Pelvic Fracture Urethral Injury in Females
Abstract
:1. Introduction
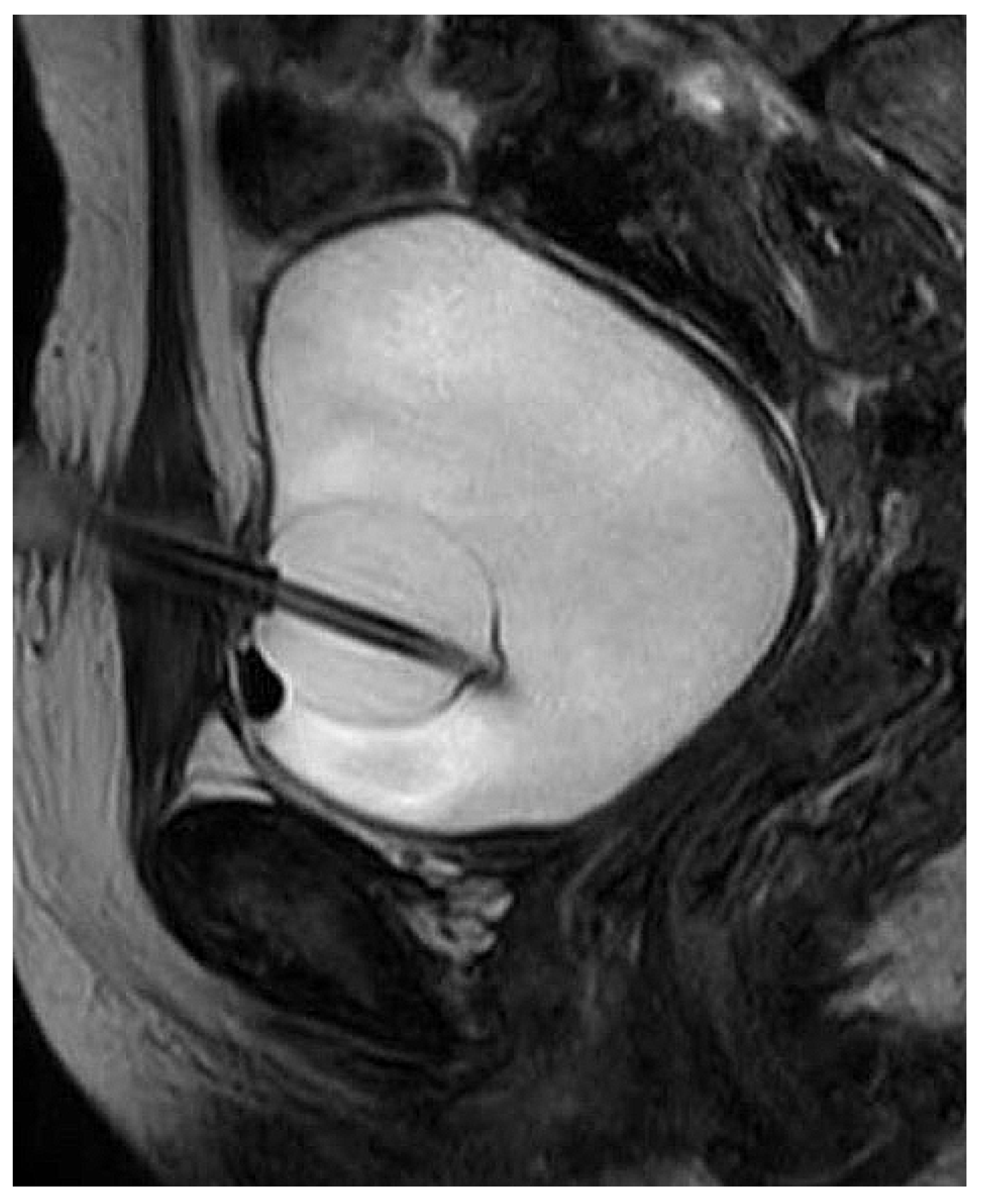
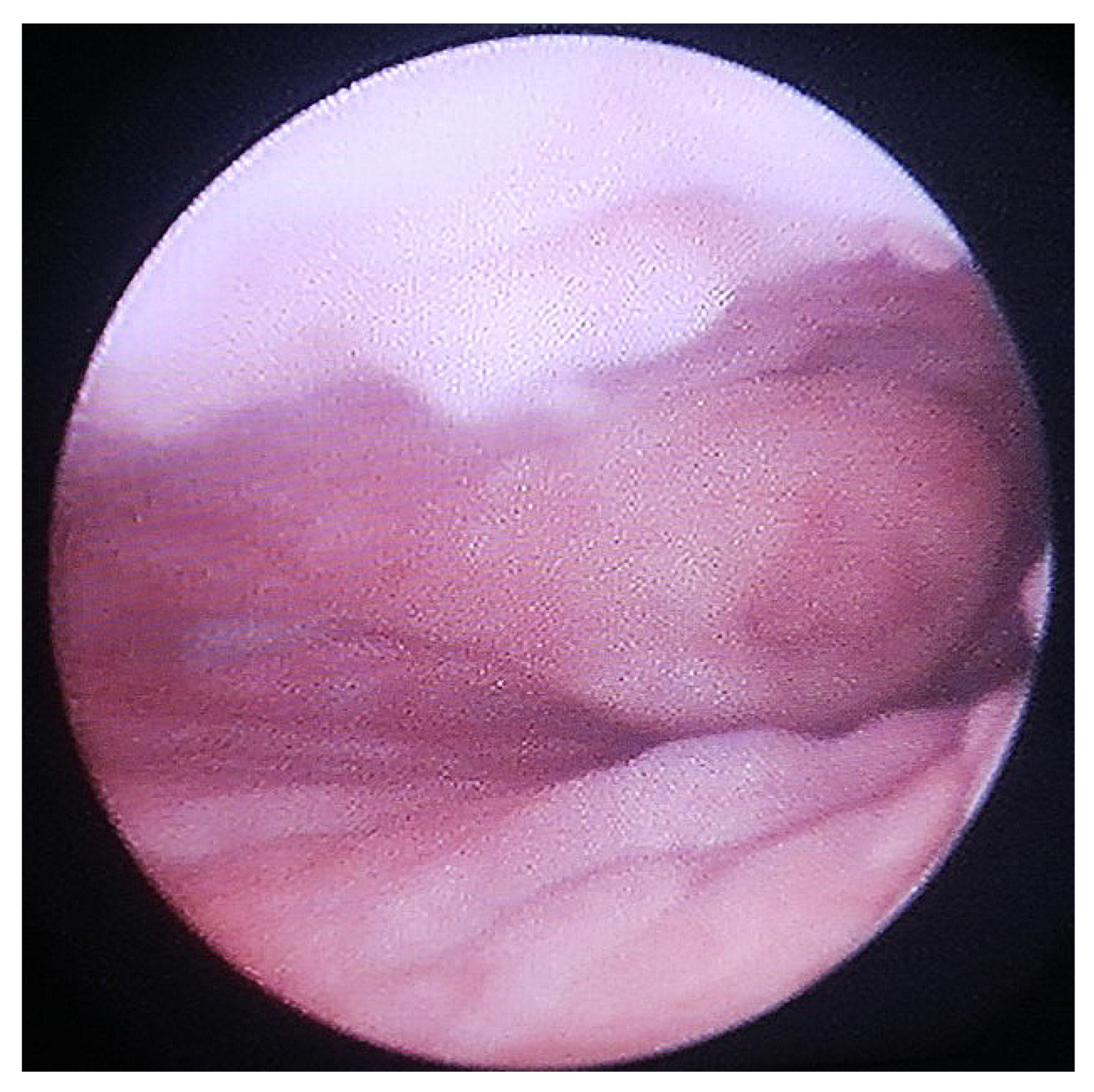
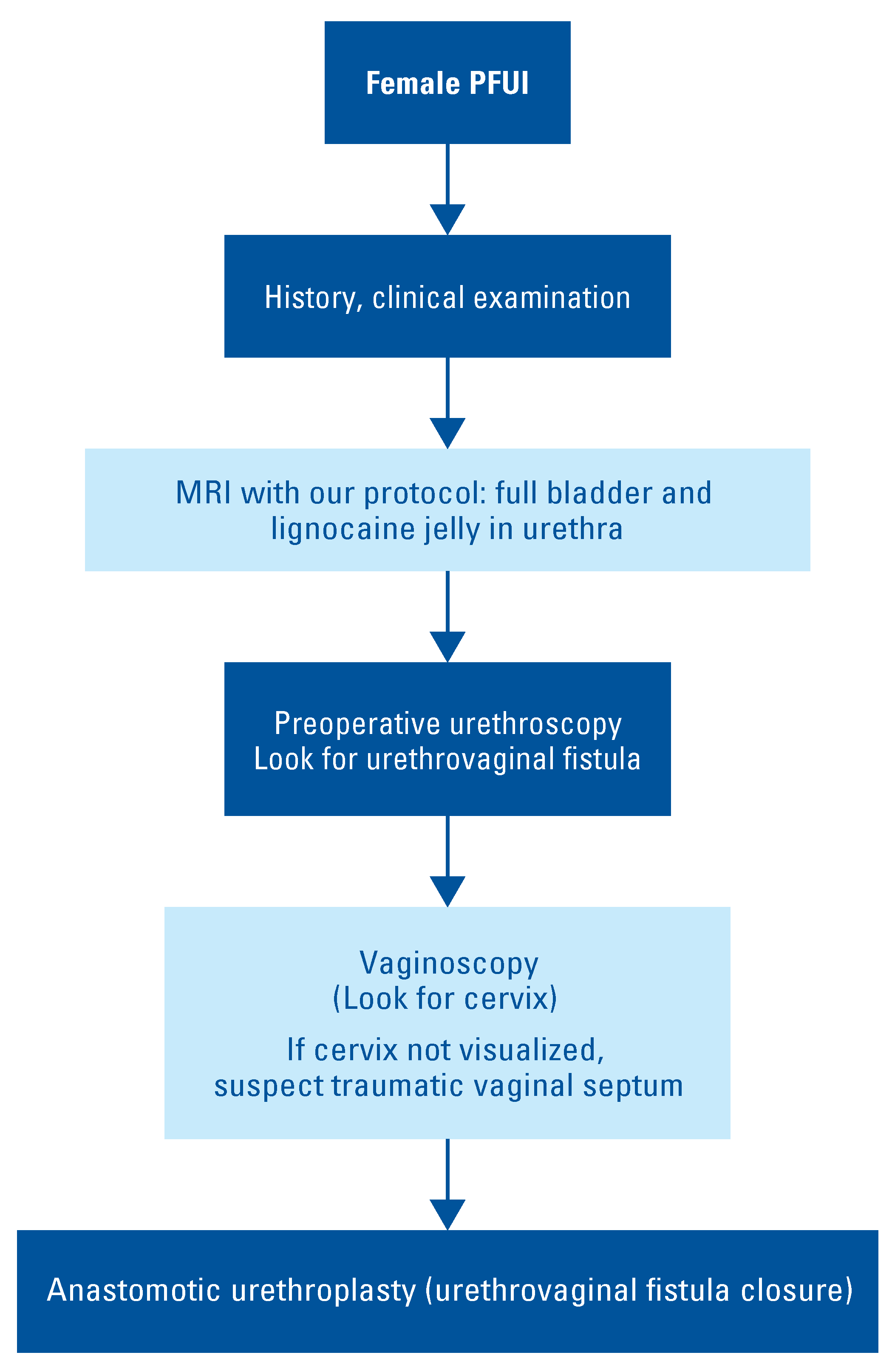
2. Materials and Methods
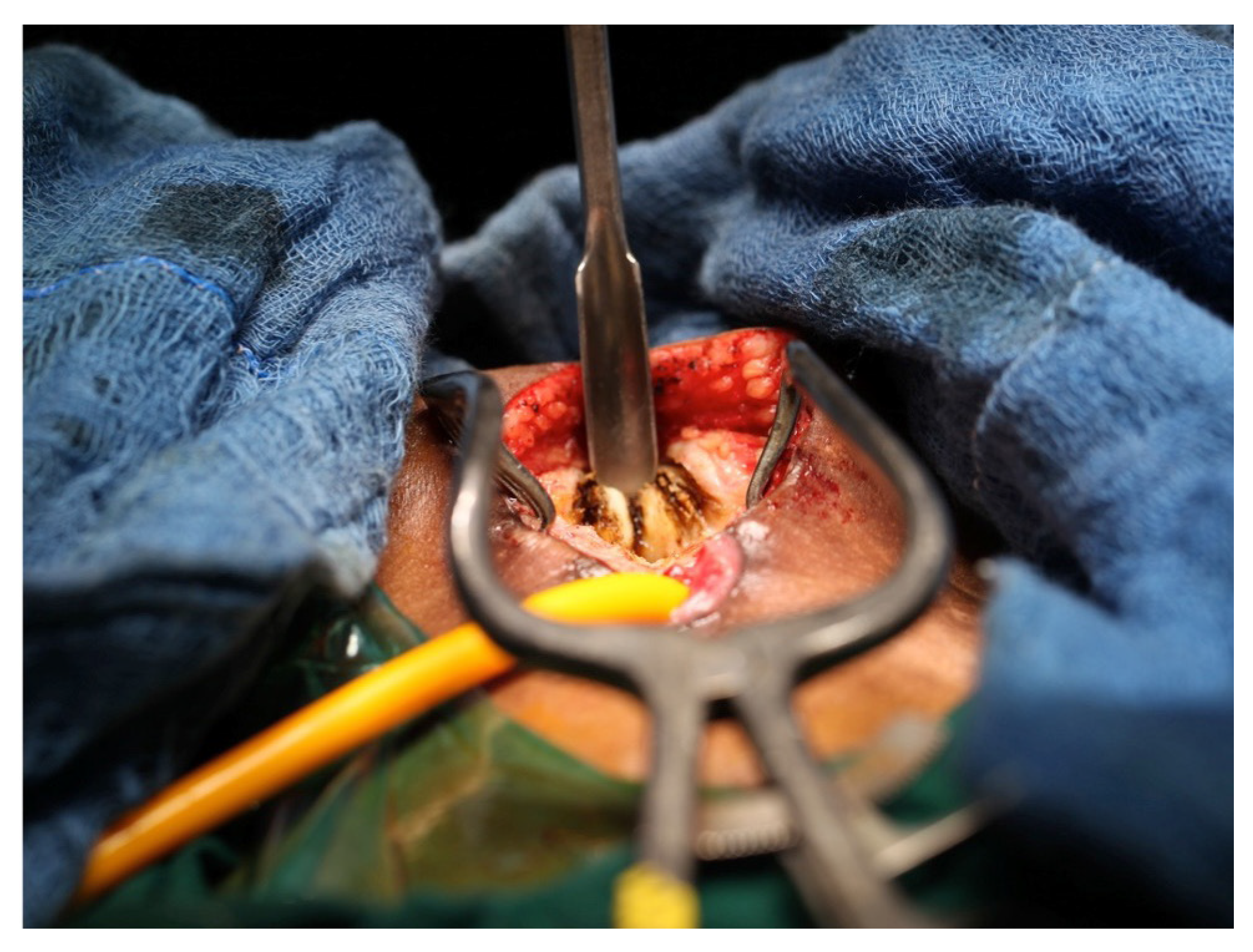
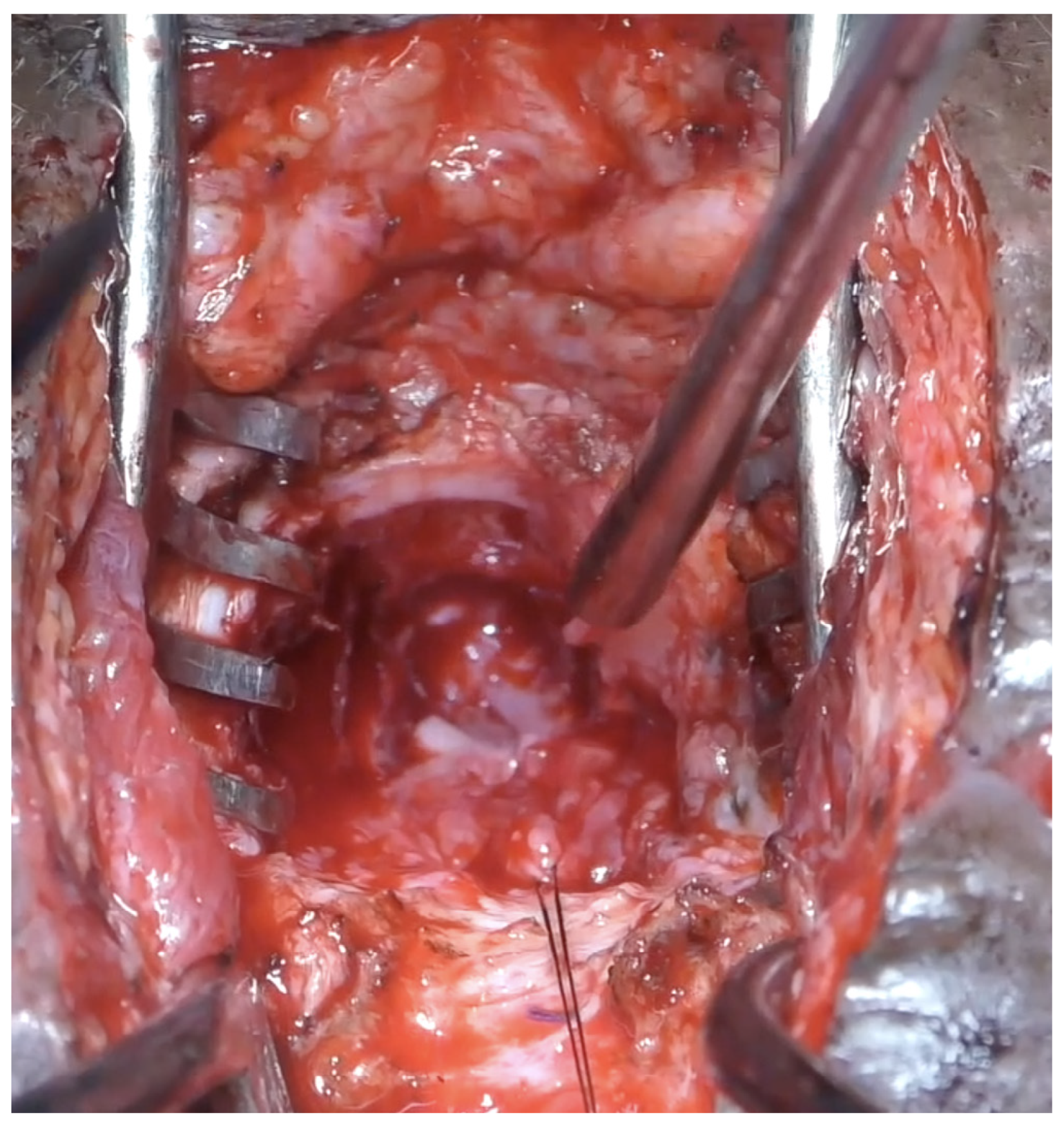
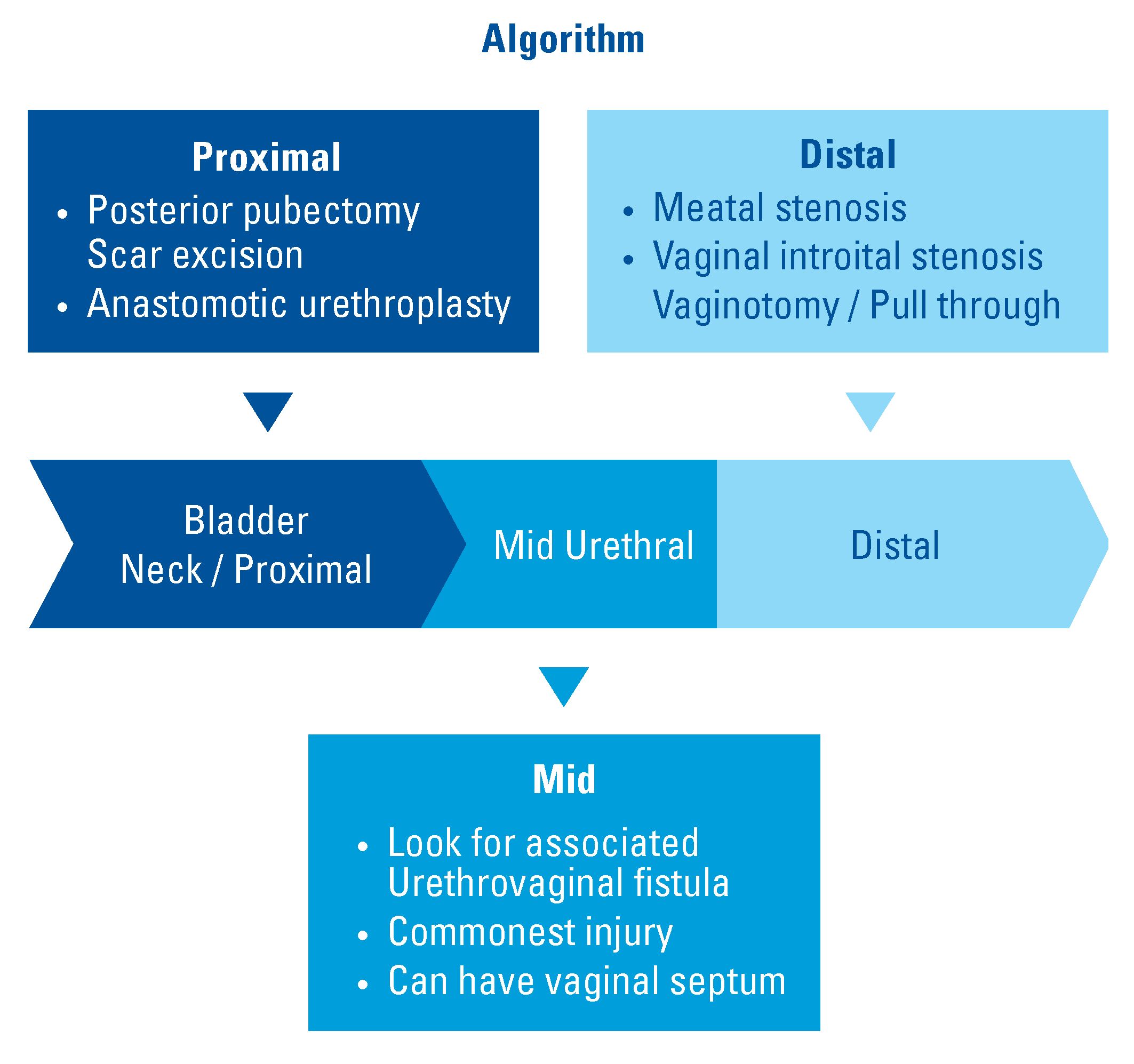
2.1. Approach
2.2. Transection at Bladder Neck
2.3. Transection at Proximal Urethra
2.4. Transection at Mid Urethra
2.5. Transection at Meatus
2.6. Urethral Lengthening
2.7. Vaginal Injury
2.8. Complete Urethral Loss
3. Results
4. Discussion
5. Conclusions
Conflicts of Interest
References
- Simpson-Smith, A. Traumatic rupture of the urethra: Eight personal cases with a review of 381 recorded ruptures. Br. J. Surg. 1936, 24, 309–332. [Google Scholar] [CrossRef]
- Antoci, J.P.; Schic, M.R., Jr. Bladder and urethral injuries in patients with pelvic fractures. J. Urol. 1982, 128, 25–26. [Google Scholar] [CrossRef] [PubMed]
- Bredael, J.J.; Kramer, S.A.; Cleeve, L.K.; Webster, G.D. Traumatic rupture of the female urethra. J. Urol. 1979, 122, 560–561. [Google Scholar] [CrossRef] [PubMed]
