Abstract
Objectives We aimed to describe the epidemiology and clinical characteristics of urogenital tuberculosis (UGTB) in Sabah, Malaysia. Methods We performed a retrospective, descriptive study based on medical records of UGTB cases identified between January 1, 2014, and November 30, 2020. Results We identified 131 cases of UGTB in Sabah. Patient gender was balanced except for a mild male predominance in the 35 to 44 age group. No cases were reported in children. The majority of the patients (96%) were diagnosed in the government facility. Among the UGTB cases, 72% of patients were from rural areas, and 29% were illiterate. The commonest presentation was frequency of micturition (28%), followed by abdominal pain (26%) and loss of appetite (26%). The common sites included renal (32%) and scrotal (25%). Diagnosis was achieved via histopathology in 39.7% of patients and smear microscopy in 35.9%. Anti-tubercular treatment duration was 8.6 (±SD 4.0) months, and 81% of patients have completed treatment. A total of 50.4% of patients had received surgical intervention; 10.7% had undergone incision and drainage, 9.9% had cystoscopy, and 6.9% underwent orchidectomy. Conclusion UGTB has varied non-specific symptoms, which poses a diagnostic challenge, leading to morbidity. Ensuring awareness via widespread education within government and private health care, along with rural outreach programs, will contribute to early recognition and treatment.
1. Introduction
Tuberculosis (TB) is an ancient disease that constitutes a global epidemic. It is caused by Mycobacterium tuberculosis, which was discovered by Robert Koch in 1882. Genomic analyses suggest that M. tuberculosis co-evolved with humans. Its early progenitor, Mycobacterium prototuberculosis, possibly infected early hominids more than 3 million years ago [1,2].
According to the WHO Global Report 2019, around 10 million people fall ill with TB each year. TB is one of the top 10 causes of death, and the leading cause from a single infectious agent (Mycobacterium tuberculosis), ranking above HIV/AIDS. Of the 10 million annual cases, 5% to 45% have features of extrapulmonary TB [3].
In the early 1940s and 1950s, TB was the main cause of death in Malaysia. Realizing its significance, the Malaysian government launched its National TB Control Program in 1961. In 2014, 92.2% of TB cases were in Malaysian citizens. The incidence of TB in Malaysia as of 2019 is 92 per 100 000, with various sources indicating that Sabah has the highest number of TB cases in Malaysia [1,4].
