Abstract
Background: Patients with heart failure (HF) may benefit greatly from cardiopulmonary rehabilitation (CR), which is provided by a team of healthcare professionals that often includes nurses. There has been no research on how nurses perceive providing CR or the hurdles that may affect referrals. Methods: All registered nurses in Saudi Arabia’s Eastern Province were given access to a cross-sectional online survey consisting of nine multiple-choice questions that address attitudes, beliefs, and barriers to CR for HF patients in Saudi Arabia. Descriptive statistics were used to characterize the respondents. Results: Altogether, 439 registered nurses participated in the online survey, with men making up 194 (44%) and women 245 (56%). The mean and SD of years of clinical experience in caring for patients with HF were 6 ± 5 years. Out of 439 nurses, 107 (24%) strongly agree, and 255 (58%) agree that CR will enhance the physical fitness of patients. However, 94 (21.1%) strongly agree, and 248 (56.4%) agree that CR might alleviate dyspnea in HF patients. The vast majority of the nurses either strongly agree (90 (20.5%)) or agree (240 (55%)), that CR would help reduce palpitations and fatigue in HF patients. Indeed, 87 (19.81%) strongly agree, and 262 (59.68%) agree that CR would help improve HF patients’ ability to perform daily activities, while 51 (11.6%) strongly agree and 223 (51%) agree that CR would help in reducing hospital readmission. It was shown that 360 (82%) of the 439 nurses favored the delivery of CR programs in hospital-supervised programs, while 368 (83.8%) ranked information on HF disease as the most important aspect of the CR program, followed by information about medications at 305 (69.4%). The availability of CR facilities (36%), the cost of therapy (35%), and the absence of an established standardized referring strategy (34%) were identified as the most significant barriers affecting the referral of patients with HF for CR by nurses. Conclusion: Generally, nurses believed CR helped improve desired clinical outcomes in HF patients. Although a hospital-based program with close supervision is optimal for administering CR, few such options exist. Referrals of patients with HF were hampered by the lack of CR facilities, the cost of intervention, and the lack of a systematic approach to referrals.
1. Introduction
Cardiopulmonary diseases are a primary cause of morbidity and death across the globe, with a huge effect on the nation’s healthcare systems []. Most studies have shown that cigarette smoking and exposure to indoor air pollution, such as biomass burning, ambient air pollution, and occupational pollutants, are among the most common risk factors for cardiopulmonary diseases [,]. Heart failure (HF) is one form of cardiopulmonary disease. HF is a significant clinical illness characterized by symptoms and signs caused by the heart’s inability to pump enough blood to fulfill the body’s demands, resulting in decreased organ perfusion and, eventually, death if not treated properly []. Worldwide, HF is the major cause of death and disability in which patients often have difficulties doing daily tasks and have low exercise tolerance []. Exertion often brings on a worsening of these symptoms, which in turn causes more complications and unneeded visits to the emergency room [,]. Many other related conditions can be associated with HF, such as chronic destructive pulmonary diseases (COPD) []. An estimated 32,200 new cases of HF are diagnosed each year in Saudi Arabia, bringing the total projected prevalence to 455,222 []. Similarly, an estimated 434,560.64 Saudis had COPD in 2019, which is a 329.82% rise over the number of people diagnosed in 1990 []. HF affects patients in every way imaginable, including their physical health, social lives, mental health, emotional health, and spiritual health []. Fatigue, shortness of breath, insomnia, drowsiness, and anxiety are all common secondary symptoms of HF that contribute to these unfavorable outcomes []. Treatment for HF aims to extend life expectancy, improve quality of life, and forestall further disease deterioration and hospitalizations []. Accordingly, as a part of a nursing care plan, nurses must take action to enhance the quality of life of their HF patients [].
The experts’ recommendations call for cardiopulmonary rehabilitation (CR) for HF patients who continue to have symptoms while receiving medication and for those who have the poor functional ability as a common intervention for such cases [,]. In clinically stable HF patients, CR increases the quality of life and exercise tolerance []. A meta-analysis of trials in patients with chronic HF provided evidence that exercise training causes a reduction in mortality and hospital admission by 45% and 38%, respectively []. Even though it has been shown that rehabilitation may increase a patient’s quality of life, its impact may be affected by the process of implementation that includes patients and the multidisciplinary team []. Because a CR program comprises a medical evaluation, patient education, dietary assistance, mental health and psychosocial support, and a physical activity counseling program, a multidisciplinary healthcare team should support a CR program [,]. The team includes physicians, nurses, respiratory therapists, physiotherapists, psychologists, occupational therapists, dietitians, psychologists, and social workers [,].
