Performance of Ventilation, Filtration, and Upper-Room UVGI in Mitigating PM2.5 and SARS-CoV-2 Levels
Abstract
1. Introduction
2. Methodology
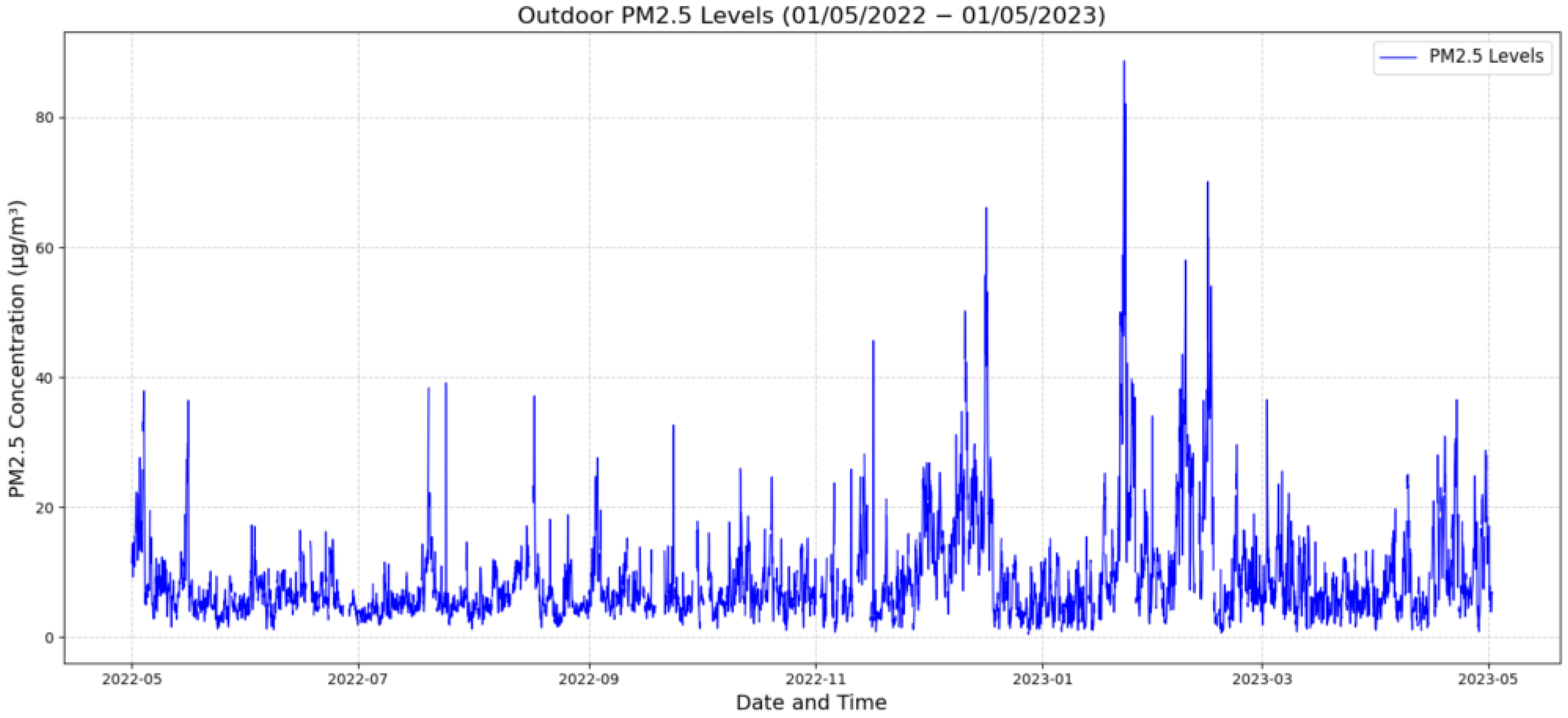
2.1. Defining Contaminants for Parametric Simulation
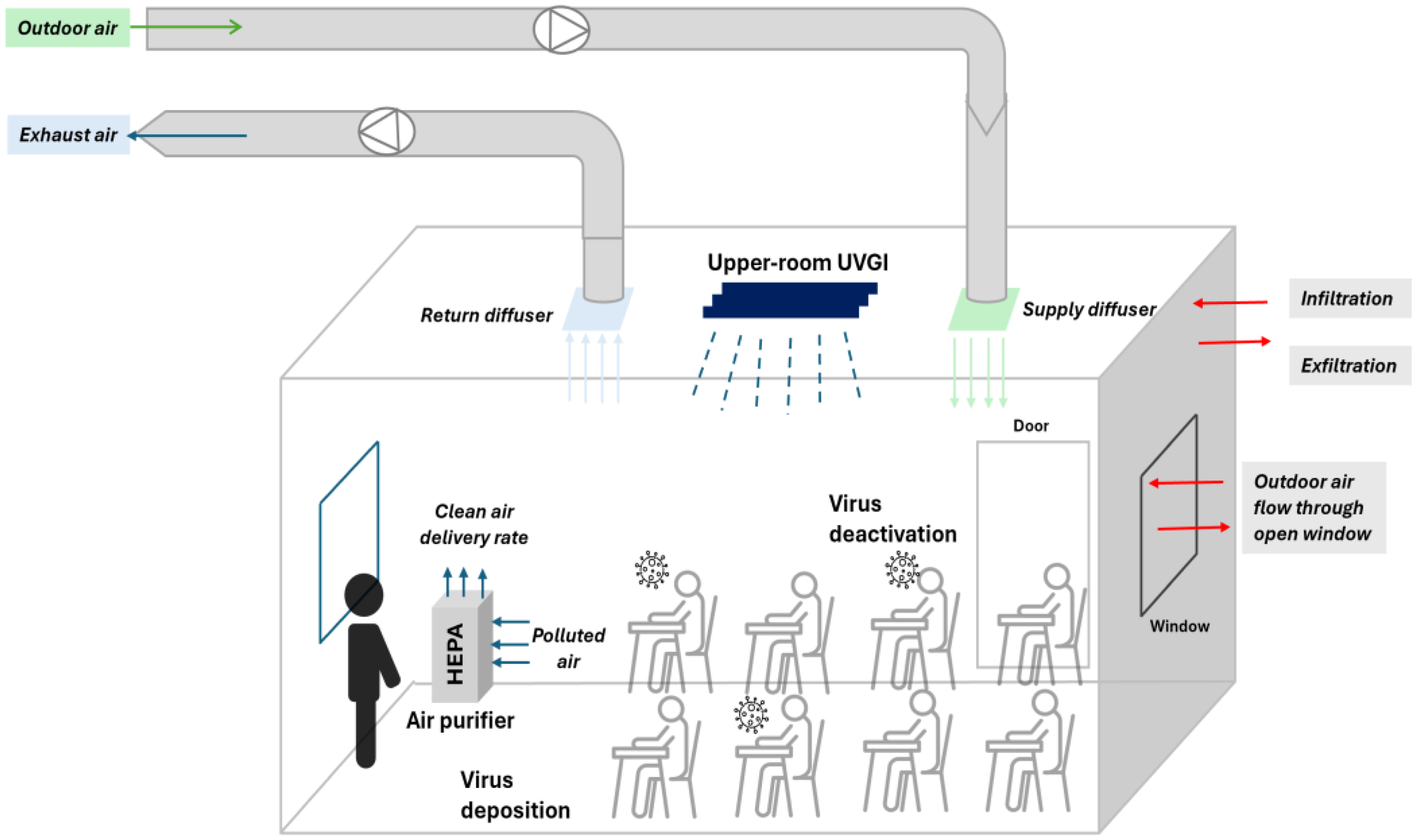
2.2. Numerical Analysis of Viral Concentration
