Effect of Over-the-Counter Whitening Dentifrices on the Color Stability and Microhardness of Composite Resins
Abstract
1. Introduction
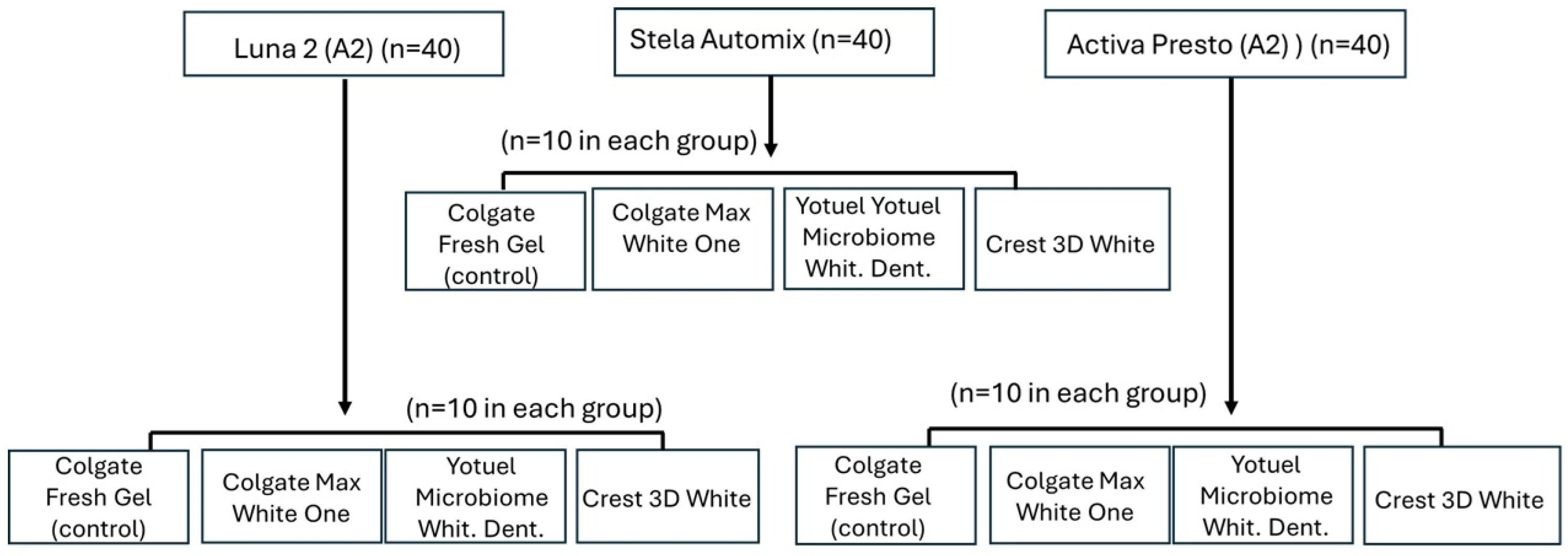
2. Materials and Methods
2.1. Sample Size Calculation
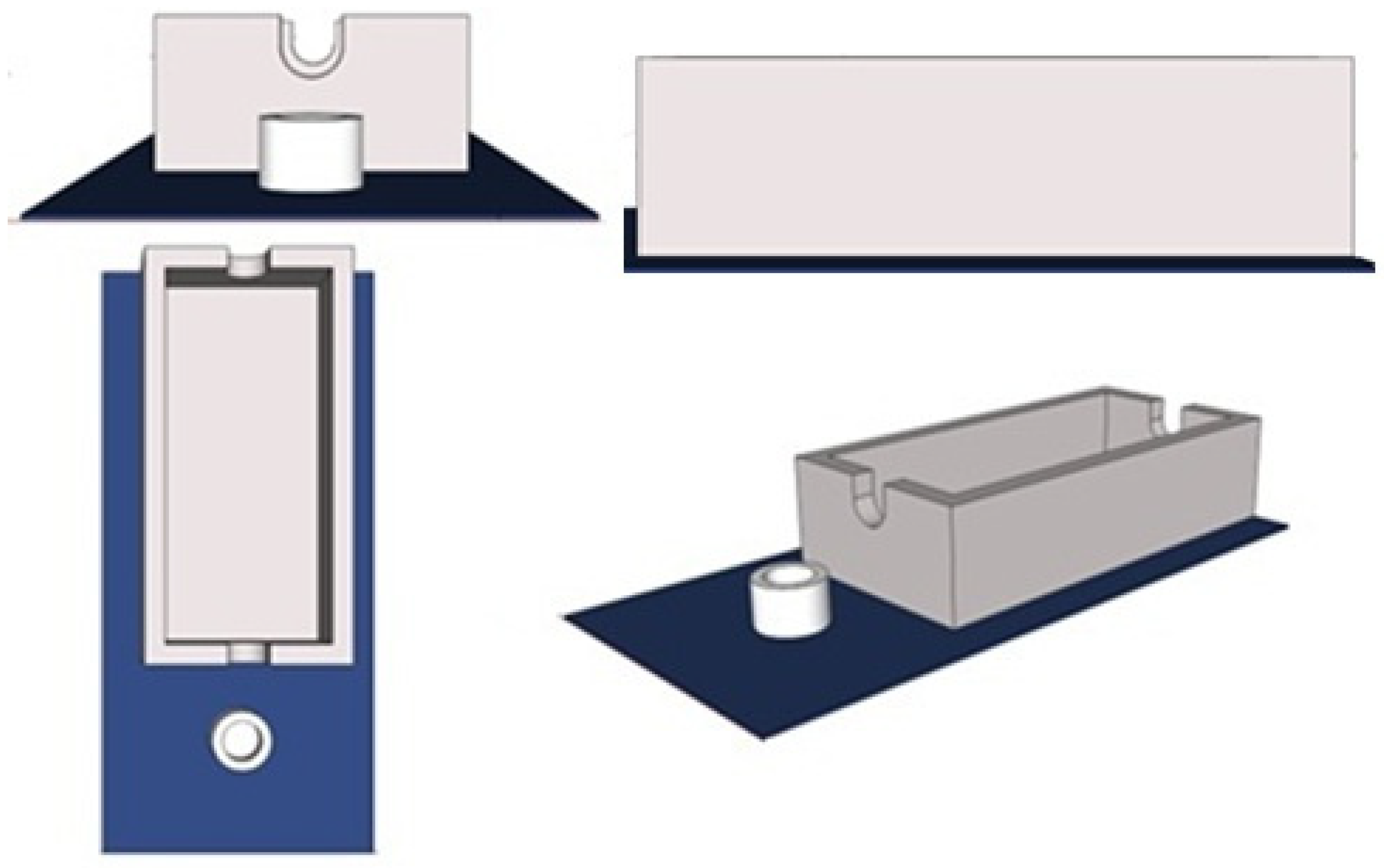
2.2. Sample Preparation
2.3. Brushing with Whitening Toothpastes
2.4. Color Measurement
2.5. Microhardness Evaluation
2.6. Statistical Analisis
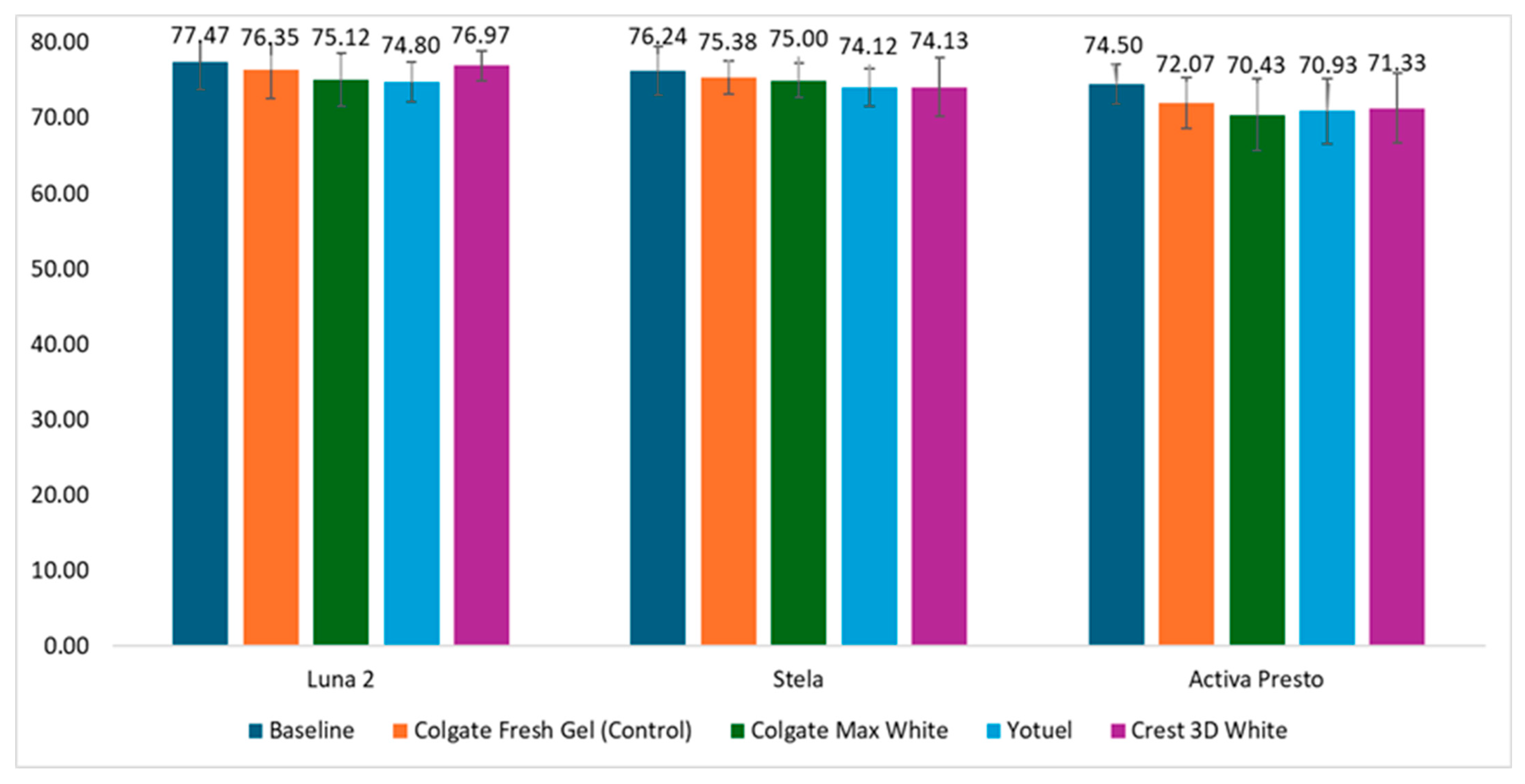
3. Results
3.1. Color Changes
3.2. Microhardness Changes
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Krayem, E.; Banerjee, A.; Milly, H. Evaluating the efficiency of two different over-the-counter tooth whitening systems: A randomised controlled clinical trial. BDJ Open 2024, 10, 41. [Google Scholar] [CrossRef] [PubMed]
- Auschill, T.M.; Hellwig, E.; Schmidale, S.; Sculean, A.; Arweiler, N.B. Efficacy, side-effects and patients’ acceptance of different bleaching techniques (OTC, in-office, at-home). Oper. Dent. 2005, 30, 156–163. [Google Scholar] [CrossRef]
- Agarwal, R.; Vasani, N.; Mense, U.S.; Prasad, N.; Shetty, A.; Natarajan, S.; Dutta, A.; Thomas, M.S. Effects of online marketplace-sourced over-the-counter tooth whitening products on the colour, microhardness, and surface topography of enamel: An in vitro study. BDJ Open 2024, 10, 67. [Google Scholar] [CrossRef]
- Roselino, L.D.M.R.; Tirapelli, C.; Pires-De-Souza, F.D.C.P. Randomized clinical study of alterations in the color and surface roughness of dental enamel brushed with whitening toothpaste. J. Esthet. Restor. Dent. 2018, 30, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, L.M.M.; Amâncio Filha, M.B.G.; Leite, J.V.C.; do Nascimento Santos, J.V.; De Medeiros, J.M.; Macedo De Oliveira, I.L.; Pecho, O.E.; Saeger Meireles, S.; Bezerra Wanderley Lima, R. Over-the-Counter Products in Tooth Bleaching: A Scoping Review. J. Dent. 2024, 145, 104989. [Google Scholar] [CrossRef]
- Tadin, A.; Galić, S.; Gavić, L. Assessment of Color Change, Esthetic Perception, Treatment Satisfaction, and Side Effects Following the Use of Over-The Counter Whitening Products. Acta Stomatol. Croat. 2023, 57, 300–315. [Google Scholar] [CrossRef] [PubMed]
- Mehrgan, S.; Kermanshah, H.; Omrani, L.R.; Ahmadi, E.; Rafeie, N. Comparison the effect of charcoal-containing, hydrogen peroxide-containing, and abrasive whitening toothpastes on color stability of a resin composite; an in vitro study. BMC Oral Health 2021, 21, 594. [Google Scholar] [CrossRef]
