Development of a Mobile Health Monitoring and Alert Application for Agricultural Workers
Abstract
1. Introduction
1.1. Motivation and Objective
1.2. Literature Review
1.3. Contributions
- We propose a modular BLE sensor framework that is capable of efficiently managing multiple simultaneous connections from heterogeneous wearable sensors.
- The framework supports the inclusion of commercial sensor devices that often lack official API support.
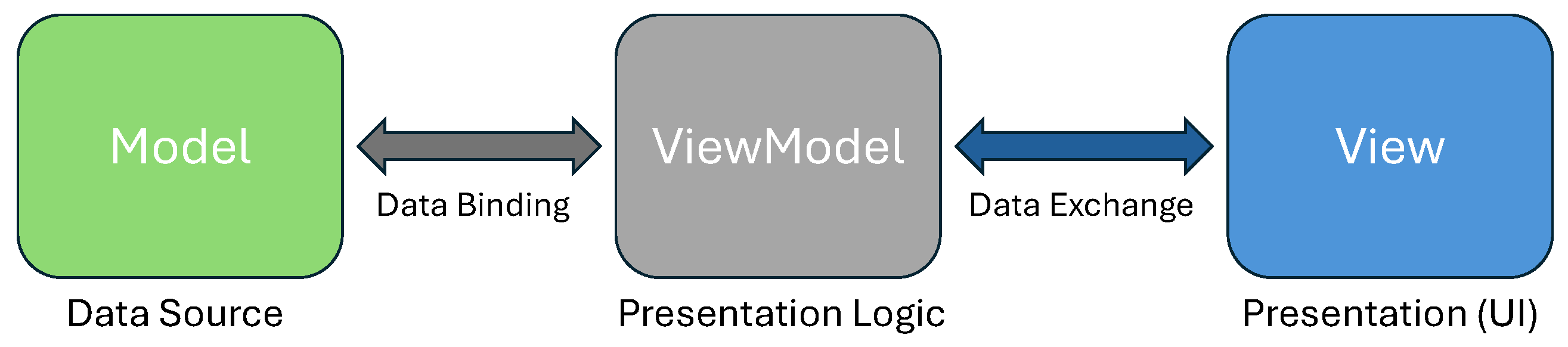
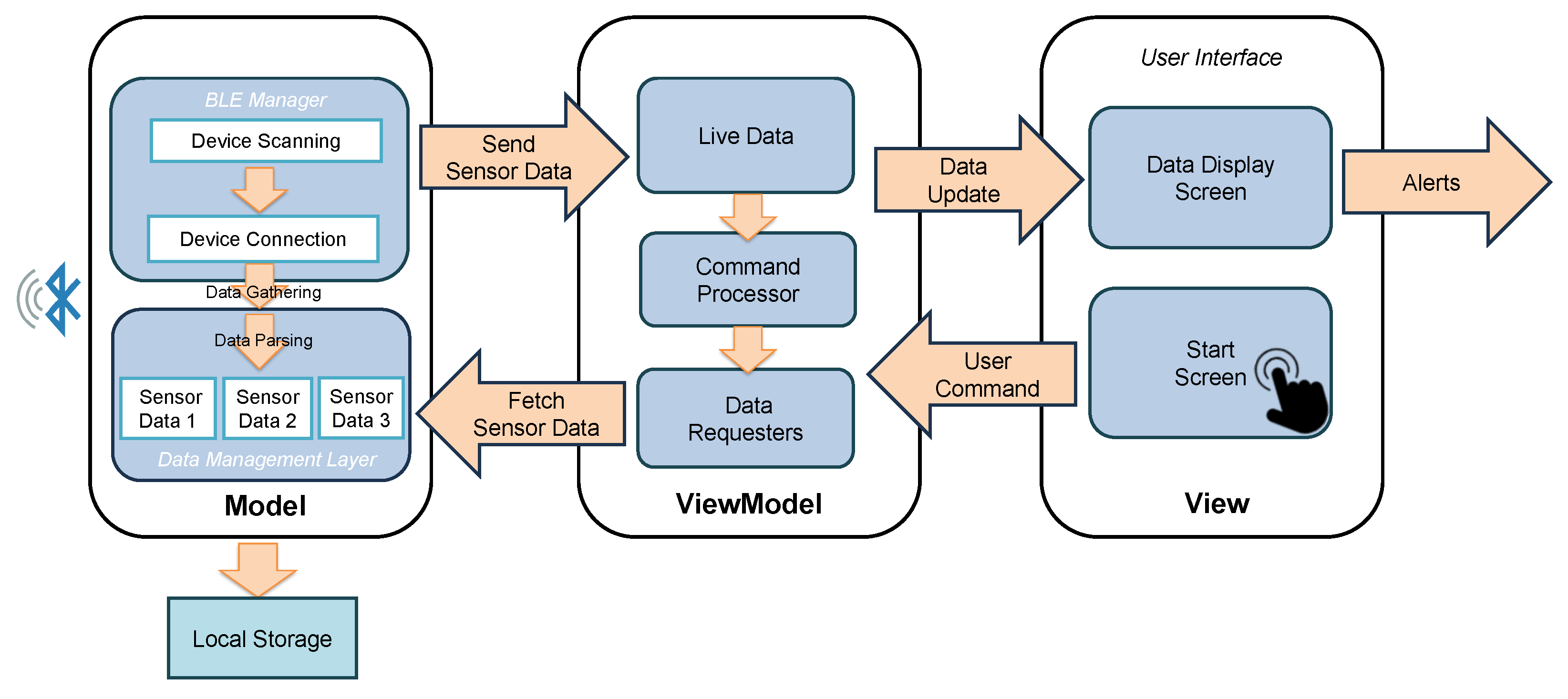
- We present a scalable Android application architecture based on the Model–View–ViewModel (MVVM), designed for ease of modification and implementation.
