Are Implant-Supported Monolithic Zirconia Single Crowns a Viable Alternative to Metal-Ceramics? A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Data Extraction
2.5. Data Synthesis
2.6. Risk of Bias
2.7. Certainty of Evidence
3. Results
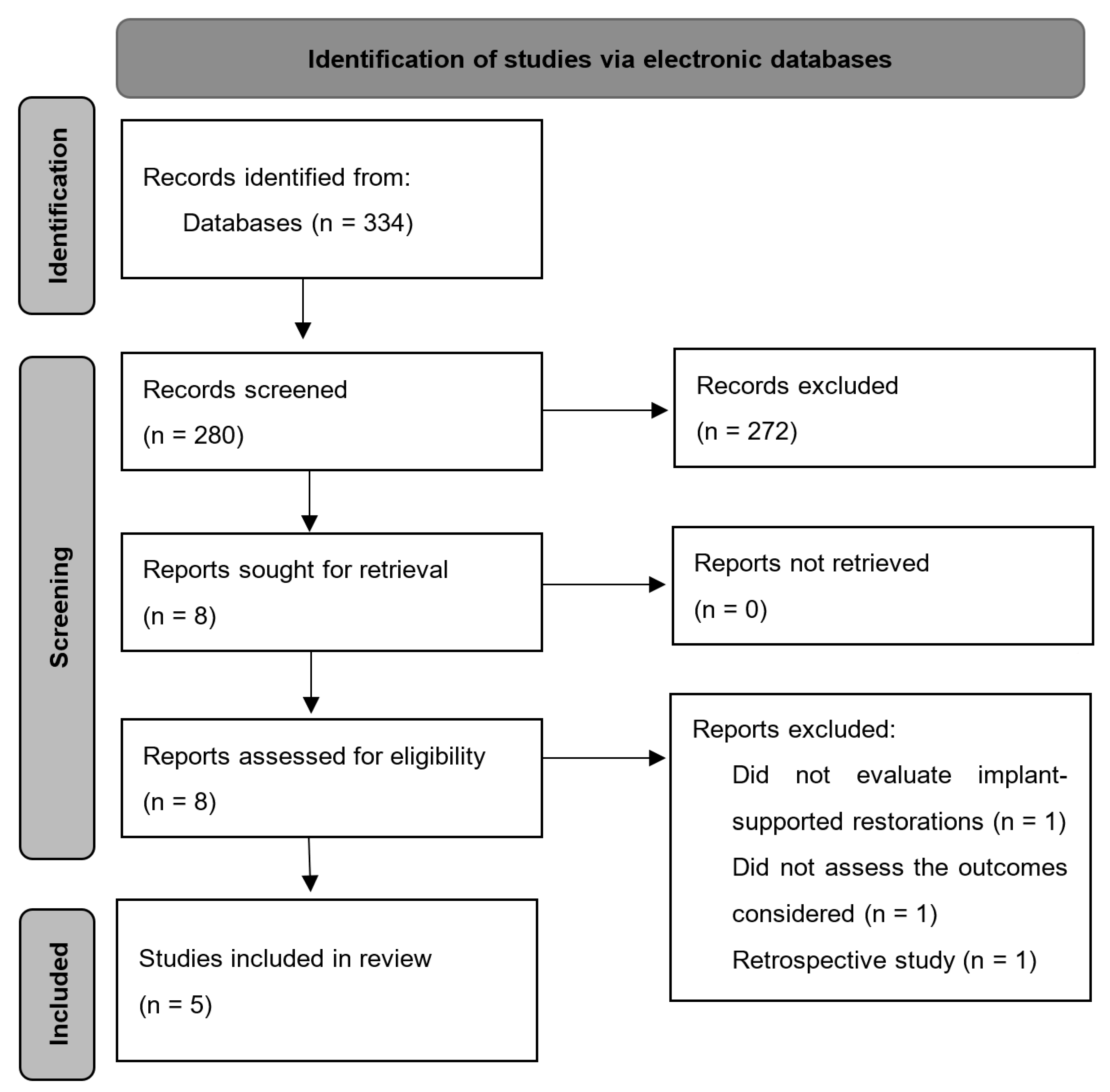
3.1. Study Selection
3.2. Characteristics of Included Studies
3.3. Meta-Analysis
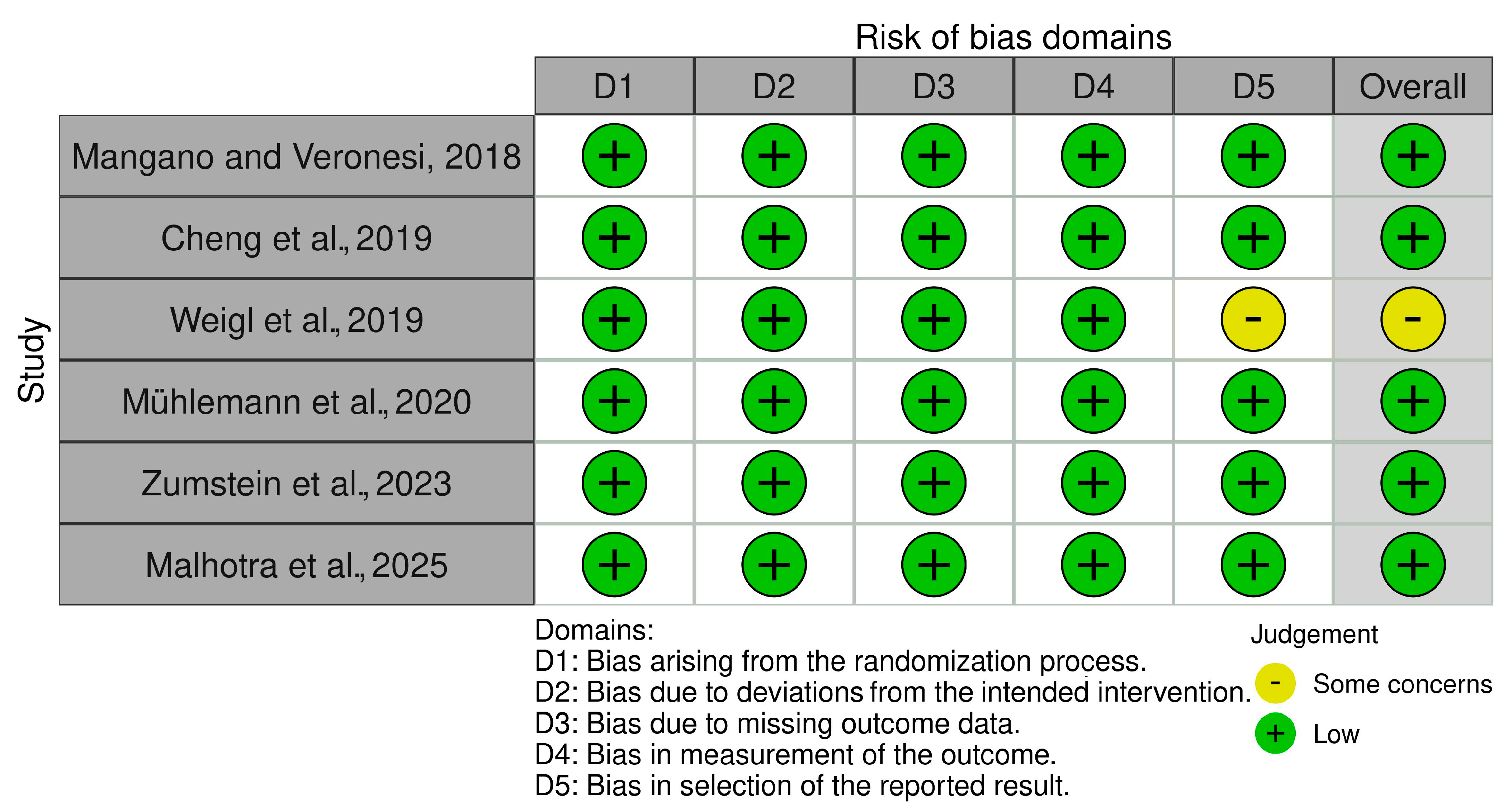
3.4. Risk of Bias
3.5. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Pjetursson, B.E.; Valente, N.A.; Strasding, M.; Zwahlen, M.; Liu, S.; Sailer, I. A systematic review of the survival and complication rates of zirconia-ceramic and metal-ceramic single crowns. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 199–214. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.A.A.; Verri, F.R.; de Luna Gomes, J.M.; Santiago Junior, J.F.; Miyashita, E.; Mendonca, G.; Pellizzer, E.P. Survival and prosthetic complications of monolithic ceramic implant-supported single crowns and fixed partial dentures: A systematic review with meta-analysis. J. Prosthet. Dent. 2024, 132, 1237–1249. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.T.; Li, J.Y.; Luo, X.; Feng, Y.; Gai, L.T.; He, F.M. Peri-implant marginal bone changes with implant-supported metal-ceramic or monolithic zirconia single crowns: A retrospective clinical study of 1 to 5 years. J. Prosthet. Dent. 2022, 128, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Weigl, P.; Saarepera, K.; Hinrikus, K.; Wu, Y.; Trimpou, G.; Lorenz, J. Screw-retained monolithic zirconia vs. cemented porcelain-fused-to-metal implant crowns: A prospective randomized clinical trial in split-mouth design. Clin. Oral Investig. 2019, 23, 1067–1075. [Google Scholar] [CrossRef]
- Lemos, C.A.A.; Verri, F.R.; Gomes, J.M.L.; de Souza Batista, V.E.; Cruz, R.S.; Oliveira, H.; Pellizzer, E.P. Ceramic versus metal-ceramic implant-supported prostheses: A systematic review and meta-analysis. J. Prosthet. Dent. 2019, 121, 879–886.e4. [Google Scholar] [CrossRef]
- Derksen, W.; Joda, T.; Chantler, J.; Fehmer, V.; Gallucci, G.O.; Gierthmuehlen, P.C.; Ioannidis, A.; Karasan, D.; Lanis, A.; Pala, K.; et al. Group 2 ITI Consensus Report: Technological developments in implant prosthetics. Clin. Oral Implant. Res. 2023, 34 (Suppl. S26), 104–111. [Google Scholar] [CrossRef] [PubMed]
