Abstract
Objectives To assess the outcomes of a conservative management approach to radiation-induced urethral stricture disease (R-USD) in an elderly population with comorbidities. Methods Patients with R-USD managed with endoscopic procedures and/or clean intermittent catheterization (CIC) between 2007 and 2019 were included. Patients were excluded if they had an obliterative stricture, prior urethral reconstruction/urinary diversion surgery, or < 3 months follow-up. Primary outcome measures were urinary tract infection (UTI), acute urinary retention (AUR), serum creatinine, uroflowmetry/post-void residual, and urinary incontinence (UI). Failure was defined as progression to reconstructive surgery or permanent indwelling catheterization. Results Ninety-one men were analyzed with a median follow-up of 15.0 months (IQR 8.9 to 37.9). Median age was 75.4 years (IQR 70.0 to 80.0), body mass index was 26.5 kg/m2 (IQR 24.8 to 30.3), and Charlson comorbidity index was 6 (IQR 5 to 8). Median stricture length was 2.0 cm (IQR 2.0 to 3.0). Stricture location was bulbar (12%), bulbomembranous (75%), and prostatic (13%). A total of 90% underwent dilation, and 44% underwent direct visual internal urethrotomy (DVIU). For those that underwent these procedures, median number of dilations and DVIUs per patient was 2 (IQR 1 to 5) and 1 (IQR 1 to 3), respectively. Forty percent used CIC. Thirty-four percent developed a UTI, and 15% had an AUR episode requiring urgent treatment. Creatinine values, uroflowmetry measurements, and UI rates remained stable. Eighty percent avoided reconstructive surgery or indwelling catheterization. Conclusion Most elderly patients with comorbidities with R-USD appear to be effectively managed in the short-term with conservative strategies. Close observation is warranted because of the risk of UTIs and AUR. The potential long-term consequences of repetitive conservative interventions must be considered.
Introduction
Radiotherapy is a commonly used modality for the treatment of pelvic malignancies, particularly prostate cancer and anorectal cancers. According to a large retrospective analysis of the Surveillance, Epidemiology, and End Results (SEER) Program from 2004 to 2013, 38% of patients with localized prostate cancer chose radiation as initial therapy [1].
Although significant technical in recent years have allowed for more targeted therapy of the malignancy, ionizing radiation treatment can still result in ischemia and fibrosis of the surrounding tissues through direct and indirect damage to cellular deoxyribonucleic acid, with significant clinical consequences. Radiation-induced urethral stricture disease (R-USD) is one of these consequences, with a reported incidence of 1.7% to 31.6% depending on the type of radiation used [2,3,4]. This subset of USD is of particular importance to the reconstructive urologist because of the risk of stricture recurrence and development or worsening of urinary incontinence (UI) after surgical treatment.
Strictures after pelvic radiotherapy most commonly affect the bulbomembranous urethra [5], although isolated bulbar strictures or prostatic stenoses can occur. Recurrence rates after urethroplasty for R-USD are reported to range from 10% to 27% in series with short median follow-up [5,6], in comparison with the 15.6% recurrence rate reported in long-term follow-up of urethroplasties of any kind [7]. Reported UI rates range from 7% to 50% for those patients who have undergone urethroplasty for R-USD [5,6,8,9,10,11]. These patients may require subsequent artificial urinary sphincter (AUS) placement, and are subject to the increased risk of AUS erosion in a radiated field [12,13,14]. These well-documented risks in reconstructive surgery for R-USD lead some to instead consider endoscopic management with urethral balloon dilation, direct vision internal urethrotomy (DVIU), and/or clean intermittent catheterization (CIC) despite stricture recurrence rates reported in the range of 40% to 60% [15]. Additionally, many of these patients are elderly and have comorbidities resulting in suboptimal surgical candidacy.
There is a dearth of literature on the outcomes of conservative treatment strategies for R-USD with the goal of avoiding invasive surgery or permanent indwelling catheterization; in particular, there is little on the safety, associated complications, and effect on quality of life of such an approach. The objective of this multi-institutional study was to evaluate the outcomes of conservative management for R-USD in patients who were not optimal surgical candidates or who were unwilling to accept the risks associated with stricture recurrence and new or worsening UI following urethroplasty.
