1. Introduction
The advancements in restorative materials and techniques have significantly improved the longevity and functionality of dental treatments, ensuring better oral health outcomes for patients. Nevertheless, a recent investigation found that only 59% of composite restorations last for five years. The number of surviving restorations reduces to 43% at ten years and to 34% at fifteen years, the moment at which 7% of restored teeth are extracted [
1,
2].
Besides individual health factors, the clinical effectiveness of dental restorations depends on several material and technological design variables [
3]. The choice of the restorative material, namely composite resins or ceramics, depends on clinical factors as the volume of the remaining dental structure, whether a direct, semi-direct or indirect restoration is advised, the biocompatibility, and the aesthetic or financial requirements [
4]. Nevertheless, regardless of the restorative option, the adhesive material used to connect the restoration and the tooth enamel or dentin plays a leading role in determining the success and longevity of restorations [
5].
The fast advancement of adhesive systems in restorative dentistry has led to the requirement for the understanding of their mechanical properties and behavior when applied to dentin or new composite materials [
6,
7,
8,
9]. The mechanical properties of adhesive systems are evaluated through some tests, such as the microtensile bond strength (μTBS) test, shear bond strength test and push-out test [
10]. The interaction of the adhesive system with the underlying dentin and the material above it varies in accordance with the type of restoration. While direct restorations require only a single adhesive interface, semi-direct and indirect restorations often involve a dual adhesive interface with the use of resin cement for bonding.
Universal adhesive systems were launched in 2011 and the manufacturers argue that they can be applied on enamel or dentin with or without etching. The application mode can partially or totally remove the minerals and change the bonding mechanism. During etching, the collagen network of dentin is exposed and the adhesive monomers can penetrate from 3 to 5 μm and form a micromechanical interlocked hybrid layer. On the contrary, the self-etch application mode promotes a submicron hybrid layer formation (smear layer) assuring micro-retention and chemical interactions [
7]. This study chooses Clearfil SE Bond 2 and Ceram x Spectra ST HV composite resin as the experimental materials because they are a great combination for reliable, durable and esthetic dental restorations. The adhesive provides strong bonding with reduced sensitivity, while the composite resin offers excellent mechanical properties and esthetics. However, proper application techniques are crucial to achieving optimal results.
Resin cements are composed of polymerizable monomers, including methacrylates, di-methacrylates and polymethacrylates, which are structurally similar to composite restorative materials but contain a lower proportion of inorganic filler particles. The weight percentage (wt%) of filler within the material significantly impacts its viscosity, with lower filler content resulting in reduced viscosity and, consequently, enhanced flowability of the luting agent. Although several studies in the literature compare direct and indirect restorations, there is still controversy over which one performs better. Some experimental studies compare the microtensile bond strength of the two types of restorations [
11,
12,
13], whereas direct FEM comparisons of μTBS between direct and indirect restorations are rare or almost inexistent. Sengun et al. [
12], in 2005, compared the dentin bond strength of directly and indirectly inserted composite restorations. The Single Bond and Clearfill SE Bond agents were used in direct restorations whereas the indirect restorations were cemented using luting cements. The results showed that the resin luting cement played an important role in the tensile bond strength of indirect restorations. In 2025, Delalíbera and coworkers concluded that direct and indirect restorations in the cervical region exhibited a comparable bond strength [
11]. Tennert et al. [
14] performed a meta-analysis to compare the longevity of posterior direct and indirect composite restorations and revealed that direct composite restorations have a lower relative risk to fail than indirect restorations. Ghassemieh, in 2008, investigated how specimen shapes and attachment methods influence stress distribution during μTBS testing using the FEM [
15]. The researcher modeled three different specimen geometries and found that the dumbbell-shaped specimens exhibited a more homogeneous stress distribution than rectangular and hourglass-shaped ones, suggesting that specimen design can significantly affect the μTBS outcomes. In 2021, Neto et al. applied the FEM to analyze the stress distribution in premolars restored with indirect IPS Empress
® CAD onlays or inlays [
5]. The cement geometry was modified to include cohesive zone models (CZMs) to perform the adhesive joint’s strength prediction. The cohesive finite elements are used to model the initiation and propagation of cracks, which can be pertinent in studying adhesive failures or delamination in dental restorations. The CZM can help to identify the stress–strain behavior of direct and indirect restorations and predict failure based on the fracture toughness of the substrates, as well as their tensile and shear cohesive strengths. Nevertheless, the use of CZM requires the definition of traction–separation laws, the critical values of the toughness of traction and shear and the cohesive strengths of tension and shear. Moreover, the validation of all mechanical properties needed in the CZM requires the knowledge of a set of experimental results that, generally, are not reported in the literature. For instance, it is important to compare experimental and numerical force–displacement curves, verify if the numerical failure patterns match those observed and perform sensitivity analyses of the normal strength, shear strength and fracture energy to evaluate the model robustness.
