Synergistic Action between Copper Oxide (CuO) Nanoparticles and Anthraquinone-2-Carboxylic Acid (AQ) against Staphylococcus aureus
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
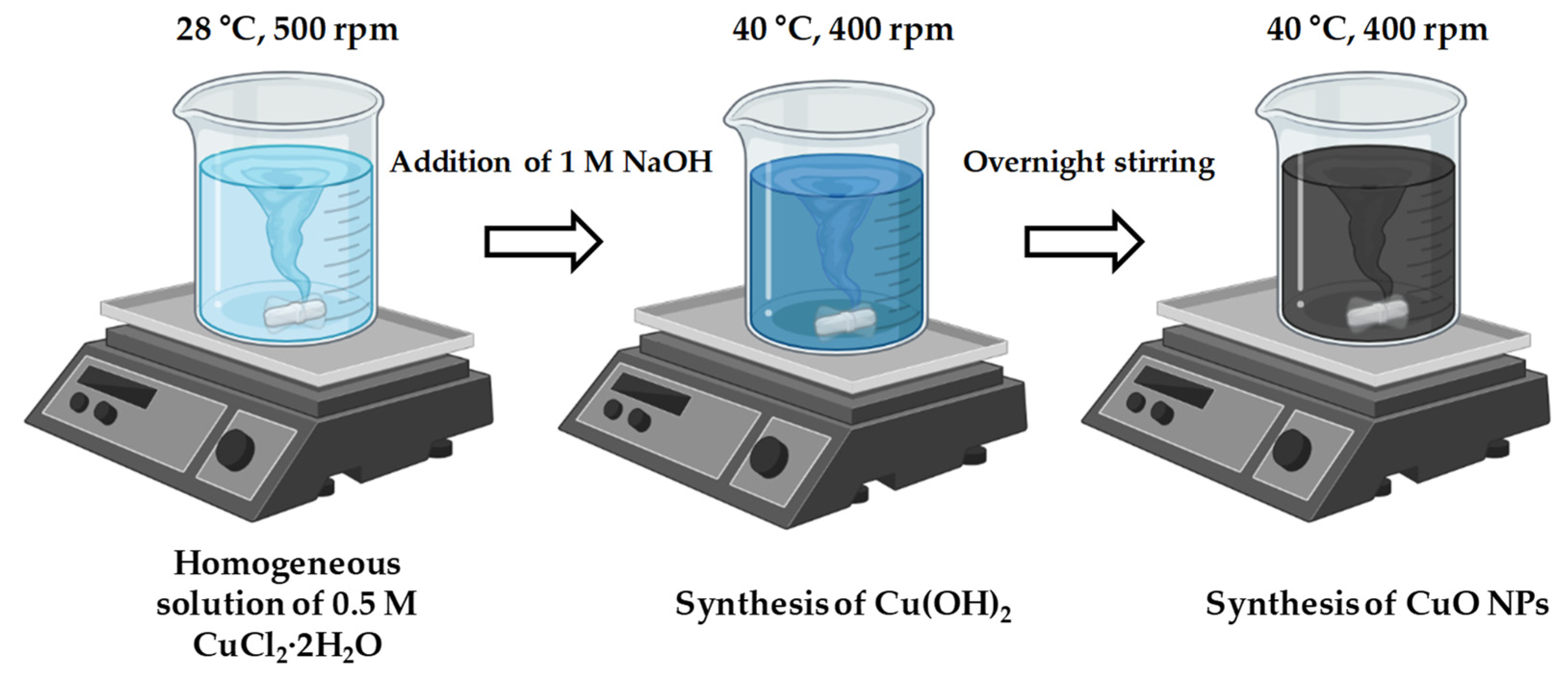
2.2. CuO NPs Synthesis
2.3. Characterization
2.3.1. X-ray Diffraction (XRD) and Transmission Electron Microscopy (TEM)
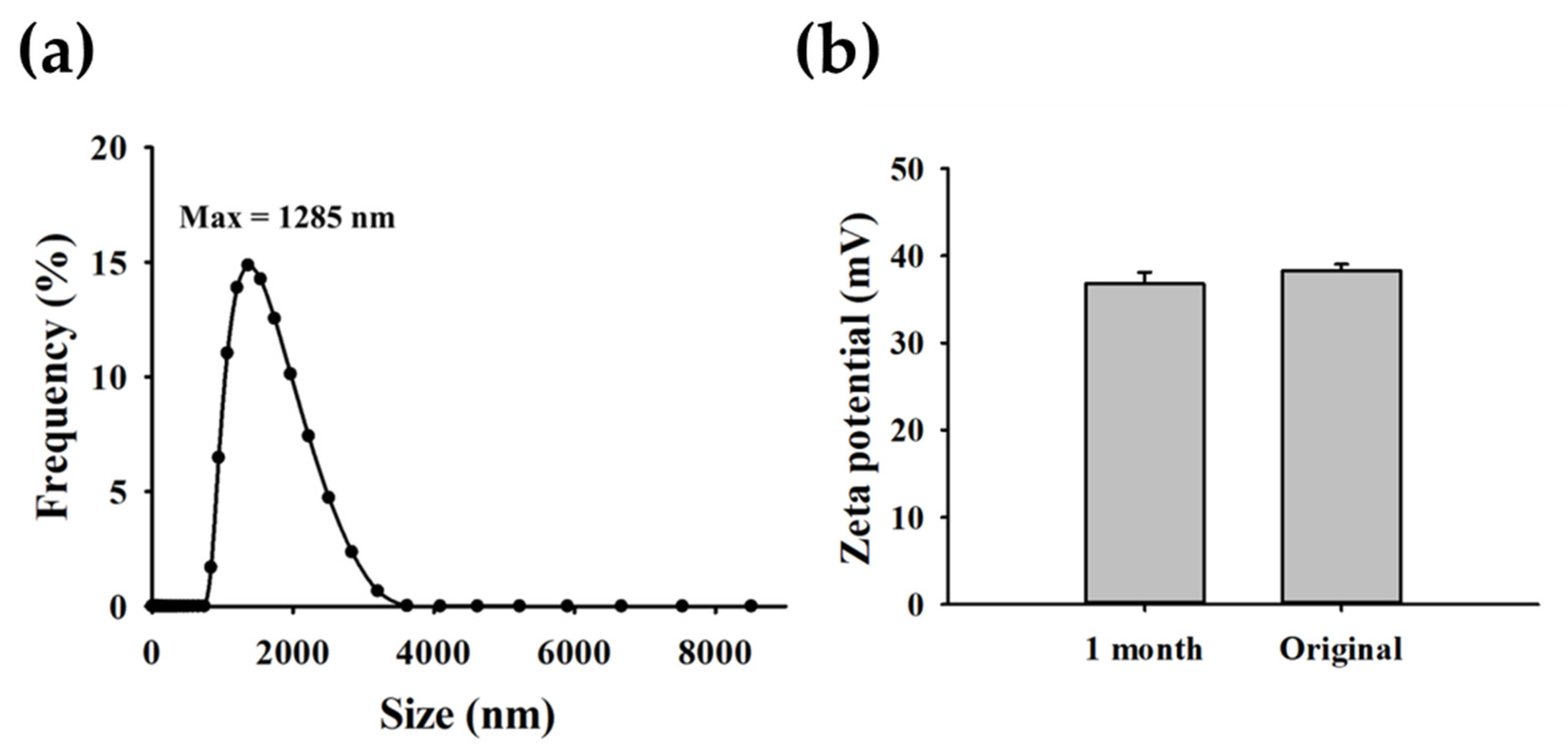
2.3.2. Dynamic Light Scattering (DLS) and Zeta Potential Measurement
2.3.3. Preparation of Bacterial Cells
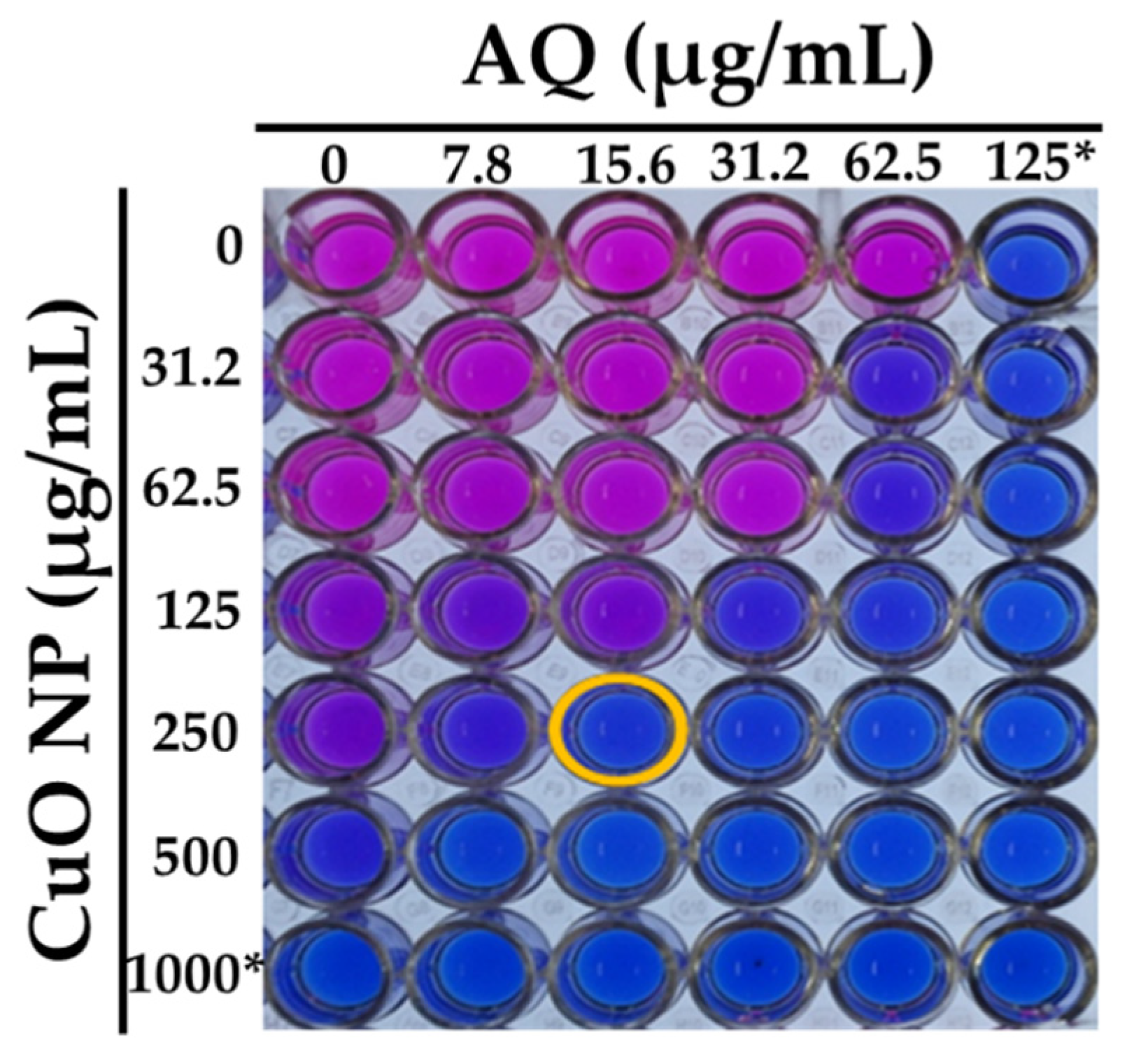
2.3.4. MIC Determination and Checkerboard Analysis
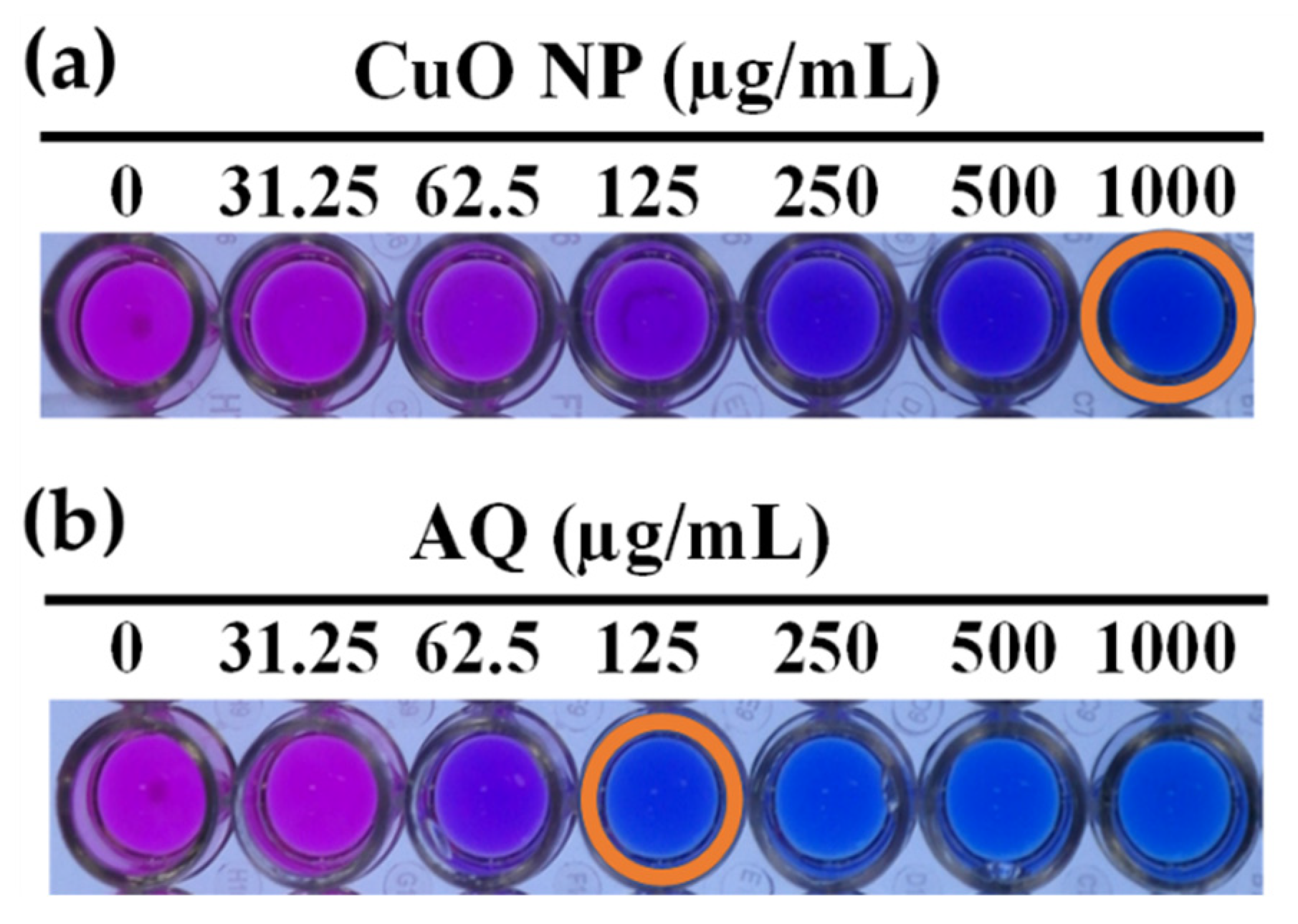
2.3.5. Resazurin Indicator Assay
2.3.6. Biofilm Formation Assay
2.3.7. Fluorescence Microscopy
2.3.8. Morphological Analysis of S. aureus ATCC 25923 with a Synergistic Combination
2.3.9. Mechanistic Evaluation of CuO NPs and AQ with Commercially Available Antibiotics
2.3.10. Statistical Analysis
3. Results and Discussion
3.1. Material Properties
3.1.1. XRD Pattern
3.1.2. Morphological Analysis
3.1.3. Size and Stability of CuO NPs
3.2. Antibacterial Activity
3.2.1. Evaluation of Antibacterial Activity
3.2.2. Checkerboard Analysis of CuO NPs/AQ Combination against S. aureus
3.3. Plausible Antibacterial Mechanism
3.3.1. Biofilm Inhibition Assay
3.3.2. Morphological Characterization of Cells: Cell Shrinkage and Loss of Cytoplasmic Volume
3.3.3. Mechanistic Behavior of the Synergistic Combination with Antibiotics
4. Limitations and Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roy, S.; Santra, S.; Das, A.; Dixith, S.; Sinha, M.; Ghatak, S.; Ghosh, N.; Banerjee, P.; Khanna, S.; Mathew-Steiner, S.; et al. Staphylococcus aureus Biofilm Infection Compromises Wound Healing by Causing Deficiencies in Granulation Tissue Collagen. Ann. Surg. 2020, 271, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Aguila-Arcos, S.; Alvarez-Rodriguez, I.; Garaiyurrebaso, O.; Garbisu, C.; Grohmann, E.; Alkorta, I. Biofilm-Forming Clinical Staphylococcus Isolates Harbor Horizontal Transfer and Antibiotic Resistance Genes. Front. Microbiol. 2017, 8, 2018. [Google Scholar] [CrossRef] [PubMed]
- Leon-Buitimea, A.; Garza-Cardenas, C.R.; Garza-Cervantes, J.A.; Lerma-Escalera, J.A.; Morones-Ramirez, J.R. The Demand for New Antibiotics: Antimicrobial Peptides, Nanoparticles, and Combinatorial Therapies as Future Strategies in Antibacterial Agent Design. Front. Microbiol. 2020, 11, 1669. [Google Scholar] [CrossRef] [PubMed]
