Exploring Polymeric Surfaces Manufactured Under Different Temperature Conditions—A Preliminary Experimental Study of Hardness
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Preparation and Experimental Conditions
2.2. Hardness Measurement
2.3. Statistical Analysis
3. Results
3.1. Surface Hardness Analysis
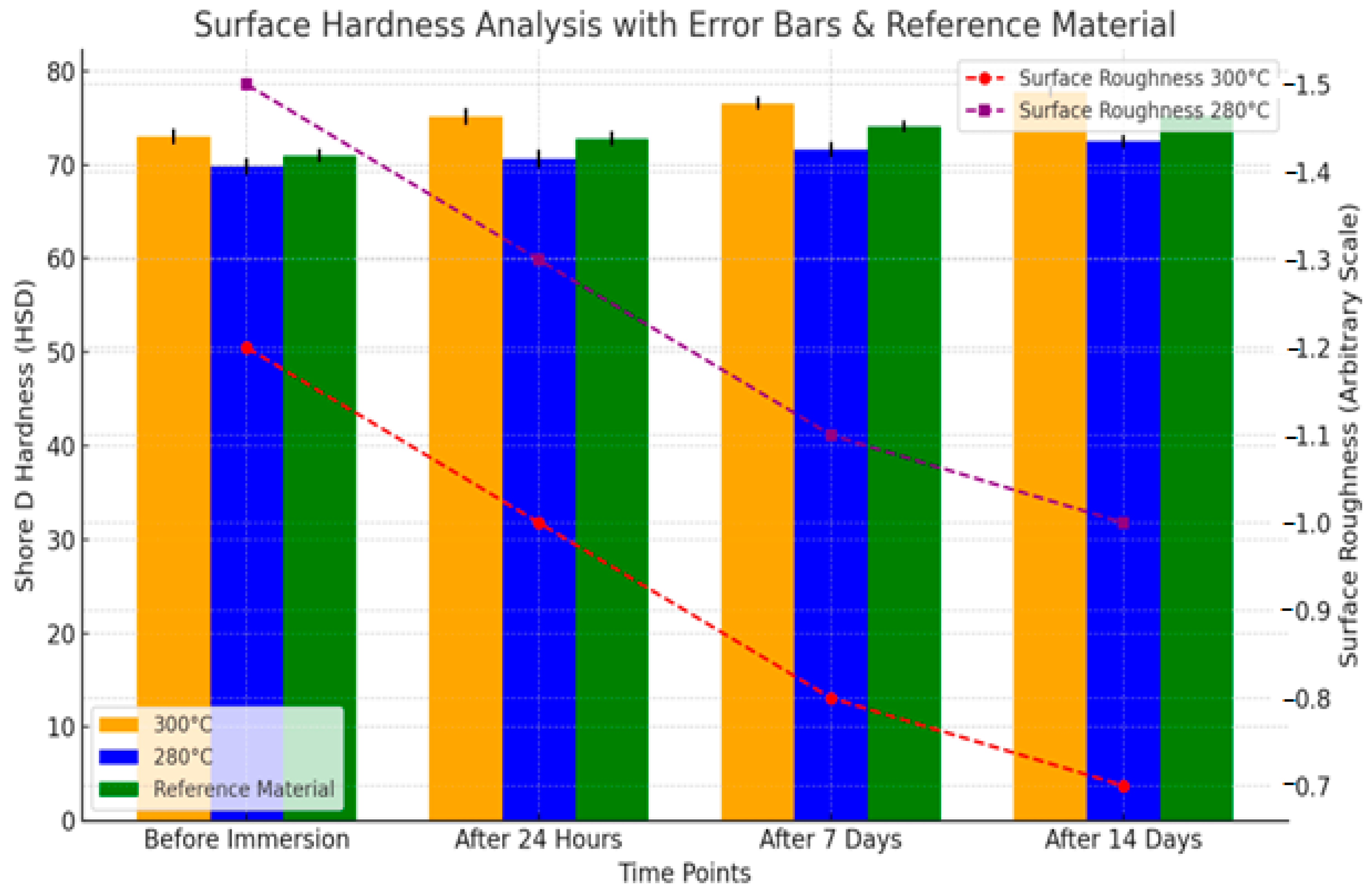
- Samples processed at 300 °C exhibited smoother surfaces over time compared to those manufactured at 280 °C.