- Epple, M.; Meyer, F.; Enax, J. A critical review of modern concepts for Teeth whitening. Dent. J. 2019, 7, 79. [Google Scholar] [CrossRef]
- Müller-Heupt, L.K.; Wiesmann-Imilowski, N.; Kaya, S.; Schumann, S.; Steiger, M.; Bjelopavlovic, M.; Deschner, J.; Al-Nawas, B.; Lehmann, K.M. Effectiveness and safety of over-the-counter tooth-whitening agents compared to Hydrogen Peroxide in Vitro. Int. J. Mol. Sci. 2023, 24, 1956. [Google Scholar] [CrossRef]
- Tantanuch, S.; Kukiattrakoon, B.; Peerasukprasert, T.; Schumann, S.; Steiger, M.; Bjelopavlovic, M.; Deschner, J.; Al-Nawas, B.; Lehmann, K.M.; Chanmanee, N.; et al. Surface roughness and erosion of nanohybrid and nano filled resin composites after immersion in red and white wine. J. Conserv. Dent. 2016, 19, 51–55. [Google Scholar]
- Gurbuz, A.; Ozkan, P.; Yilmaz, K.; Yilmaz, B.; Durkan, R. Effect of at-home whitening strips on the surface roughness and color of a composite and an ormocer restorative material. Prosthodontics 2013, 22, 69–73. [Google Scholar] [CrossRef]
- de Oliveira, M.N.; Vidigal, M.T.C.; Vieira, W.; Lins-Candeiro, C.L.; Machado Oliveira, L.; Nascimento, G.G.; Rodrigues da Silva, G.; Paranhos, L.R. Assessment of color changes and adverse effects of over-the-counter bleaching protocols: A systematic review and network meta-analysis. Clin. Oral Investig. 2024, 28, 189. [Google Scholar] [CrossRef] [PubMed]
- Amaral, C.M.; Rodrigues, J.A.; Erhardt, M.C.; Barata, M.W.; Marchi, G.M.; Heymann, H.O.; Freire Pimenta, L.A. Effect of whitening dentifrices on the superficial roughness of esthetic restorative materials. J. Esthet. Restor. Dent. 2006, 18, 102–108. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, S.; Park, Y.S. Effects of a commercial whitening toothpaste containing hydrogen peroxide and citric acid on dentin abrasion and erosion. BMC Oral Health 2023, 23, 619. [Google Scholar] [CrossRef] [PubMed]
- Melo, M.A.S.; Mokeem, L.; Sun, J. Bioactive Restorative Dental Materials-The New Frontier. Dent. Clin. N. Am. 2022, 66, 551–566. [Google Scholar] [CrossRef]
- Zhou, W.; Chen, H.; Weir, M.D.; Oates, T.W.; Zhou, X.; Wang, S.; Cheng, L.; Xu, H.H.K. Novel bioactive dental restorations to inhibit secondary caries in enamel and dentin under oral biofilms. J. Dent. 2023, 133, 104497. [Google Scholar] [CrossRef] [PubMed]