This study aims to compare the bond strength of dentin to human molars with direct and semi-direct composite resin restorations using μTBS and to observe the most recurrent types of failure in the two groups. All the results will be used to further compare and validate CZMs in modeling the microtensile bond strength experiment. The publication of these results assures a clear independence between experimental and numerical methodologies.
The null hypothesis assumes no statistically significant difference in μTBS between direct and semi-direct restorations in dentin, and the alternative hypothesis: there is a statistically significant difference in the resistance to microtensile bond strength (μTBS) between direct and semi-direct restorations in dentin.
2. Materials and Methods
2.1. Experimental Design
This ex vivo study was approved by Ethical Committee of the IRB of the Faculty of Medicine—University of Coimbra (notification CE001/2013). After patient’s informed consent, 23 mandibular third molars with no caries, fissures or restorations were collected from healthy individuals aged 18 to 40 years.
The external surfaces of the teeth were inspected and cleaned of all surrounding soft tissues or debris with periodontal curettes. Teeth were then stored at 4 °C in 1% Chloramine-T for one week and then transferred to distilled water until the start of the experimental procedures as indicated by ISO/TS 11405:2015.
2.2. Teeth Preparation
All molars were numbered and subsequently radiographed in order to determine enamel thickness and to locate the dentin–enamel junction for posterior guidance on enamel removal without damaging dentin.
Roots were then partially resected on all teeth so that the pulp tissues could be removed from the pulp chamber and remnant root canal system through cervical access. The pulp tissues were extirpated under 6.4× dental microscope magnification (Leica M300; Leica Microsystems AG, Heerbrugg, Germany) using an spherical diamond bur. The pulp cavity was then thoroughly irrigated with 2.5% sodium hypochlorite solution under 16× magnification to remove all organic debris and rinsed with distilled water to remove any residual sodium hypochlorite solution that could promote degradation of organic matter. The pulp chamber cavity was then restored using a universal adhesive system and composite resin. The adhesive system (Prime & Bond Active, Dentsply Sirona, Charlotte, NC, USA) was applied across all cavity surfaces with a micro brush for 20 s and gently dried with an air jet to ensure complete evaporation of the solvent. Once dried, the adhesive layer was light-cured for 20 s using a 1200 mW/cm2 power light-curing unit (Bluephase Style 20i, Ivoclar Vivadent, Schaan, Liechtenstein). After, the cavity was carefully filled with the fluid resin (Surefil SDR Flow, Dentsply Sirona, Charlotte, NC, USA) avoiding the formation of air bubbles. Each resin increment was applied with a maximum thickness of 1 mm using the oblique layering technique. Each layer of 1 mm was light-cured for 20 s, with the curing light positioned as close as possible to the tooth to ensure optimal polymerization.
After restoration, the cervical portion of each tooth was embedded in an acrylic resin base (Vertex, Vertex-Dental, Zeist, The Netherlands) for better handling, ensuring that the coronal portion remained clear. All teeth were stored in distilled water to prevent dentin dehydration.
The enamel was removed from all molars using a grinding wheel mounted on a dental model trimmer (Zenit, Spain) with a stream of water to remove debris, followed by precision grinding using a diamond cut-off wheel (Accutom-5, Struers, Cleveland, OH, USA) and refinement with 600-grit sandpaper disc.