Methods
After obtaining institutional review board approval, we retrospectively identified patients with R-USD placed on a conservative treatment regimen by 3 fellowship-trained reconstructive urologists at 2 participating institutions between 2007 and 2019. The decision to manage R-USD with conservative techniques, urethral reconstruction, urinary diversion surgery, or permanent indwelling catheterization was based upon a patient-centered decision-making model including thorough counseling on the risks and benefits of all treatment options. Conservative management was defined as urethral balloon dilation, DVIU, or CIC. Patients were excluded from analysis if they had an obliterative stricture, separate stricture of the pendulous urethra or fossa navicularis/meatus, isolated bladder neck contracture, prior history of urethral reconstruction or urinary diversion surgery, or less than 3 months’ follow-up.
Patient demographics, pelvic radiation details, previous urologic interventions, and stricture-related urinary symptoms were evaluated. Stricture characteristics were assessed by retrograde urethrogram, voiding cystourethrogram, and/or cystourethroscopy. The choice of diagnostic tool(s) was based on surgeon discretion, consistent with American Urological Association guidelines for male urethral stricture [16]. Treatment details were recorded, including the number of dilations and DVIUs per patient and CIC regimen details. Patients who underwent multiple different management techniques were included to reflect real-life clinical practice.
During the study period, we evaluated several primary outcome measures. These included the incidence of culture-proven urinary tract infections (UTI) requiring antibiotic therapy and acute urinary retention (AUR) episodes requiring urgent intervention such as complex urethral catheter placement or suprapubic tube placement. Objective outcomes including changes in serum creatinine levels, uroflowmetry values, and postvoid residual measurements over time were captured. The effect of conservative management strategies on urinary continence status and the need for incontinence treatment was also assessed. Conservative management failure was defined as progression to reconstructive surgery or permanent indwelling catheterization.
Categorical variables were compared with the McNemar test, chi-square test, and Fisher exact test. Continuous variables were compared with the Wilcoxon signed-rank test and the Wilcoxon rank-sum test. Statistical significance was predefined at P < 0.05.
Results
A total of 91 men were analyzed with a median followup of 15.0 months (IQR 8.9 to 37.9). Median age was 75.4 years (IQR 70.0 to 80.0), BMI was 26.5 kg/m2 (IQR 24.8 to 30.3), and Charlson comorbidity index (CCI) was 6 (IQR 5 to 8). The indication for pelvic radiation was prostate cancer (97%) and anorectal cancer (3%). Two patients who received radiation for prostate cancer also received radiation for other pelvic malignancies (one for bladder cancer and one for testicular cancer). Radiation type included external beam radiation alone (63%), brachytherapy alone (26%), combination external beam radiation and brachytherapy (5%), and protonbeam therapy (5%). Of those with prostate cancer, 81% received radiation as primary therapy, and 19% received adjuvant or salvage radiation. There were no salvage prostatectomies in this cohort.
Median stricture length was 2.0 cm (IQR 2.0 to 3.0). The majority of patients (75%) had a bulbomembranous stricture location with or without more proximal prostatic involvement. Isolated bulbar strictures and prostatic stenoses were seen in 12% and 13%, respectively. The most common urinary symptoms were slow flow (59%), urgency/frequency (52%), and nocturia (45%). UI was reported in 59% of patients at initial evaluation (42% stress UI, 34% urgency UI, 24% mixed UI). A total of 82 patients (90%) underwent urethral balloon dilation, and 40 patients (44%) underwent DVIU. For those that underwent these procedures, median number of dilations and DVIUs per patient was 2 (IQR 1 to 5) and 1 (IQR 1 to 3), respectively. CIC was used in 40% of patients.