- FakhriRavari, A.; Simiyu, B.; Morrisette, T.; Dayo, Y.; Abdul-Mutakabbir, J.C. Infectious disease: How to manage Gram-positive and Gram-negative pathogen conundrums with dual beta-lactam therapy. Drugs Context 2022, 11, 2021–8–9. [Google Scholar] [CrossRef] [PubMed]
- Grillo, S.; Puig-Asensio, M.; Schweizer, M.L.; Cuervo, G.; Oriol, I.; Pujol, M.; Carratala, J. The Effectiveness of Combination Therapy for Treating Methicillin-Susceptible Staphylococcus aureus Bacteremia: A Systematic Literature Review and a Meta-Analysis. Microorganisms 2022, 10, 848. [Google Scholar] [CrossRef] [PubMed]
- Slavin, Y.N.; Asnis, J.; Hafeli, U.O.; Bach, H. Metal nanoparticles: Understanding the mechanisms behind antibacterial activity. J. Nanobiotechnol. 2017, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Abo-Shama, U.H.; El-Gendy, H.; Mousa, W.S.; Hamouda, R.A.; Yousuf, W.E.; Hetta, H.F.; Abdeen, E.E. Synergistic and Antagonistic Effects of Metal Nanoparticles in Combination with Antibiotics Against Some Reference Strains of Pathogenic Microorganisms. Infect. Drug Resist. 2020, 13, 351–362. [Google Scholar] [CrossRef]
- Ermini, M.L.; Voliani, V. Antimicrobial Nano-Agents: The Copper Age. ACS Nano 2021, 15, 6008–6029. [Google Scholar] [CrossRef]
- Xiao, J.; Zhu, Y.; Huddleston, S.; Li, P.; Xiao, B.; Farha, O.K.; Ameer, G.A. Copper Metal-Organic Framework Nanoparticles Stabilized with Folic Acid Improve Wound Healing in Diabetes. ACS Nano 2018, 12, 1023–1032. [Google Scholar] [CrossRef]
- Guo, J.; Gao, S.H.; Lu, J.; Bond, P.L.; Verstraete, W.; Yuan, Z. Copper Oxide Nanoparticles Induce Lysogenic Bacteriophage and Metal-Resistance Genes in Pseudomonas aeruginosa PAO1. ACS Appl. Mater. Interfaces 2017, 9, 22298–22307. [Google Scholar] [CrossRef]
- Laha, D.; Pramanik, A.; Laskar, A.; Jana, M.; Pramanik, P.; Karmakar, P. Shape-dependent bactericidal activity of copper oxide nanoparticle mediated by DNA and membrane damage. Mater. Res. Bull. 2014, 59, 185–191. [Google Scholar] [CrossRef]
- Das, D.; Nath, B.C.; Phukon, P.; Dolui, S.K. Synthesis and evaluation of antioxidant and antibacterial behavior of CuO nanoparticles. Colloids Surf B Biointerfaces 2013, 101, 430–433. [Google Scholar] [CrossRef] [PubMed]
- Moniri Javadhesari, S.; Alipour, S.; Mohammadnejad, S.; Akbarpour, M.R. Antibacterial activity of ultra-small copper oxide (II) nanoparticles synthesized by mechanochemical processing against S. aureus and E. coli. Mater. Sci. Eng. C Mater. Biol. Appl. 2019, 105, 110011. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Miah, M.; Bera, A.; Saha, S.K.; Ghosh, B. Synthesis of freestanding 2D CuO nanosheets at room temperature through a simple surfactant free co-precipitation process and its application as electrode material in supercapacitors. J. Alloys Compd. 2021, 862. [Google Scholar] [CrossRef]