It is well known that nurses play an evident role in facilitating CR since the majority of nurses directly interact with HF patients who are candidates to be referred to CR programs [,]. However, cardiopulmonary rehabilitation services are not frequently used in Saudi Arabia despite evidence that CR is beneficial for HF patients []. Because nurses play such a significant role in healthcare management, including CR, understanding their attitudes and expectations is critical to increasing CR utilization among HF patients. Furthermore, no research has been conducted from the perspective of nurses on the obstacles and limitations that can affect the decision to refer HF patients to CR programs in Saudi Arabia. Therefore, this study aims to fill this knowledge gap by assessing nurses’ attitudes, beliefs, and barriers to CR for HF patients in Saudi Arabia.
2. Materials and Methods
A cross-sectional online survey was performed using the Survey Monkey platform and disseminated between 13 February and 22 July.
For this study, the researcher used, with permission, a modified questionnaire that had been developed, piloted, and validated by Aldhahir et al. []. There were nine multiple-choice questions in the survey. Additionally, to obtain a greater depth of information, respondents were given the option to provide additional feedback by answering open-ended questions.
The willingness of the nurses to finish the survey was verified by asking whether or not they were happy to participate and by answering “yes” to complete the survey. Clicking “yes” was considered consent and agreement to participate in the study. The survey consists of three parts with multiple-choice questions. The first part of the survey focused on demographic questions, such as gender, occupation, location, number of years working with HF patients, and job duties. Three questions followed in the second part that probed nurses’ perceptions of cardiopulmonary rehabilitation on a 5-point Likert scale that ranges from 1 (strongly disagree) to 5 (strongly agree). The first question asked participants to rate their level of agreement with five statements on the efficacy of cardiopulmonary rehabilitation with patients suffering from HF. The second question concerned what else, besides exercise, is included in cardiopulmonary rehabilitation, whereas the third question inquired into the most effective ways to deliver this type of treatment to HF patients. In the third part of the survey, participants were asked two questions about what variables, patient and process-related, impact the decision to recommend or not refer patients with HF for CR. The questions below based their scores on how much importance one gave to one’s impact (no influence, some influence, and strong influence).
2.1. Study Population and Sampling Strategy
Convenience sampling was used to enroll research participants. The primary target for this study was the registered nurses in the Eastern province of Saudi Arabia who had only direct interaction with HF patients in their practice. The survey was widely disseminated via nursing professional bodies and online social media platforms to ensure maximum participation from nurses. Because this was experimental research, determining an appropriate sample size was not necessary. This research received ethical approval from the Institutional Review Board, reference number (REC-43/03/041). Before any data were collected from the participants, they were given full details of the research, assured that their participation was totally voluntary, and provided with the option to provide explicit informed consent.
2.2. Statistical Analysis
The Statistical Package for Social Sciences was used to gather and analyze data (SPSS software, Version 27, Inc., Chicago, IL, USA). The categorical variables were provided in percentages and frequencies. No formal analysis was applied due to the nature of the study, which is mainly descriptive.
3. Results
Altogether, 439 registered nurses participated in the online survey. The female participants comprised 56% of the total (245). Men, on the other hand, represent 44% (194). The mean and ±SD of years of clinical experience in caring for patients with HF were 6 ± 4 years (Table 1). Additionally, Table 1 demonstrates the eleven duties that are required by the nurse in her/his caring for HF patients. Primary care (75.17%), oxygen treatment (72%), and urgent evaluation (51%) were, respectively, the most prevalent duties of nurses caring for patients with HF.

Table 1.
Demographic data and nurses’ duties (n = 439).
3.1. Opinions on Referring Patients with Heart Failure to Cardiopulmonary Rehabilitation
Of the total participants (439), 82.46% agreed that CR would enhance the physical fitness of patients; specifically, 107 (24%) strongly agree, and 255 (58%) agree. Interestingly, 94 (21.1%) strongly agree and 248 (56.4%) agree that CR might alleviate dyspnea in HF patients (Table 2). The vast majority of the participants strongly agree (90 (20.5%)) or agree (240 (55%)) that CR would help reduce palpitations and fatigue in HF patients. Moreover, 87 (19.81%) strongly agree and 262 (59.68%) agree that CR would help improve HF patients’ ability to perform daily activities, 51 (11.6%) strongly agree and 223 (51%) agree that CR would help in reducing hospital readmission.