Treatment Outcomes
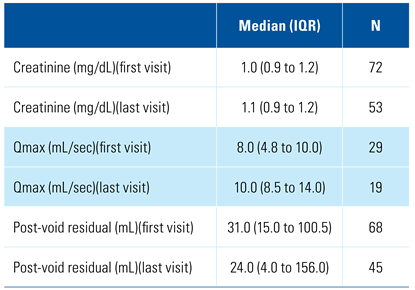
Median serum creatinine, uroflowmetry values, and post-void residual measurements remained stable between first and last visits (Table 1). Fourteen patients (15%) had an AUR episode requiring urgent treatment, with a median of 1 episode per patient (IQR 1 to 2). Median time to first AUR episode after initiation of conservative management was 14.4 months (IQR 1.7 to 48.6). Thirty-one patients (34%) developed a UTI requiring antibiotic therapy, with a median of 2 UTIs per patient (IQR 1 to 3). Median time to first UTI after initiation of conservative management was 14.3 months (IQR 4.5 to 39.4). Two patients developed urosepsis requiring hospitalization, 1 episode per patient. No patient developed severe or end-stage chronic kidney disease secondary to their stricture disease. UI rates remained stable over the study period (59% to 56%, P = 0.47). For those patients who used incontinence products, median number of pads per day (2.0 versus 1.5, P = 0.47) and median number of diapers per day (1.0 versus 1.0, P > 0.90) remained stable. Four patients (4%), none of whom progressed to urethral reconstruction, underwent subsequent AUS placement with no postoperative complications to date.

Table 1.
Objective urinary outcomes.
Treatment Failures
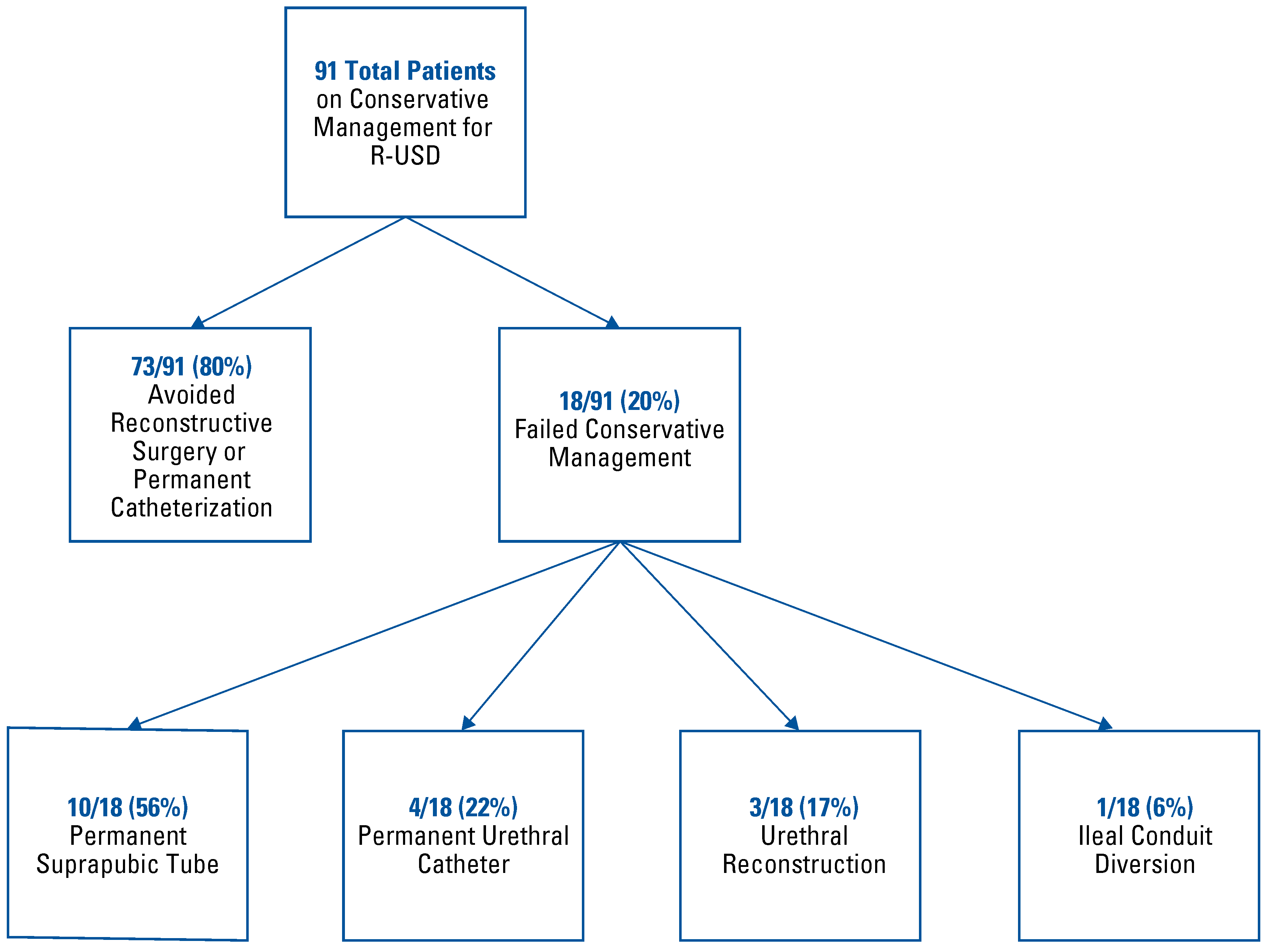
Eighteen patients (20%) started and subsequently failed conservative management strategies (Figure 1). Three patients (17%) pursued urethral reconstruction and 1 (6%) opted for ileal conduit diversion. Definitive indwelling urethral catheterization and suprapubic catheterization was pursued in 4 patients (22%) and 10 patients (56%), respectively. Failure rate stratified by radiation type was external beam radiation alone (19%), brachytherapy alone (13%), combination external beam radiation and brachytherapy (60%), and proton-beam therapy (20%). In the 55 of 91 patients (60%) with at least 1-year follow-up, failure rate was 22%.
