Abstract
Introduction: Hypertension is an important public health concern because of its associated morbidity, mortality and economic impact on society. It is a significant risk factor for cardiovascular, cerebrovascular and renal complications. A number of national and international guidelines for the management of hypertension have been published. The Joint National Committee (JNC) in 2003 published a series of guidelines to recommend the appropriate antihypertensive therapy based on the best available evidence. Objectives: This drug utilization study was intended to find out the preferred drug group prescribed either alone or in combinations and their adherence to the JNC 7 guidelines. Materials and Methods: This was a prospective cross-sectional study. Drug utilization data on 100 hypertensive patients were collected from various hospitals in Nepal. The patients who received antihypertensive drugs during their treatment period in SPSS V. 16.0. The prescribed drugs were compared with JNC 7 guidelines. Results: It was found that 40% of patients were male and 60% were female. The largest subset of female hypertensive patients (45.0%) were in the age group of >60 years and a plurality of male hypertensive patients (45.0%) were in the age group of 40–60 years. It was found that 45% of the patients had Stage 1 hypertension, 32% of the patients were in prehypertension, 17% of the patients had Stage 2 hypertension. The most frequently prescribed antihypertensive drug regimens were angiotensin receptor blockers (ARBs) (32.44%), ARB + thiazide (15.94%), diuretics (11.59%), calcium channel blockers (CCBs) + beta blockers (9.42%) and CCBs (8.7%). Thirty-nine percent received monotherapy while the remaining 61% received combination therapy. Seventy-four percent of the total prescriptions followed JNC 7 guidelines. Conclusion: There is a need to follow official guidelines in managing hypertension as a chronic disease, since these guidelines are based on various clinical trials, and the successful attainment of a target BP in patients will be made much easier by implementing them. National health policymakers should consider the evaluation and treatment of hypertension as a right in the public health system for better outcomes in terms of morbidity and mortality from hypertension.
1. Introduction
Hypertension (HTN) is the most common cardiovascular disorder and is regarded as major public health problem []. HTN is not a cause of death by itself, but it is an important risk factor for cardiovascular mortality and morbidity. HTN remains one of the most important preventable contributors []. HTN is the single most important cause of preventable mortality. It is a key contributing factor in the development of cardiovascular and cerebrovascular disease, and a major cause of stroke, myocardial infarction, heart failure and kidney disease, among others. It leads to death if not detected early and treated appropriately.
Antihypertensive drug therapy has improved remarkably in the last 56 years. The first antihypertensive agent which was developed in 1958 was chlorothiazide, the first thiazide diuretic used in treatment of HTN, which was developed from the antibiotic sulfanilamide. After the grand success of chlorothiazide in the treatment of HTN, soon more agents were developed, such as beta blockers, calcium channel blockers, angiotensin-converting enzymes, angiotensin receptor blockers and renin inhibitors [,]. Due to the increase in the number of drugs for the treatment of HTN, different complications and problems have been arising.
To counteract the problem, 39 major professional, public and voluntary organizations and seven federal agencies formed a committee known as the Joint National Committee (JNC) [].
The Key Messages of the JNC 7 Report
In persons older than 50 years, systolic blood pressure (BP) greater than 140 mmHg is a greater risk factor for HTN. Cardiovascular disease (CVD) risk doubles for each increment of 20/10 mmHg. Those who are normotensive at 55 years of age have a 90% lifetime risk of developing hypertension. Prehypertension, defined as a systolic BP of 120–139 mmHg or a diastolic BP of 80–89 mmHg, requires lifestyle modifications to prevent the progressive rise in blood pressure and CVD. Hypertension will be controlled only if patients are motivated to stay on their treatment plan. According to JNC 7 guidelines, the measured blood pressure is classified by the below blood pressure classification [].
In JNC7 guideline blood pressure is classified and simplified to four categories, which are given below (Table 1).