Table 2.
Perception on referring patients with heart failure to cardiopulmonary rehabilitation (n = 439).
3.2. Mode of Delivery and Component of Cardiopulmonary Rehabilitation
This study showed that 360 (82%) of the 439 nurses favored the delivery of CR programs in hospital-based supervised programs, whereas 121 (27.56%) chose an online program with healthcare professional assistance. However, 81 (18.45%) chose a CR program that was custom-tailored with HCP assistance available by telephone. Out of the total respondents, 368 (83%) ranked information on HF disease as the most important aspect of the CR program, followed by information about medications 305 (69.4%) (Table 3).

Table 3.
Mode of delivery and component of cardiopulmonary rehabilitation (n = 439).
3.3. Patient-Related Factors That Influence Referral Decision to Cardiopulmonary Rehabilitation
Patients’ disease-related fatigue (44%), breathlessness-related mobility limitations (41%), and patients’ knowledge of their condition and ability to manage it (40%) were reported as the most influential variables that affect referring decision of HF patients to CR (Figure 1).
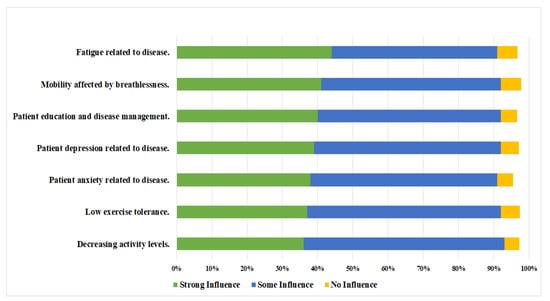
Figure 1.
Patient-related factors that influence referral decision to cardiopulmonary rehabilitation, using strong, some, or no influence as a grading tool (n = 439).
3.4. CR Referral Barriers
The most significant barriers affecting the referral of patients with HF for CR from the nurses’ perceptions were identified as the availability of CR facilities (36%), the cost of therapy (35%), and the absence of an established standardized referring strategy (34%). However, the participants agree that all of the aforementioned barriers are less likely to have a strong influence on referring HF patients to CR (Figure 2).
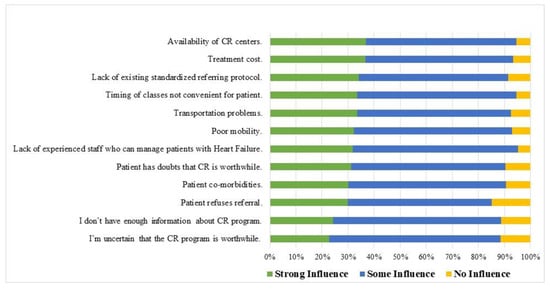
Figure 2.
Barriers to not referring patients with Heart Failure to cardiopulmonary rehabilitation, using influence graded as no, some, or strong influence (n = 439).
4. Discussion
To the best of the author’s knowledge, this is the first study of its kind in Saudi Arabia that explores the perspectives and attitudes of nurses on the value of CR programs, their critical components, and the most favored form of delivery. Moreover, this study looked at the obstacles to referring patients with HF to CR programs and the factors that influence this process. There was general agreement about the usefulness of CR as a holistic program for decreasing inpatient readmission rates, increasing exercise levels, and treating disease-related symptoms in HF patients. It was also agreed upon that stress and symptom management are crucial components of a complete CR program and that hospital-supervised CR is the optimum method of delivering the program for these patients.
A growing body of evidence shows that CR is an efficient and secure non-pharmacological therapy for patients with HF [,]. It reduces dyspnea and fatigue that comes with having HF. Additionally, it aids in enhancing physical capability, cardiovascular fitness, and quality of life, which in turn decreases hospitalization for HF patients [,]. In this study, nurses perceived CR as an effective management program for patients with HF. About 81% of the participants in the current study believe that CR will improve HF patients’ physical fitness. These findings are in line with previous studies that reported the positive role of nurses in improving outcomes of patients with HF and consequently enhancing their quality of life []. In addition, similar to previous studies [,], this study pointed out that nurses agree that CR plays a significant role in providing thorough treatment to patients with HF, which indicates great awareness and attitudes toward CR in HF patients; although, some of them reported that they do not have enough information about CR programs. As CR is a multidisciplinary program, Kellar et al. [] investigated Cardiology Fellow’s knowledge and attitude toward CR and reported a strong belief in the benefits of CR for CF patients, which supports the findings of the current study about nurses’ perceptions.
