Vesicouterine Fistula in Burkina Faso: Report of 36 Cases in a Multicentric Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study design and period
2.2. Study site and population
2.3. Definition of variables
2.4. Analysis and measures
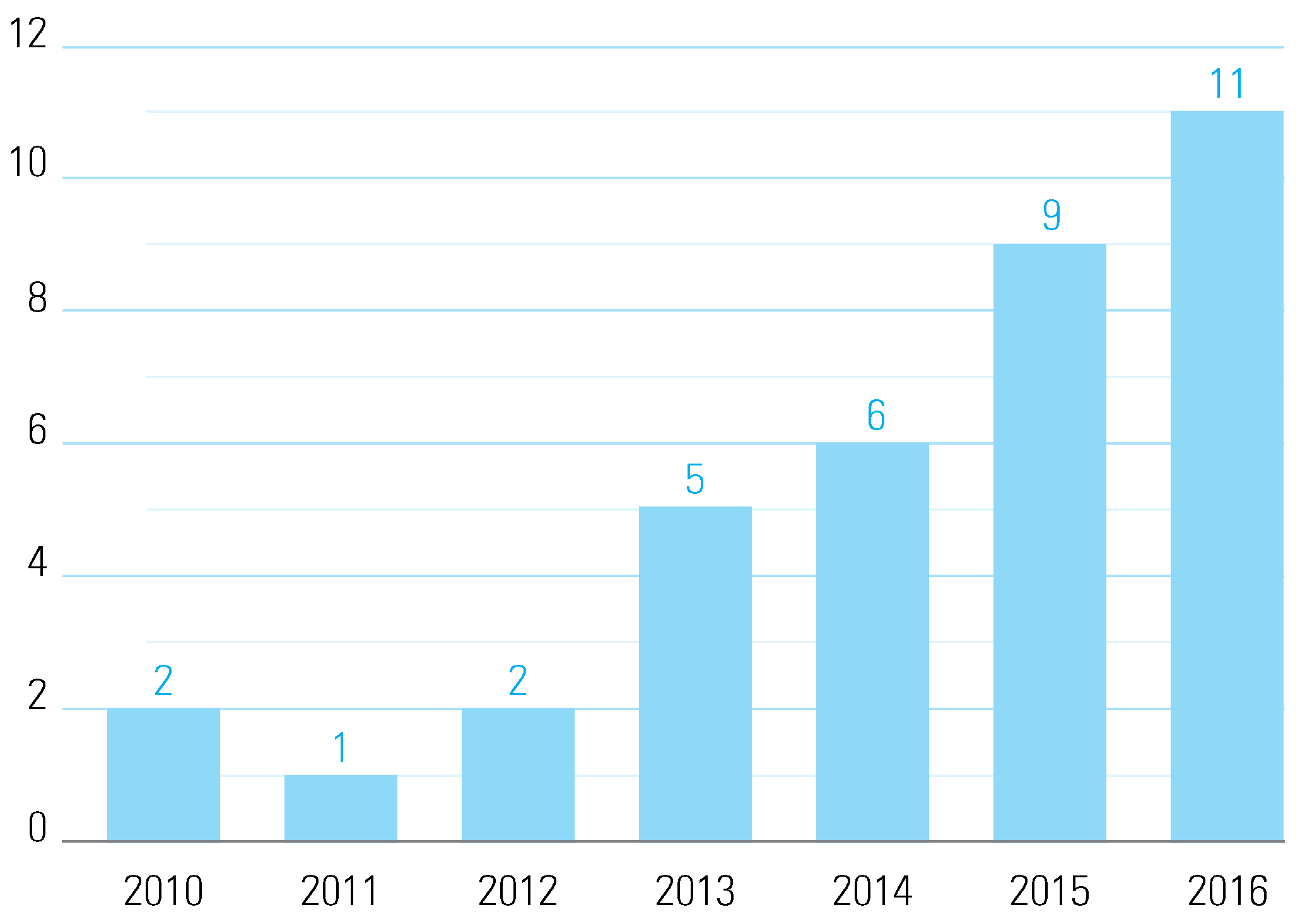
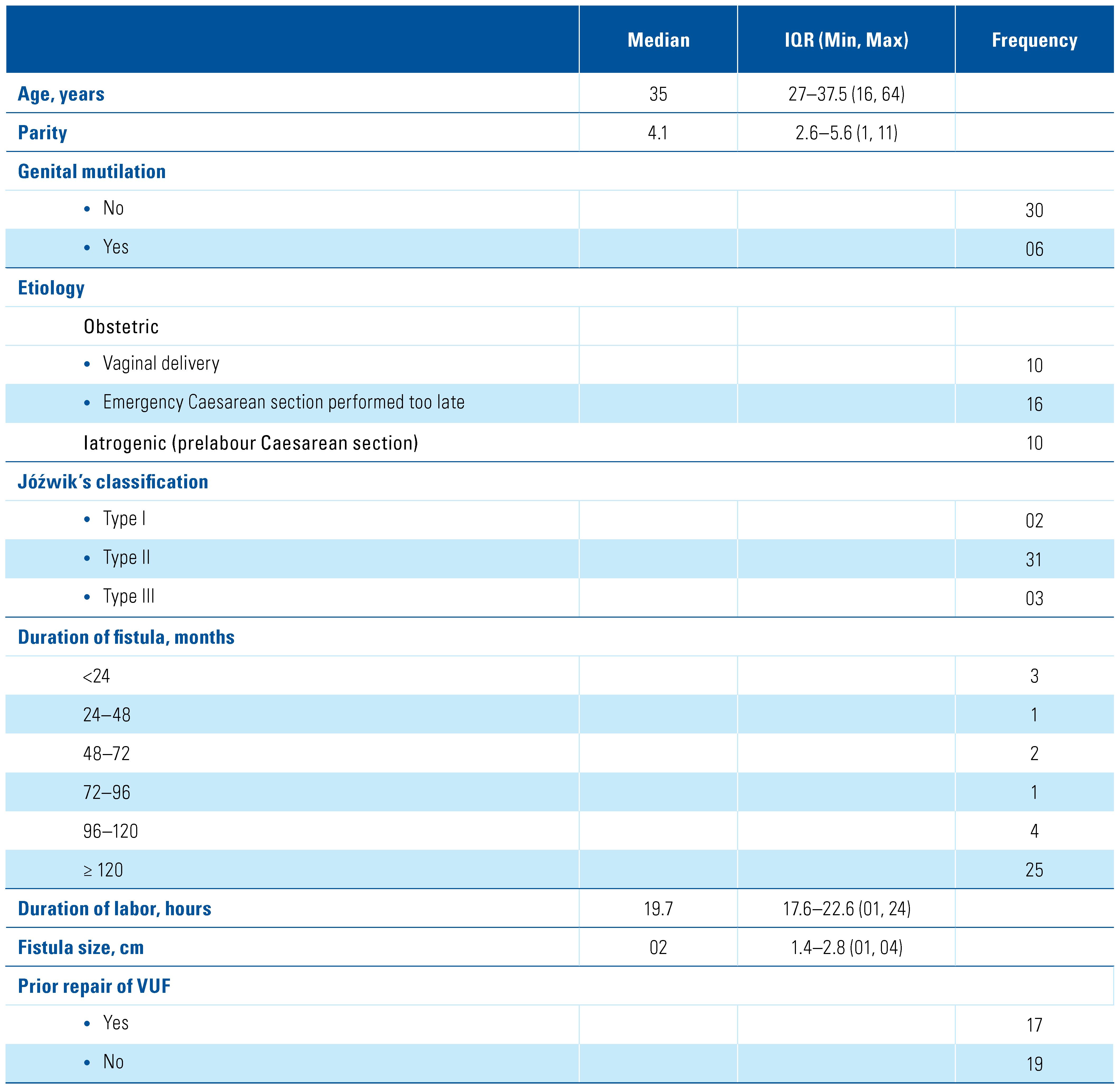
3. Results
4. Discussion
5. Conclusion
Acknowledgments
Conflicts of Interest
Abbreviations
| IQR | interquartile range |
| UGF | urogenital fistula |
| VUF | vesicouterine fistula |
References
- Drissi, M.; Karmouni, T.; Tazi, K.; El Khader, K.; Koutani, A.; Ibn Attya, A.; et al. Vesico-uterine fistulas: a 17-year experience. Prog Urol. 2008, 18, 173–176. [Google Scholar] [CrossRef]
- Karaltı, M.O.; Tınar, S.; Öztürk, N.T.; Öztekin, D.C.; Öztürk, D.C. A case with vesicouterine fistula: mini review. Arch Gynecol Obstet. 2012, 285, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Hodonou, R.; Hounnasso, P.; Biaou, O.; Akpo, C. Vesico-uterine fistula: about 15 cases at the Cotonou University Urology Clinic. Prog Urol. 2002, 12, 641–645. [Google Scholar]
- Alamoudi, O.J.; AlTheneyan, M.A.; Aldhaam, N.; Moazin, M. Early robotic repair of vesicouterine fistula: A case report and literature review. Urol Case Rep. 2017, 11, 76–78. [Google Scholar] [CrossRef] [PubMed]
- Sefrioui, O.; Benabbes Taarji, H.; Azyez, M.; Aboulfalah, A.; El Karroumi, M.; Matar, N.; et al. Vesico-uterine fistulas of obstetrical origin. About 3 cases. Ann Urol (Paris). 2002, 36, 376–380. [Google Scholar] [CrossRef]
- Kaboré, F.A.; Kambou, T.; Ouattara, A.; Zango, B.; Yaméogo, C.; Kirakoya, B.; et al. Epidemiological, etiological aspects and psychosocial impact of urogenital fistula in a cohort of 170 consecutive patients managed in three centers in Burkina Faso from 2010 to 2012. Prog Urol. 2014, 24, 526–532. [Google Scholar]