Figure 1.
Treatment failures.
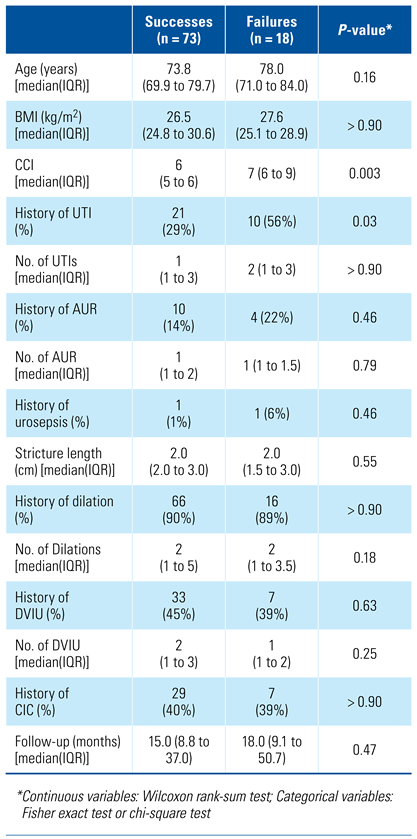
The incidence of UTI episodes was significantly higher in those who failed conservative management (P = 0.03) (Table 2). Median CCI was also statistically significantly higher in the failure group (P = 0.003). The success group and failure group were comparable with respect to which conservative interventions were performed and median follow-up.

Table 2.
Conservative management successes versus failures.
Discussion
To our knowledge, this is the largest multi-institutional study to date focusing on conservative management outcomes for R-USD. The majority of patients (80%) who were placed on a conservative management regimen over a median follow-up of 15.0 months were able to avoid invasive surgery or permanent indwelling catheterization with stable serum creatinine levels, uroflowmetry values, and post-void residual measurements. UI rates were not affected by conservative strategies, and this is an important reason why many patients elect to pursue conservative treatment rather than urethroplasty, which leads to new or worsening UI in 7% to 50% of patients [5,6,8,9,10,11]. Given that 34% of this population developed a UTI and 15% developed an AUR episode requiring urgent intervention, it is important to counsel patients on these risks when discussing stricture management options. There were few other serious stricture-related complications, including hospitalizations for urosepsis and development of severe or end-stage chronic kidney disease. Notably, the incidence of UTIs was significantly higher in the failure group (P = 0.03), and thus patients who develop UTIs should be monitored more carefully.