- Francois, P.; Fouquet, V.; Attal, J.P.; Durson, E. Commercially available fluoride-releasing restorative materials: A review and a proposal for classification. Materials 2020, 13, 2313. [Google Scholar] [CrossRef]
- Turkistani, A.; Hasanain, F.A. Surface roughness and gloss retention of bioactive resin composite after simulated toothbrush abrasion. Mater. Res. Express 2024, 11, 055401. [Google Scholar] [CrossRef]
- Abuljadayel, R.; Mushayt, A.; Al Mutairi, T.; Sajini, S. Evaluation of bioactive restorative materials’ Color Stability: Effect of Immersion Media and Thermocycling. Cureus 2023, 15, e43038. [Google Scholar] [CrossRef]
- Tan, B.L.; Yap, A.U.; Ma, H.N.; Chew, J.; Tan, W.J. Effect of beverages on color and translucency of new tooth-colored restoratives. Oper. Dent. 2015, 40, E56–E65. [Google Scholar] [CrossRef]
- Colak, G.; Katirci, G. In Vitro evaluation of the effects of whitening toothpastes on the color and surface roughness of different composite resin materials. BMC Oral Health 2023, 23, 580. [Google Scholar] [CrossRef] [PubMed]
- Dudás, C.; Forgó, Z.; Kerekes-Máthé, B. Surface roughness changes of different restoration materials after tooth brushing simulation using different toothpastes. J. Interdiscip. Med. 2017, 2, 21–24. [Google Scholar] [CrossRef]
- Paravina, R.D.; Pérez, M.M.; Ghinea, R. Acceptability and perceptibility thresholds in dentistry: A comprehensive review of clinical and research applications. J. Esthet. Restor. Dent. 2019, 31, 103–112. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.M.; Herrera, L.; Carrillo, F.; Pecho, O.; Pecho, O.E.; Dudea, D.; Gasparik, C.; Ghinea, R.; Della Bona, A. Whiteness difference thresholds in Dentistry. Dent. Mater. 2019, 35, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Pires, P.M.; de Almeida Neves, A.; Lukomska-Szymanska, M.; Farrar, P.; Ferrando Cascales, A.; Sauro, S. Bonding performance and interfacial adaptation of modern bulk-fill restorative composites after aging in artificial saliva: An in vitro study. Clin. Oral Investig. 2024, 28, 132. [Google Scholar] [CrossRef] [PubMed]
- Boaro, C.; Gonçalves, F.; Guimarães, T.C.; Ferracane, J.L.; Pfeifer, C.S.; Braga, R.R. Sorption, solubility, shrinkage and mechanical properties of low-shrinkage commercial resin composites. Dent. Mater. 2013, 29, 398404. [Google Scholar] [CrossRef] [PubMed]