Table 1.
Contemporary blood pressure classification guidelines. DBP: diastolic blood pressure; SBP: systolic blood pressure.
2. Methodology
2.1. Study Site
The study was carried out in Lalitpur Heart Clinic, Jawalakhel Nepal Heart Care Centre, Jhamsikhel and Kritipur Community Health Centre (Janapoly clinic), Kritipur and Grande International Hospital, Dhapasi.
2.2. Study Period
Data collection was carried out for 2 months over June–July 2014.
2.3. Study Design
This study was designed as a prospective cross-sectional analysis.
2.4. Study Population
The study included all willing patients who visited the cardiac care center or the hospital of Kathmandu Valley for the treatment of hypertension and who were positively diagnosed.
2.5. Inclusion Criteria
- The patients who visited in the center and diagnosed with hypertension and taking antihypertensive medicines.
- Hypertensive patients who agreed to share their information and responded to the questionnaire.
2.6. Exclusion Criteria
- The patients who visited the center and who were not diagnosed with hypertension.
2.7. Sample Size
The study included a total of 100 patients from four treatment centers: 26 from the Lalitpur Heart Clinic, 23 from the Nepal Heart Care Centre, 37 from the Janapoly clinic and 14 from the Grande International Hospital.
2.8. Data Collection Tools and Techniques
Data collection forms were filled from all the patients who gave consent for research. The required information was obtained from the medical records of the patients, such as their names, ages, genders, addresses, blood pressures, weights, prescriber names, prescriber offices, the antihypertensive drugs used, any associated diseases and medications for those associated diseases.
2.9. Statistical Tools
All the data collected from different centers were coded as per variables and data entry was done in SPSS V 16.0 data sheet and analyzed by the help of statistical software SPSS V 16.0. The analyzed data was expressed in percentage.
3. Results
Our data shows that 40 patients (40%) involved were males and 60 (60%) were females, indicating a 20% higher prevalence of hypertension in the female population.
From Figure 1 it can be seen that the plurality of female hypertension patients (45.0%) were in the age group of >60 years and the plurality of male hypertension patients (45.0%) were in the age group of 40–60 years, indicating an earlier onset of hypertension in male population in our study group. The proportions of female and male hypertension patients in the age group of <40 years were 11.7% and 17.5% respectively, which was the smallest age group.
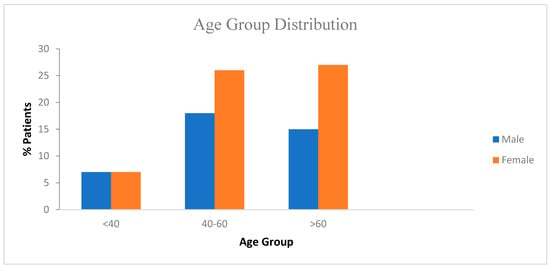
Figure 1.
Age distribution of patients.
Table 2 shows that the prevalence of Stage 1 hypertension over other stages of hypertension was higher. Among 100 patients 45% of the patients had Stage 1 hypertension, 32% of the patients had prehypertension, 17% of the patients had Stage 2 hypertension and the proportion in the normal stage was found to be 6%.

Table 2.
Stages of hypertension.
In Figure 2 it can be seen that 38% and 7% of male and female patients, respectively, were found to have diabetes mellitus. A high risk of coronary heart disease was found in 13% of female patients and in 18% of male patients. Similarly, asthma was found in 5% of male patients and in 9% of female patients. Diabetes mellitus comorbid with a high risk of coronary heart disease was found at an incidence of 4% in both male and female patients and diabetes mellitus together with chronic kidney disease was found in 2% of female patients.
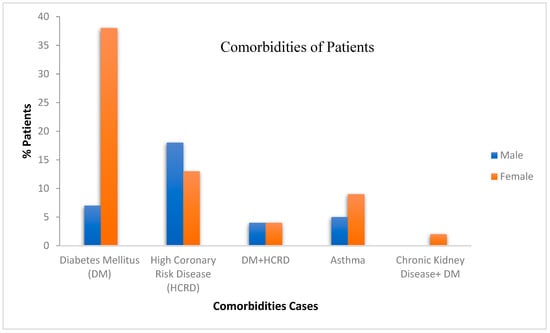
Figure 2.
Comorbidities of the patients.
Table 3 shows that angiotensin receptor blockers alone was the most commonly prescribed regimen of antihypertensive drugs in 30.44% patients, followed by angiotensin receptor blockers (ARBs) + thiazide in 15.95%, calcium channel blockers (CCBs) alone in 12.32%, CCBs + beta blockers in 9.42%, beta blockers in 8.7%, thiazide diuretics and angiotensin-converting enzyme (ACE) inhibitors in 6.52% respectively, ARB + CCB in 3.62%, diuretic combinations in 1.45%, and alpha blockers and beta blockers + thiazide in 0.72% patients, respectively.