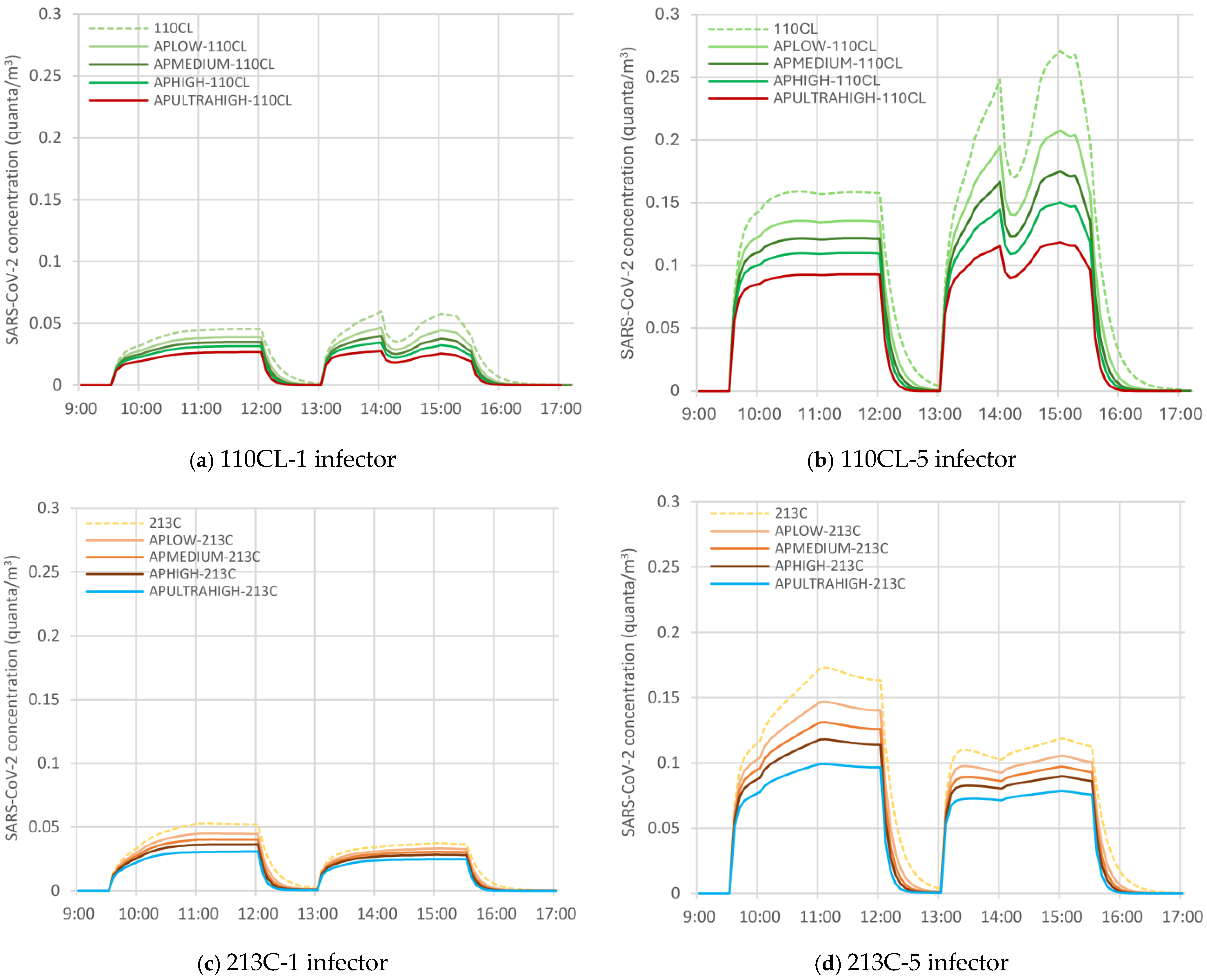
2.3. Air Purifier with HEPA Filter
2.4. Upper-Room UVGI
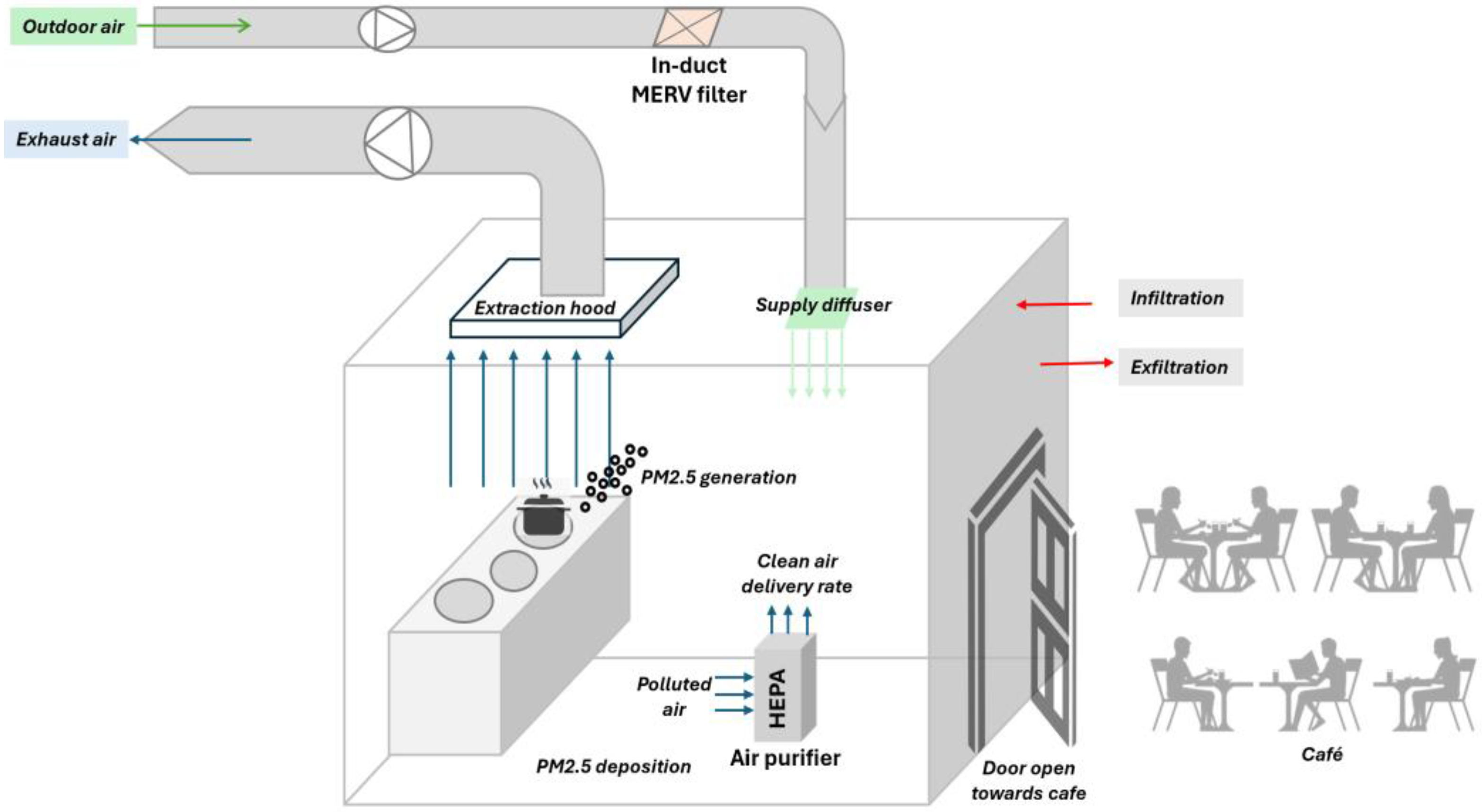
2.5. Installing In-Duct MERV Filter
2.6. Proposed Scenarios for Air Quality Improvement
3. Results
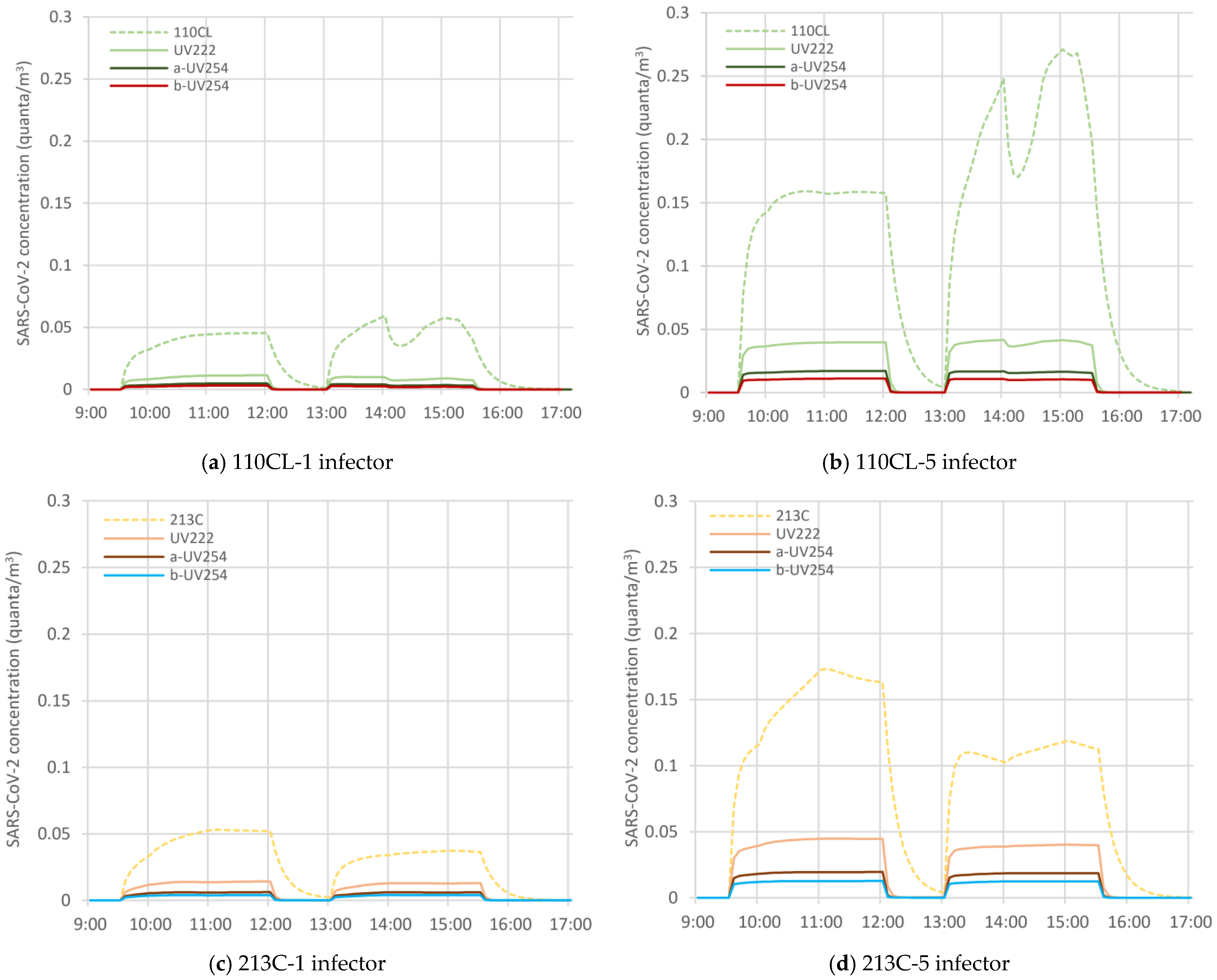