- Guarneri, J.A.G.; Maucoski, C.; Ghaffari, S.; MacNeil, B.D.; MacNeil, B.D.; Price, R.B.; Galvão Arrais, C.A. Ability of a Novel Primer to Enhance the Polymerization of a Self-Cured Resin Composite. Dent. Mater. 2025, 41, 42–50. [Google Scholar] [CrossRef]
- Dayi, B.; Öcal, F. The Effect of Whitening Toothpastes on Colour Change and Surface Roughness of Restorative Materials. Odovtos-Int. J. Dent. Sci. 2023, 25, 40–52. [Google Scholar] [CrossRef]
- Joiner, A. Whitening toothpastes: A review of the literature. J. Dent. 2010, 38, e17–e24. [Google Scholar] [CrossRef]
- Komatsu, O.B.; Nishida, H.; Sekino, T.; Yamamoto, K. Application of titanium dioxide nanotubes to tooth whitening. Nano Biomed. 2014, 6, 63–72. [Google Scholar]
- Monteiro, N.R.; Basting, R.T.; Amaral, F.L.B.D.; Gomes FranÇa, F.M.; Pedroso Turssi, C.; Lisboa Filho, P.O.; Kantovitz, K.R.; Basting, R.T. Titanium dioxide nanotubes incorporated into bleaching agents: Physicochemical characterization and enamel color change. J. Appl. Oral Sci. 2020, 28, e2019077. [Google Scholar] [CrossRef] [PubMed]
- Yu, B.; Ahn, J.S.; Lim, J.I.; Lee, Y.K. Influence of TiO2 nanoparticles on the optical properties of resin composites. Dent. Mater. 2009, 25, 1142–1147. [Google Scholar] [CrossRef] [PubMed]
- Yilmaz, M.N.; Gul, P.; Unal, M.; Turgut, G. Effects of whitening toothpastes on the esthetic properties and surface roughness of a composite resin. J. Oral Sci. 2021, 63, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.M.; Pecho, O.E.; Ghinea, R.; Pulgar, R. Recent Advances in Color and Whiteness Evaluations in Dentistry. Curr. Dent. 2019, 1, 23–29. [Google Scholar] [CrossRef]
- Cheng, Y.L.; Zhong, B.J.; Su, C.; Lu, Z.C.; Yu, H. Enhanced tooth bleaching with a hydrogen peroxide/titanium dioxide gel. BMC Oral Health 2024, 24, 923. [Google Scholar] [CrossRef]
- Ludovichetti, F.S.; Zerman, N.; Stellini, E.; Zambon, G.; Mazzoleni, S.; Zuccon, A. Dental bleaching: Patient perception and satisfaction. Minerva Dent. Oral Sci. 2024, 73, 217–223. [Google Scholar] [CrossRef]
- Mounika, A.; Mandava, J.; Roopesh, B.; Karri, G. Clinical evaluation of color change and tooth sensitivity with in-office and home bleaching treatments. Indian J. Dent. Res. 2018, 29, 423–427. [Google Scholar] [CrossRef]