Accordingly, based on the nurses’ beliefs in the current study, information about HF disease and the medications were top-rated components when delivering CR to HF patients. Such components are crucial to increase CR utilization []. Nurses are in charge of the patient’s daily care, which includes monitoring the patient’s vital signs, cardiac rhythms, and any consequences after surgery or a procedure, as well as administering drugs and educating the patient about how to use them [,]. Because nurses are in constant touch with their patients, they are in a prime position to spot important “teachable moments” throughout the day []. This highlights the importance of nurses in the provision of CR, in which longer duration of the nurses’ interactions with their patients provides a special chance to conduct a continuous, in-depth conversation about the significance of CR in outpatient settings [].
One of the findings of the study is that the most important factors in nurses’ referral decisions for HF patients to CR were patients’ perceptions of their fatigue due to disease-related symptoms (44%), patient’s perceptions of their mobility limitations due to breathlessness (41%), and patient’s knowledge of their condition and ability to manage it (40%). In other countries, electronic referral and electronic prompts have been shown to enhance CR referral, suggesting that the lack of these automated referral mechanisms in Saudi Arabia may lead to underutilization of CR across all patient categories []. Furthermore, for patients with HF, research on the links between automated referral, patient engagement, and patient outcomes in cardiac rehabilitation is needed [].
Although cardiac rehabilitation (CR) has been shown to enhance health outcomes, low participation rates are a significant cause for worry. This may be due to several factors, including those on the part of the physician, the patient, and the health service itself []. In another study with over 29,000 patients hospitalized for cardiac procedures, only 15.6% attended at least one session of CR after being discharged []. This might attribute to well-known barriers reported in the literature [], which will be discussed fully in the following sections. The nurses’ perception of the most recognized barriers, which influence referring HF patients, has been investigated in the current study. However, some of the identified barriers can be discussed and addressed with the nominated patients before CR referral. Addressing these barriers with proper solutions and strategies will improve enrollment and attendance in CR classes and overcome these barriers. These barriers can be classified as healthcare and patient-related barriers.
The availability of CR facilities was the most often mentioned barrier to referring patients with HF to CR programs (37%). Compared to developed countries such as Canada, which has 128 CR centers, CR in Saudi is still in its early stage of development []. According to the literature, there are only three CR centers in Saudi Arabia that provide CR programs to outpatients, and these facilities can only accept a small number of patients with cardiac disease []. This is consistent with other countries where these facilities are restricted and underfunded [], such as China (less than 10%) [] and Turkey. It seems that the availability of specialized CR centers is a global concern. Interestingly, Turk-Adawi et al. [] reported that only 68% of the developed countries provide CR for HF patients. Thus, the results of this study are consistent with prior research on the challenges to establishing pulmonary rehabilitation programs in Saudi Arabia, which found that one of the primary impediments was a shortage of resources in medical facilities [,,].
The participants considered the lack of a standardized referring protocol as a barrier, which has an influence (ranging from strong to some) on referring HF patients to CR programs. This result aligned with that reported by Elsakr et al. [], who investigated barriers facing physicians when referring patients to CR. Since the present clinical practice does not follow worldwide clinical guidelines, uniform standards for CR must be established and implemented nationwide. It is important to remember that interdisciplinary cooperation among nurses and other professionals is a viable option for including CR in clinical settings [].
It is well-reported that a lack of awareness among CR multidisciplinary teams could negatively affect referring rates []. Although awareness of the benefits and nature of CR programs is a potential factor for nurses, our respondents reported that they do not have enough information and were uncertain that the CR program is worthwhile. In such a situation, nurses will not be able to provide reasonable guidance and advice to HF patients about the significance and importance of CR, which in turn decrease their compliance and benefit from the programs.