Our observational retrospective cohort is consistent with other studies on R-USD in that a majority of patients (97%) underwent radiotherapy for treatment of prostate cancer [17], and a majority of strictures were bulbomembranous (75%) [9,18]. Median stricture length was 2.0 cm, which is important to consider because the American Urological Association guidelines for male urethral stricture recommend initially offering urethroplasty for bulbar urethral strictures ≥ 2 cm [16]. However, our cohort had a median age of 75.4 years and a median CCI of 6 (corresponding to a predicted 10-year survival rate of approximately 2.25%), highlighting the fact that this patient population is often elderly with significant comorbidities, which can negatively impact their candidacy for urethral reconstructive surgery [19]. Additionally, a majority of our patients already presented with UI before stricture management. One of the key challenging decisions that patients and physicians must make in this scenario is whether to proceed with urethroplasty with the potential need for subsequent AUS. There is an inherent increased risk of AUS erosion in the setting of prior radiation, and an even higher risk of erosion in patients who have had both prior radiation and urethroplasty [12,13,14].
In a 2009 study by Sullivan et al., 38 patients who developed R-USD after high-dose brachytherapy were followed to determine the need for intervention based on their stricture disease and symptoms [20]. All patients were initially treated with dilation or DVIU, with 49% requiring further endoscopic management or intermittent catheterization and only 1 patient proceeding to urethroplasty. Our study included multiple forms of radiotherapy and demonstrated similar results with respect to the need for repeat intervention, suggesting that although the risk of development of R-USD may differ between radiation modalities, the progression and outcomes may be similar once the stricture has developed.
The genesis for this study was patient-driven, as with many clinical studies. Not surprisingly, many patients hope to avoid invasive reconstructive surgery if possible and desire information on the efficacy and safety of pursuing more conservative approaches. There is a paucity of recent literature on conservative management specifically for R-USD and the unique characteristics of these strictures. This disease process is challenging to manage surgically, even in expert hands, and carries a well-documented risk of stricture recurrence and either new or worsening postoperative UI. Additionally, patients undergoing urethroplasty complicated by bothersome UI need to wait an additional 6 months before pursuing AUS placement. As seen in our cohort, R-USD also commonly occurs in elderly patients with multiple comorbidities at baseline. For all these reasons, we felt it was important to further evaluate less invasive treatment strategies for R-USD at our reconstructive centers.
Our study has several limitations, including its retrospective nature. A prospective study with direct randomization to a conservative management arm and a urethral reconstruction arm would allow for better comparison of efficacy and safety. Furthermore, separately analyzing and comparing each conservative management technique may also be helpful but would not adequately reflect real-life clinical practice. For example, some patients may not be able to continue to effectively perform CIC over time or may be unable to tolerate CIC because of radiation-induced lower urinary tract sensitivity/cystitis-like symptoms and thus require endoscopic interventions instead. Selection bias is present, as this cohort focuses on those patients who specifically pursued conservative strategies after thorough patient-centered counseling on all available treatment options. Nevertheless, we strongly believe there is utility in assessing the efficacy of such strategies in this patient population. Further analysis of this population over longer follow-up with robust patient-reported outcome data should be pursued to assess how many patients will be successfully managed with conservative techniques indefinitely. The potential long-term consequences of repetitive conservative interventions in worsening the USD must be considered when using this treatment approach [21]. This study is not advocating for conservative management over surgical reconstruction for all patients with R-USD, as many patients do benefit from both anastomotic and substitution urethroplasty techniques [10,22,23]. However, the management of USD at its core is a quality-of-life issue with often more than one lower urinary tract symptom involved. Patients should be counseled on all available treatment options for this disease process to make a well-informed decision that meets their goals of care. This study provides important data for all urology providers, and specifically reconstructive urologists, to improve patient counseling, refine clinical decision-making, and assess which patients should be followed more closely. Regardless of treatment approach, we strongly advocate for fellowship-trained reconstructive urologists to manage this complex and challenging disease process to optimize outcomes.