- Hannig, C.; Duong, S.; Becker, K.; Brunner, E.; Kahler, E.; Attin, T. Effect of bleaching on subsurface micro-hardness of composite and a polyacid modified composite. Dent. Mater. 2007, 23, 198–203. [Google Scholar] [CrossRef]
- de Abreu, D.R.; Sasaki, R.T.; Amaral, F.L.; Flório, F.M.; Tarkany Basting, R. Effect of home-use and in-office bleaching agents containing hydrogen peroxide associated with amorphous calcium phosphate on enamel microhardness and surface roughness. J. Esthet. Restor. Dent. 2011, 23, 158–168. [Google Scholar] [CrossRef]
- Fernandes, R.A.; Strazzi-Sahyon, H.B.; Suzuki, T.Y.; Fraga Briso, A.L.; Dos Santos, P.H. Effect of dental bleaching on the microhardness and surface roughness of sealed composite resins. Restor. Dent. Endod. 2020, 45, e12. [Google Scholar] [CrossRef]
- Attin, T.; Hannig, C.; Wiegand, A.; Attin, R. Effect of bleaching on restorative materials and restorations: A systematic review. Dent. Mater. 2004, 20, 852–861. [Google Scholar] [CrossRef] [PubMed]
- Worschech, C.C.; Rodrigues, J.A.; Martins, L.R.; Bovi Ambrosano, G.M. In vitro evaluation of human dental enamel surface roughness bleached with 35% carbamide peroxide and submitted to abrasive dentifrice brushing. Pesqui. Odontol. Bras. 2003, 17, 342–348. [Google Scholar] [CrossRef]
- Marigo, L.; Nocca, G.; Fiorenzano, G.; Callà, C.; Castagnola, R.; Cordaro, M.; Paolone, G.; Sauro, S. Influences of differentair-inhibition coatings on monomer release, microhardness, andcolor stability of two composite materials. BioMed Res. Int. 2019, 2019, 4240264. [Google Scholar] [CrossRef]
- Garcia, I.M.; Balhaddad, A.A.; Aljuboori, N.; Ibrahim, M.S.; Mokeem, L.; Ogubunka, A.; Mezzomo Collares, F.; Sampaio de Melo, M.A. Wear behavior and surface quality of dental bioactive ions-releasing resinsunder simulated chewing conditions. Front. Oral Health 2021, 2, 628026. [Google Scholar] [CrossRef] [PubMed]
- Thadathil Varghese, J.; Raju, R.; Farrar, P.; Prentice, L.; Prusty, B.G. Comparative analysis of self-cure and dual cure-dental composites on their physico-mechanical behaviour. Aust. Dent. J. 2024, 69, 124–138. [Google Scholar] [CrossRef] [PubMed]
- Binhasan, M.; Solimanie, A.H.; Almuammar, K.S.; Alnajres, A.R.; Alhamdan, M.M.; Al Ahdal, K.; Alfaawaz, Y.F.; Ali, K.; Vohra, F.; Abduljabbar, T. The Effect of Dentifrice on Micro-Hardness, Surface Gloss, and Micro-Roughness of Nano Filled Conventional and Bulk-Fill Polymer Composite-A Micro Indentation and Profilometric Study. Materials 2022, 15, 4347. [Google Scholar] [CrossRef]