- The increase in hardness with higher manufacturing temperatures suggests improved wear resistance.
- Hardness at 300 °C
- Hardness at 280 °C
3.1.1. Two-Way ANOVA Results
3.1.2. Post hoc Test Results
4. Discussion
- The stringent control exercised throughout this experimental investigation facilitates the production of precise and relevant data. This methodological rigor allows for the accurate determination of surface hardness values, enabling a rapid and reliable assessment of the properties of thermoplastic dental resin specimens in comparison to alternative validation techniques.
- Nonetheless, the results may be subject to bias towards favorable outcomes, given the considerable discrepancy between the controlled laboratory conditions and the complex variables present in clinical settings. Consequently, the reproducibility of these positive findings in real-world applications remains uncertain.
- Furthermore, a notable limitation of this research is its reliance on a single measurement, which may constrain the statistical robustness and generalizability of the conclusions drawn.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Romanov, B.G. Design of Complex Plastic Elements Based on Modeling and Study of the Filling Process Through Virtual Prototyping. Ph.D. Thesis, Technical University, Sofia, Bulgaria, 2015. [Google Scholar]
- Ozyilmaz, O.Y.; Akin, C. Effect of cleansers on denture base resins’ structural properties. J. Appl. Biomater. Funct. Mater. 2019, 17, 2280800019827797. [Google Scholar] [CrossRef] [PubMed]
- Beltrán-Partida, E.; Valdez-Salas, B.; Curiel-Álvarez, M.; Castillo-Uribe, S.; Escamilla, A.; Nedev, N. Enhanced Antifungal Activity by Disinfected Titanium Dioxide Nanotubes via Reduced Nano-Adhesion Bonds. Mater. Sci. Eng. C 2017, 76, 59–65. [Google Scholar] [CrossRef]
- Mangal, U.; Kim, J.-Y.; Seo, J.-Y.; Kwon, J.-S.; Choi, S.-H. Novel Poly (Methyl Methacrylate) Containing Nanodiamond to Improve the Mechanical Properties and Fungal Resistance. Materials 2019, 12, 3438. [Google Scholar] [CrossRef] [PubMed]
- Read, N.; Wang, W.; Essa, K.; Attallah, M.M. Selective laser melting of AlSi10Mg alloy: Process optimization and mechanical properties development. Mater. Des. 2015, 65, 417–424. [Google Scholar] [CrossRef]
- Gogolewski, D.; Bartkowiak, T.; Kozior, T.; Zmarzły, P. Multiscale Analysis of Surface Texture Quality of Models Manufactured by Laser Powder-Bed Fusion Technology and Machining from 316L Steel. Materials 2021, 14, 2794. [Google Scholar] [CrossRef]
- Chladek, G.; Nowak, M.; Pakieła, W.; Mertas, A. Effect of Candida albicans Suspension on the Mechanical Properties of Denture Base Acrylic Resin. Materials 2022, 15, 3841. [Google Scholar] [CrossRef]
- Radford, D.R.; Sweet, S.P.; Challacombe, S.J.; Walter, J.D. Adherence of Candida albicans to denture-base materials with different surface finishes. J. Dent. 1998, 26, 577–583. [Google Scholar] [CrossRef]
- Yunus, N.; Rashid, A.A.; Azmi, L.L.; Abu-Hassan, M.I. Some flexural properties of a nylon denture base polymer. J. Oral Rehabil. 2005, 32, 65–71. [Google Scholar] [CrossRef]