Urogenital tuberculosis (UGTB) is the third most common form of extrapulmonary TB. It occurs in 2% to 20% of individuals with pulmonary TB. UGTB affects 2 males for each female, with a mean patient age of 40 years (range 5 to 90 years) [5,6,7].
Pathogenesis of UGTB is mainly from hematogenous spread and, rarely, venereal transmission.
UGTB is often overlooked because of its non-specific symptoms, lack of awareness, and lack of foolproof diagnostic tests. Delay in diagnosis often results in irreversible organ damage and renal failure. The most common symptom, found in more than 50% of patients, is irritative voiding. The other symptoms of UGTB are fever, weight loss, anorexia, backache, and abdominal pain [8].
In this study, we aim to delineate the epidemiology and clinical characteristics of UGTB in Sabah, Malaysia.
2. Materials and Methods
We conducted a retrospective, descriptive, sub-state analysis of all notified cases of UGTB disease in Sabah State, Malaysia between January 1, 2014, and November 30, 2020. All confirmed TB cases in Sabah are recorded in “myTB,” a secure electronic database.
Using national notification data, we calculated the proportion of all cases in Malaysia occurring in Sabah State. Descriptive analysis of demographic, epidemiological, and clinical data was done using SPSS software (version 26). The categorical variables were analyzed through the study of frequencies. Maps were produced using Paintmaps.
This study was conducted in compliance with ethical principles outlined in the Declaration of Helsinki and Malaysian Good Clinical Practice Guideline.
3. Results
In the relevant time period, 35,157 TB cases were reported to the Sabah State TB surveillance database (myTB). Out of this number, 31,070 were pulmonary TB and the remining 4087 cases were extrapulmonary TB (EPTB). UGTB accounted for 131 cases, which represents 3.2% of EPTB cases (January 1, 2014, to November 30, 2020).
3.1. Patient Demographics
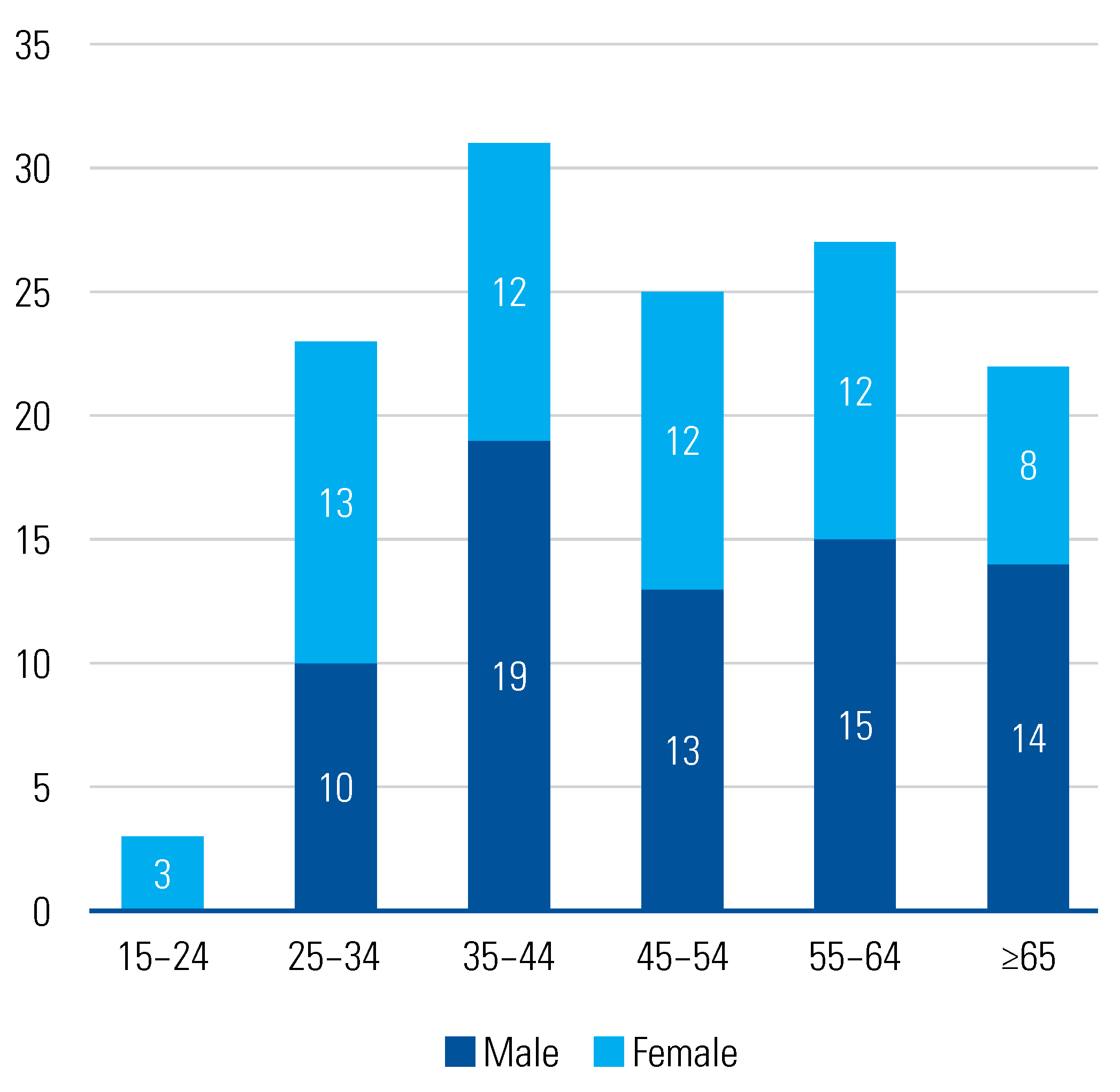
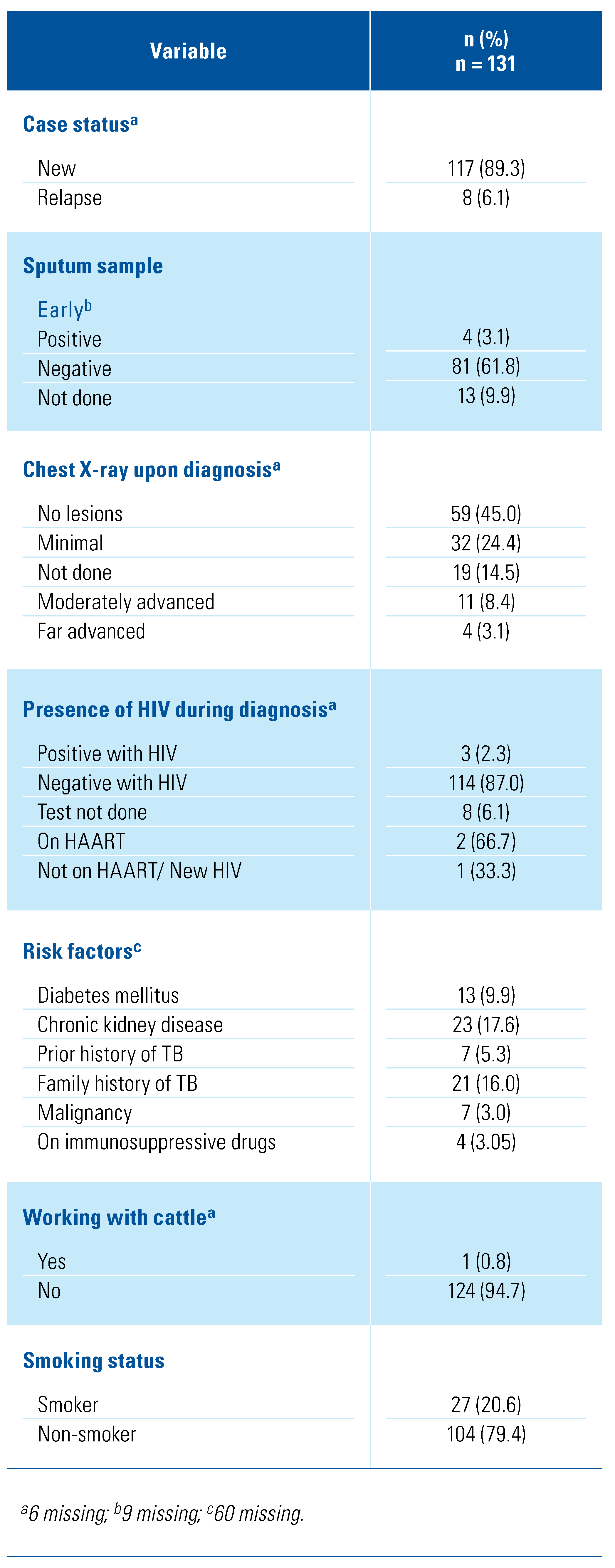
The patient demographics are summarized in Table 1. The number of patients remained fairly constant over time, with a minor peak in 2019. The mean patient age at diagnosis was 48.6 (SD: 15.0) years and patient gender was balanced except for a mild male predominance in the 35 to 44 age group (Figure 1).

Table 1.
Patient demographics.
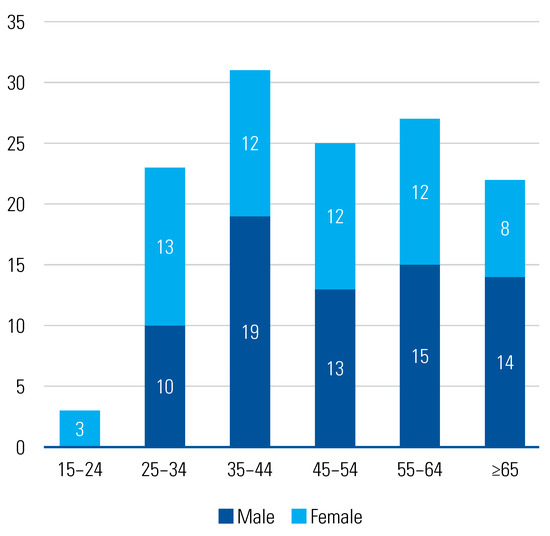
Figure 1.