- Banoee, M.; Seif, S.; Nazari, Z.E.; Jafari-Fesharaki, P.; Shahverdi, H.R.; Moballegh, A.; Moghaddam, K.M.; Shahverdi, A.R. ZnO nanoparticles enhanced antibacterial activity of ciprofloxacin against Staphylococcus aureus and Escherichia coli. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 93, 557–561. [Google Scholar] [CrossRef]
- Roy, A.S.; Parveen, A.; Koppalkar, A.R.; Prasad, M.V.N.A. Effect of Nano-Titanium Dioxide with Different Antibiotics against Methicillin-Resistant Staphylococcus aureus. J. Biomater. Nanobiotechnol. 2010, 1, 37–41. [Google Scholar] [CrossRef]
- El-Telbany, M.; Mohamed, A.A.; Yahya, G.; Abdelghafar, A.; Abdel-Halim, M.S.; Saber, S.; Alfaleh, M.A.; Mohamed, A.H.; Abdelrahman, F.; Fathey, H.A.; et al. Combination of Meropenem and Zinc Oxide Nanoparticles; Antimicrobial Synergism, Exaggerated Antibiofilm Activity, and Efficient Therapeutic Strategy against Bacterial Keratitis. Antibiotics 2022, 11, 1374. [Google Scholar] [CrossRef]
- Ruden, S.; Hilpert, K.; Berditsch, M.; Wadhwani, P.; Ulrich, A.S. Synergistic interaction between silver nanoparticles and membrane-permeabilizing antimicrobial peptides. Antimicrob. Agents Chemother. 2009, 53, 3538–3540. [Google Scholar] [CrossRef]
- Zhong, L.; Liu, H.; Samal, M.; Yun, K. Synthesis of ZnO nanoparticles-decorated spindle-shaped graphene oxide for application in synergistic antibacterial activity. J. Photochem. Photobiol. B 2018, 183, 293–301. [Google Scholar] [CrossRef]
- Verma, S.K.; Jha, E.; Panda, P.K.; Das, J.K.; Thirumurugan, A.; Suar, M.; Parashar, S.K.S. Molecular aspects of core-shell intrinsic defect induced enhanced antibacterial activity of ZnO nanocrystals. Nanomedicine 2018, 13, 43–68. [Google Scholar] [CrossRef]
- Bezza, F.A.; Tichapondwa, S.M.; Chirwa, E.M.N. Fabrication of monodispersed copper oxide nanoparticles with potential application as antimicrobial agents. Sci. Rep. 2020, 10, 16680. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.; Zhang, Y. Teaching an old dog new tricks: Drug discovery by repositioning natural products and their derivatives. Drug Discov. Today 2022, 27, 1936–1944. [Google Scholar] [CrossRef] [PubMed]
- Nourbakhsh, F.; Lotfalizadeh, M.; Badpeyma, M.; Shakeri, A.; Soheili, V. From plants to antimicrobials: Natural products against bacterial membranes. Phytother. Res. 2022, 36, 33–52. [Google Scholar] [CrossRef] [PubMed]