- Patil, U.; Nesbitt, R.; Meyer, R. Genitourinary tract injuries due to fracture of the pelvis in females: Sequelae and their management. Br. J. Urol. 1982, 54, 32–38. [Google Scholar] [CrossRef] [PubMed]
- Perry, M.O.; Husmann, D.A. Urethral injuries in female subjects following pelvic fractures. J. Urol. 1992, 147, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Barach, E.; Martin, G.; Tomlanovich, M.; Nowak, R.; Littleton, R. Blunt pelvic trauma with urethral injury in the female: A case report and review of the literature. J. Emerg. Med. 1984, 2, 101–105. [Google Scholar] [CrossRef] [PubMed]
- Carter, C.T.; Schafer, N. Incidence of urethral disruption in females with traumatic pelvic fractures. Am. J. Emerg. Med. 1993, 11, 218–220. [Google Scholar] [CrossRef] [PubMed]
- Venn, S.N.; Greenwell, T.J.; Mundy, A.R. Pelvic fracture injuries of the female urethra. BJU Int. 1991, 83, 626–630. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.B.; Surana, S.; Desai, D.J.; Orabi, H.; Iyer, S.; Kulkarni, J.; et al. Management of complex and redo cases of pelvic fracture urethral injuries. Asian J. Urol. 2018, 5, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Joshi, P.M.; Kulkarni, S.B. Management of pelvic fracture urethral injuries in the developing world. World J. Urol. 2020, 38, 3027–3034. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, S.B.; Joshi, P.M.; Hunter, C.; Surana, S.; Shahrour, W.; Alhajeri, F. Complex posterior urethral injury. Arab J. Urol. 2015, 13, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Joshi, P.M.; Desai, D.J.; Shah, D.; Joshi, D.P.; Kulkarni, S.B. Magnetic resonance imaging procedure for pelvic fracture urethral injuries and recto urethral fistulas: A simplified protocol. Turk. J. Urol. 2021, 47, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Podestá, M.L.; Jordan, G.H. Pelvic fracture urethral injuries in girls. J. Urol. 2001, 165, 1660–1665. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Kaushal, D.; Khattar, N.; Nayyar, R.; Manasa, T.; Sood, R. Pediatric pelvic fracture urethral distraction defect causing complete urethrovaginal avulsion. Indian J. Urol. 2018, 34, 76–78. [Google Scholar] [CrossRef] [PubMed]