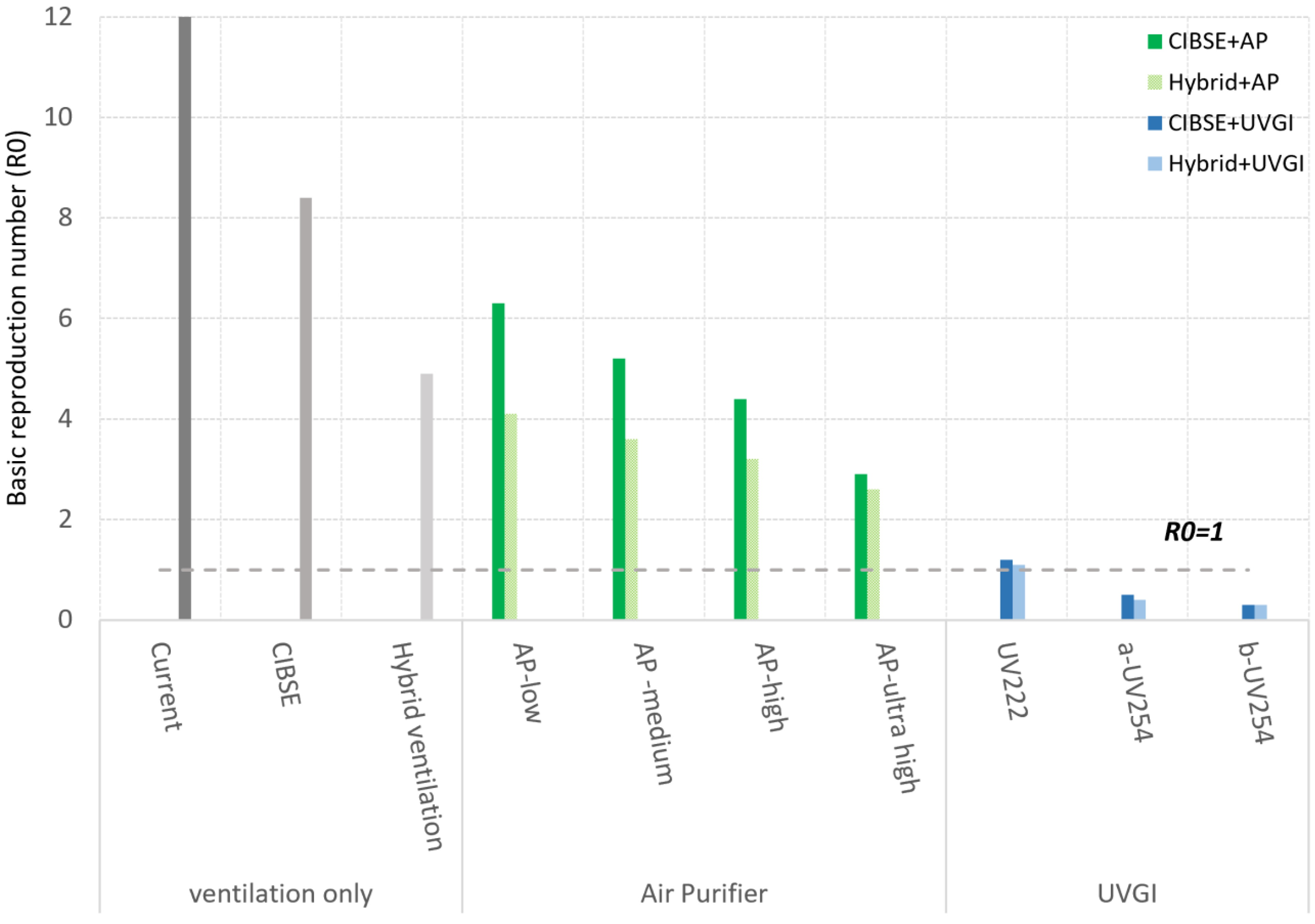
3.1. SARS-CoV-2 Controlling Strategies
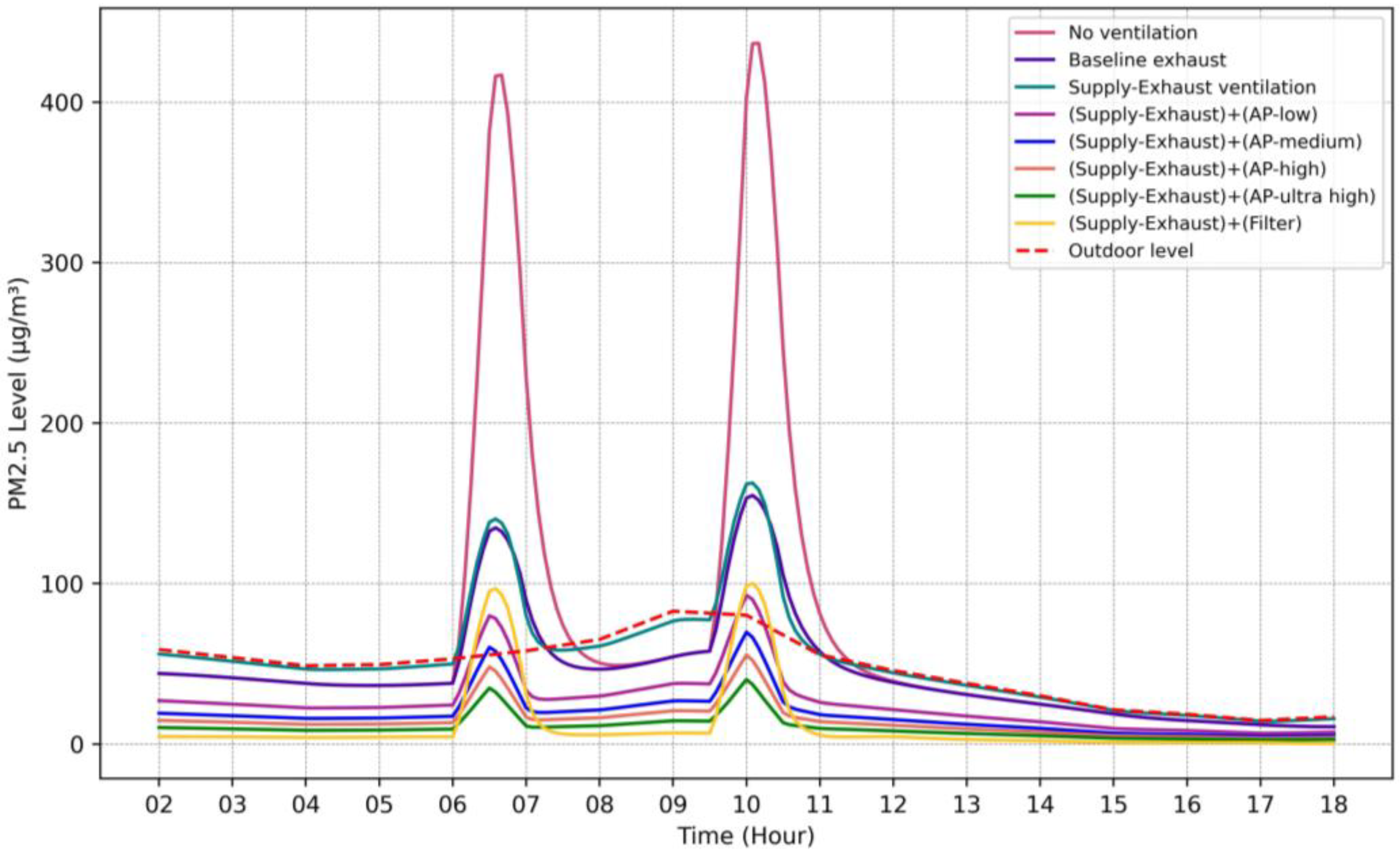
3.2. PM2.5 Controlling Strategies in the Kitchen
4. Discussion
5. Conclusions
- Hybrid ventilation achieves greater PI reductions and maintains better performance as infectors increase compared to mechanical ventilation with only a 2.5–16% drop in efficacy, compared to a 35% drop under mechanical ventilation. This results demonstrates the resilience of hybrid systems in high-risk scenarios and supports their use in buildings where controlling the virus spread under varying conditions is a priority.