- Guzzo, F.; Scognamiglio, M.; Fiorentino, A.; Buommino, E.; D’Abrosca, B. Plant Derived Natural Products against Pseudomonas aeruginosa and Staphylococcus aureus: Antibiofilm Activity and Molecular Mechanisms. Molecules 2020, 25, 5024. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Kim, Y.G.; Yong Ryu, S.; Lee, J. Calcium-chelating alizarin and other anthraquinones inhibit biofilm formation and the hemolytic activity of Staphylococcus aureus. Sci. Rep. 2016, 6, 19267. [Google Scholar] [CrossRef]
- Coenye, T.; Honraet, K.; Rigole, P.; Nadal Jimenez, P.; Nelis, H.J. In vitro inhibition of Streptococcus mutans biofilm formation on hydroxyapatite by subinhibitory concentrations of anthraquinones. Antimicrob. Agents Chemother. 2007, 51, 1541–1544. [Google Scholar] [CrossRef]
- Nam, W.; Kim, S.P.; Nam, S.H.; Friedman, M. Structure-Antioxidative and Anti-Inflammatory Activity Relationships of Purpurin and Related Anthraquinones in Chemical and Cell Assays. Molecules 2017, 22, 265. [Google Scholar] [CrossRef]
- Wei, Y.; Liu, Q.; Yu, J.; Feng, Q.; Zhao, L.; Song, H.; Wang, W. Antibacterial mode of action of 1,8-dihydroxy-anthraquinone from Porphyra haitanensis against Staphylococcus aureus. Nat. Prod. Res. 2015, 29, 976–979. [Google Scholar] [CrossRef]
- Wang, J.; Qu, Q.; Liu, X.; Cui, W.; Yu, F.; Chen, X.; Xing, X.; Zhou, Y.; Yang, Y.; Bello-Onaghise, G.; et al. 1-Hydroxyanthraquinone exhibited antibacterial activity by regulating glutamine synthetase of Staphylococcus xylosus as a virulence factor. Biomed. Pharmacother. 2020, 123, 109779. [Google Scholar] [CrossRef]
- Lee, J.H.; Kim, Y.G.; Park, S.; Hu, L.; Lee, J. Phytopigment Alizarin Inhibits Multispecies Biofilm Development by Cutibacterium acnes, Staphylococcus aureus, and Candida albicans. Pharmaceutics 2022, 14, 1047. [Google Scholar] [CrossRef]
- Zhou, J.; Qi, G.B.; Wang, H. A purpurin-peptide derivative for selective killing of Gram-positive bacteria via insertion into cell membrane. J. Mater. Chem. B 2016, 4, 4855–4861. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.M.; Zhang, J.L.; Zhou, K.; Yue, L.M.; Zhang, Y.; Wang, C.Y.; Wang, K.L.; Xu, Y. Anthraquinones as Potential Antibiofilm Agents Against Methicillin-Resistant Staphylococcus aureus. Front. Microbiol. 2021, 12, 709826. [Google Scholar] [CrossRef] [PubMed]
- Xiang, H.; Cao, F.; Ming, D.; Zheng, Y.; Dong, X.; Zhong, X.; Mu, D.; Li, B.; Zhong, L.; Cao, J.; et al. Aloe-emodin inhibits Staphylococcus aureus biofilms and extracellular protein production at the initial adhesion stage of biofilm development. Appl. Microbiol. Biotechnol. 2017, 101, 6671–6681. [Google Scholar] [CrossRef] [PubMed]