2.3. Restorative Techniques
A sample of 16 molars was selected from the 23 collected and previously prepared molars and randomly distributed into 2 groups of 8 teeth each: the first group (Group SR) was restored with semi-direct composite resin restorations (Ceram x ST HV, Dentsply Sirona, Charlotte, NC, USA) cemented with resin cement (Variolink Esthetic LC, Ivoclar Vivadent, Schaan, Liechtenstein) and the second group (Group DR) was restored with direct composite resin restorations, using the same composite resin (Ceram X ST HV, Dentsply Sirona, Charlotte, NC, USA). In both groups, a two-step self-etch adhesive (Clearfil SE Bond 2, Kuraray, Tokyo, Japan) was used to bond the restorations and all photoactivation processes were carried out using a 1200 mW/cm
2 power light-curing unit (Bluephase Style 20i, Ivoclar Vivadent, Schaan, Liechtenstein). Moreover, before performing the restorative procedures, the dentin surface was dried with a jet of air to eliminate the excess moisture existing on the surface due to storage in distilled water. The composition and manufacturer of the products used are described in
Table 1, while the restorations were built as described below:
Group SR: Each restoration was made using the semi-direct technique described in the literature. The restoration was built directly on the exposed dentin surface with the application of 1 mm of composite resin increments spread into uniform layers of restorative material, followed by 20 s of polymerization. The procedure was repeated until the total thickness reached 4 mm. Once the desired thickness was achieved, the restoration was further light-cured for an additional 20 s on all surfaces to ensure complete polymerization. The restoration was then easily detached from the surface of the dentin using pliers, as it had not been acid-etched and bonded. After detachment of the restoration, the dentin surface was washed and dried with paper and a light jet of air. The inner surface of the restoration was air-abraded with 50 μm aluminum oxide particles (Airsonic
® mini sandblaster, Hager Werken, Duisburg, Germany), projected at a 45° inclination to increase roughness and surface energy. The two-step self-etch adhesive (Clearfil SE Bond 2, Kuraray, Tokyo, Japan) was then applied with a microbrush for 20 s on the inner surface of the restoration and on the dentin surface [
16]. Resin cement (Variolink Esthetic LC, Ivoclar Vivadent, Schaan, Liechtenstein) was then spread on the bonded surface of the restoration, which was then seated in position under constant load. After 3 min, the excess cement was removed and both agents, adhesive and resin cement, polymerized. Photoactivation was carried out for 20 s on each exposed wall of the restoration.