- We validate the developed system through experiments conducted under simulated conditions relevant to agriculture.
2. Background
2.1. Mobile Health
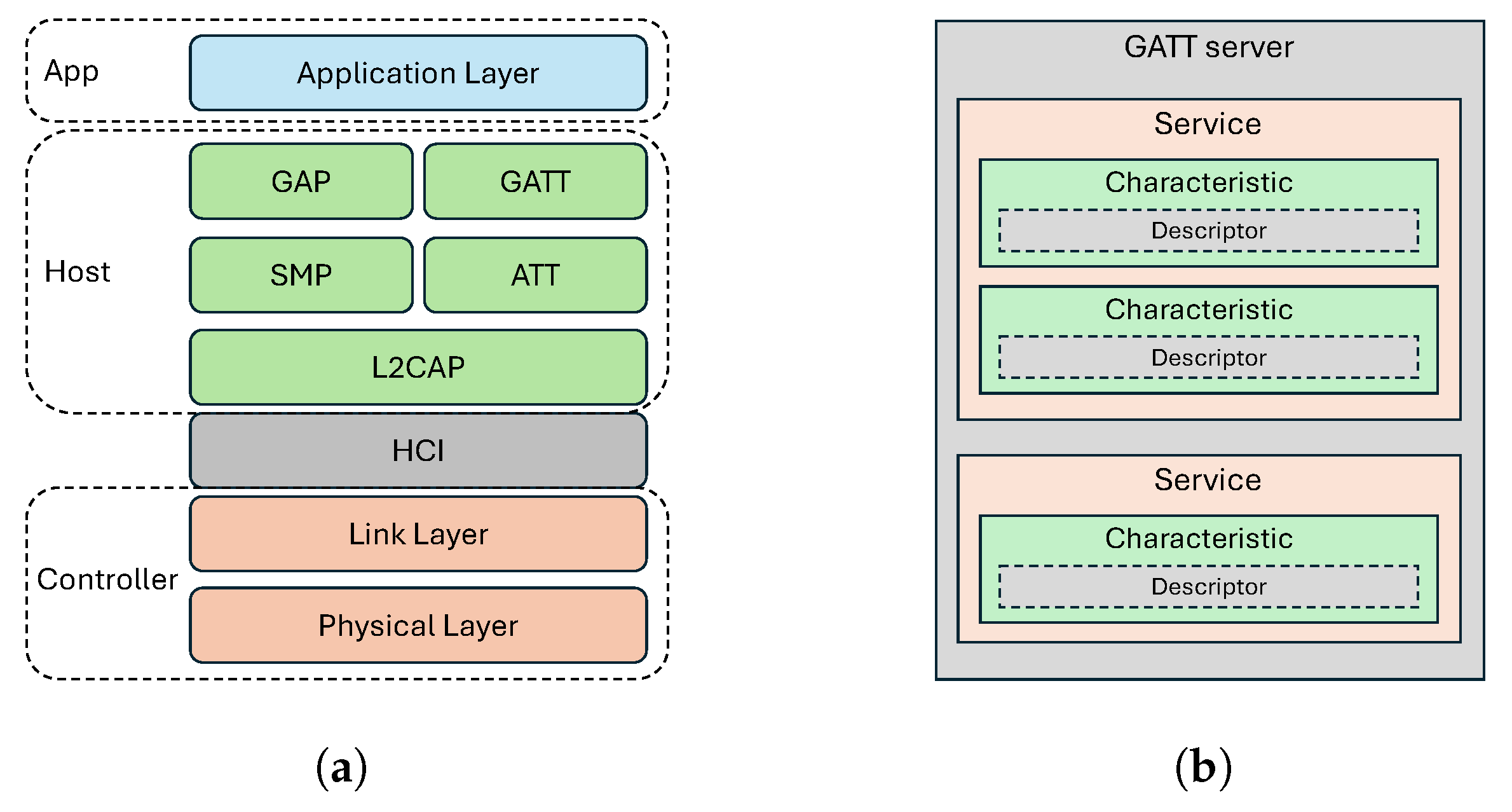
2.2. Wireless Communication: Bluetooth Low Energy (BLE)
