Delayed Speech Perception and Production after Cochlear Implantation in Bilingual Children from Non-Native Families
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
- longer acquisition time for language comprehension and correct sentence construction;
- fluctuating performance due to absence from speech therapy sessions (e.g., during periods spent back in their homelands); and
- weak verbal memory and persistence of family linguistic model for a long time.
- early diagnosis and application of hearing aid;
- optimal mapping of the CI (or CIs if binaural) and tailored fitting of the contralateral hearing aid (if present);
- good cooperation and regular involvement of the family;
- intensive and constant long-term speech therapy;
- regular exercise at home in own primary language; and
- stimulating linguistic environment at home, in social activities and educational setting.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jordaan, H. Clinical Intervention for Bilingual Children: An International Survey. Folia Phoniatr. Logop. 2008, 60, 97–105. [Google Scholar] [CrossRef] [PubMed]
- Bialystok, E.; Feng, X. Language proficiency and executive control in proactive interference: Evidence from monolingual and bilingual children and adults. Brain Lang. 2009, 109, 93–100. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman-Phillips, S.; Robbins, A.M.; Osberger, M.J. Assessing cochlear implant benefit in very young children. Ann. Otol. Rhinol. Laryngol. Suppl. 2000, 185, 42–43. [Google Scholar] [CrossRef]
- Archbold, S. Monitoring progress in children at the preverbal stage. In Cochlear Implants for Young Children; McCornick, B., Sheppard, S., Eds.; Whurr: London, UK, 1994; pp. 197–213. [Google Scholar]
- Archbold, S.; Lutman, M.; Marshall, D. Categories of auditory performance. Ann. Otol. Rhinol. Laryngol. Suppl. 1995, 166, 312–314. [Google Scholar] [PubMed]
- Zimmerman-Phillips, S.; Robbins, A.M.; Osberger, M.J. The Meaningful Use of Speech Scale; Indiana University School of Medicine Press: Indianapolis, IN, USA, 1992. [Google Scholar]
- ISTAT. Istituto Superiore di Statistica-Censimento Generale della Popolazione Italiana 2011–Gazzetta Ufficiale della Repubblica Italiana n°294, Istituto Poligrafico e Zecca dello Stato S.p.A., Roma, Italia, 18 December 2012. Available online: https://www.gazzettaufficiale.it (accessed on 12 March 2021).
- Robbins, A.M.; Green, J.A.; Waltzman, S.B. Bilingual oral language proficiency in children with cochlear implants. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 644–647. [Google Scholar] [CrossRef]