Number of GUTB cases by age group and sex, 2014 to 2020.
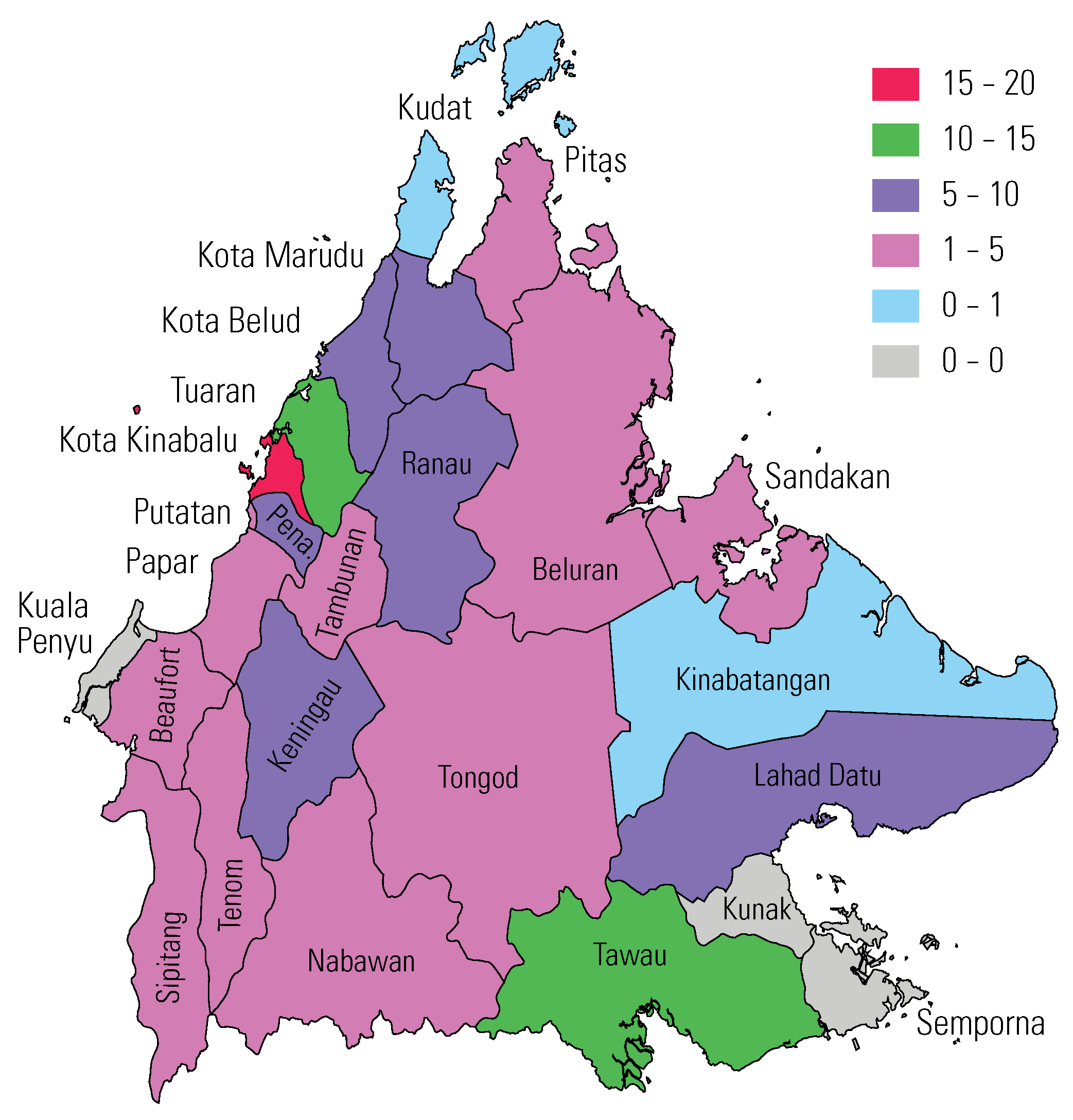
The highest number of cases was reported in Kota Kinabalu (14.0%), the state capital, which has the largest population, and the lowest number was reported from Kudat and Kinabatangan, which are both remote rural regions (Figure 2). The majority (81.7%) of patients were seen in government hospitals. Patients were Malaysian citizens in 90.1% of cases, Indonesian in 6.1%, and Filipino in 3.1%.
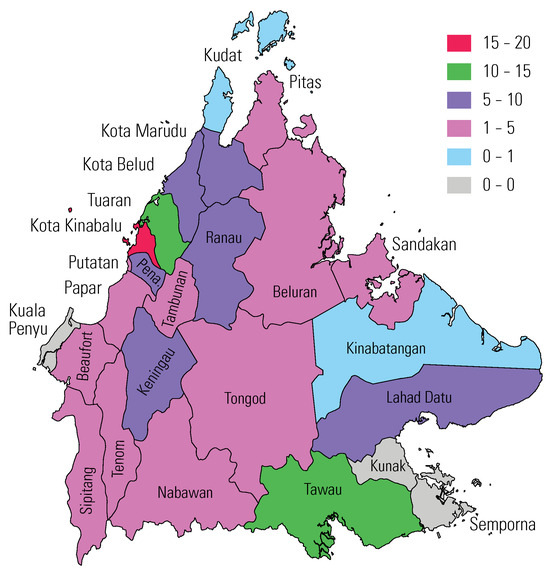
Figure 2.
Distribution of UGTB in Sabah, 2014 to 2020.