- Upper-room UVGI systems outperformed all other options in high-risk viral scenarios (five infectors) by maintaining R0 consistently below 1. However, in low-risk scenarios (one infector), APs combined with hybrid ventilation were sufficient to reduce the R0 below 1 in all rooms. This shows that while UVGI offers the highest level of control, Aps, especially medium- to high-capacity models, can provide adequate protection in less critical conditions.
- Mechanical ventilation alone (CIBSE rates) is not sufficient under multiple-infector cases unless combined with high-performance APs or UVGI. This highlights the importance of enhancing ventilation with additional control layers, especially when windows cannot be opened.
- Supply–Exhaust ventilation introduces unfiltered outdoor air and increases indoor PM2.5 levels especially in polluted areas.
- Combining Supply–Exhaust ventilation with APs or MERV13 filters is essential for achieving safe PM2.5 levels (<5 µg/m3) and maintaining stable IAQ, even during cooking. These approaches not only met the WHO targets but also reduced daily fluctuations and improved overall air quality consistency. Moreover, AP-medium and AP-high models also achieved acceptable PM2.5 levels and offered a cost-effective alternatives in less polluted conditions.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- WHO. WHO Global Air Quality Guidelines: Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide, print version; World Health Organization: Geneva, Switzerland, 2021; pp. 1–273. ISBN 978-92-4-003421-1. [Google Scholar]
- Aguilar, A.J.; de la Hoz-Torres, M.L.; Costa, N.; Arezes, P.; Martínez-Aires, M.D.; Ruiz, D.P. Assessment of ventilation rates inside educational buildings in Southwestern Europe: Analysis of implemented strategic measures. J. Build. Eng. 2022, 51, 104204. [Google Scholar] [CrossRef] [PubMed]
- Wells, W.F. Airborne Contagion and Air Hygiene: An Ecological Study of Droplet Infections; Commonwealth Fund: Cambridge, MA, USA; Harvard University Press: Cambridge, MA, USA, 1955; 423p. [Google Scholar]
- Dai, H.; Zhao, B. Association of the infection probability of COVID-19 with ventilation rates in confined spaces. Build. Simul. 2020, 13, 1321–1327. [Google Scholar] [CrossRef] [PubMed]
- Iwamura, N.; Tsutsumi, K. SARS-CoV-2 airborne infection probability estimated by using indoor carbon dioxide. Environ. Sci. Pollut. Res. 2023, 30, 79227–79240. [Google Scholar] [CrossRef]
- Biasin, M.; Bianco, A.; Pareschi, G.; Cavalleri, A.; Cavatorta, C.; Fenizia, C.; Galli, P.; Lessio, L.; Lualdi, M.; Tombetti, E.; et al. UV-C irradiation is highly effective in inactivating SARS-CoV-2 replication. Sci. Rep. 2021, 11, 6260. [Google Scholar] [CrossRef]
- Kowalski, W.J. Ultraviolet Germicidal Irradiation Handbook: UVGI for Air and Surface Disinfection; Springer: New York, NY, USA, 2009. [Google Scholar]
- Riley, R.L.; Nardell, E.A. Clearing the air: The theory and application of ultraviolet air disinfection. Am. Rev. Respir. Dis. 1990, 142, 1233–1234. [Google Scholar] [CrossRef]
- Cui, H. Quantitative Microbial risk Assessment for Airborne transmission of SARS-CoV-2 And the efficacy of Ultraviolet Germicidal Irradiation (UVGI) Systems. Master’s Thesis, Purdue University, West Lafayette, IN, USA, 2022. [Google Scholar]
- Park, S.; Mistrick, R.; Rim, D. Performance of upper-room ultraviolet germicidal irradiation (UVGI) system in learning environments: Effects of ventilation rate, UV fluence rate, and UV radiating volume. Sustain. Cities Soc. 2022, 85, 104048. [Google Scholar] [CrossRef]
- Yan, S.; Wang, L.; Birnkrant, M.J.; Zhai, Z.; Miller, S.L. Multizone Modeling of Airborne SARS-CoV-2 Quanta Transmission and infection Mitigation Strategies in Office, Hotel, Retail, and School Buildings. Buildings 2023, 13, 102. [Google Scholar] [CrossRef]
- Emmerich, S.J.; Hirnikel, D. Validation of multizone IAQ modeling of residential-scale buildings: A review. Ashrae Trans. 2001, 107, 619–628. [Google Scholar]
- Shrestha, P.; DeGraw, J.W.; Zhang, M.; Liu, X. Multizonal modeling of SARS-CoV-2 aerosol dispersion in a virtual office building. Build Environ. 2021, 206, 108347. [Google Scholar] [CrossRef]
- Noakes, C.J.; Beggs, C.B.; Sleigh, P.A. Effect of room mixing and ventilation strategy on the performance of upper room ultraviolet germicidal irradiation systems. Proc. Ashrae Iaq. 2004, 1–13. [Google Scholar]
- Lau, J.; Bahnfleth, W.; Freihaut, J. Estimating the effects of ambient conditions on the performance of UVGI air cleaners. Build Environ. 2009, 44, 1362–1370. [Google Scholar] [CrossRef]
- Abhijith, K.V.; Kukadia, V.; Kumar, P. Investigation of air pollution mitigation measures, ventilation, and indoor air quality at three schools in London. Atmos. Environ. 2022, 289, 119303. [Google Scholar] [CrossRef]
- Rawat, N.; Kumar, P. Interventions for improving indoor and outdoor air quality in and around schools. Sci. Total Environ. 2023, 858, 159813. [Google Scholar] [CrossRef] [PubMed]
- Lyu, J.; Shi, Y.; Chen, C.; Zhang, X.; Chu, W.; Lian, Z. Characteristics of PM2.5 emissions from six types of commercial cooking in Chinese cities and their health effects. Environ. Pollut. 2022, 313, 120180. [Google Scholar] [CrossRef] [PubMed]
- Kang, K.; Kim, H.; Kim, D.D.; Lee, Y.G.; Kim, T. Characteristics of cooking-generated PM 10 and PM 2.5 in residential buildings with different cooking and ventilation types. Sci. Total Environ. 2019, 668, 56–66. [Google Scholar] [CrossRef]