- Pjetursson, B.E.; Sailer, I.; Merino-Higuera, E.; Spies, B.C.; Burkhardt, F.; Karasan, D. Systematic review evaluating the influence of the prosthetic material and prosthetic design on the clinical outcomes of implant-supported multi-unit fixed dental prosthesis in the posterior area. Clin. Oral Implant. Res. 2023, 34 (Suppl. S26), 86–103. [Google Scholar] [CrossRef]
- Pjetursson, B.E.; Fehmer, V.; Sailer, I. EAO Position Paper: Material Selection for Implant-Supported Restorations. Int. J. Prosthodont. 2022, 35, 7–16. [Google Scholar] [CrossRef]
- Mühlemann, S.; Kraus, R.D.; Hämmerle, C.H.F.; Thoma, D.S. Is the use of digital technologies for the fabrication of implant-supported reconstructions more efficient and/or more effective than conventional techniques: A systematic review. Clin. Oral Implant. Res. 2018, 29 (Suppl. S18), 184–195. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Phillips, A.N. Meta-analysis: Principles and procedures. BMJ 1997, 315, 1533–1537. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; DeBeer, H.; et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Batson, E.R.; Cooper, L.F.; Duqum, I.; Mendonça, G. Clinical outcomes of three different crown systems with CAD/CAM technology. J. Prosthet. Dent. 2014, 112, 770–777. [Google Scholar] [CrossRef]
- Alarcón-Sánchez, M.A.; Castro-Alarcón, N.; Sandoval-Guevara, D.; Vázquez-Villamar, M.; Fernández-Acosta, K.; Méndez-Gómez, M.Y.; Parra-Rojas, I.; Romero-Castro, N.S. Analysis of subgingival microbiota and IL-1β, TNF-α and CX3CL1 levels in gingival crevicular fluid of fixed dental prostheses. Dent. Mater. J. 2024, 43, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Mangano, F.; Veronesi, G. Digital versus Analog Procedures for the Prosthetic Restoration of Single Implants: A Randomized Controlled Trial with 1 Year of Follow-Up. Biomed. Res. Int. 2018, 2018, 5325032. [Google Scholar] [CrossRef]
- Cheng, C.W.; Chien, C.H.; Chen, C.J.; Papaspyridakos, P. Randomized Controlled Clinical Trial to Compare Posterior Implant-Supported Modified Monolithic Zirconia and Metal-Ceramic Single Crowns: One-Year Results. J. Prosthodont. 2019, 28, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Mühlemann, S.; Lakha, T.; Jung, R.E.; Hämmerle, C.H.F.; Benic, G.I. Prosthetic outcomes and clinical performance of CAD-CAM monolithic zirconia versus porcelain-fused-to-metal implant crowns in the molar region: 1-year results of a RCT. Clin. Oral Implant. Res. 2020, 31, 856–864. [Google Scholar] [CrossRef]