2.3. Mobile Application Development
3. Methodology: Structure and Design
3.1. Wearable Sensor Selection
3.2. App Architecture Design
3.3. BLE Connection
3.4. Data Extraction and Processing
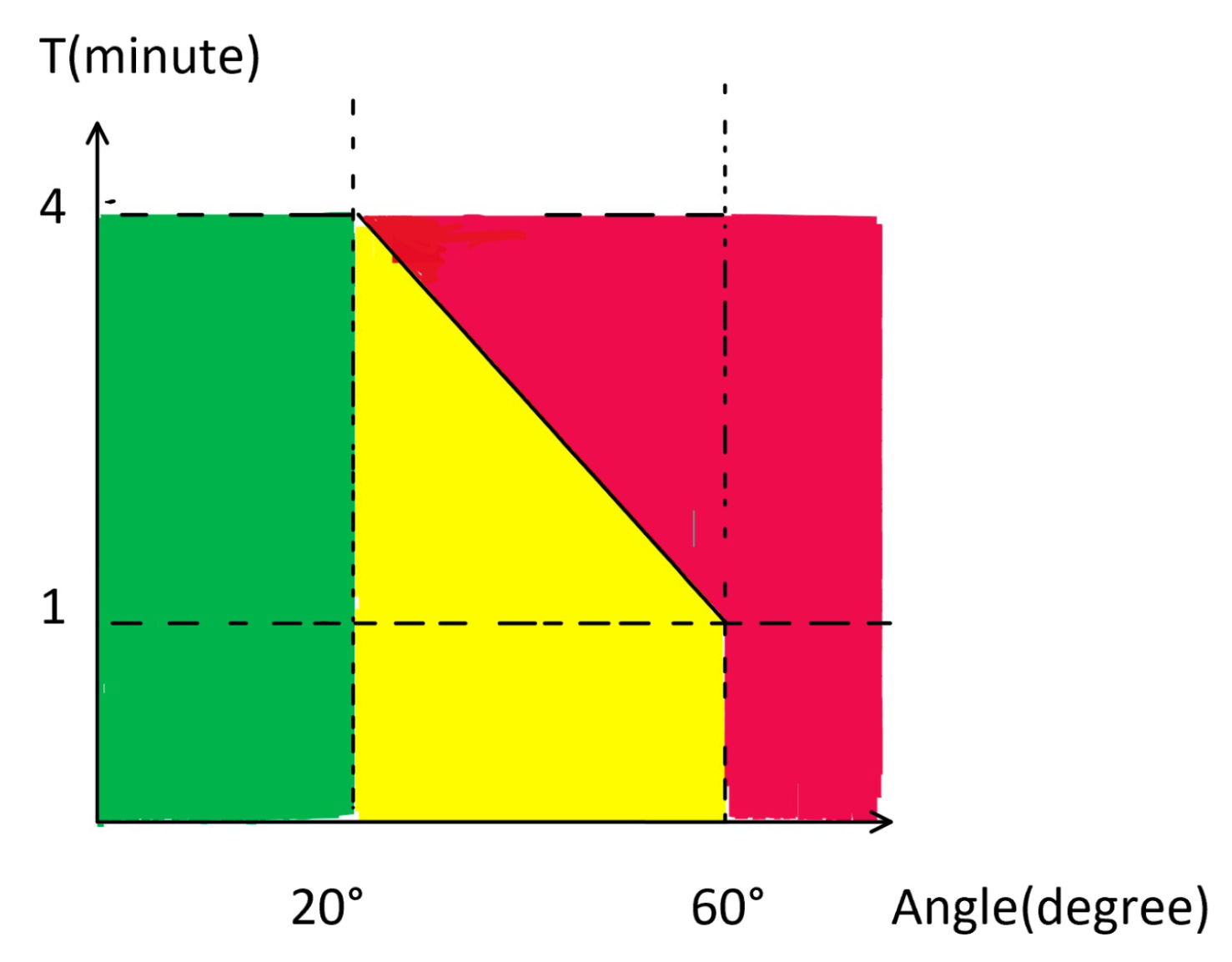
3.5. Alert Module Design