3.2. Clinical Characteristics of Patients
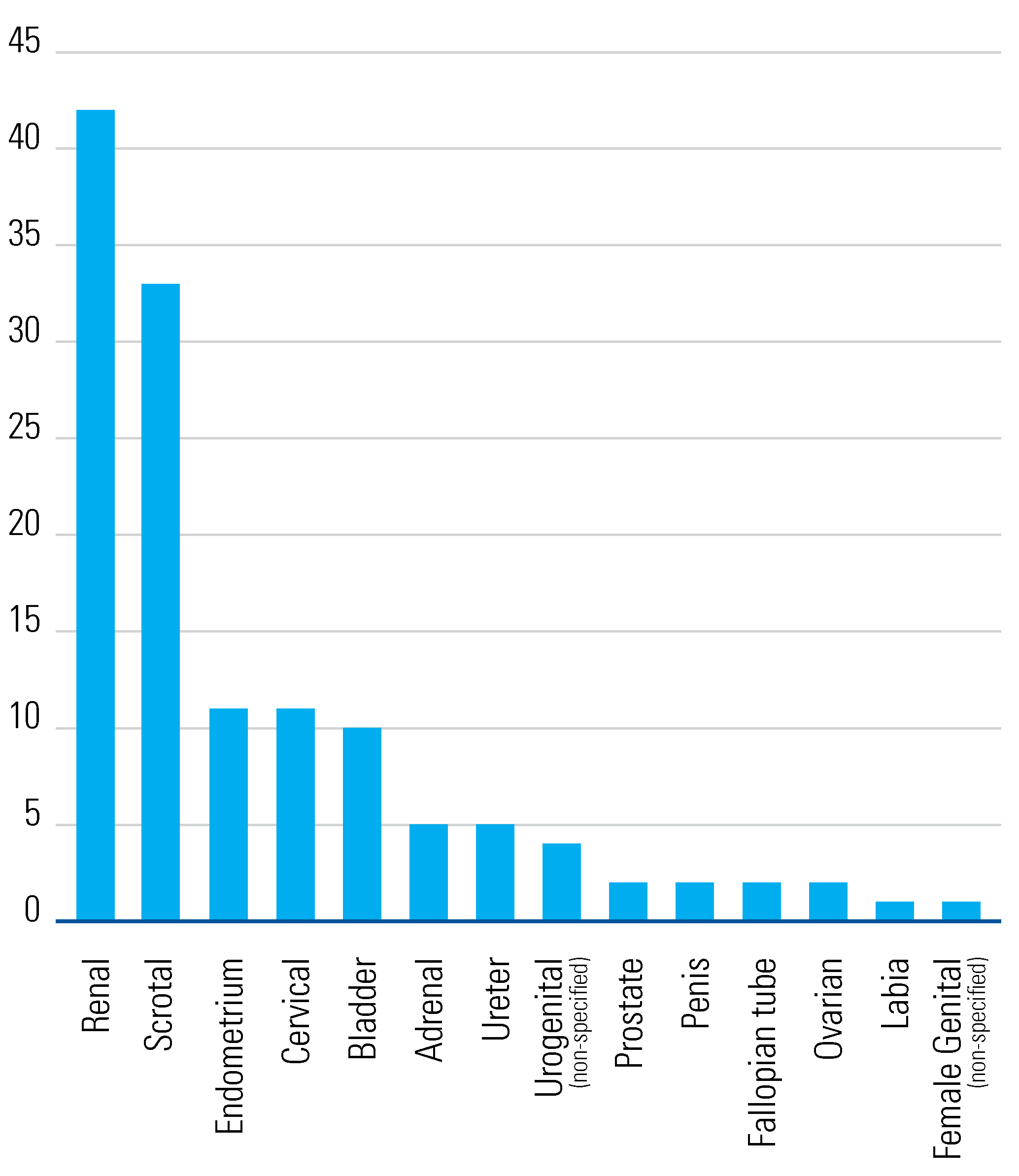
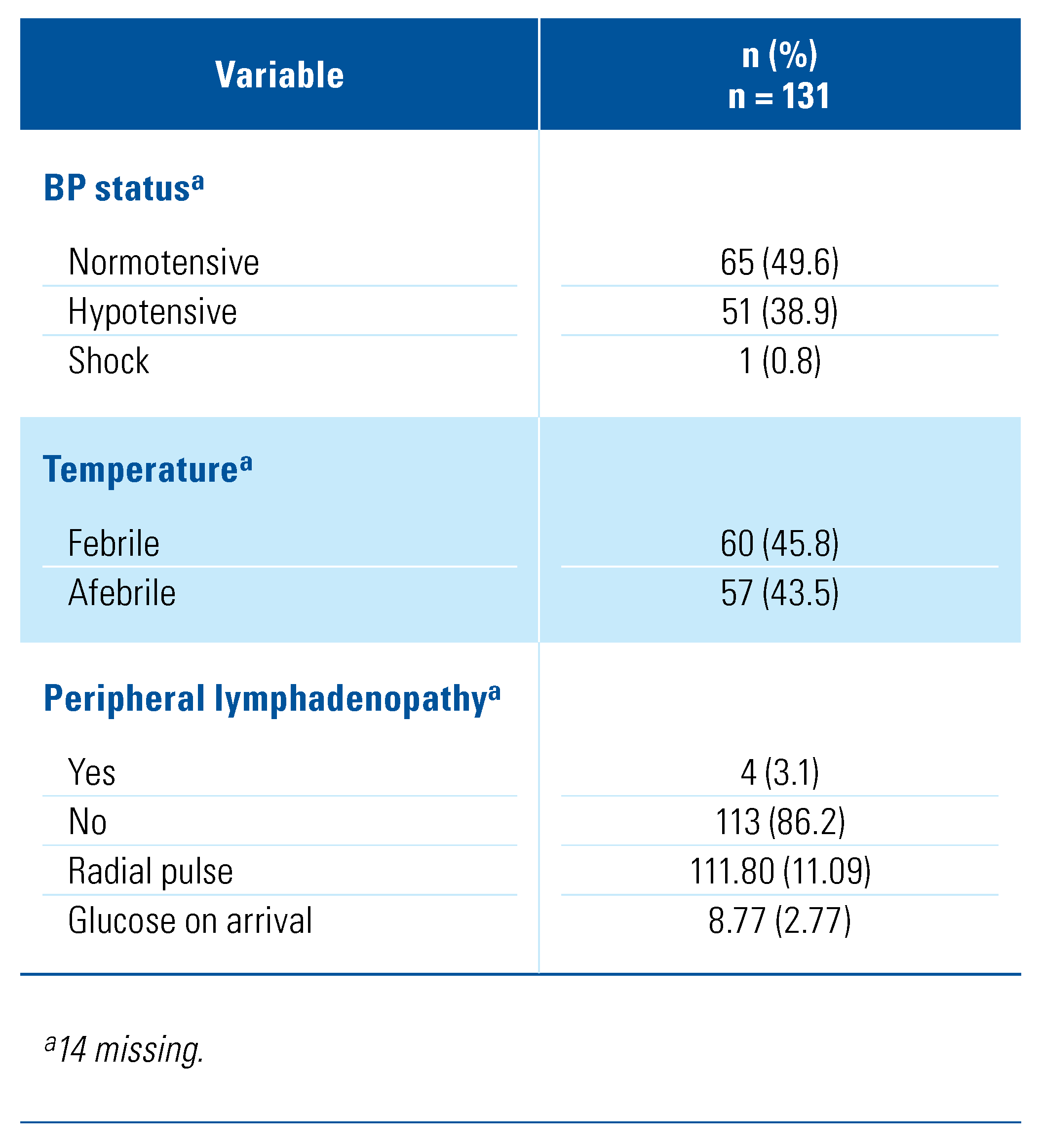
The clinical characteristics of the patient cohort are summarized in Table 2. The majority of the 131 cases 89.3%) were classified as new diagnoses. The most common sites of infection were renal (32.1%) and scrotal (25.2%), followed by endometrial and cervical (8.4% each) (Figure 3).

Table 2.
Clinical characteristics of study participants.