| No | Age at Accident (years) | Interval to Surgery (months) | Group | Mechanism of Trauma | Associated Injuries | Mode of Treatment | Location of Injury | Approach and Surgery | Continence Day Night | Uroflow (mL/s) | Follow-Up (months) | Further Intervention | Final Result |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 5 | 3 | Prepubertal | Collapsing wall | Urethrovaginal fistula | Delayed | Proximal | Abdominal, closure of UVF, anastomotic urethroplasty | Yes No | 9 | 47 | None | Success |
| 2 | 2 | 36 | Prepubertal | Collapsing wall | Urethrovaginal fistula | Delayed | Proximal | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 0a | 36 | Redo | Success |
| 3 | 9 | 4 | Prepubertal | Road traffic accident | Urethrovaginal fistula | Delayed | Proximal | Abdominal, closure of UVF, anastomotic urethroplasty | Yes No | 14 | 42 | None | Success |
| 4 | 10 | 6 | Prepubertal | Road traffic accident | Urethrovaginal fistula, lower limb fractures, degloving injury in thigh | Delayed | Mid | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 18 | 46 | None | Success |
| 5 | 11 | 4 | Prepubertal | Road traffic accident | None | Delayed | Mid | Abdominal, anastomotic urethroplasty | Yes Yes | 16 | 63 | None | Success |
| 6 | 10 | 3 | Prepubertal | Road traffic accident | Urethrovaginal fistula, lower limb fracture | Delayed | Mid | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 20 | 80 | None | Success |
| 7 | 43 | 24 | Postpubertal | Road traffic accident | Urethrovaginal fistula | Delayed | Mid | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 16 | 66 | None | Success |
| 8 | 23 | 6 | Postpubertal | Road traffic accident | Lower limb fracture | Delayed | Distal | Vaginal | Yes Yes | 19 | 112 | None | Success |
| 9 | 35 | 3 | Postpubertal | Road traffic accident | None | Delayed | Mid | Vaginal | Yes Yes | 20 | 132 | None | Success |
| 10 | 30 | 0b | Postpubertal | Road traffic accident | Vaginal injury, lower limb fracture | Primary | Mid | Vaginal | Yes Yes | 22 | 156 | None | Success |