- Munchow, E.A.; Ferreira, A.C.; Machado, R.M.; Ramos, T.S.; Rodrigues-Junior, S.A.; Zanchi, C.H. Effect of acidic solutions on the surface degradation of a micro-hybrid composite resin. Braz. Dent. J. 2014, 25, 321–326. [Google Scholar] [CrossRef]
- Arslan, M.; Murat, S.; Alp, G.; Zaimoglu, A. Evaluation of flexural strength and surface properties of prepolymerized CAD/CAM PMMA-based polymers used for digital 3D complete dentures. Int. J. Comput. Dent. 2018, 21, 31–40. [Google Scholar]
- Atalaya, S.; Çakmakb, G.; Fonsecac, M.; Schimmel, M.; Yilmazcef, B. Effect of thermocycling on the surface properties of CAD/CAM denture base materials after different surface treatments. J. Mech. Behav. Biomed. Mater. 2021, 121, 104646. [Google Scholar] [CrossRef] [PubMed]
- D’Ercole, S.; De Angelis, F.; Biferi, V.; Noviello, C.; Tripodi, D.; Di Lodovico, S.; Cellini, L.; D’Arcangelo, C. Antibacterial and Antibiofilm Properties of Three Resin-Based Dental Composites against Streptococcus mutans. Materials 2022, 15, 1891. [Google Scholar] [CrossRef] [PubMed]
- Wemken, G.; Burkhardt, F.; Spies, B.C.; Kleinvogel, L.; Adali, U.; Sterzenbach, G.; Beuer, F.; Wesemann, C. Bond Strength of Conventional, Subtractive, and Additive Manufactured Denture Bases to Soft and Hard Relining Materials. Dent. Mater. 2021, 37, 928–938. [Google Scholar] [CrossRef]
- Azpiazu-Flores, F.X.; Schricker, S.R.; Seghi, R.R.; Johnston, W.M.; Leyva Del Rio, D. Adhesive strength of 3 long-term resilient liners to CAD/CAM denture base polymers and heat-polymerized polymethyl methacrylate with thermocycling. J. Prosthet. Dent. 2022, 131, 494–499. [Google Scholar] [CrossRef]
- Bajunaid, S.O. How effective are antimicrobial agents on preventing the adhesion of Candida albicans to denture base acrylic resin materials? A systematic review. Polymers 2022, 14, 908. [Google Scholar] [CrossRef]
- Chladek, G.; Pakieła, K.; Pakieła, W.; Żmudzki, J.; Adamiak, M.; Krawczyk, C. Effect of antibacterial silver-releasing filler on the physicochemical properties of poly (methyl methacrylate) denture base material. Materials 2019, 12, 4146. [Google Scholar] [CrossRef] [PubMed]
- Fan, C.; Chu, L.; Rawls, H.R.; Norling, B.K.; Cardenas, H.L.; Whang, K. Development of an antimicrobial resin—A pilot study. Dent. Mater. 2011, 27, 322–328. [Google Scholar] [CrossRef]
- Kim, J.H.; Choe, H.C.; Son, M.K. Evaluation of Adhesion of Reline Resins to the Thermoplastic Denture Base Resin for Non-Metal Clasp Denture. Dent. Mater. J. 2014, 33, 32–38. [Google Scholar] [CrossRef][Green Version]
- Pfeiffer, P.; Rosenbauer, E.U. Residual methyl methacrylate monomer, water sorption, and water solubility of hypoallergenic denture base materials. J. Prosthet. Dent. 2004, 92, 72–78. [Google Scholar] [CrossRef]
- Rejab, L.T. The effect of the Thermopress curing technique on the water sorption and solubility of the cold and heat–cured acrylic resins. Al-Rafidain Dent. J. 2008, 8, 11–17. [Google Scholar] [CrossRef][Green Version]
- ISO 20795-1:2008; Dentistry-Denture Base Polymers. International Organization for Standardization: Geneva, Switzerland, 2008.