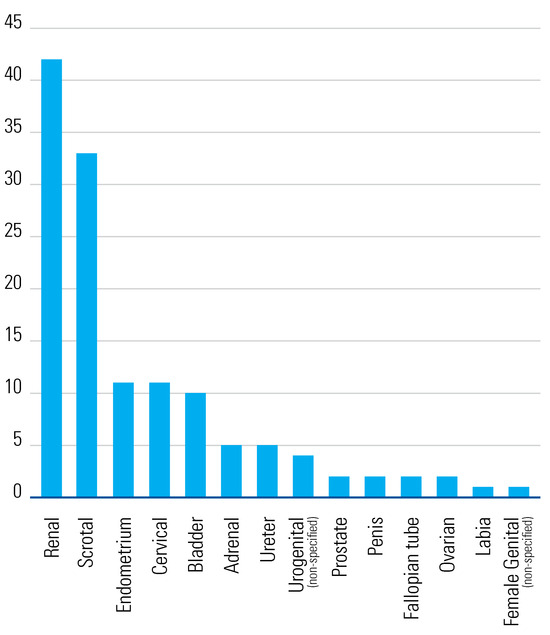
Figure 3.
Number of UGTB cases by site of involvement.
3.3. Clinical Presentation
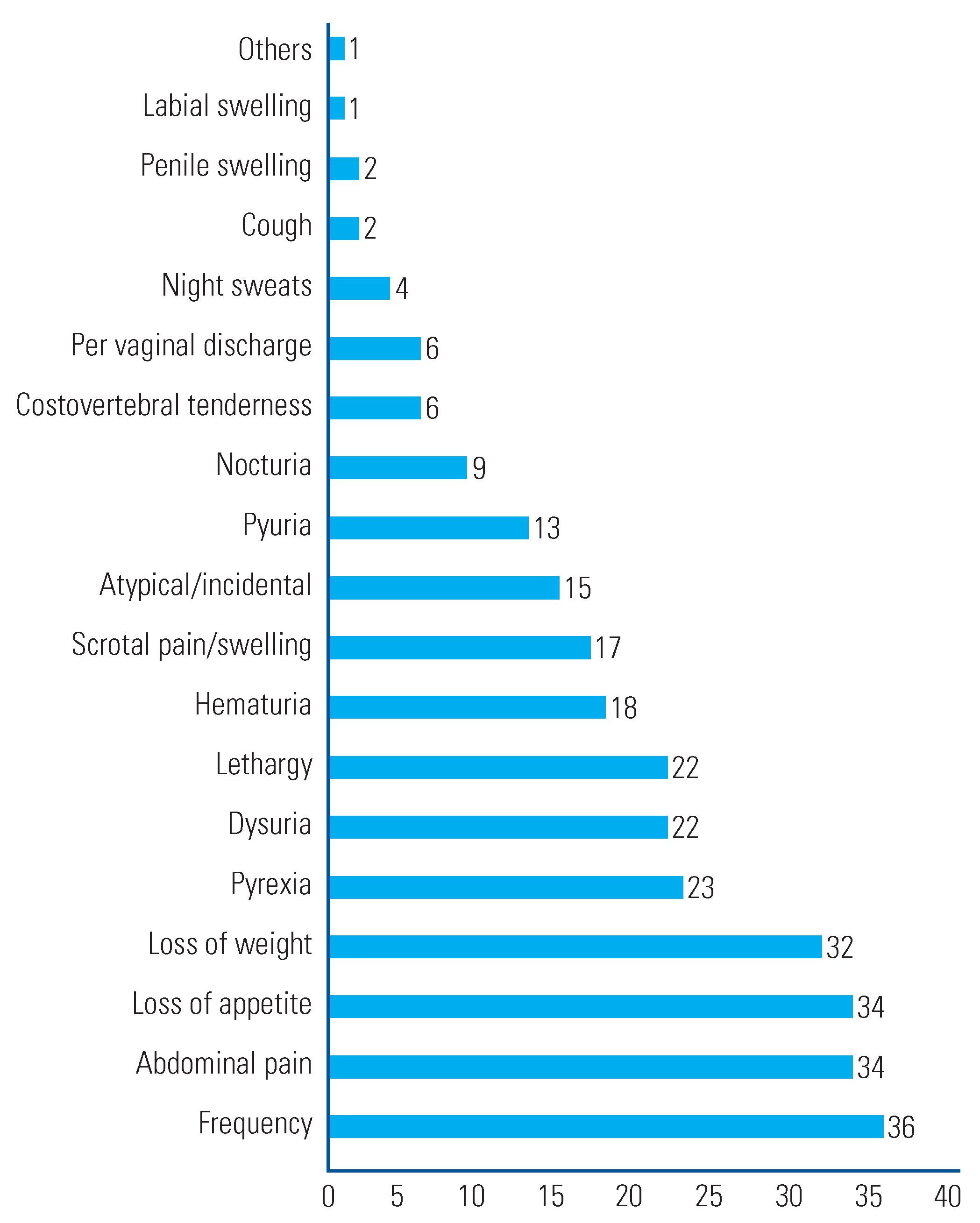
The clinical features at the time of presentation are summarized in Table 3 and Figure 4. Urinary frequency was the commonest symptom (28.2%), followed by abdominal pain and loss of appetite (each 26.0%). Overall, 45.8% of patients were found to have fever upon examination, and 3.1% presented with peripheral lymphadenopathy.