| 11 | 22 | 10 | Postpubertal | Road traffic accident | Vaginal injury | Delayed | Distal | Vaginal, meatoplasty | Yes Yes | 18 | 72 | None | Success |
| 12 | 5 | 11 | Prepubertal | Road traffic accident | Vaginal stenosis | Delayed | Distal | Vaginal, meatoplasty, vaginotomy | Yes No | 11 | 60 | Vaginal pull-through | Success |
| 13 | 21 | 3 | Postpubertal | Road traffic accident | Lower limb fracture, complete urethral loss | Delayed | Proximal, Mid, Distal | Abdominal, bladder flap | Yes No | 6 | 37 | None | Success |
| 14 | 6 | 24c | Prepubertal | Road traffic accident | Lower limb fracture, anterior vaginal wall loss | Delayed | Mid | Abdominal, closure of UVF, anastomotic urethroplasty, Martius flap with skin forming the anterior vaginal wall | Yes Yes | 12 | 12 | None | Success |
| 15 | 26 | 37d | Postpubertal | Road traffic accident | Urethrovaginal fistula | Delayed | Mid | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 22 | 14 | None | Success |
| 16 | 24 | 10 | Postpubertal | Road traffic accident | Lower limb fracture, vaginal stenosis | Delayed | Distal | Vaginal, pedicled labial flap, vaginotomy | Yes No | 14 | 48 | None | Success |