- Mady, T.M.; Abdelnabi, A.; Maha, S.; Bayoumi, R.E.; Abdelraouf, R.M. Effect of Different Mouthwashes on the Surface Microhardness and Color Stability of Dental Nanohybrid Resin Composite. Polymers 2023, 15, 815. [Google Scholar] [CrossRef]
| Product | Manufacturer | Composition |
|---|---|---|
| Stela Mix Composite Resin | SDI. Victoria, Australia | Urethane dimethacrylate (44%), glycerol dimethacrylate, 10-MDP filler (55%), fluoroaluminosilicate ionomer glass, ytterbium trifluoride opacifier, silicon dioxide, calcium aluminate, initiators, stabilizers, pigments. (Filler 61.0 wt.%.) |
| Luna 2 Composite Resin (A2) | SDI. Victoria, Australia | Urethane dimethacrylates (44%), tritylene glycol dimethacrylate, tricyclododecanedimethanol dimethacrylate fillers (56%), strontium glass, silicon dioxide, ytterbium trifluoride, initiators, stabilizers, pigments (Filler 77.0 wt.%.) |
| ActivaTM Presto Composite Resin (A2) | Pulpdent Corporation, Watertown, MA, USA | UDMA, Bis-2MP 35%. Methacrylate-functionalized calcium phosphate (MCP), silanated barium, strontium alumino-silicate glasses and silica. (Filler 56.0 wt.%.) |
| Colgate Max White One Phosphoric Acid Potassium Hydroxide Tooth Paste (Erosive Action) | Colgate-Palmolive Company, New York, NY, USA | Aqua, hydrated silica, sorbitol, PEG-12, pentasodium triphosphate, tetrapotassium pyrophosphate, aroma, sodium lauryl sulfate, cellulose gum, potassium hydroxide, phosphoric acid, cocamidopropyl betaine, sodium fluoride, sodium saccharin, xanthan gum, limonene, CI 74160. |
| Yotuel microbiome one premium whitening dentifrice Tooth Paste CP TiO2 optical effect | Bio Cosmetic Laboratories, S.L, Madrid, Spain | Glycerin, xylitol, water, potassium citrate, betaine, silica, dicalcium phosphate, sodium monofluorophosphate, flavor, titanium dioxide (TiO2), cocamidopropyl betaine, hydroxyethyl acrylate/sodium acryloyldimethyl tatouate copolymer, olea europea oil, sodium benzoate, carbomer, carbamide peroxide, potassium sorbate, sucralose, stevia rebaudiana leaf extract, cinnamon. |
