Detection and Classification of Knee Injuries from MR Images Using the MRNet Dataset with Progressively Operating Deep Learning Methods
Abstract
:1. Introduction
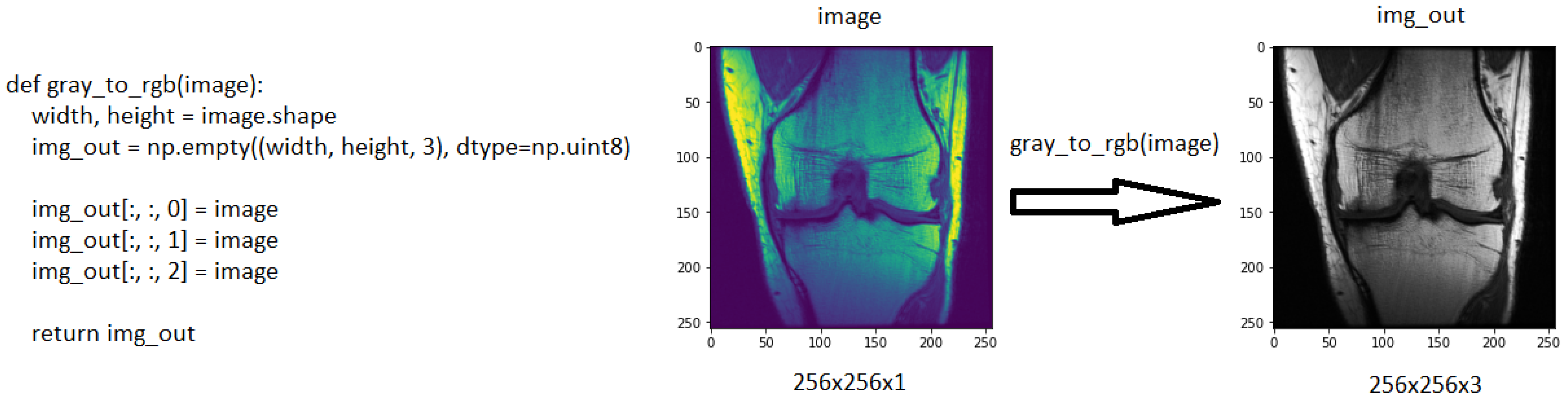
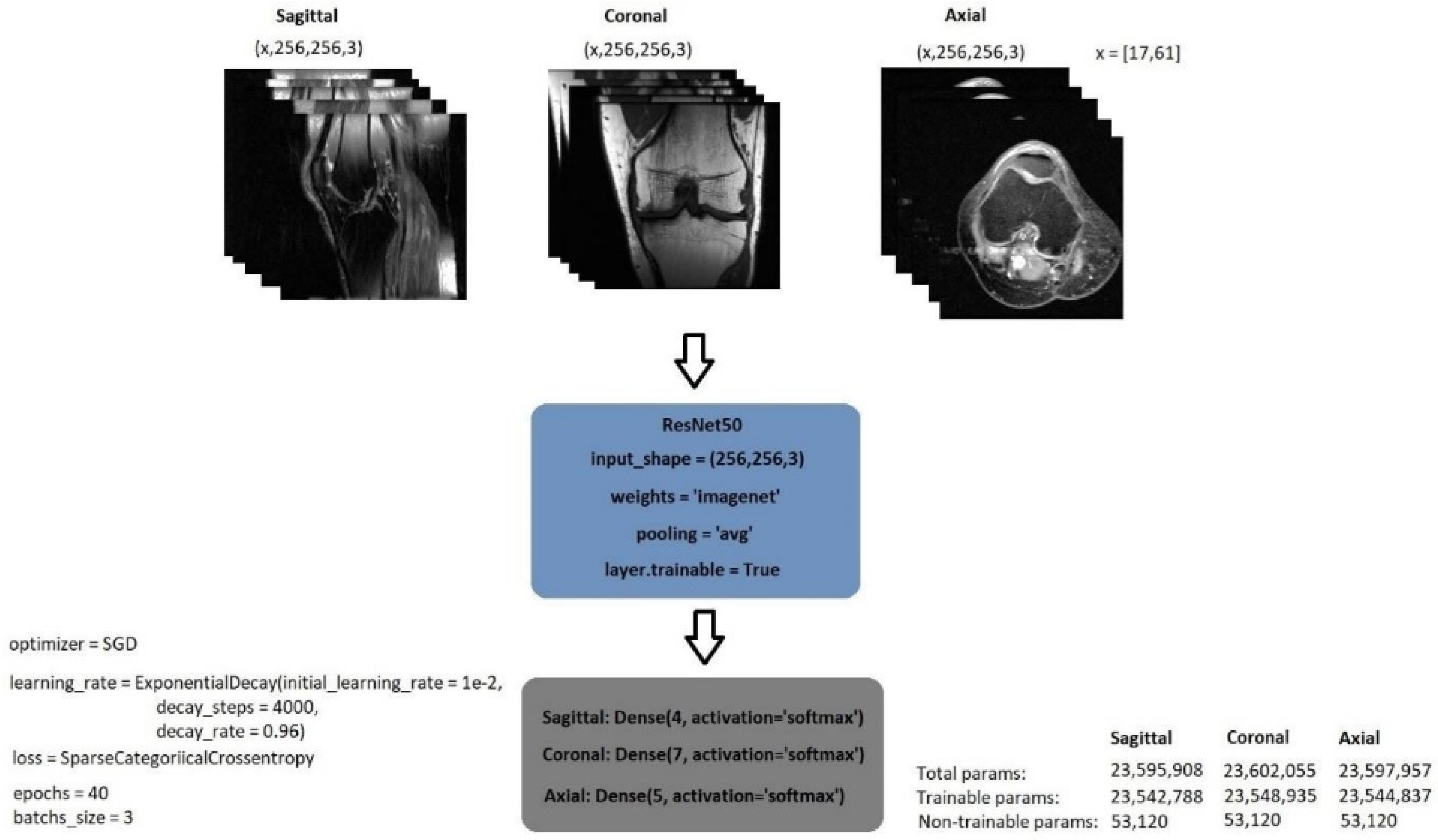
2. Materials and Methods
2.1. Dataset
2.2. Related Works
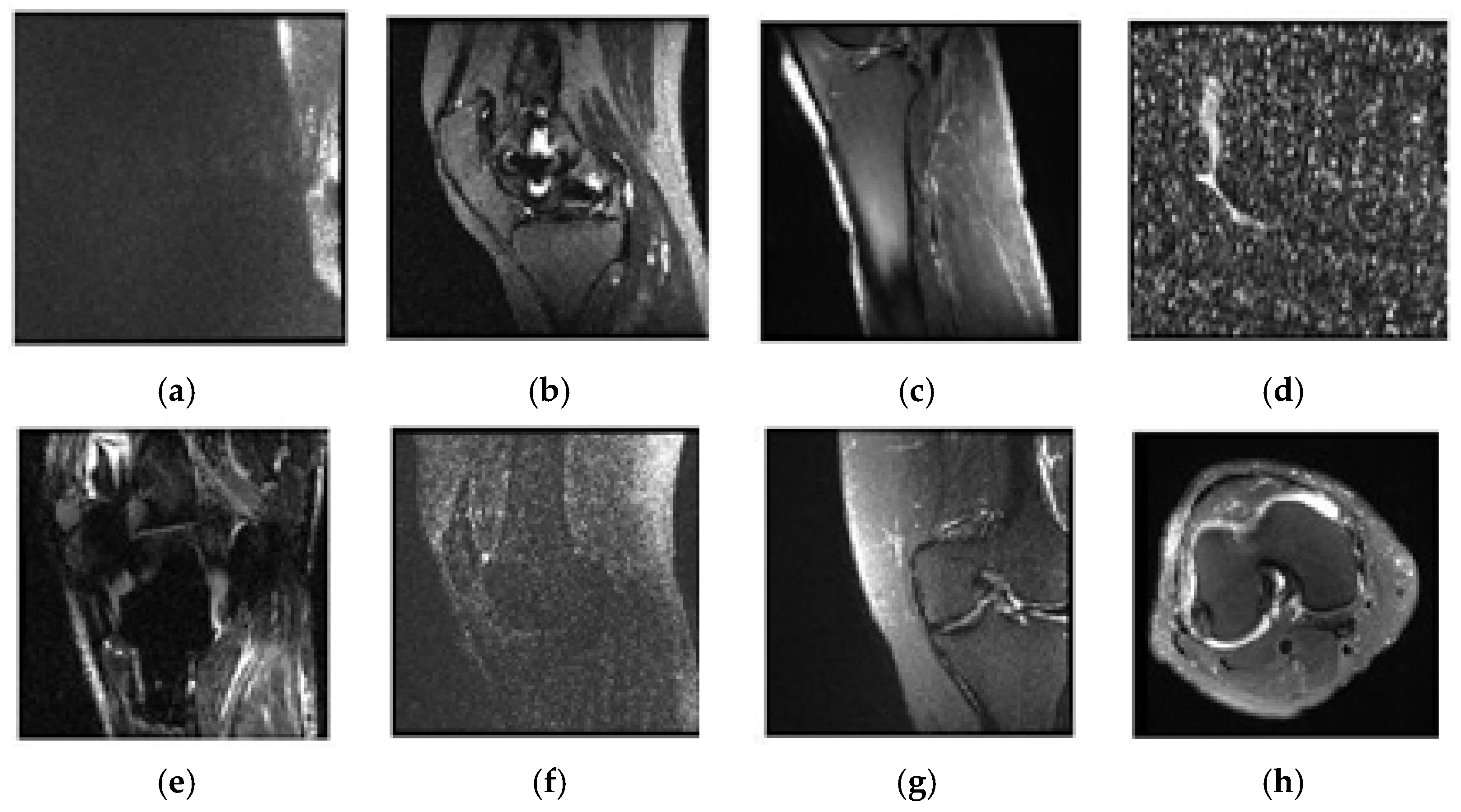
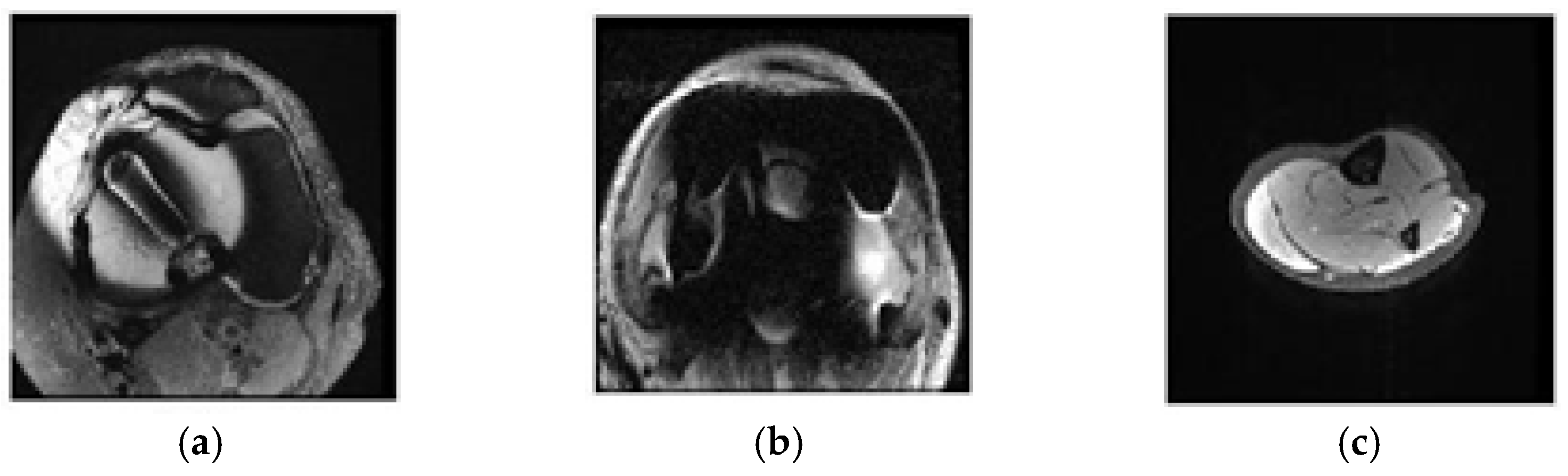
