Beneficial Impact of Vaccination Against SARS-CoV-2 on the Mental Health of IPF Patients
Abstract
Highlights
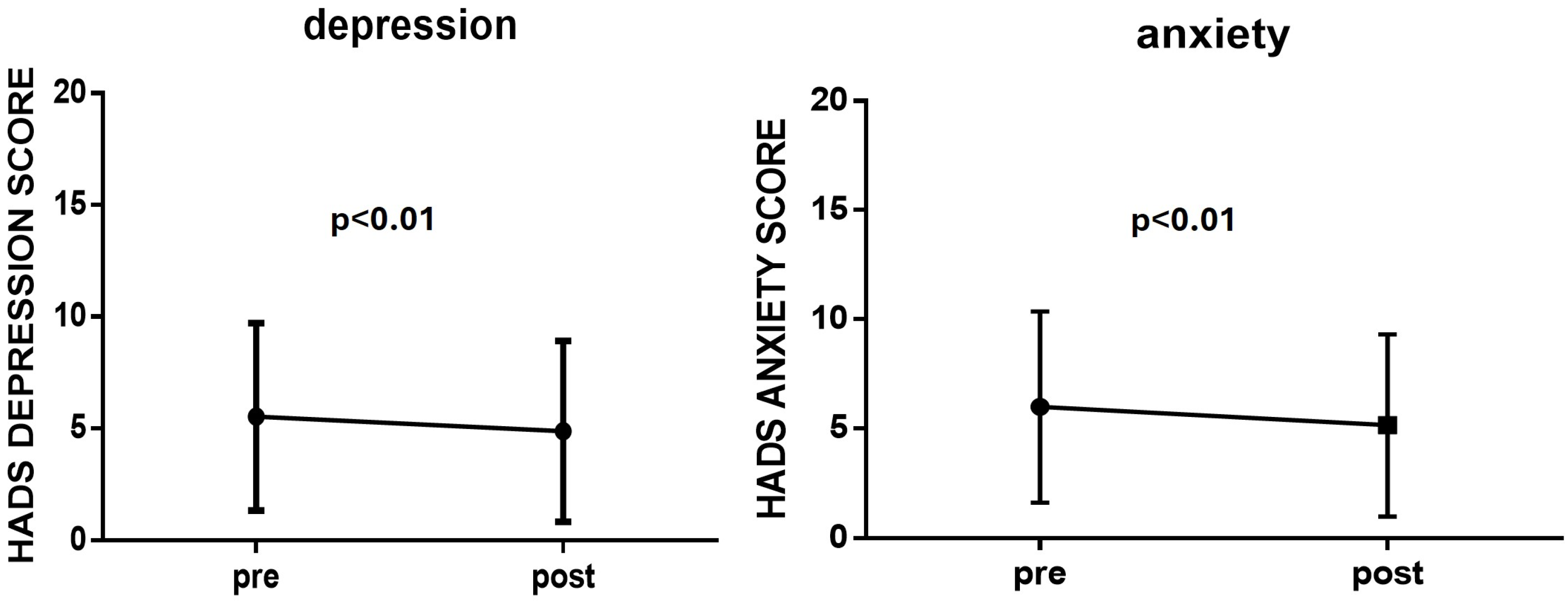
- A higher Hospital Anxiety and Depression Scale score was detected before vaccination against COVID-19.
- A significant decrease in both anxiety and depression scores one month after the first dose of vaccines in IPF patients was found.
- It seems that vaccination also offered an additional beneficial effect on depression and anxiety in IPF patients.
- Vaccination against SARS-COV-2 offered at least a beneficial effect on the inception of patients’ mental health, an important issue in patients’ well-being and quality of life, in the course of IPF.