Group DR: After elimination of excess moisture, the acidic primer was actively applied over the dentin surface using a micro brush with a rubbing motion for 20 s. The bond portion of the adhesive was then applied, and any excess was removed with gentle air blowing for 5 s. The adhesive layer was then light-cured for 20 s [
17]. After that, the adhesive surface was covered with uniform 1 mm thick increments of composite resin (Ceram x Spectra ST HV). Each increment was then polymerized for 20 s. The restoration was finished when the composite resin reached 4 mm in thickness. Final polymerization was carried out for 20 s on each exposed wall of the restoration.
All samples (Group SR and Group DR) were then stored at 37 °C in distilled water for 1 month, assuring the aging of samples.
2.4. Specimens for Microtensile
After storage, each tooth was sectioned perpendicular to the adhesive interface under constant water cooling with a low-speed cutting saw at 3000 rpm and forward speed of 0.075 mm/s (Accutom-5, Struers, Cleveland, OH, USA). Cuts were performed orthogonally at 1 mm apart in the mesial–distal and buccal lingual directions, obtaining rods with approximately 1 mm
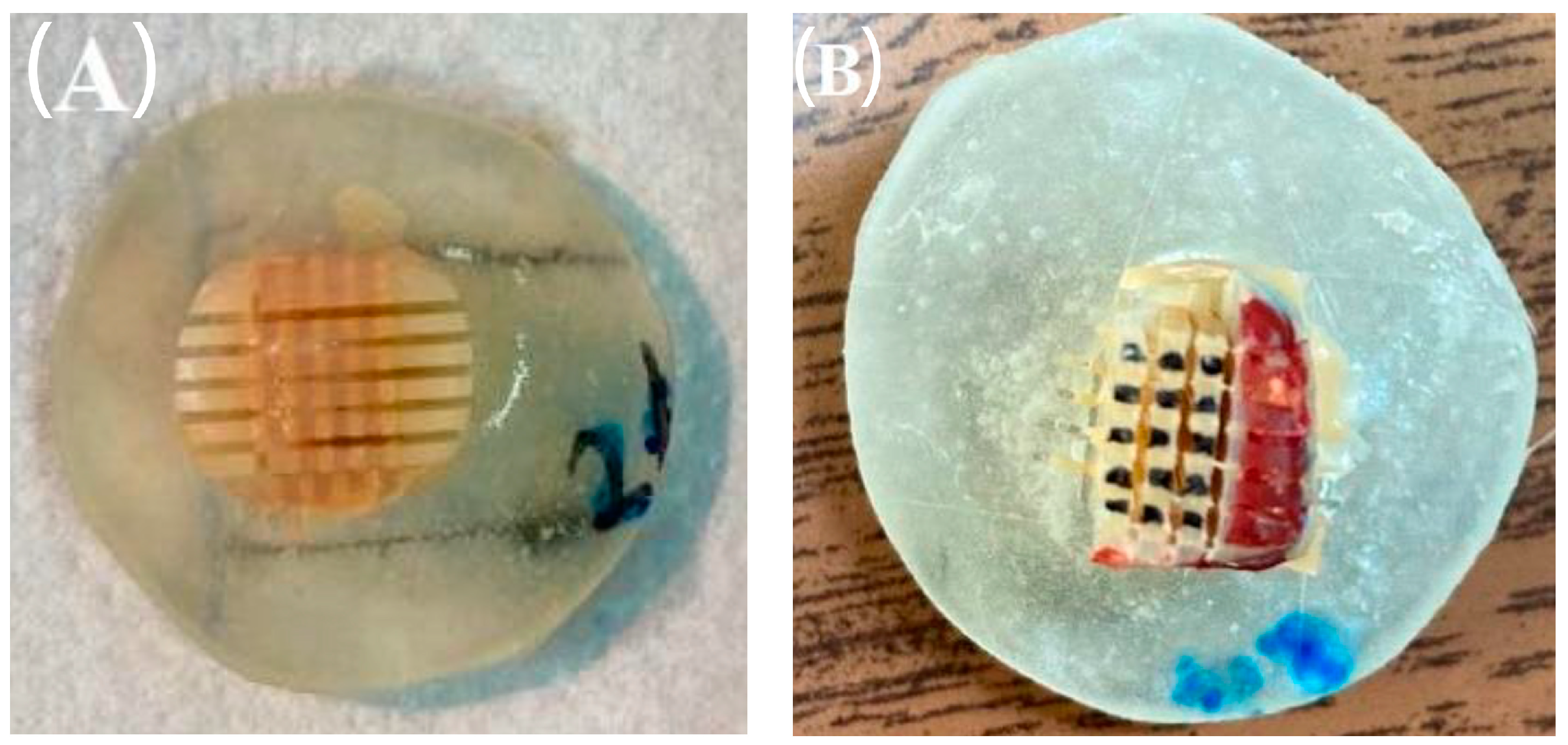
2 area, as it can be seen in
Figure 1. On each tooth, all rods were inspected for the presence of enamel and discarded accordingly (rods marked in red).
The cross-sectional area of the selected rods was confirmed with a digital caliper (Mod. 500-144b, Mitutoyo Sul America Ltda., Suzano, SP, Brazil) with a resolution of 0.01 mm and the corresponding data was recorded in a spreadsheet for posterior calculations.
2.5. Microtensile Tests
Each rod was individually fixed to metal jig using a cyanoacrylate adhesive (Instant Adhesive, Permabond, Permabond International, Englewood, NJ, USA) and then attached to a specific device for microtensile testing (Od04-Plus, Odeme Prod. Med. Odent., Luzerna, SC, Brazil), which is adapted to a universal testing machine (Autograph® AG-I, Shimadzu Corporation, Kyoto, Japan) for the μTBS test. Each specimen was pushed at a constant speed of 0.5 mm/min until failure. Failure load of each specimen (in Newtons) was recorded in a spreadsheet paired with the respective area to accurately determine the microtensile bond strength (MPa).
2.6. Failure Mode Analysis
Classification of the μTBS fracture pattern of each specimen was made using a digital optical microscope (Leica M300, Leica Microsystems, Heerbrugg, Switzerland) at 10× magnification and recorded in a spreadsheet. The fracture modes were classified as Adhesive (A), Mixed (M), Cement Cohesive (CC) and Dentin Cohesive (DC).