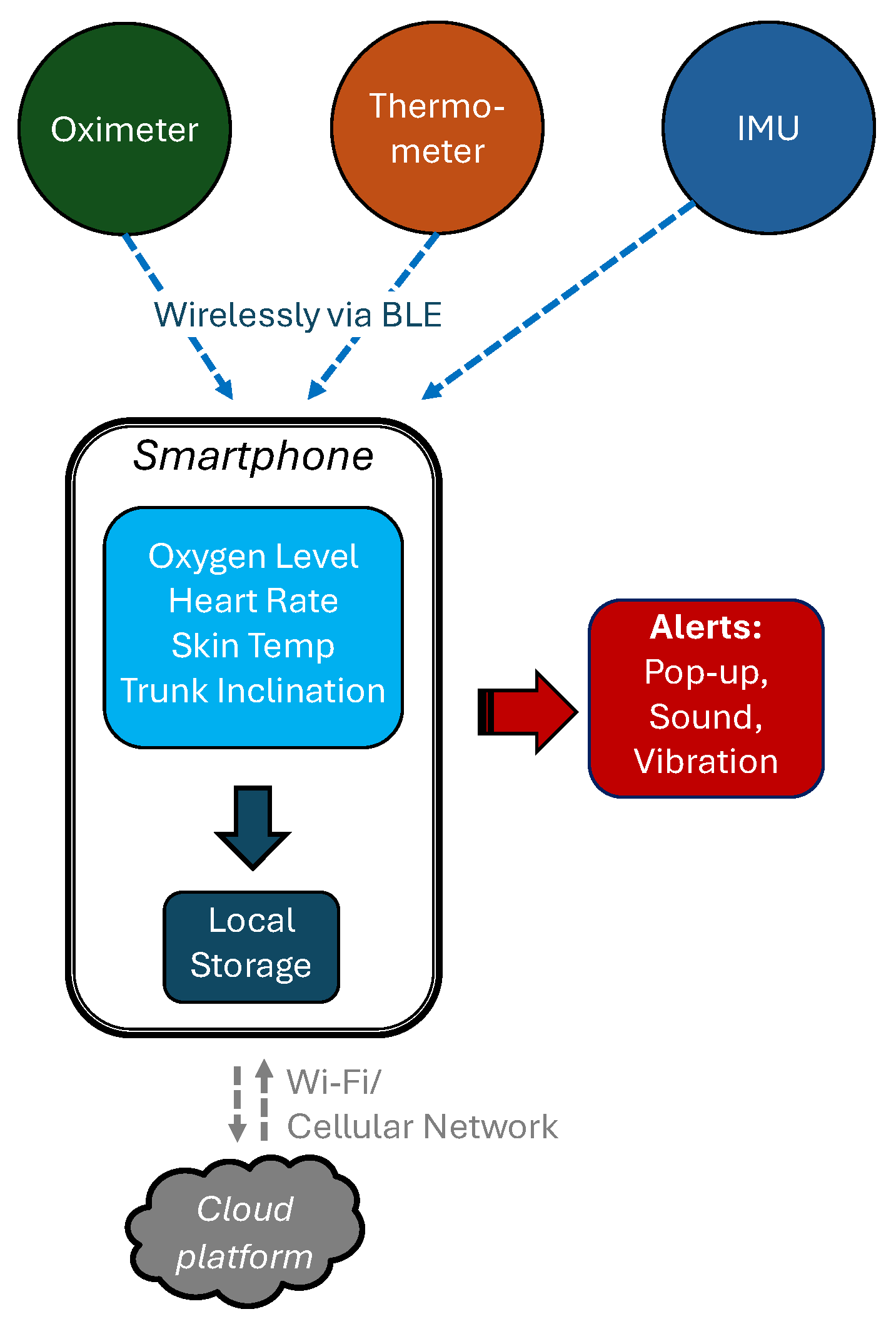
3.6. System Overview
4. Verification Experiments
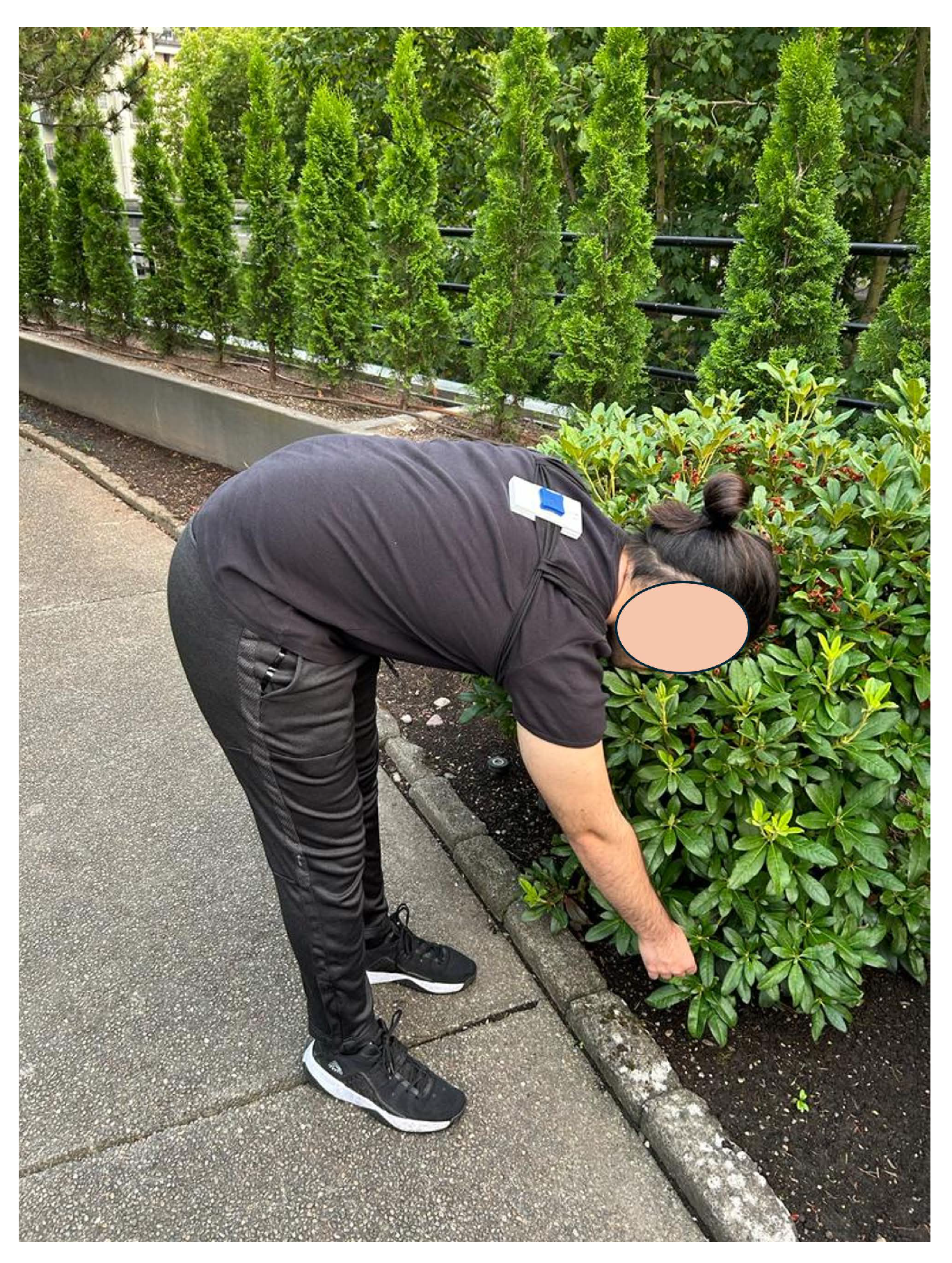
4.1. Experimental Setup and Procedure
- The participant wore the IMU belt, thermometer, and oximeter.