Table 3.
Percentage of patients administered each antihypertensive drug regimen.
Table 4 shows that ARBs were the most commonly prescribed group of antihypertensive drugs in 42.84% of non-hypertensive patients by physicians’ orders, followed by CCBs, beta blockers, diuretic combinations and ARB + thiazide group, each used in 14.29% of patients with normal blood pressure.

Table 4.
Percentage of normotensive patients prescribed each drug regimen.
Table 5 shows that angiotensin receptor blockers were the most commonly prescribed group of antihypertensive drugs in 28.21% of prehypertensive patients, followed by calcium channel blockers in 20.51%, thiazide diuretics and ACE inhibitors each in 15.39%, ARBs + thiazide in 7.69%, beta blockers in 5.13% and others in 2.56% .

Table 5.
Percentage of prehypertensive patients prescribed each drug regimen.
Table 6 shows that angiotensin receptor blockers were the most commonly prescribed group of antihypertensive drugs in 28.12% of Stage 1 patients, followed by ARB + thiazide and CCB + beta blocker each in 18.75%, beta blockers alone in 10.94% and calcium channel blockers alone in 7.81%. It was found that only 3.13% patients were prescribed thiazide only

Table 6.
Percentage of Stage 1 patients prescribed each drug regimen.
The largest proportions of Stage 1 patients prescribed a single drug were those taking ARBs at 28.12% and those taking beta blockers at 10.94%, which are smaller than the corresponding proportions reported in studies conducted in Bangalore for monotherapy with ARBs (62%) and beta blockers (15%).
Table 7 shows that angiotensin receptor blockers were the most commonly prescribed group of antihypertensive drugs, used in 40.0% of Stage 2 patients, followed by ARB + thiazide at 24.0%, calcium channel blockers at 12.0%, beta blockers and ARB + CCB each at 8.0% and thiazide diuretics and high-ceiling diuretics each in 4% patients respectively in Stage 2 hypertension.

Table 7.
Percentage of Stage 2 patients prescribed each drug regimen.
Figure 3 shows that hypertensive patients with diabetes mellitus as an associated disease were the largest group with a comorbidity, so hypoglycemic drugs were prescribed for 51 patients, similarly hypolipidemic drugs were used in 28 patients to treat high coronary risk disease, anti-asthmatic drugs were used in 15 patients for the treatment of asthma, and antiplatelets and anti-depressant drugs were prescribed to 5 and 1 patients respectively.
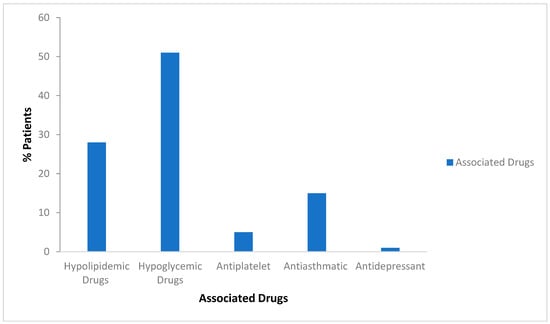
Figure 3.
Associated drugs in used in hypertension patients.
The proportions of patients prescribed one, two, three or more drugs are shown in Table 8. It can be seen that 39.0% patients received monotherapy and 61.0% received combination therapy. Among all patients, 48.0% took two drugs, 12.0% took three drugs and 1.0% took four or more drugs.