- Dukanovic, S.; Ganic, T.; Loncarevic, B.; Cvetkovic, S.; Nikolic, B.; Tenji, D.; Randjelovic, D.; Mitic-Culafic, D. Elucidating the antibiofilm activity of Frangula emodin against Staphylococcus aureus biofilms. J. Appl. Microbiol. 2022, 132, 1840–1855. [Google Scholar] [CrossRef] [PubMed]
- Park, B.S.; Kim, J.R.; Lee, S.E.; Kim, K.S.; Takeoka, G.R.; Ahn, Y.J.; Kim, J.H. Selective growth-inhibiting effects of compounds identified in Tabebuia impetiginosa inner bark on human intestinal bacteria. J. Agric. Food Chem. 2005, 53, 1152–1157. [Google Scholar] [CrossRef]
- Yi, S.; Wu, Y.; Zhang, Y.; Zou, Y.; Dai, F.; Si, Y. Antibacterial Activity of Photoactive Silk Fibroin/Cellulose Acetate Blend Nanofibrous Membranes against Escherichia coli. ACS Sustain. Chem. Eng. 2020, 8, 16775–16780. [Google Scholar] [CrossRef]
- Vanamala, K.; Tatiparti, K.; Bhise, K.; Sau, S.; Scheetz, M.H.; Rybak, M.J.; Andes, D.; Iyer, A.K. Novel approaches for the treatment of methicillin-resistant Staphylococcus aureus: Using nanoparticles to overcome multidrug resistance. Drug Discov. Today 2021, 26, 31–43. [Google Scholar] [CrossRef]
- Bai, B.; Saranya, S.; Dheepaasri, V.; Muniasamy, S.; Alharbi, N.S.; Selvaraj, B.; Undal, V.S.; Gnanamangai, B.M. Biosynthesized copper oxide nanoparticles (CuO NPs) enhances the anti-biofilm efficacy against K. pneumoniae and S. aureus. J. King Saud Univ. Sci. 2022, 34, 102120. [Google Scholar] [CrossRef]
- Naskar, A.; Cho, H.; Kim, K.S. A Nanocomposite with Extracellular Vesicles from Lactobacillus paracasei as a Bioinspired Nanoantibiotic Targeting Staphylococcus aureus. Pharmaceutics 2022, 14, 2273. [Google Scholar] [CrossRef]
- Kumari, P.; Panda, P.K.; Jha, E.; Kumari, K.; Nisha, K.; Mallick, M.A.; Verma, S.K. Mechanistic insight to ROS and Apoptosis regulated cytotoxicity inferred by Green synthesized CuO nanoparticles from Calotropis gigantea to Embryonic Zebrafish. Sci. Rep. 2017, 7, 16284. [Google Scholar] [CrossRef]
- Naskar, A.; Shin, J.; Kim, K.S. A MoS2 based silver-doped ZnO nanocomposite and its antibacterial activity against beta-lactamase expressing Escherichia coli. RSC Adv. 2022, 12, 7268–7275. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.-S.; Kim, T.; Pan, J.G. In vitro evaluation of ciclopirox as an adjuvant for polymyxin B against gram-negative bacteria. J. Antibiot. 2015, 68, 395–398. [Google Scholar] [CrossRef] [PubMed]