- The app was launched on the TCL smartphone via the Android Debug Bridge (ADB) for testing.
- The sensors began BLE advertising and were connected through the app’s start screen.
- Sensor readings were verified using the methods described earlier.
- The subject increased heart rate and bent the torso to test the alert mechanism.
- Alerts were checked for proper vibration, sound, and notifications.
- Reconnection reliability was tested by powering off or moving the devices out of the communication range.
- The phone’s local storage was checked to confirm proper data saving.
- The procedure was repeated with the second smartphone to verify consistency.
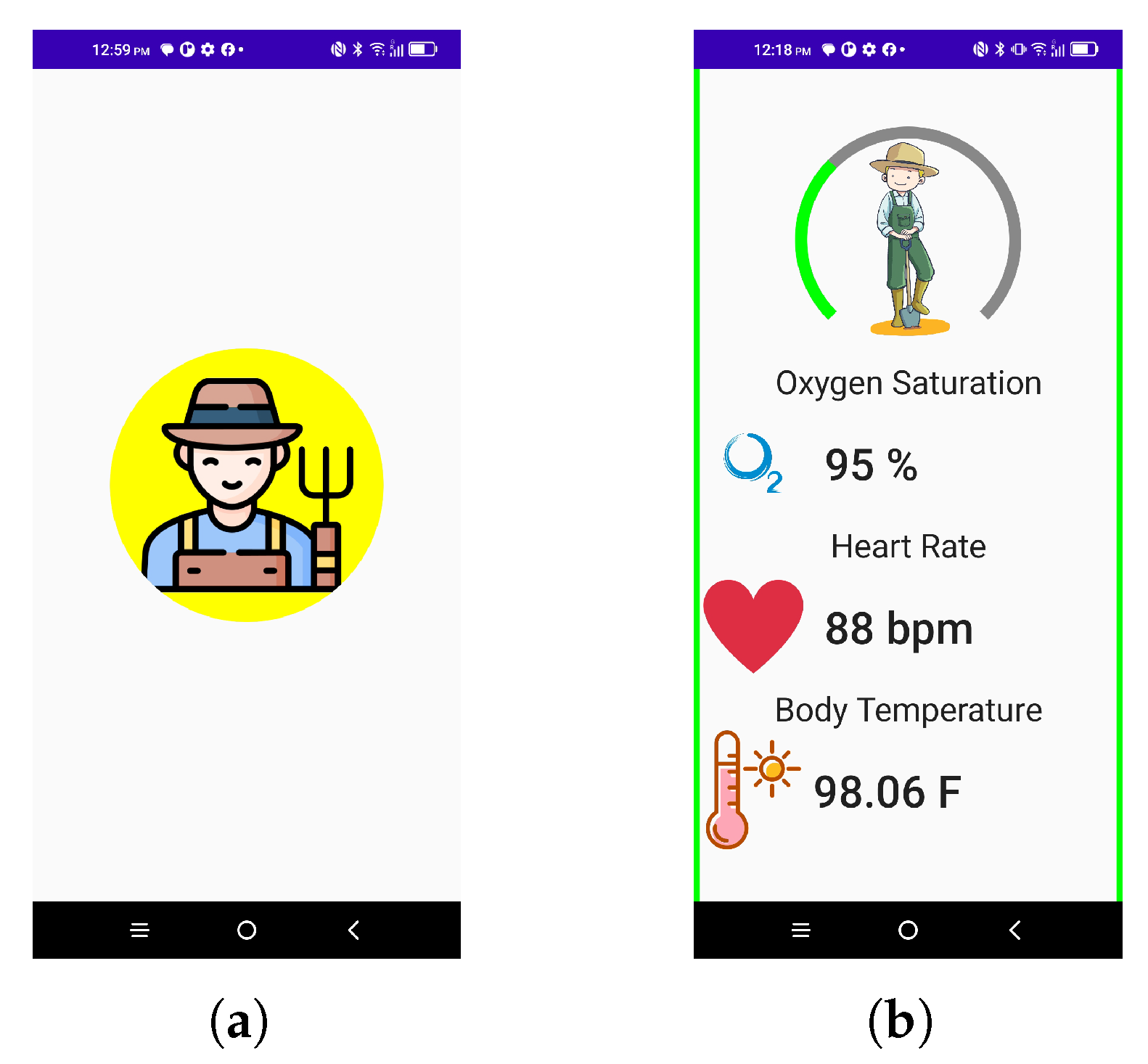
4.2. Data Monitoring via User Interface
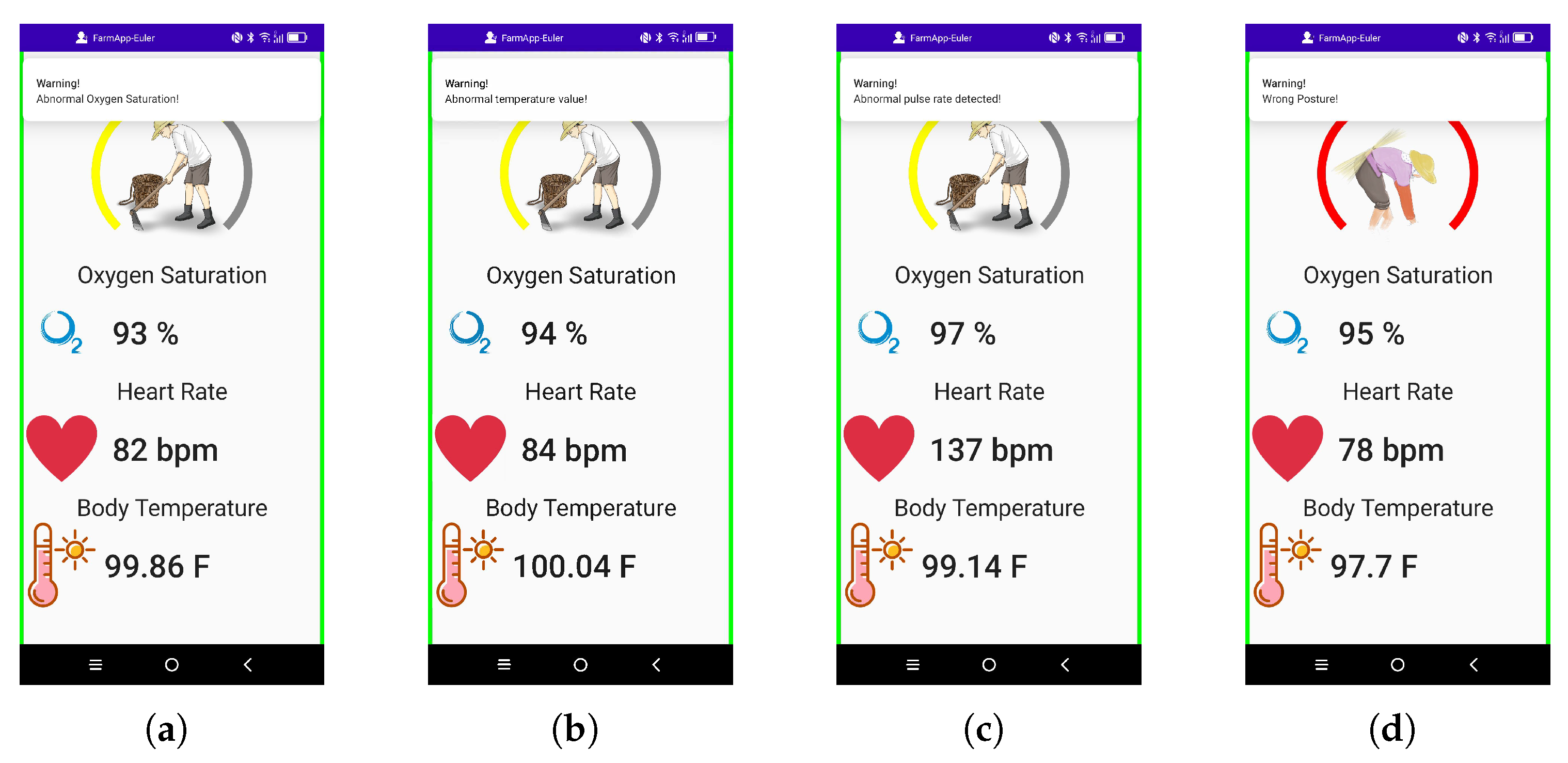
4.3. Alert Mechanism and Data Storage
5. Discussions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Walker-Bone, K.; Palmer, K.T. Musculoskeletal disorders in farmers and farm workers. Occup. Med. 2002, 52, 441–450. [Google Scholar] [CrossRef]
- Gubernot, D.M.; Anderson, G.B.; Hunting, K.L. The epidemiology of occupational heat exposure in the United States: A review of the literature and assessment of research needs in a changing climate. Int. J. Biometeorol. 2014, 58, 1779–1788. [Google Scholar] [CrossRef]
- Kim, Y.S.; Kim, J.; Chicas, R.; Xiuhtecutli, N.; Matthews, J.; Zavanelli, N.; Kwon, S.; Lee, S.H.; Hertzberg, V. Soft Wireless Bioelectronics Designed for Real-Time, Continuous Health Monitoring of Farmworkers. Adv. Healthc. Mater. 2022, 11, 2200170. [Google Scholar] [CrossRef]
- Valliappan, S.; Mohan, B.P.R.; Kumar, S.R. Design of low-cost, wearable remote health monitoring and alert system for elderly heart patients. In Proceedings of the 2017 International Conference on IoT and Application (ICIOT), Nagapattinam, India, 19–20 May 2017; pp. 1–7. [Google Scholar] [CrossRef]
- Yan, X.; Li, H.; Li, A.R.; Zhang, H. Wearable IMU-based real-time motion warning system for construction workers’ musculoskeletal disorders prevention. Autom. Constr. 2017, 74, 2–11. [Google Scholar] [CrossRef]
- Banos, O.; Villalonga, C.; García, R.; Saez, A.; Damas, M.; Holgado-Terriza, J.; Lee, S.; Pomares, H.; Rojas, I. Design, implementation and validation of a novel open framework for agile development of mobile health applications. BioMedical Eng. OnLine 2015, 14, S6. [Google Scholar] [CrossRef] [PubMed]