| Crest 3D White Brilliance Whitening two-step Tooth Paste HP TiO2 optical effect | Procter & Gamble, Cincinnati, OH, USA | Stannous fluoride 0.454%, glycerin, hydrated silica, water, zinc lactate, sodium lauryl sulfate, trisodium phosphate, flavor, sodium gluconate, sodium saccharin, xanthan gum, cellulose gum, sodium didroxide, mica, titanium dioxide (TiO2), hydrogen peroxide, carbomer, disodium pyrophosphate, sucralose, sodium hydroxide. |
| Colgate Fresh Gel Tooth Paste (Control) | Colgate-Palmolive Company, New York, NY, USA | Sorbitol, water, hydrated silica, PEG-12, sodium lauryl sulfate, PEG-12, flavor, cellulose gum, sodium fluoride, sodium saccharine, CI42090. |
| Colgate Fresh Gel (Control) | ||||||
|---|---|---|---|---|---|---|
| A | L | p | a | p | b | p |
| Luna 2/before | 88.80 ± 1.57 | 0.13 | −2.50 ± 0.65 | 0.06 | 15.50 ± 3.97 | <0.001 |
| Luna 2/after | 89.12 ± 1.37 | −2.22 ± 0.69 | 14.07 ± 3.52 | |||
| Colgate Max White | ||||||
| Luna 2/before | 89.53 ± 1.73 | 0.30 | −2.21 ± 0.55 | 0.12 | 14.68 ± 3.36 | <0.001 |
| Luna/after | 89.12 ± 1.71 | −1.98 ± 0.78 | 12.10 ± 3.21 | |||
| Yotuel | ||||||
| Luna 2/before | 89.86 ± 048 | 1 | −1.99 ± 0.43 | 0.44 | 15.22 ± 1.54 | <0.001 |
| Luna 2/after | 89.75 ± 1.01 | −1.88 ± 0.49 | 13.73 ± 1.50 | |||
| Crest 3D White | ||||||
| Luna 2/before | 89.46 ± 0.55 | 0.47 | −1.78 ± 0.32 | 0.72 | 15.16 ± 2.04 | <0.001 |
| Luna 2/after | 89.33 ± 1.25 | −1.81 ± 0.59 | 13.61 ± 2.47 | |||
| Colgate Fresh Gel (Control) | ||||||
| B | L | p | a | p | b | p |
| Stela/before | 84.25 ± 3.27 | 0.09 | 1.71 ± 0.43 | 0.17 | 19.57 ± 2.80 | 0.01 |
| Stela/after | 85.96 ± 1.84 | 1.26 ± 0.33 | 17.02 ± 1.56 | |||
| Colgate Max White | ||||||
| Stela/before | 82.70 ± 1.69 | 0.41 | 1.33 ± 0.17 | 0.12 | 19.84 ± 1.38 | <0.001 |
| Stela/after | 83.63 ± 2.08 | 1.59 ± 0.41 | 15.20 ± 2.09 | |||
| Yotuel | ||||||
| Stela/before | 83.37 ± 1.93 | 0.22 | 0.91 ± 2.57 | <0.001 | 19.15 | <0.001 |
| Stela/after | 84.03 ± 2.21 | 1.42 ± 0.25 | 16.32 | |||
| Crest 3D White | ||||||
| Stela/before | 84.27 ± 1.99 | 0.45 | 1.37 ± 0.31 | 0.93 | 18.05 ± 1.11 | 0.07 |
| Stela/after | 82.78 ± 2.81 | 1.51 ± 0.29 | 15.81 ± 1.34 | |||
| Colgate Fresh Gel (Control) | ||||||
| C | L | p | a | p | b | p |
| Activa Presto/before | 84.80 ± 1.13 | 0.65 | 1.80 ± 0.14 | 1 | 26.65 ± 0.21 | 0.08 |
| Activa Presto/after | 84.05 ± 0.49 | 1.80 ± 0.14 | 25.75 ± 0.63 | |||
| Colgate Max White | ||||||
| Activa Presto/before | 86.05 ± 1.90 | 0.12 | 2.80 ± 0.28 | 0.89 | 29.05 ± 1.48 | 0.03 |