2.3. Selecting Eligible Data
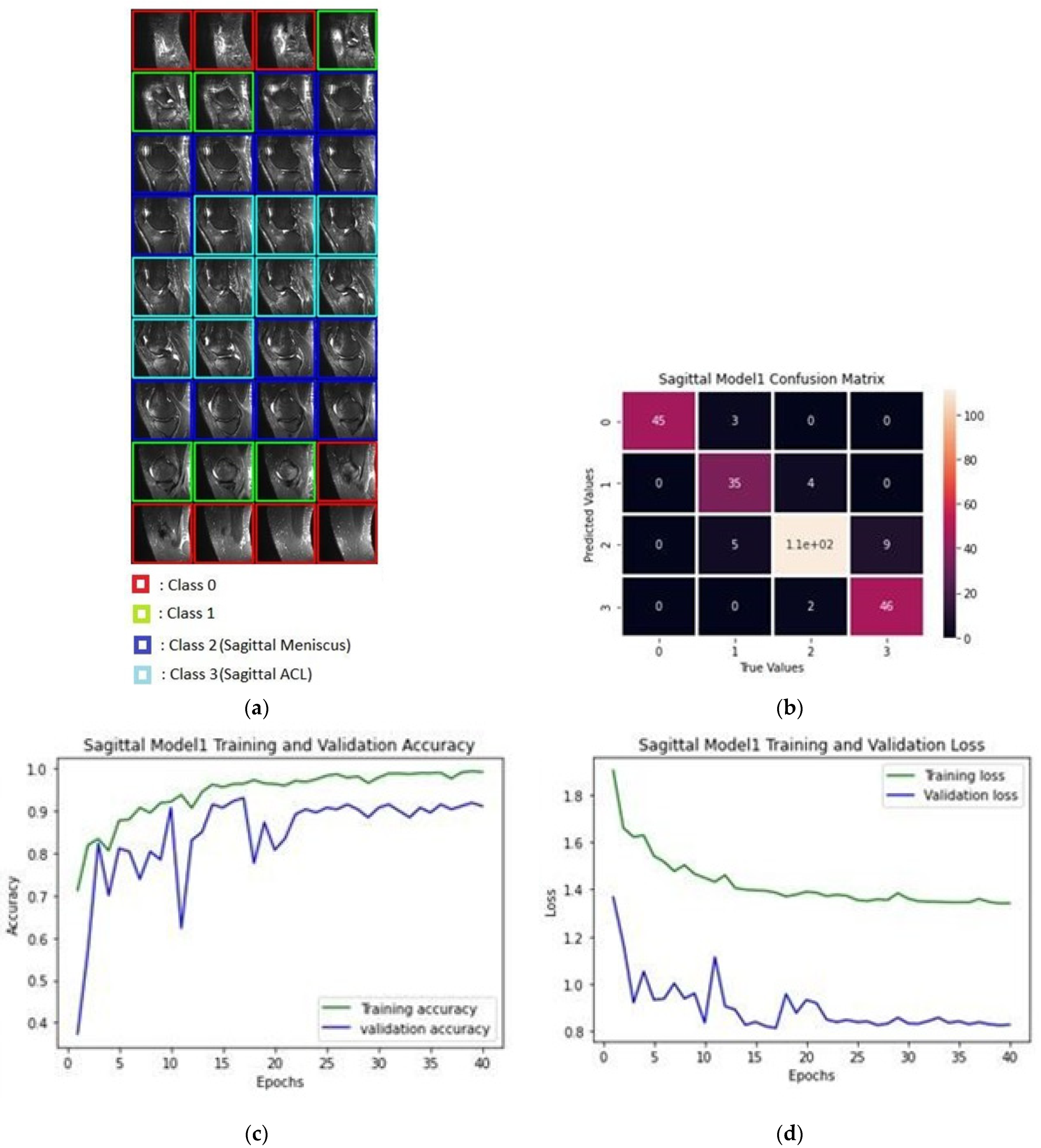
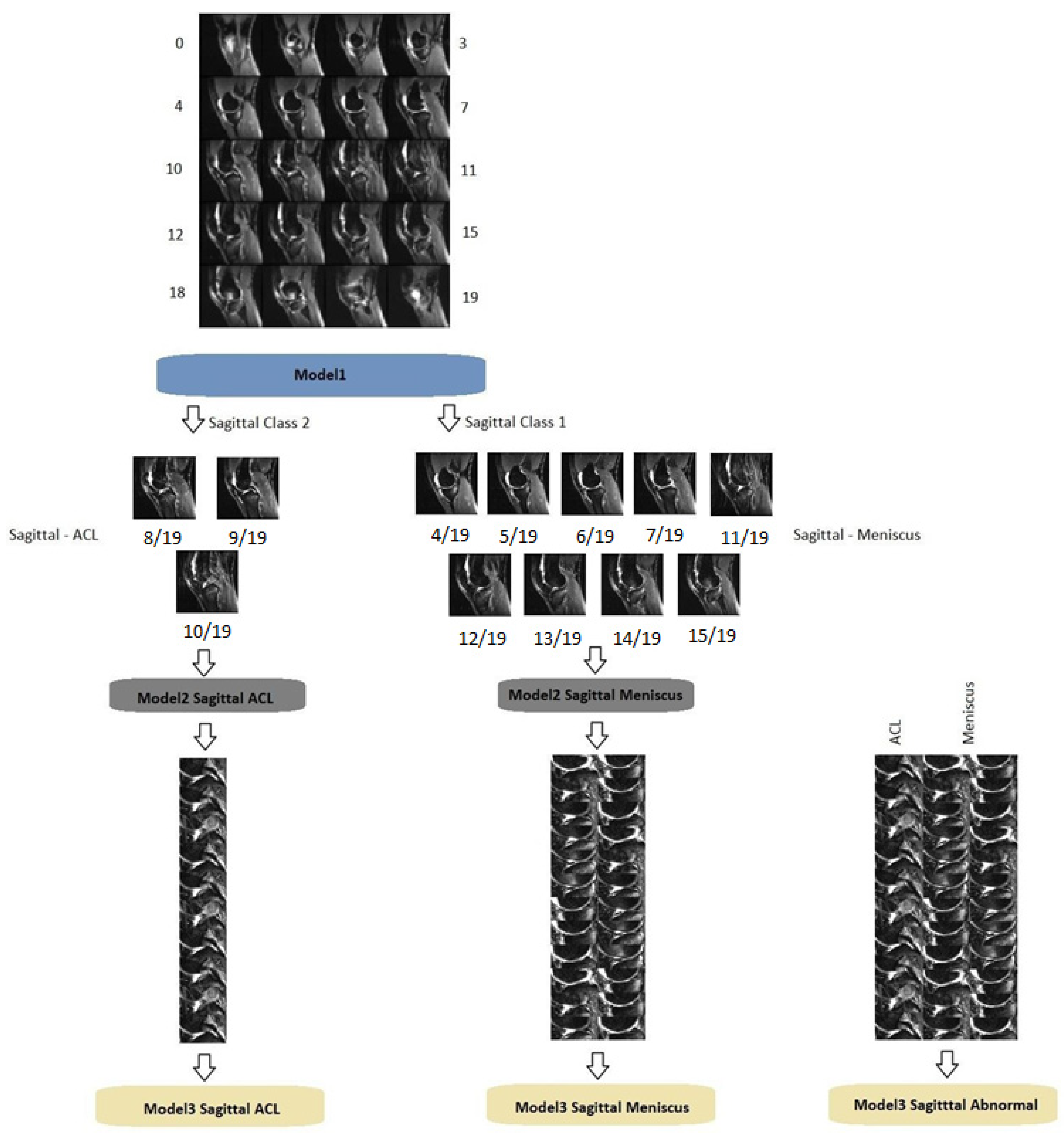
2.3.1. Classification of Sagittal Images and Results
2.3.2. Classification of Coronal Images and Results
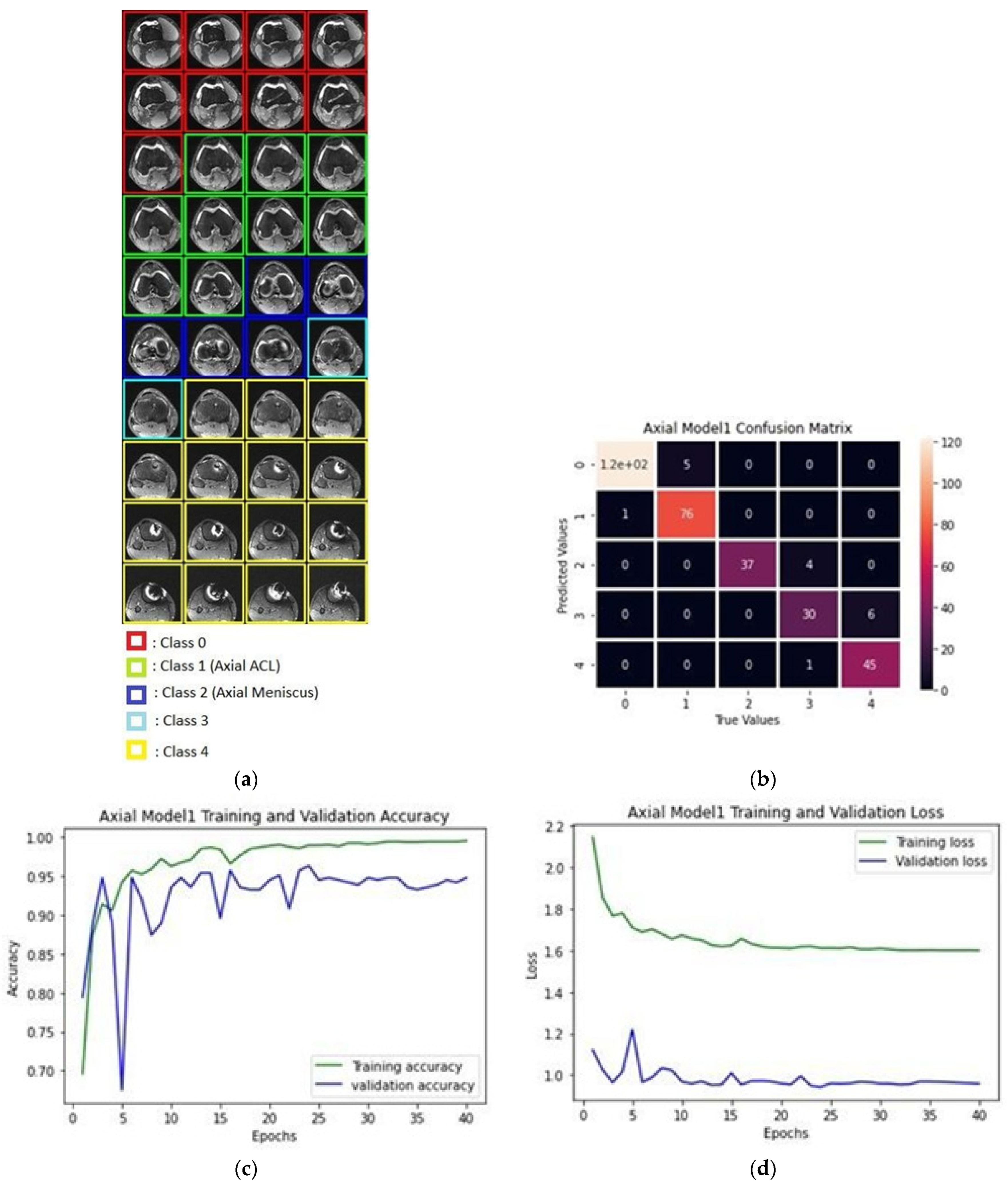
2.3.3. Classification of Axial Images and Results
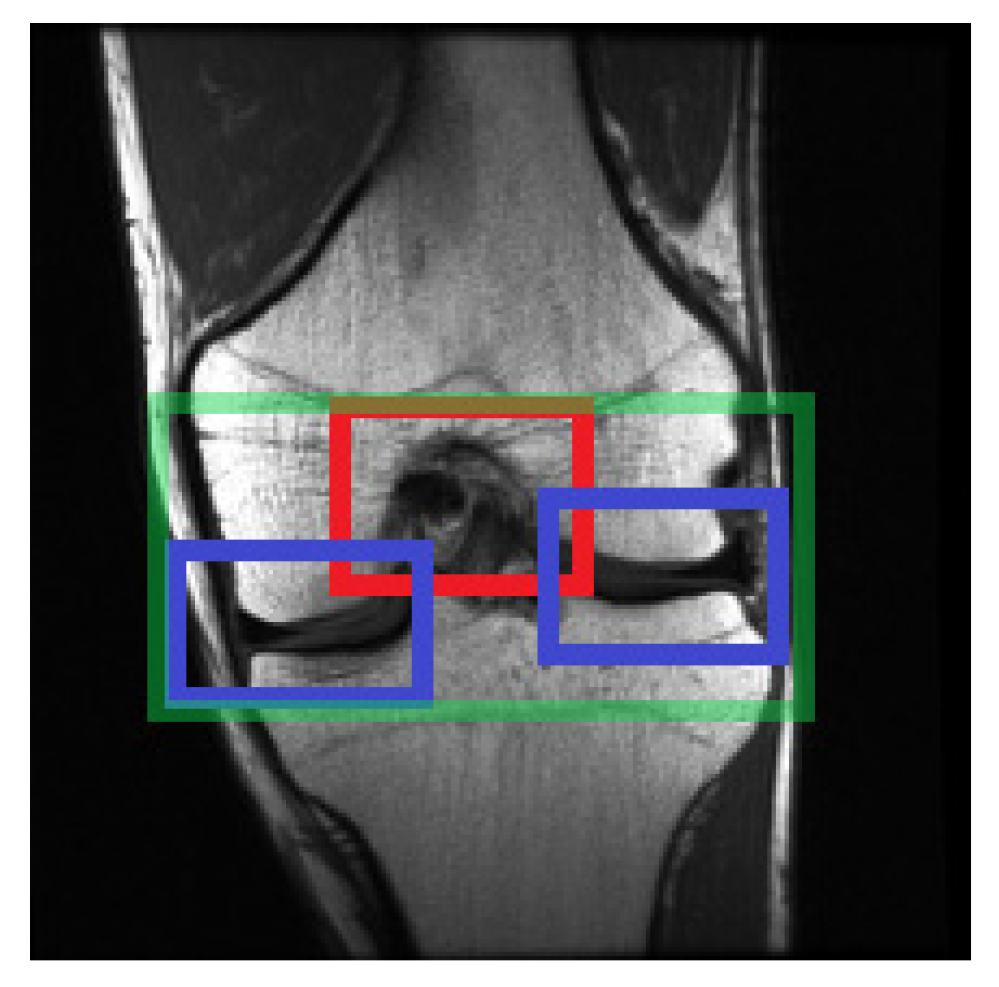
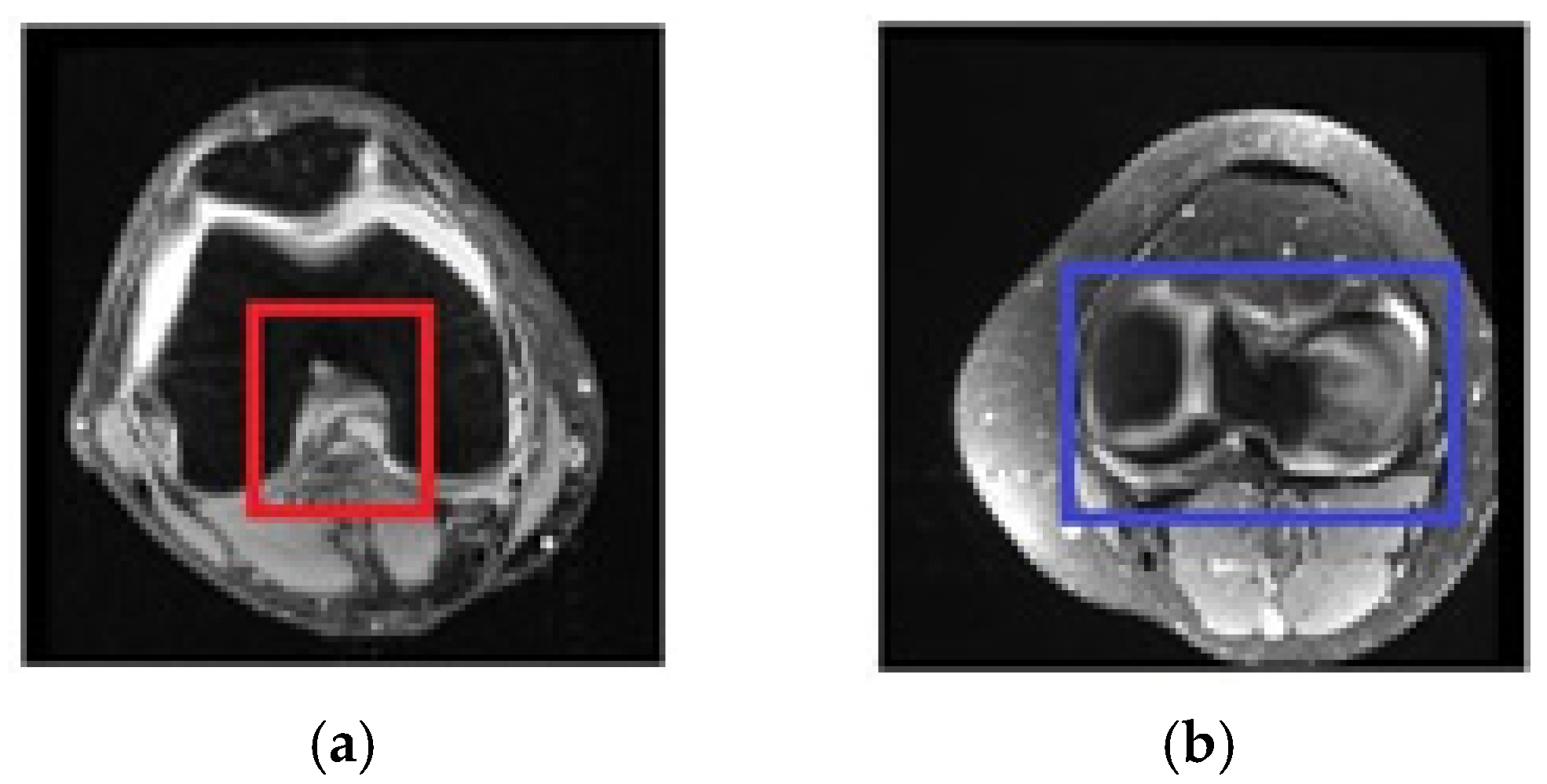
2.4. Selecting the Relevant Area
2.4.1. Selecting Relevant Areas on the Sagittal Axis
2.4.2. Selecting Relevant Regions on the Coronal Axis
2.4.3. Selecting Relevant Regions on the Axial Axis
2.4.4. Structure of the Region of Interest Model
2.5. Diagnosis
2.6. Structure of Progressively Operating Model
3. Results
- Classification of sick people as sick—“True positive”.
- Classification of healthy people as sick—“False positive”.
- Classification of healthy people as healthy—“True negative”.
- Classification of sick people as healthy—“False negative”.
4. Discussion
5. Conclusions
- For the first time, regions were classified and selected among the MR images in the diagnosis of knee problems, and successful results were achieved at the classification stage.
- The region of interest study was carried out in previous studies. However, convolutional neural networks and denoising autoencoders were employed for the first time to carry out a diagnostic study and were successful in detecting the region.
- Since our study goes through several deep learning models sequentially, it would provide later findings than other studies.