- Ng, L.C.; Musser, A.; Persily, A.K.; Emmerich, S.J. Airflow and Indoor Air Quality Models of DOE Reference Commercial Buildings; NIST Technical Note 2072; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2019; 135p. [Google Scholar] [CrossRef]
- Riley, E.C.; Murphy, G.; Riley, R.L. Airborne spread of measles in a suburban elementary school. Am. J. Epidemiol. 1978, 107, 421–432. [Google Scholar] [CrossRef]
- Yan, S.; Wang, L.; Birnkrant, M.J.; Zhai, J.; Miller, S.L. Evaluating SARS-CoV-2 airborne quanta transmission and exposure risk in a mechanically ventilated multizone office building. Build. Environ. 2022, 219, 109184. [Google Scholar] [CrossRef]
- Dols, W.S.; Polidoro, B.J.; Poppendieck, D.; Emmerich, S.J. A Tool to Model the Fate and Transport of indoor Microbiological Aerosols (FaTIMA); NIST Technical Note 2095; National Institute of Standards and Technology: Gaithersburg, MD, USA, 2020; 32p. [Google Scholar] [CrossRef]
- Moreno, T.; Pintó, R.M.; Bosch, A.; Moreno, N.; Alastuey, A.; Minguillón, M.C.; Anfruns-Estrada, E.; Guix, S.; Fuentes, C.; Buonanno, G.; et al. Tracing surface and airborne SARS-CoV-2 RNA inside public buses and subway trains. Environ. Int. 2021, 147, 106326. [Google Scholar] [CrossRef]
- Rudnick, S.N.; Milton, D.K. Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air 2003, 13, 237–245. [Google Scholar] [CrossRef]
- Polichetti, G.; Cocco, S.; Spinali, A.; Trimarco, V.; Nunziata, A. Effects of particulate matter (PM10, PM2.5 and PM1) on the cardiovascular system. Toxicology 2009, 261, 1–8. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0300483X09002121 (accessed on 25 May 2025). [CrossRef]
- Singer, B.C.; Delp, W.W.; Price, P.N.; Apte, M.G. Performance of installed cooking exhaust devices. Indoor Air 2012, 22, 222–234. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Delsante, A.; Symons, J. Derivation of capture efficiency of kitchen range hoods in a confined space. Build. Environ. 1996, 31, 461–468. [Google Scholar] [CrossRef]
- Lunden, M.M.; Delp, W.W.; Singer, B.C. Capture efficiency of cooking—Related fine and ultrafine particles by residential exhaust. Indoor Air. 2015, 25, 45–58. [Google Scholar] [CrossRef] [PubMed]
- CIBSE. Environmental Design, CIBSE Guide A; CIBSE: London, UK, 2021; ISBN 978-1-906846-55-8. [Google Scholar]
- HM Government. The Building Regulations 2010. The Building Regulations 2010 For England and Wales, Part F; HM Government: London, UK, 2013.
- Underhill, L.J.; Milando, C.W.; Levy, J.I.; Dols, W.S.; Lee, S.K.; Fabian, M.P. Simulation of indoor and outdoor air quality and health impacts following installation of energy-efficient retrofits in a multifamily housing unit. Build. Environ. 2020, 170, 106507. [Google Scholar] [CrossRef]
- Shrubsole, C.; Ridley Biddulph, P.; Milner, J.; Vardoulakis, S.; Ucci, M.; Wilkinson, P.; Chalabi, Z.; Davies, M. Indoor PM 2.5 exposure in London’s domestic stock: Modelling current and future exposures following energy efficient refurbishment. Atmos. Environ. 2012, 62, 336–343. [Google Scholar] [CrossRef]
- Abbaspour, A.; Bahadori-jahromi, A.; Janbey, A.; Godfrey, P.B.; Amirkhani, S. Enhancing indoor Air Quality and Regulatory Compliance: Ann-Depth Comparative Study on Ventilation Strategies and Their impact on SARS-CoV-2 Transmission Risk. Sustainability 2023, 16, 271. [Google Scholar] [CrossRef]
- Buonanno, G.; Stabile, L.; Morawska, L. Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ. Int. 2020, 141, 105794. [Google Scholar] [CrossRef]
- Bazant, M.Z.; Bush, J.W.M. A guideline to limit indoor airborne transmission of COVID-19. Proc. Natl. Acad. Sci. USA 2021, 118, e2018995118. [Google Scholar] [CrossRef]
- Doremalen Nvan Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; LloydSmith, J.O.; et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567. [Google Scholar] [CrossRef]
- Fabian, P.; Adamkiewicz, G.; Levy, J.I. Simulating indoor concentrations of NO2 and PM2.5 in multifamily housing for use in health—Based intervention modeling. Indoor Air. 2012, 22, 12–23. [Google Scholar]
- Tran, D.T.; Alleman, L.Y.; Coddeville, P.; Galloo, J.C. Indoor and Built Indoor particle dynamics in schools: Determination of air exchange rate, size-resolved particle deposit rate and penetration factor in real-life conditions. Indoor Built Environ. 2017, 26, 1335–1350. [Google Scholar] [CrossRef]
- Schuit, M.A.; Larason, T.C.; Krause, M.L.; Green, B.M.; Holland, B.P.; Wood, S.P.; Grantham, S.; Zong, Y.; Zarobila, C.J.; Freeburger, D.L.; et al. SARS-CoV-2 inactivation by ultraviolet radiation and visible light is dependent on wavelength and sample matrix. J. Photochem. Photobiol. B Biol. 2022, 233, 112503. [Google Scholar] [CrossRef] [PubMed]
- Walker, C.M.; Ko, G. Effect of ultraviolet germicidal irradiation on viral aerosols. Environ. Sci. Technol. 2007, 41, 5460–5465. [Google Scholar] [CrossRef]
- Beggs, C.B.; Avital, E.J. Upper-room ultraviolet air disinfection might help to reduce COVID-19 transmission in buildings: A feasibility study. Peer J. 2020, 8, e10196. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Environmental Control for Tuberculosis: Basic Upper-Room Ultraviolet Germicidal Irradiation Guidelines for Healthcare Settings; Centers for Disease Control and Prevention: Cincinnati, OH, USA, 2009; p. 87. Available online: http://www.cdc.gov/niosh/docs/2009-105/ (accessed on 20 December 2024).