Table 3.
Presentation features of patients in the study.
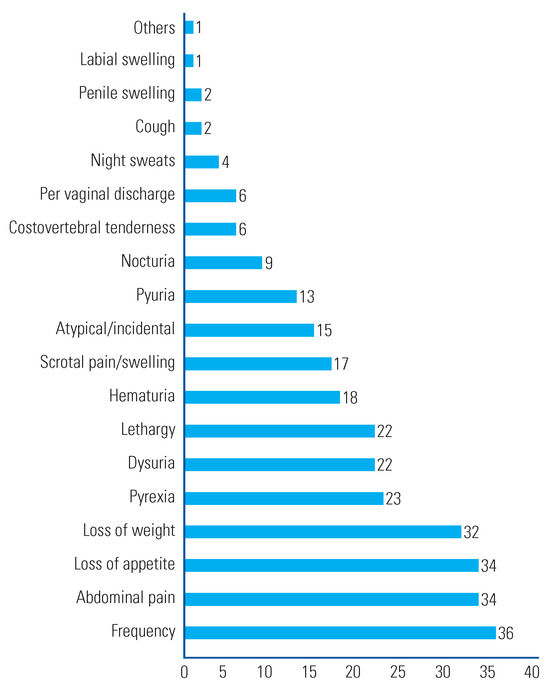
Figure 4.
Common presentations of UGTB, 2014–2020.
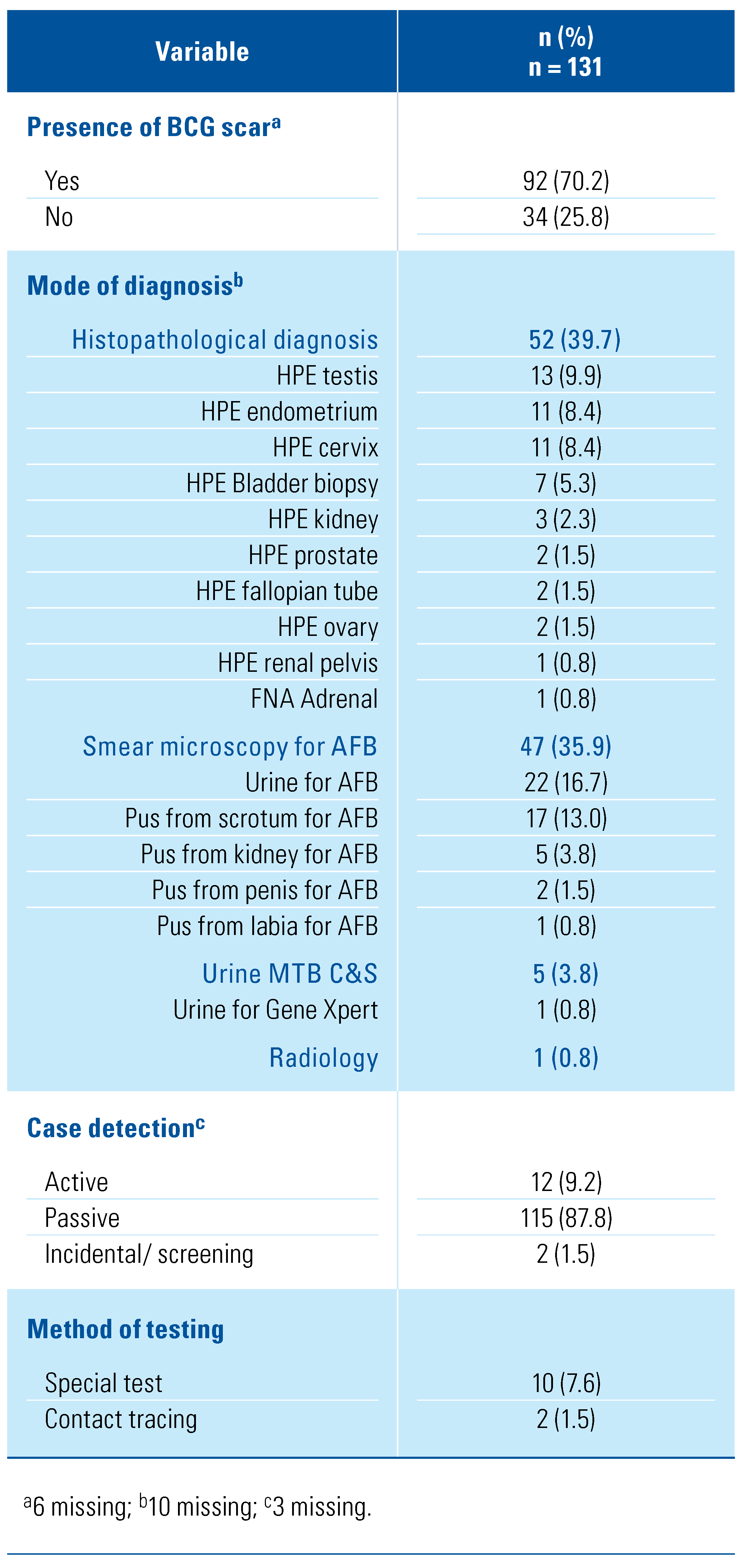
3.4. Method of Diagnosis
The means used to diagnose UGTB in the patient cohort are summarized in Table 4. Diagnosis was made by histopathological examination in 39.7%, microbial tests in 35.9%, urine for MTB culture in 3.8%, and radiological imaging in 0.8%. Information was missing for the remaining 20.6%

Table 4.