- Other study techniques, when undertaken in a hospital setting, may produce erroneous results since it is impossible to detect whether the image is damaged or over noisy.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kaul, V.; Enslin, S.; Gross, S.A. History of artificial intelligence in medicine. Gastrointest. Endosc. 2020, 92, 807–812. [Google Scholar] [CrossRef]
- Jin, D.; Harrison, A.P.; Zhang, L.; Yan, K.; Wang, Y.; Cai, J.; Miao, S.; Lu, L. Artificial intelligence in radiology. In Artificial Intelligence in Medicine, 1st ed.; Xing, L., Giger, M.L., Min, J.K., Eds.; Academic Press: London, UK, 2020; pp. 668–727. [Google Scholar]
- Amarasinghe, K.C.; Lopes, J.; Beraldo, J.; Kiss, N.; Bucknell, N.; Everitt, S.; Jackson, P.; Litchfield, N.; Denehy, L.; Blyth, B.J.; et al. A Deep Learning Model to Automate Skeletal Muscle Area Measurement on Computed Tomography Images. Front. Oncol. 2021, 11, 1135. [Google Scholar] [CrossRef]
- Seo, J.W.; Lim, S.H.; Jeong, J.G.; Kim, Y.J.; Kim, K.G.; Jeon, J.Y. A deep learning algorithm for automated measurement of vertebral body compression from X-ray images. Sci. Rep. 2021, 11, 13732. [Google Scholar] [CrossRef]
- Liu, S.; Wang, Y.; Yang, X.; Lei, B.; Liu, L.; Li, S.X.; Ni, D.; Wang, T. Deep Learning in Medical Ultrasound Analysis: A Review. Engineering 2019, 5, 261–275. [Google Scholar] [CrossRef]
- Tastan, A.; Hardalaç, N.; Kavak, S.B.; Hardalaç, F. Detection of Fetal Reactions to Maternal Voice Using Doppler Ultrasound Signals. In Proceedings of the 2018 International Conference on Artificial Intelligence and Data Processing (IDAP), Malatya, Turkey, 28–30 September 2018; pp. 1–6. [Google Scholar] [CrossRef]
- Ouyang, D.; Wu, Z.; He, B.; Zou, J. Deep learning for biomedical videos: Perspective and recommendations. In Artificial Intelligence in Medicine, 1st ed.; Xing, L., Giger, M.L., Min, J.K., Eds.; Academic Press: London, UK, 2020; pp. 132–162. [Google Scholar]
- Sreelakshmi, D.; Inthiyaz, S. A Review on Medical Image Denoising Algorithms. Biomed. Signal Process. Control. 2020, 61, 102036. [Google Scholar] [CrossRef]
- Liu, H.; Rashid, T.; Ware, J.; Jensen, P.; Austin, T.; Nasrallah, I.; Bryan, R.; Heckbert, S.; Habes, M. Adaptive Squeeze-and-Shrink Image Denoising for Improving Deep Detection of Celebral Microbleeds. In Proceedings of the MICCAI2021–24th International Conference on Medical Image Computing & Computer Assisted Intervention, Strasbourg, France, 27 September–1 October 2021. [Google Scholar] [CrossRef]
- Giovanni, B.; Olivier, L.M. Artificial Intelligence in Medicine: Today and Tomorrow. Front. Med. 2020, 7, 27. [Google Scholar] [CrossRef]
- McBee, M.P.; Awan, O.A.; Colucci, A.T.; Ghobadi, C.W.; Kadom, N.; Kansagra, A.P.; Tridandapani, S.; Aufdermann, W.F. Deep Learning in Radiology. Acad. Radiol. 2018, 25, 1472–1480. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ueda, D.; Shimazaki, A. Technical and clinical overview of deep learning in radiology. Jpn. J. Radiol. 2019, 37, 15–33. [Google Scholar] [CrossRef]
- Montagnon, E.; Cerny, M.; Cadrin-Chênevert, A.; Vincent, H.; Thomas, D.; Ilinca, A.; Vandenbroucke-Menu, F.; Turcotte, S.; Kadoury, S.; Tang, A. Deep learning workflow in radiology: A primer. Insights Imaging 2019, 11, 22. [Google Scholar] [CrossRef] [Green Version]
- Fatahi, M.; Speck, O. Magnetic resonance imaging (MRI): A review of genetic damage investigations. Mutat. Res. Rev. Mutat. Res. 2015, 764, 51–63. [Google Scholar] [CrossRef]
- Body Planes and Sections. Available online: https://med.libretexts.org/@go/page/7289 (accessed on 10 November 2021).
- Anatomical Planes of the Body. Available online: https://www.spineuniverse.com/anatomy/anatomical-planes-body (accessed on 10 November 2021).
- Bien, N.; Rajpurkar, P.; Ball, R.L.; Irvin, J.; Park, A.; Jones, E.; Bereket, M.; Patel, B.N.; Yeom, K.W.; Shpanskaya, K.; et al. Deep-learning-assisted diagnosis for knee magnetic resonance imaging: Development and retrospective validation of MRNet. PLoS Med. 2018, 15, e1002699. [Google Scholar] [CrossRef]
- Azcona, D.; McGuinness, K.; Smeaton, A.F. A Comparative Study of Existing and New Deep Learning Methods for Detecting Knee Injuries using the MRNet Dataset. In Proceedings of the 2020 International Conference on Intelligent Data Science Technologies and Applications (IDSTA), Valencia, Spain, 14 June 2020; pp. 149–155. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef]
- Silverberg, E.; Boring, C.C.; Squires, T.S. Cancer Statistics. CA Cancer J. Clin. 1990, 40, 9–26. [Google Scholar] [CrossRef] [PubMed]
- Ameri, A. A Deep Learning Approach to Skin Cancer Detection in Dermoscopy Images. J. Biomed. Phys. Eng. 2020, 10, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Moldovanu, S.; Obreja, C.; Biswas, K.C.; Moraru, L. Towards Accurate Diagnosis of Skin Lesions Using Feedforward Back Propagation Neural Networks. Diagnostics 2021, 13, 936. [Google Scholar] [CrossRef] [PubMed]
- Moldovau, S.; Michis, F.A.D.; Biswas, K.C.; Culea-Florescu, A.; Moraru, L. Skin Lesion Classification Based on Surface Fractal Dimensions and Statistical Color Cluster Features Using an Ensemble of Machine Learning Techniques. Cancers 2021, 13, 5256. [Google Scholar] [CrossRef] [PubMed]
- Chakrabarty, S.; Sotiras, A.; Milchenko, M.; LaMontagne, P.; Hileman, M.; Marcus, D. MRI-based Identification and Classification of Major Intracranial Tumor Types by Using a 3D Convolutional Neural Network: A Retrospective Multi-Institutional Analysis. Radiol. Artif. Intell. 2021, 3, e200301. [Google Scholar] [CrossRef]