- Hristov, I.; Kalachev, Y.; Grozev, L. Application of Soft Relining Materials in Dental Medicine—Clinical Results. Folia Med. 2020, 62, 147–158. [Google Scholar] [CrossRef]
- Golbidi, F.; Jalali, O. An evaluation of the Flexural Properties of Meliodent and Acropars Heat Polymerized Acrylic Resins. J. Dent. Med. TUMS 2007, 4, 55–63. [Google Scholar]
- Bajunaid, S.O.; Baras, B.H.; Balhaddad, A.A.; Weir, M.D.; Xu, H.H. Antibiofilm and Protein-Repellent Polymethylmethacrylate Denture Base Acrylic Resin for Treatment of Denture Stomatitis. Materials 2021, 14, 1067. [Google Scholar] [CrossRef]
- Rubtsova, E.A.; Chirkova, N.V.; Polushkina, N.A.; Kartavtseva, N.G.; Vecherkina, Z.V.; Popova, T.A. Evaluation of the Microbiological Examination of Removable Dentures of Thermoplastic Material. J. N. Med. Technol. 2017, 2, 314–322. [Google Scholar]
- Bulad, K.; Taylor, R.L.; Verran, J.; McCord, J.F. Colonization and penetration of denture soft lining materials by Candida albicans. Dent. Mater. 2004, 20, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Vojdani, M.; Giti, R. Polyamide as a denture base material: A literature review. J. Dent. 2015, 16, 1–9. [Google Scholar]
- Srinivasan, M.; Kamnoedboon, P.; McKenna, G.; Angst, L.; Schimmel, M.; Ozcan, M.; Müller, F. CAD/CAM removable complete dentures: A systematic review and meta-analysis of trueness of fit, biocompatibility, mechanical properties, surface characteristics, color stability, time-cost analysis, clinical and patient-reported outcomes. J. Dent. 2021, 113, 103777. [Google Scholar] [CrossRef]
- Fouda, S.M.; Gad, M.M.; Abualsaud, R.; Ellakany, P.; AlRumaih, H.S.; Khan, S.Q.; Akhtar, S.D.; Al-Qarn, F.; Al-Harbi, F.A. Flexural Properties and Hardness of CAD/CAM Denture Base Materials. J. Prosthodont. 2022, 32, 318–324. [Google Scholar] [CrossRef]
- Tripathi, P.; Phukela, S.S.; Yadav, B.; Malhotra, P. An in vitro study to evaluate and compare the surface roughness in heat-cured denture-based resin and injection-molded resin system as affected by two commercially available denture cleansers. J. Indian Prosthodont. Soc. 2018, 18, 291–298. [Google Scholar]
- Totu, E.E.; Nechifor, A.C.; Nechifor, G.; Aboul-Enein, H.Y.; Cristache, C.M. Poly (Methyl Methacrylate) with TiO2 Nanoparticles Inclusion for Stereolithographic Complete Denture Manufacturing—The Future in Dental Care for Elderly Edentulous Patients? J. Dent. 2017, 59, 68–77. [Google Scholar] [CrossRef]
- Schwindling, F.S.; Rammelsberg, P.; Stober, T. Effect of Chemical Disinfection on the Surface Roughness of Hard Denture Base Materials: A Systematic Literature Review. Int. J. Prosthodont. 2014, 27, 215–225. [Google Scholar] [CrossRef] [PubMed]
- De Rezende Pinto, L.; Acosta, E.J.; Tavora, F.F.; da Silva, P.M.; Porto, V.C. Effect of Repeated Cycles of Chemical Disinfection on the Roughness and Hardness of Hard Reline Acrylic Resins. Gerodontology 2010, 27, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Duymus, Z.Y.; Ozdogan, A.; Ulu, H.; Ozbayram, O. Evaluation of the Vickers Hardness of Denture Base Materials. Open J. Stomatol. 2016, 6, 114–119. [Google Scholar] [CrossRef]