Method of diagnosis.
Of patients tested for HIV, 87.0% were negative and 2.3% were positive at the time of diagnosis (6.1% declined testing and data were missing for the remaining 4.6%). The common risk factors were chronic kidney disease (17.6%), family history of tuberculosis(16.0%), and diabetes mellitus (9.9%). Smokers made up of 20.6% of the cases.
3.5. Treatment Outcomes
Treatment outcomes are summarized in Table 5. The mean duration of treatment was 8.6 (SD: 4.0) months and the average hospital stay was 1.0 (SD: 1.7) month. During the intensive phase, 44.2% of patients received 2 months of ethambutol, isoniazid, rifampicin, and pyrazinamide (2 EHRZ regimen) and 41.2% received the fixed-dose combination (FDC) regimen. The majority of patients (77.9%) received 4 months of isoniazid and rifampicin (4HR regimen) during the maintenance phase. The most common adverse event during the intensive phase was death (3.8%). The directly observed treatment short course (DOTS) was used in 89.3% of patients in the intensive phase, and in 76.3% during the maintenance phase. The majority of observers for the DOTS treatment were the patient’s family members (63.6%). At the point of data compilation, 81.0% of the patients had already completed their treatment, and 6.1% were lost to follow-up.

Table 5.
Treatment of patients in the study.
We found that 50.4% of patients had received surgical intervention; 10.7% had undergone incision and drainage, 9.9% had cystoscopy, and 6.9% underwent orchidectomy.
5. Discussion
Tuberculosis is a communicable disease that is a major cause of ill health, one of the top 10 causes of death worldwide, and the leading cause of death from a single infectious agent (ranking above HIV/AIDS). The disease typically affects the lungs (pulmonary TB) but can also affect other sites (extrapulmonary TB). About 90% of cases are in adults, and there are more cases among men than women. Globally, an estimated 10 million people fell ill with TB in 2019. The incidence of TB in Malaysia as of 2019 is 92 per 100 000 population [1].
Our study provides a sub-state analysis of UGTB in Sabah, Malaysia, from January 2014 to November 2020. Our findings highlight the burden of disease in Sabah; however, there are no data for comparison with other states in Malaysia. In 2019, the WHO Southeast Asia region had accounted for 44% of TB cases. Malaysia, which is within that region, has a population of 32.7 million people, and Sabah, its second largest state, accounts for 3.9 million [9].
Geographically, Sabah is situated between Indonesia and the Philippines, and these countries are amongst the top 8 countries that account for two-thirds of the global total of TB cases. Indonesia, second to India, accounts for 8.5% and the Philippines accounts for 6.0% [3]. In 2019, the Philippines had an estimated incidence of 554 per 100 000 population, Indonesia 312 per 100 000 population, and Malaysia <100 cases per 100 000 population [1,10].
Following the formation of Malaysia in 1963, cross-border movement, which had previously been considered legal, became illegal. However, proximity to Indonesia and the Philippines, and a long and porous border have made it difficult to stop all movement, and the presence of marginalized communities (sea-nomads) is of concern in eastern Sabah [10]. Most of the cases that we observed in migrants were reported in Sandakan and Lahad Datu, the coastal region through which cross-border movement commonly occurs.
Topographically, Sabah poses a challenge in term of gaining immediate health access, and delays in seeking treatment were common. During our study, 71.8% of cases were noted to be from rural areas. We also observed that most of our cases were detected by the government facilities: 96.3%, compared with 3.8% by non-governmental facilities. Continuous health education on TB, aimed at raising awareness and correcting misconceptions, is needed and should be extended to include those who use non-government facilities [11,12].
Economically, Sabah has been challenged more than the rest of Malaysia. In 2019, Sabah was one of the 4 states with the lowest GDP per capita (RM 25 326). Sabah had an unemployment rate of 5.8% in 2019 [9]. Our results have shown that 58.8% of UGTB patients were unemployed, with a high percentage of illiteracy (28.2%). This supports the view that poverty and poor education contribute to delays in access to diagnosis and care.
UGTB has insidious onset, with varied or atypical presentation, which poses difficulty in diagnosis and can delay treatment. Most patients present with local symptoms such as frequent voiding, dysuria, pyuria, or back, flank, or abdominal pain. The organs most commonly involved are kidney, bladder, fallopian tubes, and scrotum. It commonly affects middle aged subjects. The incidence is slightly higher in men, and it is uncommon in children [1,8,11,12,13,14,15]. Patients with UGTB have been reported as having more local than systemic symptoms. Our study concurs with common presentation of frequency of micturition (28.2%), followed by abdominal pain (26.0%). We also found that systemic symptoms, such loss of appetite (26.0%) and loss of weight (24.4%), were common. The sites most commonly seen in our study were kidney (32.1%) and scrotum (25.2%).