- Muhammad, K.; Khan, S.; Ser, V.H.; Albuquerque, V.H.C. Deep Learning for Multigrade Brain Tumor Classification in Smart Healthcare Systems: A Progpective Survey. IEEE Trans. Neural Netw. Learn. Syst. 2021, 32, 507–522. [Google Scholar] [CrossRef]
- Kempen, E.J.; Post, M.; Mannil, M.; Witkam, R.L.; Laan, M.; Patel, A.; Meijer, F.J.A.; Henssen, D. Performance of machine learning algotihms for glioma segmentation of brain MRI: A systematic review and meta-analysis. Eur. Radial. 2021, 31, 9638–9653. [Google Scholar] [CrossRef] [PubMed]
- Nasor, M.; Obaid, W. Detection and Localization of Early-Stage Multiple Brain Tumors Using a Hybrid Technique of Patch-Based Processing, k-means Clustering and Object Counting. Int. J. Biomed. Imaging 2020, 2020, 9035096. [Google Scholar] [CrossRef] [Green Version]
- Lei, Y.; Yin, M.; Yu, M.; Jing, Y.; Zeng, S.; Lv, W.; Li, J.; Ye, H.; Cui, X.; Dietrich, C.R. Artificial Intelligence in Medical Imaging of the Breast. Front. Oncol. 2021, 11, 2892. [Google Scholar] [CrossRef] [PubMed]
- Hu, Q.; Whitney, H.M.; Giger, M.L. A deep learning methodology for improved breast cancer diagnosis using multiparametric MRI. Sci. Rep. 2020, 10, 10536. [Google Scholar] [CrossRef] [PubMed]
- Ellman, S.; Wenkel, E.; Dietzel, M.; Bielowski, C.; Vesal, S.; Maier, A.; Hammon, M.; Janka, R.; Fasching, P.A.; Beckmann, M.W.; et al. Implementation of machine learning into clinical breast MRI: Potential for objective and accurate decision-making in suspicious breast masses. PLoS ONE 2020, 15, e0228446. [Google Scholar] [CrossRef] [Green Version]
- Krizhevsky, A.; Sutskever, I.; Hinton, G.E. Imagenet classification with deep convolutional neural networks. Adv. Neural Inf. Process. Syst. 2012, 25, 1097–1105. [Google Scholar] [CrossRef]
- He, K.; Zhang, X.; Ren, R.; Sun, J. Deep Residual Learning for Image Recognition. In Proceedings of the 2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Las Vegas, NV, USA, 27–30 June 2016; pp. 770–778. [Google Scholar] [CrossRef] [Green Version]
- Tsai, C.; Kiryati, N.; Konen, E.; Eshed, I.; Mayer, A. Knee Injury Detection using MRI with Efficiently-Layered Network (ELNet). arXiv 2020, arXiv:2005.02706v3. [Google Scholar]
- Roblot, V.; Giret, Y.; Bou Antuan, M.; Morillot, C.; Chassin, X.; Cotton, A.; Zerbib, J.; Fournier, L. Artificial intelligence to diagnose meniscus tears on MRI. Diagn. Interv. Imaging 2019, 100, 243–249. [Google Scholar] [CrossRef]
- Girshick, R. Fast R-CNN. In Proceedings of the 2015 IEEE International Conference on Computer Vision (ICCV), Santiago, Chile, 7–13 December 2015; pp. 1140–1148. [Google Scholar] [CrossRef]
- Couteaux, V.; Si-Mohamed, S.; Nempont, O.; Lefevre, T.; Popoff, A.; Pizaine, G.; Villain, N.; Bloch, I.; Cotton, A.; Boussel, L. Automatic knee meniscus tear detection and orientation classification with Mask-RCNN. Diagn. Interv. Imaging 2019, 100, 235–242. [Google Scholar] [CrossRef] [PubMed]
- He, K.; Grioxari, G.; Dollár, P. Mask R-CNN. In Proceedings of the 2017 IEEE International Conference on Computer Vision (ICCV), Venice, Italy, 22–29 October 2017; pp. 2980–2988. [Google Scholar] [CrossRef]
- Awan, M.J.; Rahim, M.S.M.; Salim, N.; Mohammed, M.A.; Begonya, G.; Abdulkareem, K.G. Efficient Detection of Knee Anterior Cruciate Ligament from Magnetic Resonance Imaging Using Deep Learning Approach. Diagnostics 2021, 11, 105. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, F.; Qi, Z.; Duan, K.; Xi, D.; Zhu, Y.; Zhu, H.; Xiong, H.; He, Q. A Comprehensive Survey on Transfer Learning. Proc. IEEE 2021, 109, 43–76. [Google Scholar] [CrossRef]
- Deng, J.; Dong, W.; Socher, R.; Li, L.; Kai, L.; Fei-Fei, L. ImageNet: A Large-Scale Hierarchical Image Database. In Proceedings of the 2009 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR 2009), Miami, FL, USA, 20–25 June 2009; pp. 248–255. [Google Scholar] [CrossRef] [Green Version]
- Russakovsky, O.; Deng, J.; Su, H.; Krause, J.; Satheesh, S.; Ma, S.; Huang, Z.; Karpathy, Z.; Khosla, A.; Bernstein, M.; et al. ImageNet Large Scale Visual Recognition Challenge. Int. J Comput Vis 2015, 115, 211–252. [Google Scholar] [CrossRef] [Green Version]
- LeCun, Y.; Bottou, L.; Bengio, Y.; Haffner, P. Gradient-Based Learning Applied to Document Rocognition. Proc. IEEE 1998, 86, 2278–2324. [Google Scholar] [CrossRef] [Green Version]
- Simonyan, K.; Zisserman, A. Very Deep Convolutional Networks for Large-Scale Image Recognition. In Proceedings of the 3rd International Conference on Learning Representations (ICLR 2015), San Diego, CA, USA, 7–9 May 2015; Available online: https://arxiv.org/abs/1409.1556 (accessed on 25 November 2021).
- ResNet and ResNetV2. Available online: https://keras.io/api/applications/resnet/ (accessed on 25 November 2021).
- Ruder, S. An overview of gradient descent optimization algorithms. arXiv 2017, arXiv:1609.04747. [Google Scholar]
- Li, Z.; Arora, S. An Exponential Learning Rate Schedule for Deep Learning. arXiv 2019, arXiv:1910.07454v3. [Google Scholar]
- Keras: The Python deep learning API. Available online: https://keras.io/ (accessed on 25 November 2021).
- ExponentialDecay. Available online: https://keras.io/api/optimizers/learning_rate_schedules/exponential_decay/ (accessed on 25 November 2021).
- SGD. Available online: https://keras.io/api/optimizers/sgd/ (accessed on 25 November 2021).