- Zumstein, K.; Waller, T.; Hämmerle, C.H.F.; Jung, R.E.; Benic, G.; Mühlemann, S. Clinical performance of monolithic zirconia crowns on titanium-zirconium reduced-diameter implants in the molar area: Interim data at three years of a randomized controlled trial. Clin. Oral Implant. Res. 2023, 34, 1354–1362. [Google Scholar] [CrossRef]
- Malhotra, T.; Kumar Yadav, B.; Singh Phukela, S.; Bhardwaj, A.; Khandait, M.; Nagpal, A.; Shetty, O. A Comparative Evaluation of Prosthetic and Biologic Outcomes as Influenced by Two Different Implant Restorative Materials: A Prospective, Split-Mouth Study. Int. J. Prosthodont. 2025, 38, 35–45. [Google Scholar]
- Zhang, Y.; Kelly, J.R. Dental Ceramics for Restoration and Metal Veneering. Dent. Clin. N. Am. 2017, 61, 797–819. [Google Scholar] [CrossRef]
- Lee, J.T.; Lee, H.J.; Park, S.Y.; Kim, H.Y.; Yeo, I.S. Consecutive unsplinted implant-supported restorations to replace lost multiple adjacent posterior teeth: A 4-year prospective cohort study. Acta Odontol. Scand. 2015, 73, 461–466. [Google Scholar] [CrossRef]
- Esquivel-Upshaw, J.F.; Clark, A.E.; Shuster, J.J.; Anusavice, K.J. Randomized clinical trial of implant-supported ceramic-ceramic and metal-ceramic fixed dental prostheses: Preliminary results. J. Prosthodont. 2014, 23, 73–82. [Google Scholar] [CrossRef]
- Lopez-Suarez, C.; Tobar, C.; Sola-Ruiz, M.F.; Pelaez, J.; Suarez, M.J. Effect of Thermomechanical and Static Loading on the Load to Fracture of Metal-Ceramic, Monolithic, and Veneered Zirconia Posterior Fixed Partial Dentures. J. Prosthodont. 2019, 28, 171–178. [Google Scholar] [CrossRef]
- López-Suárez, C.; Castillo-Oyagüe, R.; Rodríguez-Alonso, V.; Lynch, C.D.; Suárez-García, M.J. Fracture load of metal-ceramic, monolithic, and bi-layered zirconia-based posterior fixed dental prostheses after thermo-mechanical cycling. J. Dent. 2018, 73, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Coray, R.; Zeltner, M.; Ozcan, M. Fracture strength of implant abutments after fatigue testing: A systematic review and a meta-analysis. J. Mech. Behav. Biomed. Mater. 2016, 62, 333–346. [Google Scholar] [CrossRef]