We note that during our study period, treatment duration was 8.6 (±SD 3.97) months. The most common intensive phase regimens in the first 2 months were 2 EHRZ (ethambutol, isoniazid, rifampicin, pyrazinamide) 44.2% and fixed-dose combinations (FDC) consisting of 41.2%. The most common maintenance regimen was 4 months of HR (77.9%). A total of 89.3% have observed DOTs during intensive phase, DOTs was observed by family members in 63.6% of our subjects. 76.3% observed DOTs during maintenance phase. 81.0% of patients have completed treatment at the time of this study. We note that 50.4% of patients received surgical intervention. In these patients, 10.7% had undergone incision and drainage, 9.9% had cystoscopy, 9.2% did not have surgical intervention, and orchidectomy was done for 6.9% of patients. However, limitation in terms of retrieving primary records and details led to difficulty in further description of interventions and outcome.
An understanding of the local epidemiology and clinical characteristics of disease is essential to successful prevention measures and treatment implementation. No previous data collection has been done in Malaysia to evaluate UGTB. Malaysia has a complex system of data collection and TB reporting, involving both paper and electronic methods. The Sabah State TB notification system (myTB) database is the best data source available. It has been under regular audit and scrutiny of The Sabah State Department of Health. The economic challenges in Sabah, however, pose hurdles in terms of data collection which may have caused underreporting of UGTB. Furthermore, myTB has shortfalls in terms of the extent of information provided, especially for EPTB. Lack of primary records and missing documentation created a significant challenge to obtaining necessary information such as previous surgical interventions and outcome, which would further enhance our understanding of this disease.
4. Conclusions
UGTB is a relatively uncommon manifestation of extrapulmonary TB, which is challenging to diagnose. Progression is insidious, symptoms are non-specific, awareness is poor, and bacteriological diagnosis is difficult. Therefore, high levels of vigilance and clinical suspicion are required if it is to be recognized. UGTB is a contagious infectious disease that necessitates early diagnosis and treatment to prevent morbidity. Patients from endemic areas need to be assessed with high suspicion and screened for UGTB for early diagnosis and treatment. Ensuring awareness via widespread education within health care, in both the government and the private sector, along with rural outreach programs, will contribute to early recognition and treatment.
Acknowledgments
The authors would like to thank the Director General of Health, Malaysia for his permission to publish this article. The authors are grateful to Christina Rundi, Roddy Teo, The Sabah State Department of Health, along with the involved district hospitals of Sabah for making data available. We acknowledge the generous support of Sophia Lee Eu Wei, Prabakaran Balakrishnan and the staff in Urology Clinic Hospital Queen Elizabeth Sabah.
Conflicts of Interest
None declared.
Abbreviations
| DOTS | directly observed treatment short course |
| EPTB | extrapulmonary TB |
| FDC | fixed-dosanation |
| TB | tuberculosis |
| UGTB | urogenital tuberculosis |
References
- Gutierrez, M.C.; Brisse, S.; Brosch, R.; Fabre, M.; Omaïs, B.; Marmiesse, M.; et al. Ancient origin and gene mosaicism of the progenitor of Mycobacterium tuberculosis. PLoS Pathogens 2005, 1, e5. [Google Scholar] [CrossRef] [PubMed]
- Hershkovitz, I.; Donoghue, H.D.; Minnikin, D.E.; May, H.; Lee, O.Y.C.; Feldman, M.; et al. Tuberculosis origin: The Neolithic scenario. Tuberculosis. 2015, 95 (Suppl. 1), S122–S126. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO. Global tuberculosis report 2019. In World Health Organization. 2020.
- Iyawoo, K. Tuberculosis in Malaysia: Problems and prospect of treatment and control. Tuberculosis 2004, 84, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Visweswaran, R.K.; Bhat, S. Tuberculosis of the urinary tract. In: Floege J, Johnson RJ, Feehally, J., eds. Comprehensive Clinical Nephrology. Science Direct 2010, 641–648. [Google Scholar] [CrossRef]
- Figueiredo, A.; Lucon, A.; Srougi, M. Urogenital tuberculosis. In Tuberculosis and Nontuberculous Mycobacterial Infections, 7th ed.; Schlossberg, D., Ed.; ASM Press: Washington, DC, USA, 2017. [Google Scholar] [CrossRef]
- Abbara, A.; Davidson, R.N. Etiology and management of genitourinary tuberculosis. Nat. Rev. Urol. 2011, 8, 678–688. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, R.; Ansari, M.S.; Mandhani, A.; Gulia, A. Clinical presentation and diagnostic approach in cases of genitourinary tuberculosis. Indian. J. Urol. 2008, 24, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Department of Statistics, Malaysia. Available online: https://www.dosm.gov.my.
- Dollah, R.; Wan Hassan, W.S.; Peters, D.; Othman, Z. Old threats, new approach and national security in Malaysia: Issues and challenges in dealing with cross-border crime in East Coast of Sabah. Mediterr. J. Soc. Sciences 2016, 7, 178. [Google Scholar] [CrossRef]
- Kulchavenya, E.; Kholtobin, D. Diseases masking and delaying the diagnosis of urogenital tuberculosis. Ther. Adv. Urol. 2015, 7, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Merchant, S.; Bharati, A.; Merchant, N. Tuberculosis of the genitourinary system-urinary tract tuberculosis: Renal tuberculosis-part I. Indian. J. Radiol. Imaging. 2013, 23, 46–63. [Google Scholar] [CrossRef] [PubMed]
- Kulchavenya, E.; Zhukova, I.; Kholtobin, D. Spectrum of urogenital tuberculosis. J. Infect. Chemother. 2013, 19, 880–883. [Google Scholar] [CrossRef] [PubMed]
- Krishnamoorthy, S.; Palaniyandi, V.; Kumaresan, N.; Govindaraju, S.; Rajasekaran, J.; Murugappan, I.; et al. Aspects of evolving genito urinary tuberculosis-a profile of genito urinary tuberculosis (GUTB) in 110 patients. J. Clin. Diagn. Res. 2017, 11, PC01–PC05. [Google Scholar] [CrossRef] [PubMed]
- Zajaczkowski, T. Genitourinary tuberculosis: Historical and basic science review: Past and present. Cent. European J. Urol. 2012, 65, 182–187. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.