In addition to the above-mentioned barriers, there are other factors, such as the cost of treatment, influencing referring patients, and the utilization of CR, that are rated high by the respondents in this study. Currently, healthcare, including CR, is free of charge to all Saudi citizens and Non-Saudis working in the public sector. However, as mentioned earlier, due to the limited number of governmental CR centers, HF patients are constrained to private centers, which are very expensive. On the other hand, due to the health status of HF patients, the inconvenience of transport to the CR center is another factor that might influence patients’ decision to attend the rehabilitation program. Although rated third (25%) by our participants, home-based rehabilitation mode can overcome the last two factors, namely, cost and transportation difficulties.
The lack of experienced staff who can manage HF patients is considered one of the barriers that have some influence on referring patients to CR, as perceived by the nurses in the current study (Figure 2). However, it is axiomatic that lack of work experience correlates well with a negative attitude toward CR, as reported earlier []. This emphasizes the need to add courses at both undergraduate and postgraduate levels with sufficient training afterward. Surely, this will greatly improve cardiac rehabilitation services and increase patients’ trust and satisfaction.
Regarding the patients’ related barriers, according to the literature, less than 30% of eligible patients for CR do attend the classes, and of those who are referred, only 40% do complete the CR course []. This is due to several reasons. Nurses who participated in this study perceived certain factors, which are typical symptoms of HF, that might prevent patients from attending the CR program. These include physical and psychological conditions illustrated in Figure 1. The most specified physical factors are fatigue (44%) and breathlessness (41%). The current result is in line with Fine’s study (2009), which reported that 69% to 88% of HF patients experience fatigue as the most prevalent symptom []. A similar frequency was reported for breathlessness as an HF symptom []. Some of the patient-related factors indicated by the participants that might affect the referral decision to CR are the low tolerance to exercises and decreasing activity level. However, these should not cause any concern because it has been previously reported that CR improves exercise tolerance [] and physical activity in patients of all ages []. Thus, this fact should be explained fully to HF patients, and they should be encouraged to attend the CR program. However, HF patients need psychological support to improve their physical activity level, as it was found that physical activity correlates negatively with depression []. For instance, the timing of classes must be convenient for HF patients. This factor is emphasized when these individuals are employed. The conflict between CR classes and work time, as well as the long time required for rehabilitation, will hinder the compliance rate as perceived by our participants (Figure 2). Previous studies have reported other reasons for low compliance rather than time conflicts. These include patients’ age, sex, ethnicity, and health knowledge level [].
For practice implications, simpler, low-cost approaches should be proposed that may take advantage of unsupervised delivery methods while still meeting the need for comprehensive CR programs. Nurses should use counseling and other evidence-based interventions that encourage patients to participate and stick to treatment plans. Policymakers and consumers should utilize this data to improve the design and development of such programs while taking into account all the identified barriers. To enhance the clinical outcomes of cardiac patients, there is an obvious need for more research into the effectiveness of these approaches in Saudi Arabia.
5. Study Limitations
Several cautions should be noted about this research. This research might be biased since it relied on a sample method that could be considered arbitrary: convenience sampling. Second, the research excluded other types of medical personnel who could be engaged in the treatment of HF patients. In addition, qualitative interviews would have helped collect more complete data on the challenges faced by CR programs.
6. Conclusions
Nurses agreed that CR was beneficial in enhancing targeted clinical outcomes. While a supervised hospital-based program was the ideal manner of CR delivery, there were only a few CR programs available. The scarcity of CR centers was a significant barrier to referring patients with HF.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board, reference number (REC-43/03/041).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available based on reasonable request from the corresponding author.
Conflicts of Interest
The author declares no conflict of interest.