| Activa Presto/after | 87.25 ± 0.77 | 2.89 ± 0.14 | 24.90 ± 2.26 | |||
| Yotuel | ||||||
| Activa Presto/before | 85.90 ± 0.14 | 0.04 | 1.70 ± 0.56 | 0.65 | 30.60 ± 1.97 | 0.04 |
| Activa Presto/after | 89.15 ± 0.49 | 1.45 ± 0.07 | 26.15 ± 0.63 | |||
| Crest 3D White | ||||||
| Activa Presto/before | 84.70 ± 2.82 | 0.03 | 1.35 ± 0.63 | 0.31 | 25.40 ± 4.10 | 0.65 |
| Activa Presto/after | 88.50 ± 1.41 | 1.50 ± 0.42 | 24.20 ± 2.12 | |||
| Colgate Fresh Gel (Control) | Colgate Max White | Yotuel | Crest White | |
|---|---|---|---|---|
| ΔEab | ||||
| mean ± SD | mean ± SD | mean ± SD | mean ± SD | |
| Luna 2 | 1.59 ± 0.52 aA | 2.86 ± 1.27 aA | 1.89 ± 0.66 A | 2.08 ± 2.11 A |
| Stela | 4.28 ± 1.73 A | 5.46 ± 1.43 a,b,A | 3.38 ± 1.32 a,A | 3.75 ± 1.80 b |
| Activa Presto | 4.12 ± 0.69 | 4.37 ± 1.04 | 5.72 ± 1.69 A | 4.08 ± 1.02 A |
| ΔE00 | ||||
| Luna 2 | 0.97 ± 028 a,A | 1.84 ± 0.77 a,b,A | 1.23 ± 0.40 b,A | 1.42 ± 1.28 |
| Stela | 2.58 ± 1.05 A | 3.30 ± 1.07 a,b,A | 2.11 ± 0.74 a,A | 2.40 ± 1.17 b |
| Activa Presto | 2.05 ± 0.43 | 2.11 ± 0.62 | 2.96 ± 0.45 A | 3.57 ± 0.90 |
| ΔWID | ||||
| Luna 2 | 1.08 ± 0.56 A,B | 2.14 ± 1.33 A | 1.32 ± 1.21 | 1.61 ± 1.78 |
| Stela | 4.72 ± 3.08 a,b,A | 4.97 ± 1.61 c,d,A | 2.26 ± 1.57 a,c | 1.37 ± 1.86 b,d |
| Activa Presto | 3.90 ± 0.29 B | 5.17 ± 2.41 A | 3.13 ± 3.70 | 2.44 ± 1.94 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, X.; Melo, M.P.; Folguera, S.; Llena, C. Effect of Over-the-Counter Whitening Dentifrices on the Color Stability and Microhardness of Composite Resins. J. Compos. Sci. 2025, 9, 324. https://doi.org/10.3390/jcs9070324
Yu X, Melo MP, Folguera S, Llena C. Effect of Over-the-Counter Whitening Dentifrices on the Color Stability and Microhardness of Composite Resins. Journal of Composites Science. 2025; 9(7):324. https://doi.org/10.3390/jcs9070324
Chicago/Turabian StyleYu, Xinnuo, Maria Pilar Melo, Sofia Folguera, and Carmen Llena. 2025. "Effect of Over-the-Counter Whitening Dentifrices on the Color Stability and Microhardness of Composite Resins" Journal of Composites Science 9, no. 7: 324. https://doi.org/10.3390/jcs9070324
APA StyleYu, X., Melo, M. P., Folguera, S., & Llena, C. (2025). Effect of Over-the-Counter Whitening Dentifrices on the Color Stability and Microhardness of Composite Resins. Journal of Composites Science, 9(7), 324. https://doi.org/10.3390/jcs9070324