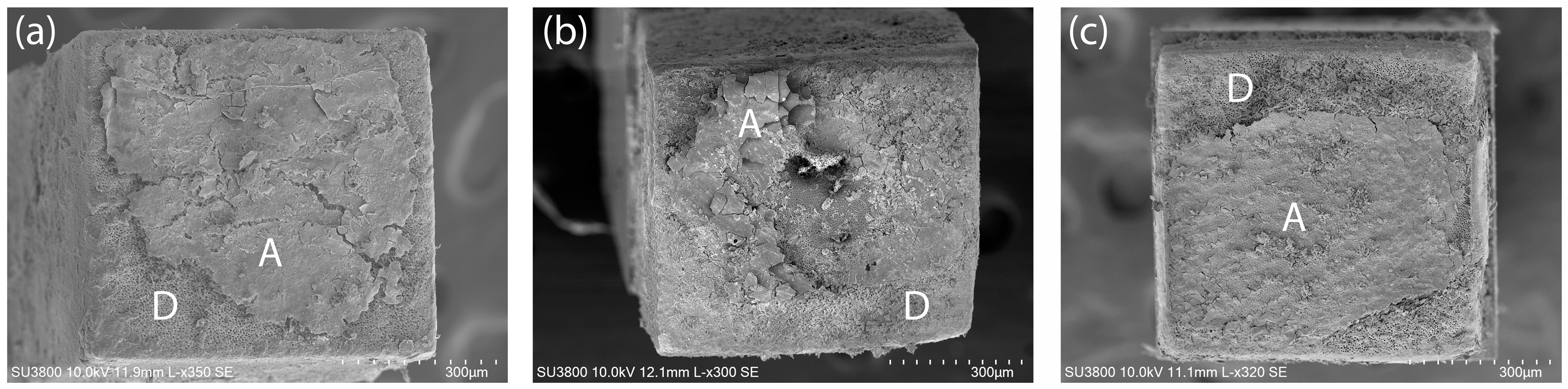
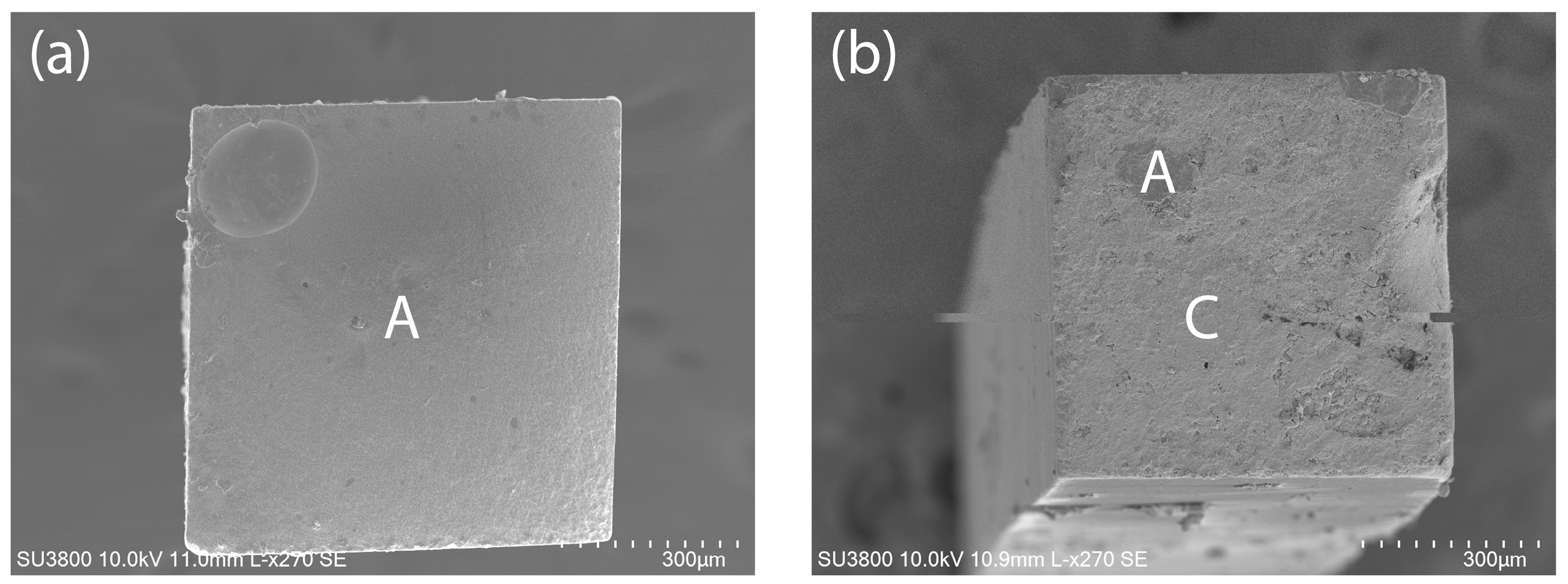
The surface topology of representative samples of each group and type of failure were also observed with a Scanning Electron Microscope (SEM) (Hitachi SU3800, Hitachi, Tokyo, Japan) with accelerating voltage of 10.0 kV, at magnifications ranging from 270× to 350×. All specimens were previously sputter-coated with gold particles of 3–5 nm (Cressington 108 auto Sputter Coater, Cressington Scientific Instruments Ltd., Watford, UK) and representative images of the samples from each group were captured using SEM (
Figure 2 and
Figure 3).