- Saygılı, A.; Varlı, S. Automated Diagnosis of Meniscus Tears from MRI of the Knee. Int. Sci. Vocat. Stud. J. 2019, 3, 92–104. [Google Scholar]
- Dalal, N.; Triggs, B. Histograms of oriented gradients for human detection. In Proceedings of the 2005 IEEE Computer Society Conference on Computer Vision and Pattern Recognition (CVPR’05), San Diego, CA, USA, 20–25 June 2005. [Google Scholar] [CrossRef] [Green Version]
- Song, K.; Yan, Y.; Chen, W.; Zhang, X. Research and Perspective on Local Binary Pattern. Acta Autom. Sin. 2013, 39, 730–744. [Google Scholar] [CrossRef]
- Sharma, P.; Yadav, U.; Sharma, D. The concept of sensitivity and specificity in relation to two types of errors and its application in medical research. Math. Sci. Res. J. 2009, 2, 53–58. [Google Scholar]
- Chicco, D.; Jurman, G. The advantages of the Matthews correlation coefficient (MCC) over F1 score and accuracy in binary classification evaluation. BMC Genom. 2020, 21, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradley, A.P. The use of the area under the ROC curve in the evaluation of machine learning algorithms. Pattern Recognition 1997, 30, 1145–1159. [Google Scholar] [CrossRef] [Green Version]
- Rummel, S.; Hueman, M.T.; Costantino, N.; Shriver, C.D.; Ellsworth, R.E. Tumour location within the breast: Does tumour site have prognostic ability? Ecancermedicalscience 2015, 9, 552. [Google Scholar] [CrossRef] [Green Version]
- Wu, S.; Zhou, J.; Ren, Y.; Sun, J.; Li, F.; Lin, Q.; Lin, H.; He, Z. Tumor location is a prognostic factor for survival of Chinese women with T1-2N0M0 breast cancer. Int. J. Surg. 2014, 12, 394–398. [Google Scholar] [CrossRef] [Green Version]
- Sagberg, L.M.; VERSEN, D.H.; Fyllingen, E.H.; Jakola, A.S.; Reinertsen, I.; Solheim, O. Brain atlas for assessing the impact of tumor location on perioperative quality of life in patients with high-grade glioma: A prospective population-based cohort study. Neuroimage Clin. 2019, 21, 101658. [Google Scholar] [CrossRef] [PubMed]






| Sagittal Plain | Class 0 | Class 1 | Class 2 (ACL) | Class 3 (Meniscus) |
|---|---|---|---|---|
| Train | 219 | 180 | 515 | 236 |
| Validation | 45 | 43 | 117 | 55 |
| Sample Weights | 2.35 | 2.86 | 1.0 | 2.18 |
| Sagittal Plane | Total | Utilised | Unselected | Unselected List |
|---|---|---|---|---|
| Train | 1130 | 1124 | 6 | 0003, 0370, 0544, 0582, 0665, 0776 |
| Validation | 120 | 118 | 2 | 1159, 1230 |
| Coronal Plane | Class 0 | Class 1 | Class 2 | Class 3 (ACL and Meniscus) | Class 4 | Class 5 | Class 6 |
|---|---|---|---|---|---|---|---|
| Train | 139 | 139 | 144 | 188 | 126 | 139 | 354 |
| Validation | 44 | 22 | 36 | 56 | 44 | 28 | 89 |
| Sample Weights | 2.55 | 2.55 | 2.46 | 1.88 | 2.81 | 2.55 | 1.0 |
| Coronal Plane | Total | Utilised | Unselected | Unselected List |
|---|---|---|---|---|
| Train | 1130 | 1123 | 7 | 0310, 0544, 0610, 0665, 0975, 1010, 1043 |
| Validation | 120 | 120 | 0 | - |
| Axial Plane | Class 0 | Class 1 (ACL) | Class 2 (Meniscus) | Class 3 | Class 4 |
|---|---|---|---|---|---|
| Train | 508 | 327 | 162 | 166 | 281 |
| Validation | 122 | 81 | 37 | 35 | 51 |
| Sample Weights | 1.0 | 1.55 | 3.14 | 3.06 | 1.81 |
| Axial Plane | Total | Utilised | Unselected | Unselected List |
|---|---|---|---|---|
| Train | 1130 | 1128 | 2 | 0577, 0665 |
| Validation | 120 | 119 | 1 | 1136 |
| Plane | Task | Train Positive | Train Negative | Sample Weights Positive—Negative | Validation Positive | Validation Negative |
|---|---|---|---|---|---|---|
| Sagittal | ACL | 392 | 732 | 4.46–1.0 | 51 | 67 |
| Meniscus | 206 | 918 | 1.87–1.0 | 54 | 66 | |
| Abnormal | 907 | 217 | 1.0–4.18 | 93 | 25 | |
| Coronal | ACL | 207 | 916 | 4.43–1.0 | 54 | 66 |
| Meniscus | 395 | 728 | 1.84–1.0 | 52 | 68 | |
| Abnormal | 906 | 217 | 1.0–4.18 | 95 | 25 | |
| Axial | ACL | 208 | 920 | 4.42–1.0 | 54 | 65 |
| Meniscus | 396 | 732 | 1.85–1.0 | 52 | 67 | |
| Abnormal | 911 | 217 | 1.0–4.20 | 95 | 24 |
| Plane | Train | Validation | Task | Accuracy | Sensitivity | Specificity | MCC | ROC-AUC |
|---|---|---|---|---|---|---|---|---|
| ACL | 0.7881 | 0.5741 | 0.9688 | 0.6025 | 0.8947 | |||
| Sagittal | 1124 | 118 | Meniscus | 0.7712 | 0.5686 | 0.9254 | 0.5403 | 0.7987 |
| Abnormal | 0.8898 | 0.9462 | 0.68 | 0.6571 | 0.9316 | |||
| ACL | 0.7583 | 0.8519 | 0.6818 | 0.5346 | 0.8297 | |||
| Coronal | 1123 | 120 | Meniscus | 0.75 | 0.7115 | 0.7794 | 0.4910 | 0.7393 |
| Abnormal | 0.8667 | 0.9473 | 0.56 | 0.5644 | 0.8029 | |||
| ACL | 0.8319 | 0.7222 | 0.9231 | 0.6655 | 0.8721 | |||
| Axial | 1128 | 119 | Meniscus | 0.6891 | 0.7115 | 0.6716 | 0.3801 | 0.7075 |
| Abnormal | 0.8992 | 0.9579 | 0.6667 | 0.6702 | 0.8596 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kara, A.C.; Hardalaç, F. Detection and Classification of Knee Injuries from MR Images Using the MRNet Dataset with Progressively Operating Deep Learning Methods. Mach. Learn. Knowl. Extr. 2021, 3, 1009-1029. https://doi.org/10.3390/make3040050
Kara AC, Hardalaç F. Detection and Classification of Knee Injuries from MR Images Using the MRNet Dataset with Progressively Operating Deep Learning Methods. Machine Learning and Knowledge Extraction. 2021; 3(4):1009-1029. https://doi.org/10.3390/make3040050
Chicago/Turabian StyleKara, Ali Can, and Fırat Hardalaç. 2021. "Detection and Classification of Knee Injuries from MR Images Using the MRNet Dataset with Progressively Operating Deep Learning Methods" Machine Learning and Knowledge Extraction 3, no. 4: 1009-1029. https://doi.org/10.3390/make3040050
APA StyleKara, A. C., & Hardalaç, F. (2021). Detection and Classification of Knee Injuries from MR Images Using the MRNet Dataset with Progressively Operating Deep Learning Methods. Machine Learning and Knowledge Extraction, 3(4), 1009-1029. https://doi.org/10.3390/make3040050