- Yadav, S.; Pulekar, T.V.; Cheeran, A.; Awandekar, V.D. Wireless Emergency Patient Monitoring System. In Proceedings of the 2018 Fourth International Conference on Biosignals, Images and Instrumentation (ICBSII), Chennai, India, 22–24 March 2018; pp. 206–212. [Google Scholar] [CrossRef]
- Singh, N.K.; Ricke, D.O. Towards an open data framework for body sensor networks supporting bluetooth low energy. In Proceedings of the 2016 IEEE 13th International Conference on Wearable and Implantable Body Sensor Networks (BSN), San Francisco, CA, USA, 14–17 June 2016; pp. 396–401. [Google Scholar] [CrossRef]
- Vishwakarma, P.K.; Singh, R. A–Review on IoT-Assisted ECG Monitoring Framework for Health Care Applications. In Proceedings of the 2021 Fourth International Conference on Computational Intelligence and Communication Technologies (CCICT), Sonepat, India, 3 July 2021; pp. 203–207. [Google Scholar] [CrossRef]
- Petropoulos, A.; Sikeridis, D.; Antonakopoulos, T. Wearable Smart Health Advisors: An IMU-Enabled Posture Monitor. IEEE Consum. Electron. Mag. 2020, 9, 20–27. [Google Scholar] [CrossRef]
- Umapathy, K.; Chandramohan, S.; Muthukumaran, D.; Sivakumar, M.; Vinoth, M.; Selvakumar, S. Edge and Android Application based Health Monitor. In Proceedings of the 2023 5th International Conference on Smart Systems and Inventive Technology (ICSSIT), Tirunelveli, India, 23–25 January 2023; pp. 32–34. [Google Scholar] [CrossRef]
- Mahmud, M.S.; Wang, H.; Esfar-E-Alam, A.M.; Fang, H. A Wireless Health Monitoring System Using Mobile Phone Accessories. IEEE Internet Things J. 2017, 4, 2009–2018. [Google Scholar] [CrossRef]
- Taylor, S.A.; Sharif, H. Wearable Patient Monitoring Application (ECG) using Wireless Sensor Networks. In Proceedings of the 2006 International Conference of the IEEE Engineering in Medicine and Biology Society, New York, NY, USA, 30 August–3 September 2006; pp. 5977–5980. [Google Scholar] [CrossRef]
- Ali, S.M.; Noghanian, S.; Khan, Z.U.; Alzahrani, S.; Alharbi, S.; Alhartomi, M.; Alsulami, R. Wearable and Flexible Sensor Devices: Recent Advances in Designs, Fabrication Methods, and Applications. Sensors 2025, 25, 1377. [Google Scholar] [CrossRef]
- Tao, D.; Xie, C.; Jaffrezic-Renault, N.; Guo, Z. Flexible and wearable electrochemical sensors for health and safety monitoring. Talanta 2025, 291, 127863. [Google Scholar] [CrossRef]