- Azevedo, A.; Machado, A.L.; Vergani, C.E.; Giampaolo, E.T.; Pavarina, A.C. Hardness of Denture Base and Hard Chair-Side Reline Acrylic Resins. J. Appl. Oral Sci. 2005, 13, 291–295. [Google Scholar] [CrossRef]
- Çakmak, G.; Donmez, M.B.; Akay, C.; Abou-Ayash, S.; Schimmel, M.; Yilmaz, B. Effect of Thermal Cycling on the Flexural Strength and Hardness of New-Generation Denture Base Materials. J. Prosthodont. 2023, 32, 81–86. [Google Scholar] [CrossRef]
- Bahrani, F.; Safari, A.; Vojdani, M.; Karampoor, G.; Patil, S.J. Comparison of Hardness and Surface Roughness of Two Denture Bases Polymerized by Different Methods. World J. Dent. 2012, 3, 171–175. [Google Scholar] [CrossRef]


| Temperature (°C) | Before Immersion (HSD) | After 24 h (HSD) | After 7 Days (HSD) |
|---|---|---|---|
| 300 | 73 | 76.7 | 77.6 |
| 280 | 69.4 | 70.4 | 71.6 |
| Time Point | Sample 1 (HSD) | Sample 2 (HSD) | Sample 3 (HSD) | Mean HSD |
|---|---|---|---|---|
| Before immersion | 73 | 73.6 | 72 | 73.0 |
| After 24 h | 73.8 | 76 | 76.7 | 75.15 |
| After 7 days | 76.4 | 76.7 | 77.6 | 76.57 |
| Time Point | Sample 1 (HSD) | Sample 2 (HSD) | Sample 3 (HSD) | Mean HSD |
|---|---|---|---|---|
| Before immersion | 69.4 | 70.2 | 69.9 | 69.83 |
| After 24 h | 71.1 | 70.4 | 70.4 | 70.63 |
| After 7 days | 73.5 | 71.6 | 70.8 | 71.63 |
| Before immersion (300 °C) | 73.0 | 73.6 | 72.0 | 72.87 |
| After 24 h (300 °C) | 73.8 | 76.0 | 76.7 | 75.50 |
| After 7 days (300 °C) | 76.4 | 76.7 | 77.6 | 76.90 |
| Before Immersion | After 24 h | After 7 Days | |
|---|---|---|---|
| Mean values HSD | 73 | 73.8 | 76.4 |
| 73.6 | 76 | 76.7 | |
| 72 | 76.7 | 77.6 |
| Mean values HSD | Before Immersion | After 24 h | After 7 Days |
| 69.4 | 69.9 | 73.5 | |
| 71.1 | 70.4 | 70.8 | |
| 71 | 71.1 | 70.8 | |
| 70.2 | 70.4 | 71.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chuchulska, B.; Dimitrova, M.; Dochev, B.; Georgiev, K. Exploring Polymeric Surfaces Manufactured Under Different Temperature Conditions—A Preliminary Experimental Study of Hardness. J 2025, 8, 22. https://doi.org/10.3390/j8030022
Chuchulska B, Dimitrova M, Dochev B, Georgiev K. Exploring Polymeric Surfaces Manufactured Under Different Temperature Conditions—A Preliminary Experimental Study of Hardness. J. 2025; 8(3):22. https://doi.org/10.3390/j8030022
Chicago/Turabian StyleChuchulska, Bozhana, Mariya Dimitrova, Boyan Dochev, and Kliment Georgiev. 2025. "Exploring Polymeric Surfaces Manufactured Under Different Temperature Conditions—A Preliminary Experimental Study of Hardness" J 8, no. 3: 22. https://doi.org/10.3390/j8030022
APA StyleChuchulska, B., Dimitrova, M., Dochev, B., & Georgiev, K. (2025). Exploring Polymeric Surfaces Manufactured Under Different Temperature Conditions—A Preliminary Experimental Study of Hardness. J, 8(3), 22. https://doi.org/10.3390/j8030022