References
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update from the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.H.; Jahan, S.A.; Kabir, E. A review of diseases associated with household air pollution due to the use of biomass fuels. J. Hazard. Mater. 2011, 192, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Khot, U.N.; Khot, M.B.; Bajzer, C.T.; Sapp, S.K.; Ohman, E.M.; Brener, S.J.; Ellis, S.G.; Lincoff, A.M.; Topol, E.J. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003, 290, 898–904. [Google Scholar] [CrossRef] [PubMed]
- Roger, V.L. Epidemiology of Heart Failure. Circ. Res. 2013, 113, 646–659. [Google Scholar] [CrossRef] [PubMed]
- Bragazzi, N.L.; Zhong, W.; Shu, J.; Abu, M.A.; Lotan, D.; Grupper, A.; Younis, A.; Dai, H. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. Eur. J. Prev. Cardiol. 2021, 28, 1682–1690. [Google Scholar] [CrossRef]
- Britz, J.A.; Dunn, K.S. Self-care and quality of life among patients with heart failure. J. Am. Acad. Nurse Pract. 2010, 22, 480–487. [Google Scholar] [CrossRef]
- Macchia, A.; Monte, S.; Romero, M.; D’Ettorre, A.; Tognoni, G. The prognostic influence of chronic obstructive pulmonary disease in patients hospitalised for chronic heart failure. Eur. J. Heart Fail. 2007, 9, 942–948. [Google Scholar] [CrossRef]
- AbuRuz, M.E.; Alaloul, F.; Saifan, A.; Masa’deh, R.; Abusalem, S. Quality of Life for Saudi Patients With Heart Failure: A Cross-Sectional Correlational Study. Glob. J. Health Sci. 2016, 8, 49. [Google Scholar] [CrossRef][Green Version]
- Alqahtani, J.S. Prevalence, incidence, morbidity and mortality rates of COPD in Saudi Arabia: Trends in burden of COPD from 1990 to 2019. PLoS ONE 2022, 17, e0268772. [Google Scholar] [CrossRef]
- Heo, S.; Lennie, T.A.; Okoli, C.; Moser, D.K. Quality of life in patients with heart failure: Ask the patients. Heart Lung 2009, 38, 100–108. [Google Scholar] [CrossRef]
- Redeker, N.S.; Conley, S.; Anderson, G.; Cline, J.; Andrews, L.; Mohsenin, V.; Jacoby, D.; Jeon, S. Effects of Cognitive Behavioral Therapy for Insomnia on Sleep, Symptoms, Stress, and Autonomic Function Among Patients With Heart Failure. Behav. Sleep Med. 2018, 18, 190–202. [Google Scholar] [CrossRef]
- Rice, H.; Say, R.; Betihavas, V. The effect of nurse-led education on hospitalisation, readmission, quality of life and cost in adults with heart failure. A systematic review. Patient Educ. Couns. 2018, 101, 363–374. [Google Scholar] [CrossRef]
- Bozkurt, B.; Fonarow, G.C.; Goldberg, L.R.; Guglin, M.; Josephson, R.A.; Forman, D.E.; Lin, G.; Lindenfeld, J.; O’Connor, C.; Panjrath, G.; et al. Cardiac Rehabilitation for Patients with Heart Failure. J. Am. Coll. Cardiol. 2021, 77, 1454–1469. [Google Scholar] [CrossRef]
- Heran, B.S.; Chen, J.M.; Ebrahim, S.; Moxham, T.; Oldridge, N.; Rees, K.; Thompson, D.R.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst. Rev. 2011, Cd001800. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Davos, C.; Francis, D.P.; Coats, A.J. Exercise training meta-analysis of trials in patients with chronic heart failure (ExTraMATCH). BMJ 2004, 328, 189. [Google Scholar] [CrossRef]
- Forman, D.E.; Sanderson, B.K.; Josephson, R.A.; Raikhelkar, J.; Bittner, V. American College of Cardiology’s Prevention of Cardiovascular Disease Section. Heart Failure as a Newly Approved Diagnosis for Cardiac Rehabilitation: Challenges and Opportunities. J. Am. Coll. Cardiol. 2015, 65, 2652–2659. [Google Scholar] [CrossRef]
- Piña, I.L.; Apstein, C.S.; Balady, G.J.; Belardinelli, R.; Chaitman, B.R.; Duscha, B.D.; Fletcher, B.J.; Fleg, J.L.; Myers, J.N.; Sullivan, M.J. American Heart Association Committee on exercise, rehabilitation, and prevention. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. Circulation 2003, 107, 1210–1225. [Google Scholar] [CrossRef]