| 17 | 27 | 14 | Postpubertal | Road traffic accident | None | Delayed | Distal | Vaginal, urethroplasty with laser incision of vaginal septum | Yes Yes | 14 | 24 | Vaginal pull-through | Vaginal septum Amenorrhea |
| 18 | 21 | 11 | Postpubertal | Road traffic accident | Urethrovaginal fistula | Delayed | Mid | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 22 | 32 | None | Success |
| 19 | 38 | 22 | Postpubertal | Road traffic accident | Urethrovaginal fistula, limb fracture | Delayed | Proximal | Abdominal, closure of UVF, anastomotic urethroplasty | Yes Yes | 21 | 18 | None | Success |
| 20 | 9 | 11 | Prepubertal | Road traffic accident | Urethrovaginal fistula | Delayed | Bladder neck | Abdominal, anastomotic urethroplasty | Yes Yes | 19 | 12 | None | Success |
| 21 | 10 | 10 | Prepubertal | Road traffic accident | None | Delayed | Distal | Meatoplasty, vaginal pull-through | Yes Yes | 11 | 12 | None | Success |
| 22 | 24 | 9 | Postpubertal | Fall from train | Urethrovaginal fistula | Delayed | Mid | Abdominal, anastomotic urethroplasty | Yes Yes | 22 | 12 | None | Success |