- Youssef, A.F. The uterine isthmus and its sphincter mechanism, a radiographic study. I. The uterine isthmus under normal conditions. Am J Obstet Gynecol. 1958, 75, 1305–1319. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; Kohli, U.A.; Sood, A.; Tripathy, S.; Gupta, M. Vesicouterine fistula: Youssef’s syndrome. Med J Armed Forces India. 2015, 71, 175–177. [Google Scholar] [CrossRef]
- Sombié, I.; Meda, Z.C.; Savadogo, G.; Sanou, G.; Dadjoari, M. Trends in the rate and place of cesarean section deliveries in Burkina Faso. Santé Publique. 2017, 29, 133. [Google Scholar] [CrossRef]
- DiMarco, C.S.; DiMarco, D.S.; Klingele, C.J.; Gebhart, J.B. Vesicouterine fistula: A review of eight cases. Int Urogynecol, J. 2006, 17, 395–399. [Google Scholar] [CrossRef]
- Józwik, M.; Józwik, M. Clinical classification of vesicouterine fistula. Int J Gynecol Obstet. 2000, 70, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Saeed, S.; Nawaz, N.; Murtaza, B.; Mahmood, A. Urogenital fistula in females—A four years experience. Pak Armed Forces Med, J. 2016, 66, 361–366. [Google Scholar]
- Egziabher, T.G.; Eugene, N.; Ben, K.; Fredrick, K. Obstetric fistula management and predictors of successful closure among women attending a public tertiary hospital in Rwanda: a retrospective review of records. BMC Res Notes. 2015, 8, 774. [Google Scholar] [CrossRef] [PubMed]
- Richter, L.A.; Lee, H.; Nishimwe, A.; Niteka, L.C.; Kielb, S.J. Characteristics of genitourinary fistula in Kigali, Rwanda; 5-year trends. Urology. 2021, 150, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Benchekroun, A.; El Alj, H.A.; El Sayegh, H.; Lachkar, A.; Nouini, Y.; Benslimane, L.; et al. Les fistules vésico-vaginales: À propos de 1050 cas. Ann Urol. 2003, 37, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Hadzi-Djokic, J.B.; Pejcic, T.P.; Colovic, V.C. Vesico-uterine fistula: report of 14 cases. BJU Int. 2007, 100, 1361–1363. [Google Scholar] [CrossRef]