- Mello, C.C.; Santiago Junior, J.F.; Lemos, C.A.A.; Galhano, G.A.; Evangelisti, E.; Scotti, R.; Verri, F.R.; Pellizzer, E.P. Evaluation of the accuracy and stress distribution of 3-unit implant supported prostheses obtained by different manufacturing methods. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 102, 66–74. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, V.V.M.; Fae, D.S.; Rosa, C.; Bento, V.A.A.; Lacerda, M.; Pellizzer, E.P.; Lemos, C.A.A. Is the clinical performance of internal conical connection better than internal non-conical connection for implant-supported restorations? A systematic review with meta-analysis of randomized controlled trials. J. Prosthodont. 2023, 32, 382–391. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.A.A.; Verri, F.R.; Noritomi, P.Y.; de Souza Batista, V.E.; Cruz, R.S.; de Luna Gomes, J.M.; de Oliveira Limírio, J.P.J.; Pellizzer, E.P. Biomechanical Evaluation of Different Implant-Abutment Connections, Retention Systems, and Restorative Materials in the Implant-Supported Single Crowns Using 3D Finite Element Analysis. J. Oral Implantol. 2022, 48, 194–201. [Google Scholar] [CrossRef]
- Santiago Junior, J.F.; Pellizzer, E.P.; Verri, F.R.; de Carvalho, P.S. Stress analysis in bone tissue around single implants with different diameters and veneering materials: A 3-D finite element study. Mater. Sci. Eng. C Mater. Biol. Appl. 2013, 33, 4700–4714. [Google Scholar] [CrossRef]
- Borges Radaelli, M.T.; Idogava, H.T.; Spazzin, A.O.; Noritomi, P.Y.; Boscato, N. Parafunctional loading and occlusal device on stress distribution around implants: A 3D finite element analysis. J. Prosthet. Dent. 2018, 120, 565–572. [Google Scholar] [CrossRef]
- de Luna Gomes, J.M.; Lemos, C.A.A.; Santiago Junior, J.F.; de Moraes, S.L.D.; Goiato, M.C.; Pellizzer, E.P. Optimal number of implants for complete-arch implant-supported prostheses with a follow-up of at least 5 years: A systematic review and meta-analysis. J. Prosthet. Dent. 2019, 121, 766–774.e3. [Google Scholar] [CrossRef] [PubMed]
- Lemos, C.A.; de Souza Batista, V.E.; Almeida, D.A.; Santiago Júnior, J.F.; Verri, F.R.; Pellizzer, E.P. Evaluation of cement-retained versus screw-retained implant-supported restorations for marginal bone loss: A systematic review and meta-analysis. J. Prosthet. Dent. 2016, 115, 419–427. [Google Scholar] [CrossRef] [PubMed]