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Joshi, P.M.; Bandini, M.; Yepes, C.; Bhadranavar, S.; Sharma, V.; Bafna, S.; Kulkarni, S.B. Pelvic Fracture Urethral Injury in Females. Soc. Int. Urol. J. 2022, 3, 77-86. https://doi.org/10.48083/MBXR6354
Joshi PM, Bandini M, Yepes C, Bhadranavar S, Sharma V, Bafna S, Kulkarni SB. Pelvic Fracture Urethral Injury in Females. Société Internationale d’Urologie Journal. 2022; 3(2):77-86. https://doi.org/10.48083/MBXR6354
Chicago/Turabian StyleJoshi, Pankaj M., Marco Bandini, Christian Yepes, Shreyas Bhadranavar, Vipin Sharma, Sandeep Bafna, and Sanjay B. Kulkarni. 2022. "Pelvic Fracture Urethral Injury in Females" Société Internationale d’Urologie Journal 3, no. 2: 77-86. https://doi.org/10.48083/MBXR6354
APA StyleJoshi, P. M., Bandini, M., Yepes, C., Bhadranavar, S., Sharma, V., Bafna, S., & Kulkarni, S. B. (2022). Pelvic Fracture Urethral Injury in Females. Société Internationale d’Urologie Journal, 3(2), 77-86. https://doi.org/10.48083/MBXR6354