- Arul Selvaraj, R.C.; Rajendran, M.; Nagaiah, H.P. Re-Potentiation of beta-Lactam Antibiotic by Synergistic Combination with Biogenic Copper Oxide Nanocubes against Biofilm Forming Multidrug-Resistant Bacteria. Molecules 2019, 24, 3055. [Google Scholar] [CrossRef]
- Caso Coelho, V.; Pereira Neves, S.D.; Cintra Giudice, M.; Benard, G.; Lopes, M.H.; Sato, P.K. Evaluation of antimicrobial susceptibility testing of Nocardia spp. isolates by broth microdilution with resazurin and spectrophotometry. BMC Microbiol. 2021, 21, 331. [Google Scholar] [CrossRef] [PubMed]
- O’Toole, G.A. Microtiter dish biofilm formation assay. J. Vis. Exp. 2011, 2437. [Google Scholar] [CrossRef]
- Pham, D.T.N.; Khan, F.; Phan, T.T.V.; Park, S.K.; Manivasagan, P.; Oh, J.; Kim, Y.M. Biofilm inhibition, modulation of virulence and motility properties by FeOOH nanoparticle in Pseudomonas aeruginosa. Braz. J. Microbiol. 2019, 50, 791–805. [Google Scholar] [CrossRef]
- Shin, J.; Naskar, A.; Ko, D.; Kim, S.; Kim, K.-S. Bioconjugated Thymol-Zinc Oxide Nanocomposite as a Selective and Biocompatible Antibacterial Agent against Staphylococcus Species. Int. J. Mol. Sci. 2022, 23, 6770. [Google Scholar] [CrossRef]
- Shin, J.; Magar, K.B.S.; Lee, J.; Kim, K.-S.; Lee, Y.R. Design, synthesis, and discovery of novel oxindoles bearing 3-heterocycles as species-specific and combinatorial agents in eradicating Staphylococcus species. Sci. Rep. 2019, 9, 8012. [Google Scholar] [CrossRef]
- Cheng, G.; Hight Walker, A.R. Transmission electron microscopy characterization of colloidal copper nanoparticles and their chemical reactivity. Anal. Bioanal. Chem. 2010, 396, 1057–1069. [Google Scholar] [CrossRef]
- Ingle, A.P.; Rai, M. Copper nanoflowers as effective antifungal agents for plant pathogenic fungi. IET Nanobiotechnol. 2017, 11, 546–551. [Google Scholar] [CrossRef]
- Nicolae Dopcea, G.; Dopcea, I.; Nanu, A.E.; Diguta, C.F.; Matei, F. Resistance and cross-resistance in Staphylococcus spp. strains following prolonged exposure to different antiseptics. J. Glob. Antimicrob. Resist. 2020, 21, 399–404. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.M.; Horswill, A.R. Staphylococcus epidermidis-Skin friend or foe? PLoS Pathog. 2020, 16, e1009026. [Google Scholar] [CrossRef]
- Byrd, A.L.; Deming, C.; Cassidy, S.K.B.; Harrison, O.J.; Ng, W.I.; Conlan, S.; Program, N.C.S.; Belkaid, Y.; Segre, J.A.; Kong, H.H. Staphylococcus aureus and Staphylococcus epidermidis strain diversity underlying pediatric atopic dermatitis. Sci. Transl. Med. 2017, 9, eaal4651. [Google Scholar] [CrossRef] [PubMed]