Conclusion
In short-term follow-up, conservative management strategies for R-USD, such as endoscopic techniques and CIC, appear to be effective for most elderly patients with comorbidities. This is important to consider in these patients, who may not be optimal surgical candidates and in patients who strongly desire to avoid invasive surgery, the risk of worsening UI, or permanent indwelling catheterization. Close observation is warranted because of the risk of UTIs and AUR.
The potential long-term consequences of repetitive conservative interventions must be considered as well. Ultimately, management decisions should focus on achieving patient-specific goals of care.
Acknowledgments
The Biostatistics, Epidemiology, and Research Design (BERD) Center of Tufts Clinical and Translational Science Institute (CTSI) provided assistance with statistical analysis.
Conflicts of Interest
None declared.
Abbreviations
| AUR | acute urinary retention |
| AUS | artificial urinary sphincter |
| CCI | Charlson comorbidity index |
| CIC | clean intermittent catheterization |
| DVIU | direct visual internal urethrotomy |
| R-USD | radiation-induced urethral stricture disease |
| UI | urinary incontinence |
| UTI | urinary tract infection |
References
- Chen, J.; Oromendia, C.; Halpern, J.A.; Ballman, K.V. National trends in management of localized prostate cancer: A population based analysis 2004-2013. Prostate 2018, 78, 512–520. [Google Scholar] [CrossRef] [PubMed]
- Hofer, M.D.; Liu, J.S.; Morey, A.F. Treatment of radiation-induced urethral strictures. Urol. Clin. N. Am. 2017, 44, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Elliott, S.P.; Meng, M.V.; Elkin, E.P.; McAninch, J.W.; Duchane, J.; Carroll, P.R.; et al. CaPSURE Investigators. Incidence of urethral stricture after primary treatment for prostate cancer: Data from CaPSURE. J. Urol. 2007, 178, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Awad, M.A.; Gaither, T.W.; Osterberg, E.C.; Murphy, G.P.; Baradaran, N.; Breyer, B.N. Prostate cancer radiation and urethral strictures: A systematic review and meta-analysis. Prostate Cancer Prostatic Dis. 2018, 21, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Glass, A.S.; McAninch, J.W.; Zaid, U.B.; Cinman, N.M.; Breyer, B.N. Urethroplasty after radiation for prostate cancer. Urology 2012, 79, 1402–1405. [Google Scholar] [CrossRef] [PubMed]
- Meeks, J.J.; Brandes, S.B.; Morey, A.F.; Thom, M.; Mehdiratta, N.; Valadez, C.; et al. Urethroplasty for radiotherapy induced bulbomembranous strictures: A multi-institutional experience. J. Urol. 2011, 185, 1761–1765. [Google Scholar] [CrossRef] [PubMed]
- Meeks, J.J.; Erickson, B.A.; Granieri, M.A.; Gonzalez, C.M. Stricture recurrence after urethroplasty: A systematic review. J. Urol. 2009, 182, 1266–1270. [Google Scholar] [CrossRef] [PubMed]
- Chung, P.H.; Esposito, P.; Wessells, H.; Voelzke, B.B. Incidence of stress urinary incontinence after posterior urethroplasty for radiation-induced urethral strictures. Urology 2018, 114, 188–192. [Google Scholar] [CrossRef] [PubMed]
- Hofer, M.D.; Zhao, L.C.; Morey, A.; Scott, J.F.; Chang, A.J.; Brandes, S.B.; et al. Outcomes after urethroplasty for radiotherapy induced bulbomembranous urethral stricture disease. J. Urol. 2014, 191, 1307–1312. [Google Scholar] [CrossRef] [PubMed]