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raghu, G.; Remy-Jardin, M.; Richeldi, L.; Thomson, C.C.; Inoue, Y.; Johkoh, T.; Kreuter, M.; Lynch, D.A.; Maher, T.M.; Martinez, F.J.; et al. Idiopathic Pulmonary Fibrosis (an Update) and Progressive Pulmonary Fibrosis in Adults: An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline. Am. J. Respir. Crit. Care Med. 2022, 205, e18–e47. [Google Scholar] [CrossRef] [PubMed]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Ou, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Esposito, A.J.; Menon, A.A.; Ghosh, A.J.; Putman, R.K.; Fredenburgh, L.E.; El-Chemaly, S.Y.; Goldberg, H.J.; Baron, R.M.; Hunninghake, G.M.; Doyle, T.J. Increased Odds of Death for Patients with Interstitial Lung Disease and COVID-19: A Case–Control Study. Am. J. Respir. Crit. Care Med. 2020, 202, 1710–1713. [Google Scholar] [CrossRef]
- Papiris, S.A.; Bouros, D.; Markopoulou, K.; Kolilekas, L.; Papaioannou, A.I.; Tzilas, V.; Tzouvelekis, A.; Fouka, E.; Papakosta, D.; Daniil, Z.; et al. Early COVID-19 lockdown in Greece and idiopathic pulmonary fibrosis: A beneficial “impact” beyond any expectation. Eur. Respir. J. 2021, 57, 2003111. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Choi, S.M.; Lee, Y.J.; Cho, Y.-J.; Yoon, H.I.; Lee, J.-H.; Lee, C.-T.; Park, J.S. Clinical impact of depression and anxiety in patients with idiopathic pulmonary fibrosis. PLoS ONE 2017, 12, e0184300. [Google Scholar] [CrossRef] [PubMed]
- Tzouvelekis, A.; Karampitsakos, T.; Kourtidou, S.; Bouros, E.; Tzilas, V.; Katsaras, M.; Antonou, C.; Dassiou, M.; Bouros, D. Impact of Depression on Patients With Idiopathic Pulmonary Fibrosis. Front. Med. 2020, 7, 29. [Google Scholar] [CrossRef] [PubMed]
- Ryerson, C.J.; Berkeley, J.; Carrieri-Kohlman, V.L.; Pantilat, S.Z.; Landefeld, C.S.; Collard, H.R. Depression and functional status are strongly associated with dyspnea in interstitial lung disease. Chest 2011, 139, 609–616. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Michopoulos, I.; Douzenis, A.; Kalkavoura, C.; Christodoulou, C.; Michalopoulou, P.; Kalemi, G.; Fineti, K.; Patapis, P.; Protopapas, K.; Lykouras, L. Hospital Anxiety and Depression Scale (HADS): Validation in a Greek general hospital sample. Ann. Gen. Psychiatry 2008, 7, 4. [Google Scholar] [CrossRef]
- Tzanakis, N.; Samiou, M.; Lambiri, I.; Antoniou, K.; Siafakas, N.; Bouros, D. Evaluation of health-related quality-of-life and dyspnea scales in patients with idiopathic pulmonary fibrosis. Correlation with pulmonary function tests. Eur. J. Intern. Med. 2005, 16, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, K.; Howley, P. The impact of COVID-19 vaccination for mental well-being. Eur. Econ. Rev. 2022, 150, 104293. [Google Scholar] [CrossRef] [PubMed]
- Συστάσεις εμβολιασμού κατά την περίοδο της πανδημίας COVID19-Υπουργείο Υγείας. Available online: https://www.moh.gov.gr/articles/health/dieythynsh-dhmosias-ygieinhs/emboliasmoi/systaseis-emboliasmoy-kata-thn-periodo-ths-pandhmias-covid19 (accessed on 14 July 2024).