- Shanks, L.C.; Moore, S.M.; Zeller, R.A. Predictors of cardiac rehabilitation initiation. Rehabil. Nurs. 2007, 32, 152–157. [Google Scholar] [CrossRef]
- Arena, R.; Williams, M.; Forman, D.E.; Cahalin, L.P.; Coke, L.; Myers, J.; Hamm, L.; Kris-Etherton, P.; Humphrey, R.; Bittner, V.; et al. Increasing referral and participation rates to outpatient cardiac rehabilitation: The valuable role of healthcare professionals in the inpatient and home health settings: A science advisory from the American Heart Association. Circulation 2012, 125, 1321–1329. [Google Scholar] [CrossRef]
- Rashed, M.; Theruvan, N.; Gad, A.; Shaheen, H. Cardiac Rehabilitation: Future of Heart Health in Saudi Arabia, a Perceptual View. World J. Cardiovasc. Dis. 2020, 10, 666–677. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alqahtani, J.S.; Alghamdi, S.M.; Alqarni, A.A.; Khormi, S.K.; Alwafi, H.; Samannodi, M.; Siraj, R.A.; Alhotye, M.; Naser, A.Y.; et al. Physicians’ Attitudes, Beliefs and Barriers to a Pulmonary Rehabilitation for COPD Patients in Saudi Arabia: A Cross-Sectional Study. Healthcare 2022, 10, 904. [Google Scholar] [CrossRef] [PubMed]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; Burri, H.; Butler, J.; Čelutkienė, J.; Chioncel, O.; et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2021, 42, 3599–3726. [Google Scholar] [PubMed]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2013, 62, e147–e239. [Google Scholar] [CrossRef]
- Long, L.; Mordi, I.R.; Bridges, C.; Sagar, V.A.; Davies, E.J.; Coats, A.J.; Dalal, H.; Rees, K.; Singh, S.J.; Taylor, R.S. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 2019, 2019, CD003331. [Google Scholar] [CrossRef] [PubMed]
- Taylor, R.S.; Long, L.; Mordi, I.R.; Madsen, M.T.; Davies, E.J.; Dalal, H.; Rees, K.; Singh, S.J.; Gluud, C.; Zwisler, A.D. Exercise-based rehabilitation for heart failure: Cochrane systematic review, meta-analysis, and trial sequential analysis. JACC Heart Fail. 2019, 7, 691–705. [Google Scholar] [CrossRef]
- Cao, Y.; Davidson, P.M.; DiGiacomo, M. Cardiovascular disease in China: An urgent need to enhance the nursing role to improve health outcomes. J. Clin. Nurs. 2009, 18, 687–693. [Google Scholar] [CrossRef]
- Fernandez, R.S.; Salamonson, Y.; Griffiths, R.; Juergens, C.; Davidson, P. Sociodemographic predictors and reasons for participation in an outpatient cardiac rehabilitation programme following percutaneous coronary intervention. Int. J. Nurs. Pract. 2008, 14, 237–242. [Google Scholar] [CrossRef]
- Kellar, G.; Hickey, G.W.; Goss, F.; Fertman, C.; Forman, D.E. Cardiac Rehabilitation Knowledge and Attitudes of Cardiology Fellows. J. Cardiopulm. Rehabil. Prev. 2021, 41, 30–34. [Google Scholar] [CrossRef]
- Krantz, M.J.; Havranek, E.P.; Mehler, P.S.; Haynes, D.K.; Long, C.S. Impact of a cardiac risk reduction program in vulnerable patients hospitalized with coronary artery disease. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2004, 24, 768–775. [Google Scholar] [CrossRef]
- Rassin, M. Nurses’ professional and personal values. Nurs. Ethics 2008, 15, 614–630. [Google Scholar] [CrossRef]
- McBride, C.M.; Emmons, K.M.; Lipkus, I.M. Understanding the potential of teachable moments: The case of smoking cessation. Health Educ. Res. 2003, 18, 156–170. [Google Scholar] [CrossRef]
- Gravely-Witte, S.; Leung, Y.W.; Nariani, R.; Tamim, H.; Oh, P.; Chan, V.M.; Grace, S.L. Effects of cardiac rehabilitation referral strategies on referral and enrollment rates. Nat. Rev. Cardiol. 2010, 7, 87–96. [Google Scholar] [CrossRef]
- Buttery, A.K.; Carr-White, G.; Martin, F.C.; Glaser, K.; Lowton, K. Limited availability of cardiac rehabilitation for heart failure patients in the United Kingdom: Findings from a national survey. Eur. J. Prev. Cardiol. 2014, 21, 928–940. [Google Scholar] [CrossRef]