- Canullo, L.; Pesce, P.; Patini, R.; Antonacci, D.; Tommasato, G. What Are the Effects of Different Abutment Morphologies on Peri-implant Hard and Soft Tissue Behavior? A Systematic Review and Meta-Analysis. Int. J. Prosthodont. 2020, 33, 297–306. [Google Scholar] [CrossRef]



| Author/Year | Pati-ents, n | Mean Age | Restora-tions, n | Region | Restorative Material | Implant System/Connection/Abutment/Fixation | Prosthetic Complications, n | Survival, n (%) | Peri-Implant Bone Loss (mm) | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|
| Mangano and Veronesi, 2018 [15] | 50 | 52.6 years | ML: 25 MC: 25 | Ant: 0 Post: 50 PM and M | ML: Monolithic Zirconia (Katana, Kuraray Noritake) MC: Custom titanium abutment + feldspathic porcelain. | Exacone, Cone Morse, Ti-Base, Cement-retained | ML: 1 CF MC: 0 | ML: 25 (100%) MC: 25 (100%) | ML: 0.39 ± 0.29 MC: 0.54 ± 0.32 | 1 year |
| Cheng et al., 2019 [16] | 40 | 47.8 yeas | ML: 36 MC: 34 | Ant: 0 Post: 70 PM and M | ML: Monolithic Zirconia (Ceramil zi or Ceramill Zolid; Amann Girrbach) MC: Custom Gold Abutment | Straumann, SynOcta Gold Abutment, Screw-retained | ML: 1 SL MC: 5 SL; 2 DB; 1 CF | ML: 34 (97.2%) MC: 34 (100%) | NA | 1 year |
| Weigl et al., 2019 [4] | 22 | 43 years | ML: 22 MC: 22 | Ant: 0 Post: 44 PM and M | ML: Monolithic Zirconia (NR) MC: Custom Gold + Felspathic | Ankylos, Internal connection, Ti-Base, ML: Screw-retained; MC: Cement-retained | ML: 1 SL; 2 RFSH MC: 2 CF; 2 DB | ML: 22 (100%) MC: 22 (100%) | ML: 0.78 ± 0.76 MC: 0.82 ± 0.74 | 1 year |
| Mühlemann et al., 2020 [17] | 76 | 57 years | ML: 39 MC: 37 | Ant: 0 Post: 76 M | ML: Monolithic Zirconia (Lava Plus, 3M ESPE) MC: Custom Gold + Feldspathic ceramic | Straumann, Regular Neck (RN), external connection, Ti-Base, Screw-retained | ML: 0 MC: 4 CF | ML: 38 (97.4%) MC: 36 (97.3%) | ML: −0.15 ± 0.76 MC: −0.33 ± 0.71 | 1 year |
| Zumstein et al., 2023 [18] | 59 | 55.4 years | ML: 32 MC: 27 | Ant: 0 Post: 59 M | ML: Monolithic Zirconia (Lava Plus, 3M ESPE) MC: Custom Gold + Feldspathic ceramic | Straumann, Regular Neck (RN), external connection, Ti-Base, Screw-retained | ML: 0 MC: 4 CF | ML: 27 (80%) MC: 24 (88.8%) | ML: −0.15 ± 0.21 MC: −0.10 ± 0.19 | 3 years |
| Malhotra et al., 2025 [19] | 20 | 18 to 40 years | ML: 20 MC: 20 | Ant: 0 Post: 40 M | ML: Monolithic Zirconia (4Y-PSZ; Zir-X Zirconia Block) MC: UCLA/Ni-Cr + Feldspathic ceramic | Internal Hexagon (Tri-lobe) connection, UCLA and Ti-Base, Screw-retained | ML: 2 AF; 2 SL MC: 4 CF; 8 AF; 7 SL | ML: 20 (100%) MC: 20 (100%) | ML: 1.79 ± 0.12 MC: 1.89 ± 0.21 | 2 years |