- Jena, S.; Panda, S.; Nayak, K.C.; Singh, D.V. Identification of Major Sequence Types among Multidrug-Resistant Staphylococcus epidermidis Strains Isolated from Infected Eyes and Healthy Conjunctiva. Front. Microbiol. 2017, 8, 1430. [Google Scholar] [CrossRef]
- Hiltunen, A.K.; Savijoki, K.; Nyman, T.A.; Miettinen, I.; Ihalainen, P.; Peltonen, J.; Fallarero, A. Structural and Functional Dynamics of Staphylococcus aureus Biofilms and Biofilm Matrix Proteins on Different Clinical Materials. Microorganisms 2019, 7, 584. [Google Scholar] [CrossRef]
- Schilcher, K.; Horswill, A.R. Staphylococcal biofilm development: Structure, regulation, and treatment strategies. Microbiol. Mol. Biol. Rev. 2020, 84, e00026-19. [Google Scholar] [CrossRef]
- Rajamohan, R.; Raorane, C.J.; Kim, S.C.; Lee, Y.R. One Pot Synthesis of Copper Oxide Nanoparticles for Efficient Antibacterial Activity. Materials 2022, 16, 217. [Google Scholar] [CrossRef]
- Dell’Annunziata, F.; Folliero, V.; Palma, F.; Crudele, V.; Finamore, E.; Sanna, G.; Manzin, A.; De Filippis, A.; Galdiero, M.; Franci, G. Anthraquinone Rhein Exhibits Antibacterial Activity against Staphylococcus aureus. Appl. Sci. 2022, 12, 8691. [Google Scholar] [CrossRef]
- Cruz, C.D.; Shah, S.; Tammela, P. Defining conditions for biofilm inhibition and eradication assays for Gram-positive clinical reference strains. BMC Microbiol. 2018, 18, 173. [Google Scholar] [CrossRef]
- Ravikumar, V.; Mijakovic, I.; Pandit, S. Antimicrobial Activity of Graphene Oxide Contributes to Alteration of Key Stress-Related and Membrane Bound Proteins. Int. J. Nanomed. 2022, 17, 6707–6721. [Google Scholar] [CrossRef]
- Lebre, P.H.; De Maayer, P.; Cowan, D.A. Xerotolerant bacteria: Surviving through a dry spell. Nat. Rev. Microbiol. 2017, 15, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Kornder, J.D. Streptomycin revisited: Molecular action in the microbial cell. Med. Hypotheses 2002, 58, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Aguirre Rivera, J.; Larsson, J.; Volkov, I.L.; Seefeldt, A.C.; Sanyal, S.; Johansson, M. Real-time measurements of aminoglycoside effects on protein synthesis in live cells. Proc. Natl. Acad. Sci. USA 2021, 118, e2013315118. [Google Scholar] [CrossRef] [PubMed]





| Species | Strain Type | Strain Number | MIC (µg/mL) | |
|---|---|---|---|---|
| CuO NPs | AQ | |||
| S. aureus | Type MDR MDR | ATCC 25923 MRSA1 MRSA2 | 1000 1000 1000 | 125 250 250 |
| S. epidermidis | Type MSSE | KCTC 13171 ATCC 12228 | 1000 500 | 125 62.5 |
| S. saprophyticus | Type | ATCC 15305 | 1000 | 250 |
| Species | Strain Type | Strain ID | Single Component | Combination | |||