- Koltai, J.; Raifman, J.; Bor, J.; McKee, M.; Stuckler, D. COVID-19 Vaccination and Mental Health: A Difference-In-Difference Analysis of the Understanding America Study. Am. J. Prev. Med. 2022, 62, 679–687. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, R.C.; Wetherall, K.; Cleare, S.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.L.; O’Carroll, R.E.; O’Connor, D.B.; Platt, S.; Scowcroft, E.; et al. Mental health and well-being during the COVID-19 pandemic: Longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry J. Ment. Sci. 2021, 218, 326–333. [Google Scholar] [CrossRef]
- Willis, D.E.; Andersen, J.A.; Bryant-Moore, K.; Selig, J.P.; Long, C.R.; Felix, H.C.; Curran, G.M.; McElfish, P.A. COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 2021, 14, 2200–2207. [Google Scholar] [CrossRef]
| n = 180 | |
|---|---|
| Age (years), median (IQR) | 73.5 (68–78) |
| Gender (men), n (%) | 142 (78.9) |
| Smoking, n (%) | |
| Current | 94 (52.2) |
| Ex | 38 (21.1) |
| Disease duration (months), median (IQR) | 36 (20–53) |
| FVC (%), median (IQR) | 79 (64–91) |
| DLCO (%), median (IQR) | 46 (37–58) |
| Anti-fibrotic treatment (%) | 146 (81.1) |
| SARS-CoV-2 infection, n (%) | |
| Yes | 5 (2.8) |
| No | 175 (97.2) |
| HAD-Anxiety score before vaccination, median (IQR) | 6 (2–9) |
| HAD-Depression score before vaccination, median (IQR) | 5 (2–8) |
| Vaccination against influenza, n (%) | 177 (98.3) |
| Vaccination against Streptococcus pneumoniae, n (%) | 176 (97.8) |
| Intention towards vaccination against SARS-CoV-2, n (%) | 177 (98.3) |
| Comorbidities | |
| Coronary Artery Disease, n (%) | 29 (16.1) |
| Arterial hypertension, n (%) | 100 (55.6) |
| Diabetes mellitus, n (%) | 50 (27.8) |
| Cancer, n (%) | 18 (10) |
| Depression, n (%) | 23 (12.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Polish Respiratory Society. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomos, I.; Papaioannou, A.I.; Daniil, Z.I.; Dimeas, I.E.; Kirgou, P.; Gogali, A.; Tatsis, K.; Papanikolaou, I.; Tzilas, V.; Tzouvelekis, A.; et al. Beneficial Impact of Vaccination Against SARS-CoV-2 on the Mental Health of IPF Patients. Adv. Respir. Med. 2024, 92, 466-471. https://doi.org/10.3390/arm92060042
Tomos I, Papaioannou AI, Daniil ZI, Dimeas IE, Kirgou P, Gogali A, Tatsis K, Papanikolaou I, Tzilas V, Tzouvelekis A, et al. Beneficial Impact of Vaccination Against SARS-CoV-2 on the Mental Health of IPF Patients. Advances in Respiratory Medicine. 2024; 92(6):466-471. https://doi.org/10.3390/arm92060042
Chicago/Turabian StyleTomos, Ioannis, Andriana I. Papaioannou, Zoe I. Daniil, Ilias E. Dimeas, Paraskevi Kirgou, Athena Gogali, Konstantinos Tatsis, Ilias Papanikolaou, Vasilios Tzilas, Argyrios Tzouvelekis, and et al. 2024. "Beneficial Impact of Vaccination Against SARS-CoV-2 on the Mental Health of IPF Patients" Advances in Respiratory Medicine 92, no. 6: 466-471. https://doi.org/10.3390/arm92060042
APA StyleTomos, I., Papaioannou, A. I., Daniil, Z. I., Dimeas, I. E., Kirgou, P., Gogali, A., Tatsis, K., Papanikolaou, I., Tzilas, V., Tzouvelekis, A., Tsiri, P., Steiropoulos, P., Ntolios, P., Xyfteri, A., Antoniou, K., Symvoulakis, E., Haritou, A., Maniati, M., Kolilekas, L., ... Papiris, S. (2024). Beneficial Impact of Vaccination Against SARS-CoV-2 on the Mental Health of IPF Patients. Advances in Respiratory Medicine, 92(6), 466-471. https://doi.org/10.3390/arm92060042