| Certainty Assessment | № of Patients | Effect | Certainty | ||||||||
| Number of studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Monolithic | Metal-Ceramic | Relative (95% CI) | Absolute (95% CI) | |
| Prosthetic Complications | |||||||||||
| 5 | randomized trials | not serious | not serious | not serious | very serious b | none | 9/162 (5.6%) | 39/158 (24.7%) | RR 0.26 (0.14 to 0.47) | 183 fewer per 1000 (from 212 fewer to 131 fewer) | ⨁⨁◯◯ Low |
| Implant Survival Rates | |||||||||||
| 5 | randomized trials | not serious | not serious | not serious | very serious b | none | 8/174 (4.6%) | 4/165 (2.4%) | RR 1.66 (0.56 to 4.94) | 16 more per 1000 (from 11 fewer to 96 more) | ⨁⨁◯◯ Low |
| Marginal Bone Loss | |||||||||||
| 4 | randomized trials | not serious | serious a | not serious | very serious b | none | 138 | 131 | - | MD 0.05 lower (0.11 lower to 0.02 higher) | ⨁◯◯◯ Very low |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Mota Fonseca, L.C.; Faé, D.S.; Fernandes, B.N.; da Costa, I.; Miranda, J.S.; Lemos, C.A.A. Are Implant-Supported Monolithic Zirconia Single Crowns a Viable Alternative to Metal-Ceramics? A Systematic Review and Meta-Analysis. Ceramics 2025, 8, 63. https://doi.org/10.3390/ceramics8020063
da Mota Fonseca LC, Faé DS, Fernandes BN, da Costa I, Miranda JS, Lemos CAA. Are Implant-Supported Monolithic Zirconia Single Crowns a Viable Alternative to Metal-Ceramics? A Systematic Review and Meta-Analysis. Ceramics. 2025; 8(2):63. https://doi.org/10.3390/ceramics8020063
Chicago/Turabian Styleda Mota Fonseca, Liandra Constantina, Daniele Sorgatto Faé, Beatriz Neves Fernandes, Izabela da Costa, Jean Soares Miranda, and Cleidiel Aparecido Araujo Lemos. 2025. "Are Implant-Supported Monolithic Zirconia Single Crowns a Viable Alternative to Metal-Ceramics? A Systematic Review and Meta-Analysis" Ceramics 8, no. 2: 63. https://doi.org/10.3390/ceramics8020063
APA Styleda Mota Fonseca, L. C., Faé, D. S., Fernandes, B. N., da Costa, I., Miranda, J. S., & Lemos, C. A. A. (2025). Are Implant-Supported Monolithic Zirconia Single Crowns a Viable Alternative to Metal-Ceramics? A Systematic Review and Meta-Analysis. Ceramics, 8(2), 63. https://doi.org/10.3390/ceramics8020063