2.7. Statistical Analysis
The statistical analysis of μTBS data was performed using the SPSS Statistics 23.0 (SPSS, Chicago, IL, USA) [
5,
18]. Since the microtensile bond strength values did not meet the assumptions of normality (Kolmogorov–Smirnov test) and homogeneity of variances (Levène test) for each group, a non-parametric approach using the Mann–Whitney U test was used to compare the two groups. Pre-test failures (rods that fractured during the manipulation process) were excluded from the analysis. Evaluation of the association between groups and pre-test failures and failure modes was performed using the cross-tabulation feature and the Fisher’s Exact test and the Chi-Square test, respectively, with a confidence level of 95%.
3. Results
A total of 85 and 80 rods were obtained for groups DR and SR, respectively. Three rods were excluded from the DR group and 15 rods were excluded in the SR group due to pre-test failure, indicating that pre-test failures were not independent of the type of restoration (p = 0.002).
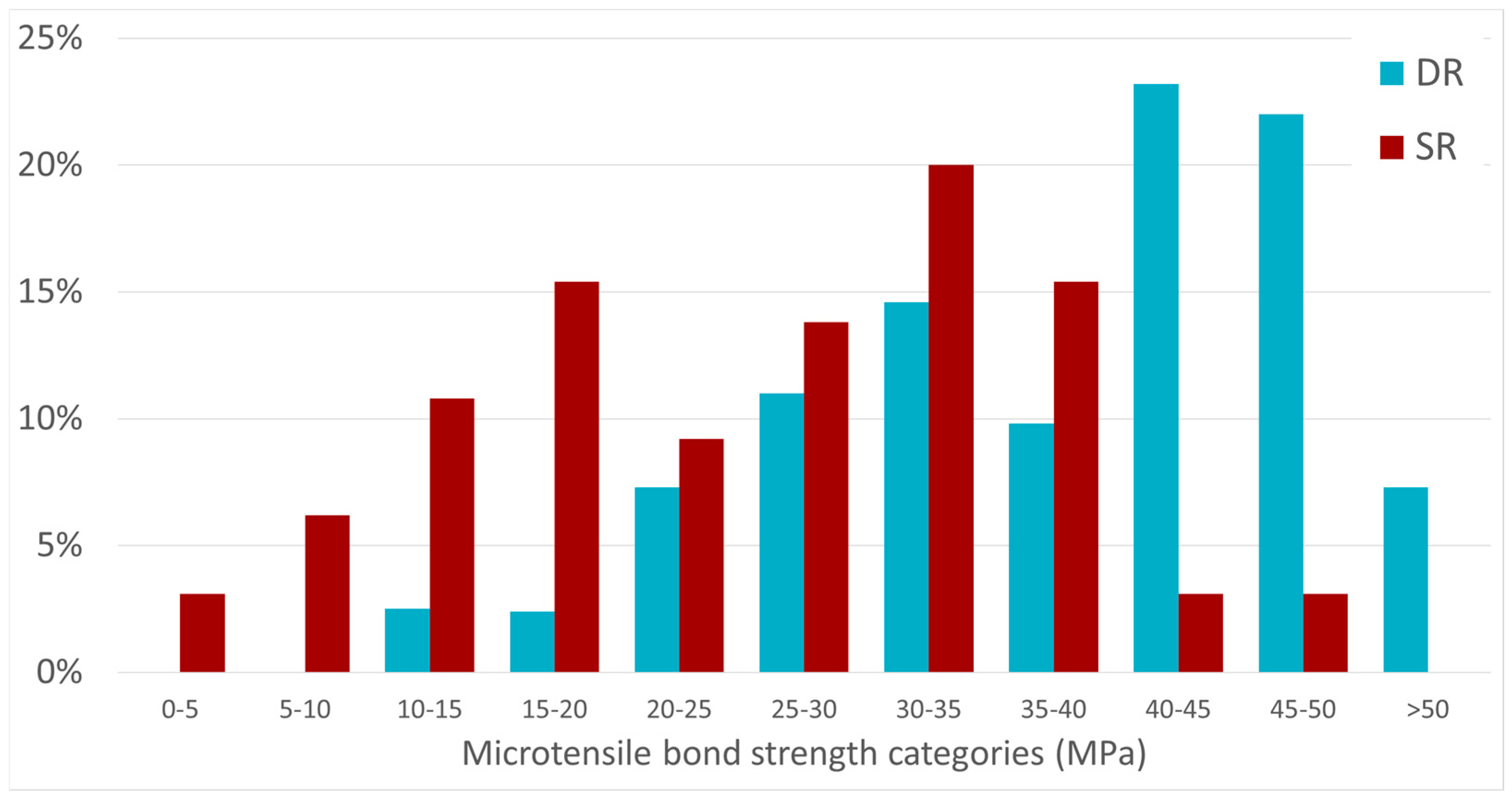
The bond strength data (MPa) of the DR and SR groups are shown in
Table 2. The mean microtensile bond strength of the DR group was 38.15 ± 10.75 MPa, whereas group SR presented a mean value of 25.45 ± 10.91 MPa. A similar difference of approximately 13 MPa was also observed for the median values of the microtensile bond strength for the two groups, which was statistically significant (
p < 0.001).