- Dai, B.; Gao, C.; Xie, Y. Flexible wearable devices for intelligent health monitoring. View 2022, 3, 20220027. [Google Scholar] [CrossRef]
- Huang, G.; Chen, X.; Liao, C. AI-Driven Wearable Bioelectronics in Digital Healthcare. Biosensors 2025, 15, 410. [Google Scholar] [CrossRef]
- Donisi, L.; Cesarelli, G.; Pisani, N.; Ponsiglione, A.M.; Ricciardi, C.; Capodaglio, E. Wearable Sensors and Artificial Intelligence for Physical Ergonomics: A Systematic Review of Literature. Diagnostics 2022, 12, 3048. [Google Scholar] [CrossRef]
- Kumar, S.; Nilsen, W.; Pavel, M.; Srivastava, M. Mobile Health: Revolutionizing Healthcare Through Transdisciplinary Research. Computer 2013, 46, 28–35. [Google Scholar] [CrossRef]
- Bangash, J.I.; Abdullah, A.H.; Anisi, M.H.; Khan, A.W. A survey of routing protocols in wireless body sensor networks. Sensors 2014, 14, 1322–1357. [Google Scholar] [CrossRef] [PubMed]
- Hajar, M.S.; Al-Kadri, M.O.; Kalutarage, H.K. A survey on wireless body area networks: Architecture, security challenges and research opportunities. Comput. Secur. 2021, 104, 102211. [Google Scholar] [CrossRef]
- Abdulmalek, S.; Nasir, A.; Jabbar, W.A.; Almuhaya, M.A.M.; Bairagi, A.K.; Khan, M.A.; Kee, S.H. IoT-Based Healthcare-Monitoring System towards Improving Quality of Life: A Review. Healthcare 2022, 10, 1993. [Google Scholar] [CrossRef] [PubMed]
- Townsend, K.; Cufi Akiba, C.; Davidson, R. Getting Started with Bluetooth Low Energy: Tools and Techniques for Low-Power Networking; O’Reilly: Sebastopol, CA, USA, 2014; p. 33. [Google Scholar]
- Heydon, R. Bluetooth Low Energy; Pearson: Upper Saddle River, NJ, USA, 2012; pp. 38–48. [Google Scholar]
- Llorens-Vernet, P.; Miró, J. Standards for Mobile Health–Related Apps: Systematic Review and Development of a Guide. JMIR MHealth UHealth 2020, 8, e13057. [Google Scholar] [CrossRef] [PubMed]
- Radhakrishnan, M.; Misra, A.; Balan, R.K.; Lee, Y. Smartphones and BLE Services: Empirical Insights. In Proceedings of the 2015 IEEE 12th International Conference on Mobile Ad Hoc and Sensor Systems, Dallas, TX, USA, 19–22 October 2015; pp. 226–234. [Google Scholar] [CrossRef]
- Android Studio & App Tools, Google for Developers. Available online: https://developer.android.com/studio (accessed on 20 July 2025).