- Ouédraogo, C.M.; Ouédraogo, A.; Ouattara, A.; Lankoandé, J. The practice of cesarean section in a district hospital in Ouagadougou Epidemiological, clinical and prognostic aspects for 3,381 cases. Med Sante Trop. 2015, 25, 194–199. [Google Scholar] [PubMed]
- Józwik, M.; Józwik, M.; Łotocki, W. Vesicouterine fistula—An analysis of 24 cases from Poland. Int J Gynecol Obstet. 1997, 57, 169–172. [Google Scholar] [CrossRef] [PubMed]
- Birge, O.; Ozbey, E.G.; Erkan, M.M.; Arslan, D.; Kayar, I. Youssef’s syndrome following Cesarean section. Case Rep Obstet Gynecol. 2015, 2015, 1–4. [Google Scholar] [CrossRef]
- Yip, S.K.; Leung, T.Y. Vesicouterine fistula: an updated review. Int Urogynecol J Pelvic Floor Dysfunct. 1998, 9, 252–256. [Google Scholar] [CrossRef]
- Goyal, L.D. Vesicouterine fistula following vaginal birth after Caesarean section in a multiparous woman-a rare case report and review of literature. ARC Journal of Gynecology and Obstetrics. 2016, 1, 1–2. [Google Scholar] [CrossRef]
- Nouira, Y.; Feki, W.; Rhouma, S.B.; Salah, I.B.; Horchani, A. Vesicouterine fistula as a complication of forceps delivery: A case report. Int Urogynecol J Pelvic Floor Dysfunct. 2005, 16, 512–514. [Google Scholar] [CrossRef] [PubMed]
- Bastakoti, R.; Saha, R. Conservative management of uterovesical fistula following primary Caesarean section. Journal of Kathmandu Medical College. 2013, 2, 211–113. [Google Scholar] [CrossRef]
- Józwik, M.; Józwik, M. Spontaneous closure of vesicouterine fistula. Account for effective hormonal treatment. Urol Int. 1999, 62, 183–187. [Google Scholar] [CrossRef]
- Sylla, C.; Fall, P.A.; Diallo, A.B.; Ndoye, A.K.; Ba, M.; Gueye, S.M.; et al. Vesicouterine fistulas: about 5 cases. Prog Urol. 2000, 634–637. [Google Scholar]