The distribution of frequencies of the two groups across the 5 MPa range categories of microtensile bond strength is presented in
Figure 4. It is possible to observe that more than a third of the IR group has values of μTBS that are below 10 MPa, whereas more than 50% of the DR group presents with μTBS values above 40 MPa.
The percentages of failure types according to the two groups of restorations are given in
Table 3, where only the IR group showed a predominance of adhesive failures, whereas the DR restoration group showed a predominance of cohesive failures in the composite.
The number of premature failures in the IR group was significantly higher than in the DR group. Improper sectioning can introduce microcracks or change the resistant cross-section of the specimens, leading to higher standard deviations. Nevertheless, the standard deviation values presented in
Table 2 for both groups are in good agreement. Hence, the higher percentage of premature failures in the IR group can be related to the polymerization phase, wherein the Clearfil SE Bond 2 adhesive seems to work well in the cementation of indirect restorations with a dual-cure resin cement (Clearfil Se Bond 2, Kuraray Nortikate Dental Inc., Tokyo, Japan).
4. Discussion
The present study evaluated the μTBS of direct and indirect composite resin restorations. It should be noted that despite the same restorative material and adhesive system being used in both restoration strategies, both restorations had significantly different adhesive strength and fracture patterns. Hence, the results indicate a statistically significant difference between the bond strength of the two types of restorations in the cervical region.
Before the microtensile test, a small number of premature failures, or pre-test failures (PF), were observed during the slice formation protocol. The occurrence of slice fails was related to several factors, such as the preparation and handling of the samples, the cutting parameters to obtain the slices, the variations in the more homogeneous structure of the dental substrate and the complex protocol due to the reduced dimensions of the samples. Moreover, in the indirect protocol, the stage of making the restoration, the cementation process and the thermal activation tend to transfer the problem to the thin layer of resin cement and adhesive, leading to higher levels of premature failure. In this study, the number of samples in the IR group was about 20% smaller than those used in the DR group. In the present study, the non-parametric Mann–Whitney U test was chosen because of its robustness in analyzing imbalanced sample sizes.
The results presented in
Table 3 show a minimum bond strength of 14.0 MPa for the DR group, while for the IR group, this value was 3.4 MPa, representing a value that is 77.1% smaller than that of the DR group. The disparity diminishes when comparing both groups’ maximum and average bond strength values, with observed differences of 32.4% and 33.3%, respectively. The results presented here agree with those presented in published works [
14,
19]. Generally, direct restorations have a higher micro tensile bond strength than indirect restorations, and one of the factors directly related to this is the polymerization process [
20,
21]. In direct restoration, the polymerization of all materials is performed in place. Hence, any shrinkage during material curing can create stress and marginal or internal gaps but can still allow for a continuous bond to the tooth, which is very difficult to ensure in the IR group. Nevertheless, in this study, the contraction of composite resin during photopolymerization does not seem to have a significant influence on the bond strength of the indirect restoration and, as evidence of this conclusion, the results in
Table 3 indicate that the IR group exhibits a high percentage of adhesive-type failures, and a very small percentage that are related to the cohesive failure of the composite resin. Moreover, the values of μTBS presented here are in agreement with those reported by other researchers [
12,
13,
22,
23]. Adhesion failure is a consequence of mechanical, chemical or biological factors and manifests by the physical separation of the bonded surfaces. The chemical mechanism of failure can include the disruption of molecular interactions produced by hydrolysis and water absorption, oxidation and degradation, chemical contaminants, pH and environmental effects, or weak interfacial bonding [
17]. The biological failure mechanism involves microbial and biochemical processes that weaken the linkage between the adhesive and substrate, resulting in biofilm formation, microbial degradation and biochemical corrosion.