- Taylor, R.S.; Dalal, H.M.; McDonagh, S.T.J. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat. Rev. Cardiol. 2022, 19, 180–194. [Google Scholar] [CrossRef]
- Strens, D.; Colle, A.; Vrijens, F.; Paulus, D.; Eyssen, M.; Van Brabandt, H.; Van Vlaenderen, I. Multidisciplinary outpatient rehabilitation following cardiac revascularization or valve surgery: Patient-related factors for uptake. Eur. J. Prev. Cardiol. 2013, 20, 422–430. [Google Scholar] [CrossRef]
- Elsakr, C.; Bulger, D.A.; Roman, S.; Kirolos, I.; Khouzam, R.N. Barriers physicians face when referring patients to cardiac rehabilitation: A narrative review. Ann. Transl. Med. 2019, 7, 414. [Google Scholar] [CrossRef]
- Turk-Adawi, K.I.; Terzic, C.; Bjarnason-Wehrens, B.; Grace, S.L. Cardiac rehabilitation in Canada and Arab countries: Comparing availability and program characteristics. BMC Health Serv. Res. 2015, 15, 521. [Google Scholar] [CrossRef]
- Turk-Adawi, K.; Sarrafzadegan, N.; Grace, S.L. Global availability of cardiac rehabilitation. Nat. Rev. Cardiol. 2014, 11, 586–596. [Google Scholar] [CrossRef]
- Zhu, H.; Ye, Z.; Ning, L.; Han, X.; Wu, Y. Knowledge and Attitude of the Medical Staff Concerning Cardiac Rehabilitation in Zhejiang Province, China: A Cross-Sectional Study. Patient Prefer. Adherence 2020, 14, 1771–1777. [Google Scholar] [CrossRef]
- Alsubaiei, M.E.; Cafarella, P.A.; Frith, P.A.; McEvoy, R.D.; Effing, T.W. Barriers for setting up a pulmonary rehabilitation program in the Eastern Province of Saudi Arabia. Ann. Thorac. Med. 2016, 11, 121. [Google Scholar] [CrossRef]
- Aldhahir, A.M.; Alghamdi, S.M.; Alqahtani, J.S.; Alqahtani, K.A.; Al Rajah, A.M.; Alkhathlan, B.S.; Singh, S.J.; Mandal, S.; Hurst, J.R. Pulmonary rehabilitation for COPD: A narrative review and call for further implementation in Saudi Arabia. Ann. Thorac. Med. 2021, 16, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Abu Hasheesh, M.O. Health care professionals’ awareness and knowledge of cardiac rehabilitation programs among cardiovascular disease patients in Al-Madinah, Saudi Arabia. Life Sci. J. 2014, 11, 911–917. [Google Scholar]
- Chindhy, S.; Taub, P.R.; Lavie, C.J.; Shen, J. Current challenges in cardiac rehabilitation: Strategies to overcome social factors and attendance barriers. Expert Rev. Cardiovasc. Ther. 2020, 18, 777–789. [Google Scholar] [CrossRef] [PubMed]
- Fini, A.; da Cruz, D.d.L.M. Characteristics of fatigue in heart failure patients: A literature review. Rev. Lat. Am. Enferm. 2009, 17, 557–565. [Google Scholar] [CrossRef][Green Version]
- Franzen, K.; Blomqvist, K.; Saveman, B.I. Impact of chronic heart failure on elderly persons’ daily life: A validation study. Eur. J. Cardiovasc. Nurs. 2006, 5, 137–145. [Google Scholar] [CrossRef]
- Marchionni, N.; Fattirolli, F.; Fumagalli, S.; Oldridge, N.; Del Lungo, F.; Morosi, L.; Burgisser, C.; Masotti, G. Improved exercise tolerance and quality of life with cardiac rehabilitation of older patients after myocardial infarction: Results of a randomized, controlled trial. Circulation 2003, 107, 2201–2206. [Google Scholar] [CrossRef]
- Klompstra, L.; Jaarsma, T.; Stromberg, A. Physical activity in patients with heart failure: Barriers and motivations with special focus on sex differences. Patient Prefer. Adherence 2015, 9, 1603–1610. [Google Scholar] [CrossRef]
- Lindwall, M.; Rennemark, M.; Halling, A.; Berglund, J.; Hassmén, P. Depression and exercise in elderly men and women: Findings from the Swedish national study on aging and care. J. Aging Phys. Act. 2007, 15, 41–55. [Google Scholar] [CrossRef]
- Tian, Y.; Deng, P.; Li, B.; Wang, J.; Li, J.; Huang, Y.; Zheng, Y. Treatment models of cardiac rehabilitation in patients with coronary heart disease and related factors affecting patient compliance. Rev. Cardiovasc. Med. 2019, 20, 27–33. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).