|---|---|---|---|---|---|---|---|
| MIC (µg/mL) | FICI | ||||||
| CuO NPs | AQ | CuO NPs | AQ | ||||
| S. aureus | Type MDR MDR | ATCC 25923 MRSA1 MRSA2 | 1000 1000 1000 | 125 250 250 | 250 250 500 | 15.6 125 62.5 | 0.37 0.75 0.75 |
| S. epidermidis | Type MSSE | KCTC 13171 ATCC 12228 | 1000 500 | 125 62.5 | 250 250 | 62.5 15.6 | 0.75 0.75 |
| S. saprophyticus | Type | ATCC 15305 | 1000 | 250 | 500 | 125 | 1 |
| Antibiotics | Acronym | MIC 1 (μg/mL) | |||
|---|---|---|---|---|---|
| Control | +CuO NPs | +AQ | Synergy | ||
| Kanamycin | KAN | <1 | <1 | <1 | <1 |
| Streptomycin | STR | 2 | <1 | 4 | <1 |
| Tiamulin | TIA | 0.5 | 0.5 | 0.5 | 0.5 |
| Quinupristin/dalfopristin | SYN | 0.25 | 1 | 0.25 | 0.5 |
| Linezolid | LZD | 2 | 2 | 2 | 2 |
| Mupirocin | MUP | <0.12 | <0.12 | <0.12 | <0.12 |
| Vancomycin | VAN | 1 | 2 | 1 | 1 |
| Chloramphenicol | CHL | 8 | 8 | 8 | 8 |
| Fusidic acid | FUS | 0.25 | 0.25 | 0.5 | 0.5 |
| Penicillin | PEN | 0.06 | 0.12 | 0.06 | 0.12 |
| Trimethoprim | TMP | >4 | >4 | 2 | >4 |
| Rifampin | RIF | 0.008 | <0.008 | 0.015 | 0.008 |
| Erythromycin | ERY | 0.25 | 0.25 | 0.25 | 0.25 |
| Ciprofloxacin | CIP | 0.12 | 0.12 | 0.25 | 0.25 |
| Tetracycline | TET | 0.25 | 0.5 | 0.25 | 0.5 |
| Clindamycin | CLI | 0.12 | 0.12 | 0.06 | 0.12 |
| Cefoxitin | FOX | 2 | 1 | 2 | 2 |
| Gentamicin | GEN | 0.25 | 0.12 | 0.25 | <0.12 |
| Sulfamethoxazole | SMX | 32 | 128 | >128 | >128 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Srivastava, P.; Kim, Y.; Cho, H.; Kim, K.-s. Synergistic Action between Copper Oxide (CuO) Nanoparticles and Anthraquinone-2-Carboxylic Acid (AQ) against Staphylococcus aureus. J. Compos. Sci. 2023, 7, 135. https://doi.org/10.3390/jcs7040135
Srivastava P, Kim Y, Cho H, Kim K-s. Synergistic Action between Copper Oxide (CuO) Nanoparticles and Anthraquinone-2-Carboxylic Acid (AQ) against Staphylococcus aureus. Journal of Composites Science. 2023; 7(4):135. https://doi.org/10.3390/jcs7040135
Chicago/Turabian StyleSrivastava, Prakhar, Yongjun Kim, Hyejin Cho, and Kwang-sun Kim. 2023. "Synergistic Action between Copper Oxide (CuO) Nanoparticles and Anthraquinone-2-Carboxylic Acid (AQ) against Staphylococcus aureus" Journal of Composites Science 7, no. 4: 135. https://doi.org/10.3390/jcs7040135
APA StyleSrivastava, P., Kim, Y., Cho, H., & Kim, K.-s. (2023). Synergistic Action between Copper Oxide (CuO) Nanoparticles and Anthraquinone-2-Carboxylic Acid (AQ) against Staphylococcus aureus. Journal of Composites Science, 7(4), 135. https://doi.org/10.3390/jcs7040135







