J. Prim. Prev. 2020, 41, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Issaka, R.B.; Bell-Brown, A.; Snyder, C.; Atkins, D.L.; Chew, L.; Weiner, B.J.; Strate, L.; Inadomi, J.M.; Ramsey, S.D. Perceptions on Barriers and Facilitators to Colonoscopy Completion After Abnormal Fecal Immunochemical Test Results in a Safety Net System. JAMA Netw. Open 2021, 4, e2120159. [Google Scholar] [CrossRef]
- Bobridge, A.; Bampton, P.; Cole, S.; Lewis, H.; Young, G. The psychological impact of participating in colorectal cancer screening by faecal immuno-chemical testing—The Australian experience. Br. J. Cancer 2014, 111, 970–975. [Google Scholar] [CrossRef]
- Kapidzic, A.; Korfage, I.J.; van Dam, L.; van Roon, A.H.; Reijerink, J.C.; Zauber, A.G.; van Ballegooijen, M.; Kuipers, E.J.; van Leerdam, M.E. Quality of life in participants of a CRC screening program. Br. J. Cancer 2012, 107, 1295–1301. [Google Scholar] [CrossRef]
- Bynum, S.A.; Davis, J.L.; Green, B.L.; Katz, R.V. Unwillingness to participate in colorectal cancer screening: Examining fears, attitudes, and medical mistrust in an ethnically diverse sample of adults 50 years and older. Am. J. Health Promot. 2012, 26, 295–300. [Google Scholar] [CrossRef]
- Decruz, G.M.; Ng, C.H.; Lim, K.T.; Devi, M.K.; Lim, F.; Tai, C.H.; Chong, C.S. Afterthoughts on colonoscopy. Was it that bad? J. Med. Screen. 2021, 28, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Vemulapalli, K.C.; Lahr, R.E.; Rex, D.K. 2021 Patient Perceptions Regarding Colonoscopy Experience. J. Clin. Gastroenterol. 2023, 57, 400–403. [Google Scholar] [CrossRef] [PubMed]
- Flugelman, A.A.; Stein, N.; Segol, O.; Lavi, I.; Keinan-Boker, L. Delayed Colonoscopy Following a Positive Fecal Test Result and Cancer Mortality. JNCI Cancer Spectr. 2019, 3, pkz024. [Google Scholar] [CrossRef] [PubMed]
- Hochbaum, G.; Rosenstock, I.; Kegels, S. Health Belief Model; Public Health Service: Washington, DC, USA, 2016. (Original Work Published 1952). [Google Scholar]
- Cheng, S.Y.; Li, M.C.; Chia, S.L.; Huang, K.C.; Chiu, T.Y.; Chan, D.C.; Chiu, H.M. Factors affecting compliance with confirmatory colonoscopy after a positive fecal immunochemical test in a national colorectal screening program. Cancer 2018, 124, 907–915. [Google Scholar] [CrossRef] [PubMed]
- Selby, K.; Baumgartner, C.; Levin, T.R.; Doubeni, C.A.; Zauber, A.G.; Schottinger, J.; Jensen, C.D.; Lee, J.K.; Corley, D.A. Interventions to Improve Follow-up of Positive Results on Fecal Blood Tests: A Systematic Review. Ann. Intern. Med. 2017, 167, 565–575. [Google Scholar] [CrossRef]
- DeGroff, A.; Schroy, P.C., 3rd; Morrissey, K.G.; Slotman, B.; Rohan, E.A.; Bethel, J.; Murillo, J.; Ren, W.; Niwa, S.; Leadbetter, S.; et al. Patient Navigation for Colonoscopy Completion: Results of an RCT. Am. J. Prev. Med. 2017, 53, 363–372. [Google Scholar] [CrossRef]
- Silvester, J.A.; Kalkat, H.; Graff, L.A.; Walker, J.R.; Singh, H.; Duerksen, D.R. Information seeking and anxiety among colonoscopy-naive adults: Direct-to-colonoscopy vs traditional consult-first pathways. World J. Gastrointest. Endosc. 2016, 8, 701–708. [Google Scholar] [CrossRef]
- Parker, S.; Zipursky, J.; Ma, H.; Baumblatt, G.L.; Siegel, C.A. A Web-based Multimedia Program Before Colonoscopy Increased Knowledge and Decreased Anxiety, Sedation Requirement, and Procedure Time. J. Clin. Gastroenterol. 2018, 52, 519–523. [Google Scholar] [CrossRef]
- Bertels, L.; van der Heijden, S.; Hoogsteyns, M.; Dekker, E.; van Asselt, K.; van Weert, H.; Knottnerus, B. GPs’ perspectives on colorectal cancer screening and their potential influence on FIT-positive patients: An exploratory qualitative study from a Dutch context. BJGP Open 2019, 3, bjgpopen18X101631. [Google Scholar] [CrossRef]
- Correia, A.; Rabeneck, L.; Baxter, N.N.; Paszat, L.F.; Sutradhar, R.; Yun, L.; Tinmouth, J. Lack of follow-up colonoscopy after positive FOBT in an organized colorectal cancer screening program is associated with modifiable health care practices. Prev. Med. 2015, 76, 115–122. [Google Scholar] [CrossRef]
- Mastrokostas, A.; Gavana, M.; Gkrizioti, M.; Smyrnakis, E.; Cholongitas, E.; Benos, A.; Haidich, A.-B. Discrepancies and misconceptions of perceived colorectal cancer screening barriers between primary health professionals and unscreened population. A comparative study in Greece. J. BUON 2018, 23, 67–76. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).