- Paradise, J.; Nicoladis, E.; Genesse, F. Early emergence of structural constraints on code-mixing: Evidence from French-English bilingual children. Bilingualism 2000, 3, 348–352. [Google Scholar] [CrossRef]
- Deuchar, M.; Quay, S. Bilingual Acquisition: Theoretical Implications of a Case Study; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Comeau, L.; Genesee, F. Bilingual children’s repair strategies during dyadic communication. In Trends in Bilingual Acqui-Sition; Cenoz, J., Genesee, F., Eds.; John Benjamin: Amsterdam, The Netherlands, 2001; pp. 231–256. [Google Scholar]
- Gutiérrez-Clellen, V.F.; Simon-Cereijido, G.; Wagner, C. Bilingual children with language impairment: A comparison with monolinguals and second language learners. Appl. Psycholinguist. 2008, 29, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.A.; Bunta, F. Positive and negative transfer in the phonological systems of bilingual speakers. Int. J. Biling. 2011, 16, 388–401. [Google Scholar] [CrossRef]
- Genessee, F. Bilingualism and language impairment. In MIT Encyclopedia of Communication Disorders; Kent, R., Ed.; The MIT Press: Cambridge, MA, USA, 2003. [Google Scholar]
- Waltzman, S.B.; Robbins, A.M.; Green, J.E.; Cohen, N.L. Second oral language capabilities in children with cochlear im-plants. Otol. Neurotol. 2003, 24, 757–763. [Google Scholar] [CrossRef]
- Genessee, F.; Nicoladis, E. Language development in bilingual preschool children. In Meeting the Challenge of Linguistics and Cultural Diversity in Early Childhood; Garcia, E., McLaughlin, B., Eds.; Teachers College Press: New York, NY, USA, 1995; pp. 18–33. [Google Scholar]
- Rabbit, P. Mild hearing loss can cause apparent memory failures which increase with age and reduce with IQ. Acta Otolaryngol. Suppl. 1991, 476, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Robbins, A.M.; Koch, D.B.; Osberger, M.J.; Zimmerman-Phillips, S.; Kishon-Rabin, L. Effect of Age at Cochlear Implantation on Auditory Skill Development in Infants and Toddlers. Arch. Otolaryngol. Head Neck Surg. 2004, 130, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.; El-Kashlan, H.; Zwolan, T.A. Children with Cochlear Implants Who Live in Monolingual and Bilingual Homes. Otol. Neurotol. 2008, 29, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Bunta, F.; Douglas, M. The Effects of Dual-Language Support on the Language Skills of Bilingual Children with Hearing Loss Who Use Listening Devices Relative to Their Monolingual Peers. Lang. Speech Hear. Serv. Sch. 2013, 44, 281–290. [Google Scholar] [CrossRef]