Nevertheless, a more recent study developed by Delaíbera et al. [
4] reported no statistically significant differences in the μTBS between direct and indirect restorations in the cervical region of human premolars. The comparison of the μTBS values presented by Delaíbera et al. and those in
Table 2 reveals that the DR group has mean values that are two times higher. Moreover, the failure type of this group also shows some discrepancies; cohesive composite failure is dominant in this work, whereas in the research of Delaíbera et al., adhesive failure is dominant. The main reason for these differences might be related to the materials used, i.e., adhesive and resin cement, as well as composite resin and, eventually, with the restoration protocols or even tooth characteristics. The single bond universal adhesive (3M
TM ESPE, Single Bond Universal Adhesive, Technical Product Profile, St. Paul, MN, USA) used by Delaíbera et al. shows values for μTBs with the dentin that are in the range of 42–45 MPa. In contrast, the Clearfill
TM SE Bond 2 (CLEARFILL
TM SE BOND 2, Kurary Noritake Dental Inc., Tokyo, Japan) has values that might reach 70 MPa. On the other hand, the composite employed by Delaíbera et al. (3M
TM Filtek
TM Z350 XT, Universal Restorative, Technical Product Profile, St. Paul, MN, USA) has values of tensile strength that are similar to the Ceram x Sepctra ST HV composite.
The resin cement applied by Delaíbera and co-workers is a dual-polymerized resin, which has both chemical and light activation, allowing for complete polymerization even in places with no polymerization light [
24]. Nevertheless, light activation remains essential to achieve maximum conversion, optimal mechanical properties, and strong adhesion. The two materials used to create indirect restorations were the Rely X Ultimate dual-resin cement and the Single Bond Universal adhesive. In this study, the indirect restorations were built using the Ceram x Sepctra ST HV composite cemented through the Variolink Ivolcar LC (Variolink
® Esthetic, Ivoclar Vivadent, scientific Documentation, Schaan, Liechtenstein), and the cementation was initiated purely by light curing. The lower average bond strength of the IR group compared to the direct restoration group may be due to this resin cement layer. As reported in the literature [
25,
26], this is considered the weakest link in restoration strategies in which the restorative piece is cemented. The polymerization phase, after the restorative piece comes in contact, is to ensure the adhesion between the two substrates (dentin and composite resin). Nevertheless, the thickness and opacity of the composite material can reduce light penetration, leading to incomplete polymerization and residual monomers, which can reduce the mechanical strength and promote long-term degradation. On the other hand, resin-based cements shrink during polymerization and are the elements that are most subject to thermal changes; this can create gaps, microleakage and marginal breakdowns that may contribute to changes in the cement layer formed, compromising the marginal sealing and integrity of the restoration. Another factor that may influence the cement layer’s mechanical properties is its tendency to absorb water, so adequate polymerization of the cement is very important to avoid hydrolytic degradation. Nevertheless, because there is a significant variation between the minimum and maximum values of the IR group, there may have inadvertently been some violations of the restoration protocol. On the other hand, the indirect restoration protocol is semi-direct, since the restoration is created over the dentin without adhesion and is removed after for further cementation. In this process, we may be interfering with the dentin–collagen matrix by impregnating resinous compounds and the subsequent photopolymerization inside the dentinal tubules. Once the restorative piece is finished, when it is detached from the dentin, the dentin structure is altered and, possibly, the dentin tubes are obliterated, which will impair the subsequent cementation of the restorative piece and the ability to create a quality adhesive interface, influencing the adhesive strength values. One special recommendation to minimize the sectioning effect is to use a low-speed diamond saw with cooling to prevent damage. Additionally, the sectioning should be perpendicular with minimal force to prevent thermal stress and fractures and, finally, the specimens with visible cracks or irregularities should be discarded to ensure reliable data.
The analysis of the types of failure showed a higher percentage of adhesive-type failures in the indirect restoration group (
Table 3). The same was also observed in other studies [
11,
12,
13]. This is because the surface area of around 1 mm
2 allows most failures to be adhesive due to improved stress distribution during loading [
11]. We also observed a considerable percentage of cohesive composite failures in the DR group, which may have occurred due to small bubbles or gaps during incremental resin insertion, making the 1 mm
2 resin portion of some slices more fragile and prone to fracture. It was also observed that most of the universal adhesive was detached from the resin surface and remained covering the substrate in the indirect restoration groups, confirming resin adhesive failure,
Figure 4).
This study analyzed adhesion to dentin in a controlled environment without considering important factors in the oral cavity, such as mechanical stress, temperature, and the presence of saliva, all of which are factors that can alter adhesion values and reduce the effect found here. Even so, under the same conditions, using the same adhesive, we found a statistical difference between the two types of restorations.