- Buonanno, M.; Randers-Pehrson, G.; Bigelow, A.W.; Trivedi, S.; Lowy, F.D.; Spotnitz, H.M.; Hammer, S.M.; Brenner, D.J. 207-nm UV Light—A Promising Tool for Safe Low-Cost Reduction of Surgical Site Infections. I: In Vitro Studies. PLoS ONE 2013, 8, e76968. [Google Scholar] [CrossRef]
- Blatchley, E.R.; Brenner, D.J.; Claus, H.; Cowan, T.E.; Linden, K.G.; Liu, Y.; Mao, T.; Park, S.J.; Piper, P.J.; Simons, R.M.; et al. Far UV-C radiation: An emerging tool for pandemic control. Crit. Rev. Environ. Sci. Technol. 2023, 53, 733–753. [Google Scholar] [CrossRef]
- ACGIH. 2021 TLVs and BEIs: Based on the Documentation of the Threshold Limit Values for Chemical and Physical Agents & Biological Exposure Indices; Ansi/Ashrae: Atlanta, GA, USA, 2019. [Google Scholar]
- ANSI/ASHRAE Standard 55; Thermal Environmental Conditions for Human Occupancy. ANSI/ASHRAE: Atlanta, GA, USA, 2017; Volume 7. p. 60.
- Santarpia, J.L.; Herrera, V.L.; Rivera, D.N.; Ratnesar-Shumate, S.; Reid, S.P.; Ackerman, D.N.; Denton, P.W.; Martens, J.W.S.; Fang, Y.; Conoan, N.; et al. The size and culture ability of patient generated SARS-CoV2 aerosol. J. Expo. Sci. Environ. Epidemiol. 2021, 32, 706–711. [Google Scholar] [CrossRef]
- Lee, B.U. Minimum sizes of respiratory particles carrying SARS-CoV-2 and the possibility of aerosol generation. Int. J. Environ. Res. Publ. Health 2020, 17, 6960. [Google Scholar] [CrossRef]
- Santarpia, J.L.; Rivera, D.N.; Herrera, V.L.; Morwitzer, M.J.; Creager, H.M.; Santarpia, G.W.; Crown, K.K.; Brett-Major, D.M.; Schnaubelt, E.R.; Broadhurst, M.J.; et al. Aerosol and surface contamination of SARS-CoV-2 observed in quarantine and isolation care. Sci. Rep. 2020, 10, 12732. [Google Scholar] [CrossRef]
- Lednicky, J.A.; Lauzardo, M.; Alam, M.M.; Elbadry, M.A.; Stephenson, C.J.; Gibson, J.C.; Morris, J.G. Isolation of SARS-CoV-2 from the air in a car driven by a COVID patient with mild illness. Int. J. Infect. Dis. 2021, 108, 212–216. [Google Scholar] [CrossRef]
- Mallach, G.; Kasloff, S.B.; Kovesi, T.; Kumar, A.; Kulka, R.; Krishnan, J.; Robert, B.; McGuinty, M.; Otter-Moore Sden Yazji, B.; Cutts, T. Aerosol SARS-CoV-2 in hospitals and long-term care homes during the COVID-19 pandemic. PLoS ONE 2021, 16, e0258151. [Google Scholar] [CrossRef] [PubMed]
- Justo Alonso, M.; Dols, W.S.; Mathisen, H.M. Using Co-simulation between Energy Plus and CONTAM to evaluate recirculation-based, demand-controlled ventilation strategies in an office building. Build. Environ. 2022, 211, 108737. [Google Scholar] [CrossRef]
- Abbaspour, A.; Bahadori-jahromi, A.; Mylona, A.; Janbey, A.; Godfrey, P.B. Mitigation of airborne contaminants dispersion in and educational building and investigate its impacts on indoor air quality and energy performance. Eng. Futur. Sustain. 2023, 1. [Google Scholar] [CrossRef]
- Brager, G.; Borgeson, S.; Lee, Y. Summary Report: Control Strategies for Mixed-Mode Buildings. 207AD. Available online: https://escholarship.org/uc/item/8kp8352h (accessed on 10 January 2025).
- Brager, G. Mixed-Mode Cooling; Oxford University Press: Oxford, UK, 2006; p. 8. [Google Scholar]
- Peng, Y.; Lei, Y.; Tekler, Z.D.; Antanuri, N.; Lau, S.K.; Chong, A. Hybrid system controls of natural ventilation and HVAC in mixed-mode buildings: A comprehensive review. Energy Build. 2022, 276, 112509. Available online: https://www.sciencedirect.com/science/article/abs/pii/S0378778822006806 (accessed on 18 October 2023). [CrossRef]
- Li, Z.; Ma, X.; Liao, Y. Combined performance of upper-room UVGI and ceiling-mounted air cleaners Foremoving active bioaerosol. Build. Environ. 2025, 267, 112230. [Google Scholar] [CrossRef]
- Lee, B.; Bahneth, W.P. Effects of installation location on performance and economics of in-duct ultraviolet germicidal irradiation systems for air disinfection. Build. Environ. 2013, 67, 193–201. [Google Scholar] [CrossRef]

| Recommendation | PM2.5 (µg/m3) | |
|---|---|---|
| 24 h | Annual | |
| Interim target 1 | 75 | 35 |
| Interim target 2 | 50 | 25 |
| Interim target 3 | 37.5 | 15 |
| Interim target 4 | 25 | 10 |
| AQG level | 15 | 5 |
| Input Parameter | Value | |
|---|---|---|
| Building model | ||
| Type | College building | |
| Types of most occupied rooms | Classroom–Laboratory–Café | |
| Occupancy schedules | Provided based on college’s annual time table for 2023 | |
| Number of occupants in studied zones | 110CL | 15 |
| 213C | 15 | |
| Kitchen | 1 | |
| Floor area of studied zones | 110CL | 54 m2 |
| 213C | 49 m2 | |
| Kitchen | 14 m2 | |
| Number of Occupied Days per Week | 110CL | 4 days |
| 213C | 3 days | |
| Kitchen | 6 days | |
| Number of floors | 3 | |
| Total floor area | 2500 m2 | |
| Floor height | 2.8 m | |
| Location and weather file | London-TRY weather file from CIBSE | |