- Bunta, F.; Douglas, M.; Dickson, H.; Cantu, A.; Wickesberg, J.; Gifford, R.H. Dual language versus English-only support for bilingual children with hearing loss who use cochlear implants and hearing aids. Int. J. Lang. Commun. Disord. 2016, 51, 460–472. [Google Scholar] [CrossRef] [PubMed]
- Bunta, F.; Goodin-Mayeda, C.E.; Procter, A.; Hernandez, A. Initial Stop Voicing in Bilingual Children with Cochlear Implants and Their Typically Developing Peers with Normal Hearing. J. Speech Lang. Hear. Res. 2016, 59, 686–698. [Google Scholar] [CrossRef]
- Sabri, M.; Fabiano-Smith, L. Phonological Development in a Bilingual Arabic–English-Speaking Child with Bilateral Cochlear Implants: A Longitudinal Case Study. Am. J. Speech-Lang. Pathol. 2018, 27, 1506–1522. [Google Scholar] [CrossRef] [PubMed]
- Sosa, A.V.; Bunta, F. Speech Production Accuracy and Variability in Monolingual and Bilingual Children with Cochlear Implants: A Comparison to Their Peers with Normal Hearing. J. Speech Lang. Hear. Res. 2019, 62, 2601–2616. [Google Scholar] [CrossRef] [PubMed]
- Teschendorf, M.; Janeschik, S.; Bagus, H.; Lang, S.; Arweiler-Harbeck, D. Speech Development after Cochlear Implantation in Children from Bilingual Homes. Otol. Neurotol. 2011, 32, 229–235. [Google Scholar] [CrossRef]
- Keilmann, A.; Friese, B.; Hoffmann, V. Receptive and productive speech and language abilities in hearing-impaired chil-dren with German as a second language. Int. J. Pediatr. Otorhinolaryngol. 2019, 120, 100–107. [Google Scholar] [CrossRef]
- Deriaz, M.; Pelizzone, M.; Pérez Fornos, A. Simultaneous development of 2 oral languages by child cochlear implant re-cipients. Otol. Neurotol. 2014, 35, 1541–1544. [Google Scholar] [CrossRef]
- Guiberson, M. Bilingual skills of deaf/hard of hearing children from Spain. Cochlear Implant. Int. 2013, 15, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Forli, F.; Giuntini, G.; Ciabotti, A.; Bruschini, L.; Löfkvist, U.; Berrettini, S. How does a bilingual environment affect the results in children with cochlear implants compared to monolingual-matched children? An Italian follow-up study. Int. J. Pediatr. Otorhinolaryngol. 2018, 105, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Woodson, E.W.; Masur, J.; Bent, J. Pediatric cochlear implantation: Role of language, income, and ethnicity. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Mahon, M.; Rajput, K.; Vickers, D.; Mahon, H. Expert opinion: Assessing cochlear implant candidacy and progress for people with English as an additional language. Cochlear Implant. Int. 2016, 17, 59–61. [Google Scholar] [CrossRef] [PubMed]