- Policastro, C.G.; Simhan, J.; Martins, F.E.; Lumen, N.; Venkatesan, K.; Angulo, J.C.; et al. A multi-institutional critical assessment of dorsal onlay urethroplasty for post-radiation urethral stenosis. World J. Urol. 2021, 39, 2669–2675. [Google Scholar] [CrossRef] [PubMed]
- Ahyai, S.A.; Schmid, M.; Kuhl, M.; Kluth, L.A.; Soave, A.; Riechardt, S.; et al. Outcomes of ventral onlay buccal mucosa graft urethroplasty in patients after radiotherapy. J. Urol. 2015, 194, 441–446. [Google Scholar] [CrossRef] [PubMed]
- Brant, W.O.; Erickson, B.A.; Elliott, S.P.; Powell, C.; Alsikafi, N.; McClung, C.; et al. Risk factors for erosion of artificial urinary sphincters: A multicenter prospective study. Urology 2014, 84, 934–938. [Google Scholar] [CrossRef] [PubMed]
- McGeady, J.B.; McAninch, J.W.; Truesdale, M.D.; Blaschko, S.D.; Kenfield, S.; Breyer, B.N. Artificial urinary sphincter placement in compromised urethras and survival: A comparison of virgin, radiated and reoperative cases. J. Urol. 2014, 192, 1756–1761. [Google Scholar] [CrossRef] [PubMed]
- Fuller, T.W.; Ballon-Landa, E.; Gallo, K.; et al. Outcomes and risk factors of revision and replacement artificial urinary sphincter implantation in radiated and nonradiated cases. J. Urol. 2020, 204, 110–114. [Google Scholar] [CrossRef] [PubMed]
- Herschorn, S.; Elliott, S.; Coburn, M.; Wessells, H.; Zinman, L. SIU/ICUD Consultation on urethral strictures: Posterior urethral stenosis after treatment of prostate cancer. Urology 2014, 83, S59–70. [Google Scholar] [CrossRef] [PubMed]
- Wessells, H.; Angermeier, K.W.; Elliott, S.; Gonzalez, C.M.; Kodama, R.; Peterson, A.C.; et al. Male urethral stricture: American Urological Association guideline. J. Urol. 2017, 197, 182–190. [Google Scholar] [CrossRef] [PubMed]
- Vetterlein, M.W.; Kluth, L.A.; Zumstein, V.; Meyer, C.P.; Ludwig, T.A.; Soave, A.; et al. Buccal mucosal graft urethroplasty for radiation-induced urethral strictures: An evaluation using the extended urethral stricture surgery patient-reported outcome measure (USS PROM). World J. Urol. 2020, 38, 2863–2872. [Google Scholar] [CrossRef] [PubMed]
- Merrick, G.S.; Butler, W.M.; Wallner, K.E.; Galbreath, R.W.; Anderson, R.L.; Allen, Z.A.; et al. Risk factors for the development of prostate brachytherapy related urethral strictures. J. Urol. 2006, 175, 1376–1380. [Google Scholar] [CrossRef]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, L.; Williams, S.G.; Tai, K.H.; Foroudi, F.; Cleeve, L.; Duchesne, G.M. Urethral stricture following high dose rate brachytherapy for prostate cancer. Radiother. Oncol. 2009, 91, 232–236. [Google Scholar] [CrossRef]
- Hudak, S.J.; Atkinson, T.H.; Morey, A.F. Repeat transurethral manipulation of bulbar urethral strictures is associated with increased stricture complexity and prolonged disease duration. J. Urol. 2012, 187, 1691–1695. [Google Scholar] [CrossRef] [PubMed]
- Keith, C.G.; Davenport, M.T.; Kavoussi, M.; Yi, Y.A.; Bergeson, R.L.; Morey, A.F. Long-term outcomes of anastomotic urethroplasty for radiation-induced strictures. World J. Urol. 2020, 38, 3055–3060. [Google Scholar] [CrossRef] [PubMed]
- Rozanski, A.T.; Vanni, A.J. Ventral buccal mucosa graft urethroplasty with gracilis muscle flap for high risk, long segment urethral strictures: A 20-year experience. Urology 2020, 140, 178–180. [Google Scholar] [CrossRef] [PubMed]
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2022 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.