- Sjøveian, S.; Vangen, S.; Mukwege, D.; Onsrud, M. Surgical outcome of obstetric fistula: a retrospective analysis of 595 patients. Acta Obstet Gynecol Scand. 2011, 90, 753–760. [Google Scholar] [CrossRef]
- Meda, I.B.; Millogo, T.; Baguiya, A.; Ouédraogo/Nikiema, L.; Coulibaly, A.; Kouanda, S. Rate of and factors associated with indications for cesarean deliveries: results of a national review in Burkina Faso. Int J Gynaecol Obstet. 2016, 135 (Suppl. 1), S51–S57. [Google Scholar]
 |
This is an open access article under the terms of a license that permits non-commercial use, provided the original work is properly cited. © 2021 The Authors. Société Internationale d'Urologie Journal, published by the Société Internationale d'Urologie, Canada.
Share and Cite
Ouedraogo, B.; Kirakoya, B.; Kabore, M.; Millogo, A.; Ouattara, A.; Kaboré, F.A. Vesicouterine Fistula in Burkina Faso: Report of 36 Cases in a Multicentric Study. Soc. Int. Urol. J. 2021, 2, 210-215. https://doi.org/10.48083/NFMO2987
Ouedraogo B, Kirakoya B, Kabore M, Millogo A, Ouattara A, Kaboré FA. Vesicouterine Fistula in Burkina Faso: Report of 36 Cases in a Multicentric Study. Société Internationale d’Urologie Journal. 2021; 2(4):210-215. https://doi.org/10.48083/NFMO2987
Chicago/Turabian StyleOuedraogo, Boureima, Brahima Kirakoya, Moussa Kabore, Adama Millogo, Adama Ouattara, and Fasnewinde Aristide Kaboré. 2021. "Vesicouterine Fistula in Burkina Faso: Report of 36 Cases in a Multicentric Study" Société Internationale d’Urologie Journal 2, no. 4: 210-215. https://doi.org/10.48083/NFMO2987
APA StyleOuedraogo, B., Kirakoya, B., Kabore, M., Millogo, A., Ouattara, A., & Kaboré, F. A. (2021). Vesicouterine Fistula in Burkina Faso: Report of 36 Cases in a Multicentric Study. Société Internationale d’Urologie Journal, 2(4), 210-215. https://doi.org/10.48083/NFMO2987