- Anderson, C. The Model-View-ViewModel (MVVM) Design Pattern. In Pro Business Applications with Silverlight 5; Apress: Berkeley, CA, USA, 2012; pp. 461–499. [Google Scholar]
- LightBlue, Punch Through Design. Available online: https://punchthrough.com/lightblue-features/ (accessed on 20 July 2025).
- Jubran, A. Pulse oximetry. Crit. Care 2015, 19, R11. [Google Scholar] [CrossRef]
- Geneva, I.I.; Cuzzo, B.; Fazili, T.; Javaid, W. Normal Body Temperature: A Systematic Review. Open Forum Infect. Dis. 2019, 6, ofz032. [Google Scholar] [CrossRef]
- Spodick, D.H. Normal sinus heart rate: Appropriate rate thresholds for sinus tachycardia and bradycardia. South. Med. J. 1996, 89, 666–667. [Google Scholar] [CrossRef]
- ISO-11226:2000; Ergonomics—Evaluation of Static Working Postures. Technical Report; International Organization for Standardization: Geneva, Switzerland, 2006.
- Alam, U.K.; Ryu, J.C.; Kim, J.H. IMU-based estimation of body posture: Laboratory validation in simulated commercial fishing. Int. J. Ind. Ergon. 2025, 106, 103712. [Google Scholar] [CrossRef]
- Logcat Command-Line Tool, Google for Developers. Available online: https://developer.android.com/tools/logcat (accessed on 20 July 2025).

| Byte No. | Data (in Hex) | Description |
|---|---|---|
| 0 | 3A | Packet start |
| 1 | 01 | OpenMAT ID LSB (ID = 1) |
| 2 | 00 | OpenMAT ID MSB |
| 3 | 09 | Command no. LSB |
| 4 | 00 | Command no. MSB |
| 5 | 34 | Data length LSB (56 bytes) |
| 6 | 00 | Data length MSB |
| 7–10 | 5F 37 2A 00 | Timestamp |
| 11–14 | CD CC 4C 3F | Euler data x-axis |
| 15–18 | 66 66 86 3A | Euler data y-axis |
| 19–22 | 9A 99 99 3D | Euler data z-axis |
| ⋮ | ⋮ | ⋮ |
| 63 | 12 | Check sum LSB |
| 64 | 34 | Check sum MSB |
| 65 | 0A | Message end byte 2 |
| 66 | 0D | Message end byte 1 |
| Time (s) | Walnut Temperature (F) | Koogeek Temperature (F) | Difference |
|---|---|---|---|
| 0 | 97.52 | 97.70 | 0.18 |
| 20 | 97.52 | 97.70 | 0.18 |
| 40 | 97.70 | 97.70 | 0.00 |
| 60 | 97.70 | 97.70 | 0.00 |
| 80 | 97.70 | 97.88 | 0.18 |
| 100 | 97.70 | 97.88 | 0.18 |
| Time (s) | Body Temperature (°F) | Oxygen Saturation (%) | Heart Rate (bpm) | Trunk Inclination (deg) |
|---|---|---|---|---|
| 10.354 | 97.52 | 97 | 94 | 48.33 |
| 10.446 | 97.52 | 97 | 94 | 47.78 |
| 10.583 | 97.52 | 97 | 94 | 46.64 |
| 10.661 | 97.52 | 96 | 95 | 46.23 |
| 10.759 | 97.52 | 96 | 95 | 46.70 |
| 10.849 | 97.52 | 96 | 95 | 48.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the International Institute of Knowledge Innovation and Invention. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oztoprak, O.; Ryu, J.-C. Development of a Mobile Health Monitoring and Alert Application for Agricultural Workers. Appl. Syst. Innov. 2025, 8, 133. https://doi.org/10.3390/asi8050133
Oztoprak O, Ryu J-C. Development of a Mobile Health Monitoring and Alert Application for Agricultural Workers. Applied System Innovation. 2025; 8(5):133. https://doi.org/10.3390/asi8050133
Chicago/Turabian StyleOztoprak, Omer, and Ji-Chul Ryu. 2025. "Development of a Mobile Health Monitoring and Alert Application for Agricultural Workers" Applied System Innovation 8, no. 5: 133. https://doi.org/10.3390/asi8050133
APA StyleOztoprak, O., & Ryu, J.-C. (2025). Development of a Mobile Health Monitoring and Alert Application for Agricultural Workers. Applied System Innovation, 8(5), 133. https://doi.org/10.3390/asi8050133