| Ventilation system | Air handling unit | |
| Total ventilation rate | 5289 m3/h-calculated and validated in previous study [34] | |
| ACH | 0.8–1.0 h−1 [34] | |
| External wall/floor leakage area | 2.2 cm2/m2 (@4 Pa) | |
| Outdoor air | 100% | |
| Recirculating air | 0% | |
| SARS-CoV-2 model | ||
| Source | Infected person | |
| Generation rate | 65 quanta/h [22,35] | |
| Breathing rate | 0.75 m3/h- light activity (whispering and speaking) [36] | |
| Deposition rate | 0.24 h−1 [24] | |
| Deactivation rate | 0.63 h−1 [37] | |
| Initial concentration | 0 quanta | |
| PM2.5 model | ||
| Source | Cooking activity (gas-burner) | |
| Generation rate | 1.56 mg/min [38] | |
| Deposition rate | 0.5 h−1 [39] | |
| Initial concentration | Same as outdoor level | |
| Outdoor PM2.5 penetration factor | 1.0 [33] | |
| CADR, m3/h | Max. Room Area, m2 | Efficiency, % | Manufacturer | Model | Power Consumption, W | |
|---|---|---|---|---|---|---|
| AP-low | 390 | 99 | 99.99 | Winix- South Korea | 5300 | 50 |
| AP-medium | 697 | 274 | 99.98 | Levoit-China | Core-600s | 49 |
| AP-high | 1016 | 342 | 99.9 | Medify-USA | MA-112 | 120 |
| AP-ultra high | 1614 | 110 | 99.97 | Blueair- Sweden | Pro XL | 256 |
| Wavelength (nm) | Average Fluence Rate (µW/cm2) | Susceptibility Constant (cm2/mJ) | Radiation Volume (Fraction of Room Volume %) | |
|---|---|---|---|---|
| UV222 | 222 | 3 | 4.22 | 1 |
| a-UV254 | 254 | 40 | 2.93 | 0.3 |
| b-UV254 | 254 | 50 | 3.77 | 0.3 |
| Scenarios | Applied Strategies | |
|---|---|---|
| 1 | No ventilation (worst case) | Without any ventilation |
| 2 | Baseline Exhaust | Only exhaust hood |
| 3 | Supply–Exhaust Ventilation | Hood + supply fresh air (OA) |
| 4 | HEPA Purification | Supply–Exhaust ventilation + AP (4 types from Table 3) |
| 5 | MERV13 Filtration | Supply–Exhaust ventilation + filtering supply OA |
| Zones | 213C | 110CL | |||
|---|---|---|---|---|---|
| Exposure time (h) | 2.5 | 2.5 | |||
| Scenarios | Number of infectors | PI (%) | R0 | PI (%) | R0 |
| Baseline ventilation | 1 | 29.4 | 4.4 | 28.0 | 4.2 |
| 2 | 50.2 | 7.5 | 48.1 | 7.2 | |
| 5 | 82.5 | 12.4 | 80.1 | 12.1 | |
| CIBSE ventilation (only mechanical) | 1 | 15.3 | 2.3 | 15.2 | 2.3 |
| 2 | 28.3 | 4.2 | 28.1 | 4.2 | |
| 5 | 56.4 | 8.5 | 56.1 | 8.4 | |
| Hybrid ventilation | 1 | 6.1 | 0.9 | 8.4 | 1.3 |
| 2 | 9.4 | 1.4 | 15.2 | 2.3 | |
| 5 | 18.6 | 2.8 | 32.7 | 4.9 | |
| Scenarios | Mean (µg/m3) | Min (µg/m3) | Max (µg/m3) | SD | 75th Percentile | Percentage of PM2.5 Levels Greater than 15 µg/m3 (%) | |
|---|---|---|---|---|---|---|---|
| No ventilation (worst case) | 21.98 | 0.32 | 436.71 | 63.04 | 9.57 | 16.47 | |
| Baseline Exhaust | 10.51 | 0.32 | 154.97 | 17.57 | 9.02 | 14.48 | |
| Supply–Exhaust Ventilation | 17.58 | 0.39 | 162.70 | 16.57 | 11.17 | 17.58 | |
| HEPA Purification | AP-low | 5.71 | 0.18 | 92.7 | 8.83 | 5.29 | 6.52 |
| AP-medium | 4.08 | 0.13 | 69.73 | 6.48 | 3.74 | 4.60 | |
| AP-high | 3.15 | 0.10 | 55.52 | 5.07 | 2.87 | 3.74 | |
| AP-ultra high | 2.21 | 0.07 | 40.22 | 3.60 | 2.00 | 2.57 | |
| MERV13 Filtration | 4.00 | 0.02 | 100.16 | 14.73 | 0.97 | 5.31 | |
| Scenarios | No Ventilation (Worst Case) | Baseline Exhaust | Supply- Exhaust Ventilation | HEPA Purification | MERV13 Filtration | |||
|---|---|---|---|---|---|---|---|---|
| AP-Low | AP- Medium | AP-High | AP- Ultra high | |||||
| Mean (µg/m3) | 54.8 | 37.7 | 45.0 | 22.0 | 15.7 | 12.1 | 8.5 | 8.5 |
| Baseline to Hybrid | Baseline to CIBSE | ||||
|---|---|---|---|---|---|
| Zones | 213C | 110CL | 213C | 110CL | |
| % reduction in PI | 1 | 79% | 70% | 48% | 46% |
| 5 | 77% | 59% | 31% | 30% | |
| Reduction in system efficacy | 2.5% | 16% | 35% | 35% | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abbaspour, A.; Seraj, H.; Bahadori-Jahromi, A.; Janbey, A. Performance of Ventilation, Filtration, and Upper-Room UVGI in Mitigating PM2.5 and SARS-CoV-2 Levels. Clean Technol. 2025, 7, 53. https://doi.org/10.3390/cleantechnol7030053
Abbaspour A, Seraj H, Bahadori-Jahromi A, Janbey A. Performance of Ventilation, Filtration, and Upper-Room UVGI in Mitigating PM2.5 and SARS-CoV-2 Levels. Clean Technologies. 2025; 7(3):53. https://doi.org/10.3390/cleantechnol7030053
Chicago/Turabian StyleAbbaspour, Atefeh, Hamidreza Seraj, Ali Bahadori-Jahromi, and Alan Janbey. 2025. "Performance of Ventilation, Filtration, and Upper-Room UVGI in Mitigating PM2.5 and SARS-CoV-2 Levels" Clean Technologies 7, no. 3: 53. https://doi.org/10.3390/cleantechnol7030053
APA StyleAbbaspour, A., Seraj, H., Bahadori-Jahromi, A., & Janbey, A. (2025). Performance of Ventilation, Filtration, and Upper-Room UVGI in Mitigating PM2.5 and SARS-CoV-2 Levels. Clean Technologies, 7(3), 53. https://doi.org/10.3390/cleantechnol7030053