| NFC | NNFC | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Unilateral vs. Bilateral CI | Delay (mo) | Speech Processor | Implant | Etiology | Patient | Unilateral vs. Bilateral CI | Delay (mo) | Speech Processor | Implant | Etiology |
| 1 | B sim | CP 810 | N5 | Syndr | 12 | B seq | 31 | BTE | CI24RE | I | |
| 2 | U | BW | CI24RE | I | 13 | B seq | 28 | BW | CI24RE | CX26 | |
| 3 | B seq | 19 | BW | CI24RE | I | 14 | B sim | - | Freedom BTE | CI24RE | CX26 |
| 4 | U | BW | CI24RE | I | 15 | B sim | - | CP 810 | N5 | I | |
| 5 | U | BW | CI24RE | CHARGE | 16 | B sim | - | CP 810 | N5 | I | |
| 6 | B seq | 9 | BW | CI24RE | I | 17 | U | - | Freedom BW | CI24RE | Consanguineity |
| 7 | U | BTE | CI24RE | CX26 | 18 | B sim | - | Freedom BTE | CI24RE | I | |
| 8 | B seq | 38 | BW | CI24RE | I | 19 | B sim | - | Freedom BTE | CI24RE | Meningitis |
| 9 | U | BTE | CI24RE | Waanderburg | - | - | - | - | - | - | |
| 10 | B sim | CP 810 | N5 | I | - | - | - | - | - | - | |
| 11 | U | BW | CI24RE | CX26 | - | - | - | - | - | - | |
| Patient | Country of Origin | Country of Birth | Home Language | Parental Competence for Italian Language | Parental Level of Education |
|---|---|---|---|---|---|
| 12 | Albania | Albania | Albanian | F: Sufficient M: None | F: Primary M: Primary |
| 13 | Romania | Italy | Romanian | F: good M: Sufficient | F: Secondary M: Primary |
| 14 | Romania | Italy | Romanian | F: Sufficient M: Very limited | F: Primary M: Primary |
| 15 | Romania | Italy | Romanian | F: Sufficient M: Sufficient | F: Primary M: Primary |
| 16 | Romania | Italy | Romanian | F: good M: Sufficient | F: Secondary M: Primary |
| 17 | Pakistan | Italy | Urdu | F: Very limited M: None | F: None M: None |
| 18 | Romania | Italy | Romanian | F: Sufficient M: Sufficient | F: Primary M: Secondary |
| 19 | Morocco | Morocco | Arabic | F: Poor M: None | F: Primary M: None |
| Analyzed Ages | NFC | NNFC | P |
|---|---|---|---|
| Age at CI (mo) | 48 (38–59) | 57 (38–80.5) | 0.5 |
| Age at diagnosis (mo) | 6 (3.5–17.5) | 18.5 (8–34.5) | 0.1 |
| Hearing age (mo) | 28 (22–35) | 26 (22–43) | 0.9 |
| Verbal age (mo) | 35 (30.5–46.5) | 36 (26.5–52) | 0.9 |
| Questionnaire | NFC | NNFC | P |
|---|---|---|---|
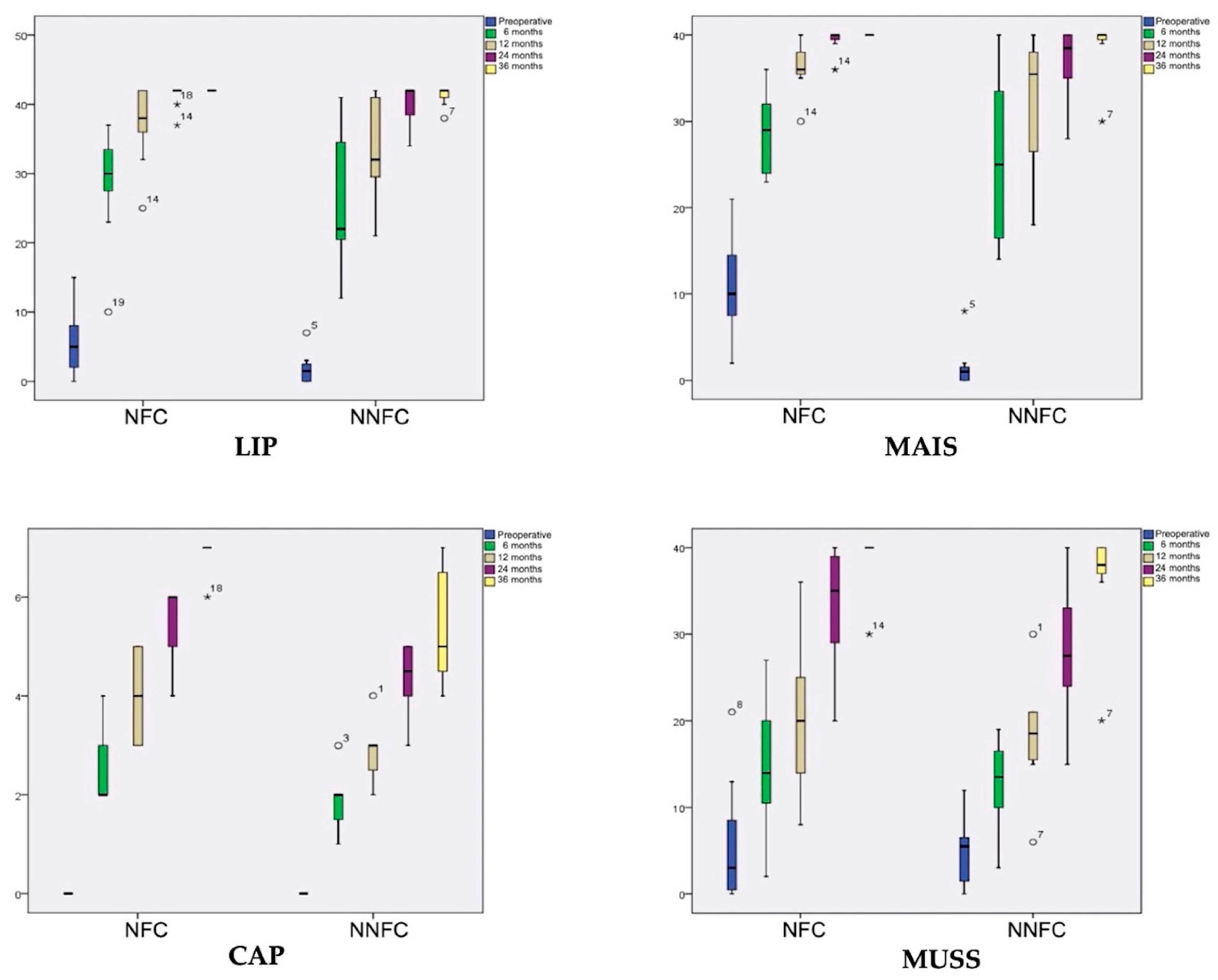
| LIP (preoperative) | 5 (2–8) | 1.5 (0–2.5) | 0.051 |
| LIP (6 mo) | 30 (27.5–33.5) | 22 (20.5–34.5) | 0.4 |
| LIP (12 mo) | 38 (36–42) | 32 (29.5–41) | 0.1 |
| LIP (24 mo) | 42 (42–42) | 42 (38.5–42) | 0.4 |
| LIP (36 mo) | 42 (42–42) | 42 (41–42) | 0.4 |
| MAIS (preoperative) | 10 (7.5–14.5) | 1 (0–1.5) | 0.001 |
| MAIS (6 mo) | 29 (24–32) | 25 (16.5–33.5) | 0.6 |
| MAIS (12 mo) | 36 (35.5–38) | 35.5 (26.5–38) | 0.4 |
| MAIS (24 mo) | 40 (39.5–40) | 38.5 (35–40) | 0.1 |
| MAIS (36 mo) | 40 (40–40) | 40 (39.5–40) | 0.4 |
| CAP (preoperative) | 0 | 0 | 1 |
| CAP (6 mo) | 2 (2–3) | 2 (1.5–2) | 0.09 |
| CAP (12 mo) | 4 (3–5) | 3 (2.5–3) | 0.02 |
| CAP (24 mo) | 6 (5–6) | 4.50 (4–5) | 0.009 |
| CAP (36 mo) | 7 (7–7) | 5 (4.5–6.5) | 0.007 |
| MUSS (preoperative) | 3 (0.5–8.5) | 5.5 (1.5–6.5) | 0.6 |
| MUSS (6 mo) | 14 (10.5–20) | 13.5 (10–16.5) | 0.7 |
| MUSS (12 mo) | 20 (14–25) | 18.5 (15.5–21) | 0.8 |
| MUSS (24 mo) | 35 (29–39) | 27.5 (24–33) | 0.1 |
| MUSS (36 mo) | 40 (40–40) | 38 (37–40) | 0.08 |
| Questionnaire | NFC | NNFC | |
|---|---|---|---|
| P | P | ||
| LIP (6 mo) | LIP (preoperative) | 0.005 | 0.012 |
| LIP (12 mo) | LIP (6 mo) | 0.003 | 0.012 |
| LIP (24 mo) | LIP (12 mo) | 0.02 | 0.02 |
| LIP (36 mo) | LIP (24 mo) | 0.2 | 0.1 |
| MAIS (6 mo) | MAIS (preoperative) | 0.003 | 0.012 |
| MAIS (12 mo) | MAIS (6 mo) | 0.003 | 0.02 |
| MAIS (24 mo) | MAIS (12 mo) | 0.005 | 0.02 |
| MAIS (36 mo) | MAIS (24 mo) | 0.1 | 0.04 |
| CAP (6 mo) | CAP (preoperative) | 0.003 | 0.01 |
| CAP (12 mo) | CAP (6 mo) | 0.002 | 0.02 |
| CAP (24 mo) | CAP (12 mo) | 0.003 | 0.01 |
| CAP (36 mo) | CAP (24 mo) | 0.002 | 0.04 |
| MUSS (6 mo) | MUSS (preoperative) | 0.003 | 0.012 |
| MUSS (12 mo) | MUSS (6 mo) | 0.003 | 0.011 |
| MUSS (24 mo) | MUSS (12 mo) | 0.003 | 0.011 |
| MUSS (36 mo) | MUSS (24 mo) | 0.012 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nassif, N.; Barezzani, M.G.; Redaelli de Zinis, L.O. Delayed Speech Perception and Production after Cochlear Implantation in Bilingual Children from Non-Native Families. J. Otorhinolaryngol. Hear. Balance Med. 2021, 2, 4. https://doi.org/10.3390/ohbm2010004
Nassif N, Barezzani MG, Redaelli de Zinis LO. Delayed Speech Perception and Production after Cochlear Implantation in Bilingual Children from Non-Native Families. Journal of Otorhinolaryngology, Hearing and Balance Medicine. 2021; 2(1):4. https://doi.org/10.3390/ohbm2010004
Chicago/Turabian StyleNassif, Nader, Maria Grazia Barezzani, and Luca Oscar Redaelli de Zinis. 2021. "Delayed Speech Perception and Production after Cochlear Implantation in Bilingual Children from Non-Native Families" Journal of Otorhinolaryngology, Hearing and Balance Medicine 2, no. 1: 4. https://doi.org/10.3390/ohbm2010004
APA StyleNassif, N., Barezzani, M. G., & Redaelli de Zinis, L. O. (2021). Delayed Speech Perception and Production after Cochlear Implantation in Bilingual Children from Non-Native Families. Journal of Otorhinolaryngology, Hearing and Balance Medicine, 2(1), 4. https://doi.org/10.3390/ohbm2010004