Table 8.
Proportion of patients prescribed each number of drugs.
All the prescription information collected from different Heart care Centers of the Kathmandu Valley were analyzed according to JNC 7 guidelines. Figure 4 shows that Lalitpur Heart Clinic, Nepal heart Care Center, Grande International Hospital and Janapoly clinic’s prescriptions followed JNC 7 guidelines by 92.3%, 86.95%, 71.42% and 54.05%, respectively, whereas a greater percentage of prescriptions which did not comply with JNC 7 guidelines were found in the Janapoly clinic (i.e., 45.95%), with the numbers for Grande International Hospital, Nepal Heart Care Center and Lalitpur Heart Clinic being 28.58%, 13.05% and 7.7% respectively.
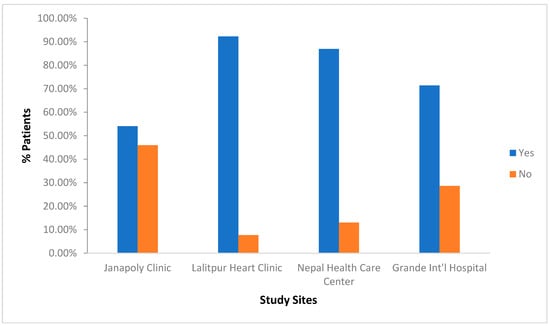
Figure 4.
Compliance with JNC 7 Guidelines.
Cost analysis indicated that most patients were charged below 1500 rupees per month for the treatment of hypertension with associated drugs, and only the four-case numbers 60, 63, 40, and 1 paid more than this. It was found that 25% of patients paid less than 500 rupees per month for their treatment, 50% patients were charged below 1000 rupees per month, and the remaining 25% of the patients were charged below 1500 rupees per month. The patients without comorbidities were charged below rupees 600 per month in only one case (i.e., case number 27).
The patients were divided into different categories according to their blood pressure, and the cost of the total drugs which they used during their treatment was analyzed on a monthly basis. Our data in Figure 5 show that the 4% of normal stage patients paid less than 500 rupees, and 2% were charged 501–1000 rupees per month for their treatment. In the prehypertensive stage, 22% patients were charged below Rs 500 and 10% were charged Rs 501–1000 per month for their treatment. In both Stage 1 and Stage 2 hypertension, most patients paid less than 500 rupees, and there was a similar proportion of patients who were charged between 1001 and 1500 rupees and more than 1501 rupees.
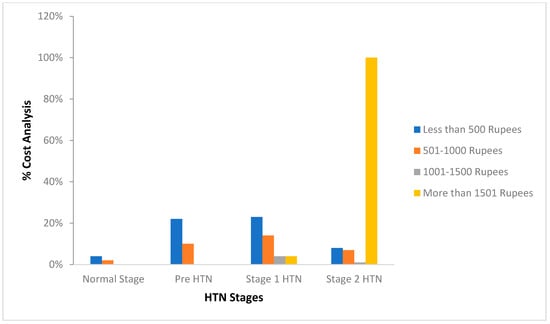
Figure 5.
Stage-wise total cost analysis of the drugs. HTN: hypertension.
4. Discussion
The main aim of antihypertensive therapy is to prevent hypertension-related morbidity, mortality and complications []. As antihypertensive prescription is required for the entire life, the side effects, quality of life and cost of drugs are also important aspects. Keeping all factors in mind, various prescribing guidelines have been formulated. Treatment guidelines can be monitored by several methods. Drug utilization studies are one such method [].
Our study group showed a higher prevalence of hypertension in elderly patients (i.e., >40 years). However, most females showed an earlier onset of hypertension than males (i.e., 20% greater than in males).
Data also revealed that there was a greater proportion of female patients than male patients who had hypertension along with diabetes mellitus and HTN with asthma, but the percentage of male patients with high-risk coronary disease was higher than in female patients. In hypertension along with its comorbidities, the most frequently prescribed group of drugs are ARBs. The associated drugs which were mostly prescribed in comorbidities were hypoglycemic drugs because the number of patients with DM was greater. Similarly, hypolipidemic drugs, anti-asthmatic drugs, antiplatelet and anti-depressant drugs were also prescribed to patients [].
Hypertension is placed into different categories as given by the JNC 7 guidelines, and our data analysis results showed that patients with Stage 1 hypertension were observed in greater number (45%), followed by prehypertension (32%), Stage 2 hypertension (17%), and normotension (6%) [].
This study also found that JNC 7 guidelines were followed in 74% of the study group. In all stages of hypertension, the most frequently prescribed group of drugs were ARBs, in prehypertension ARBs were followed by CCBs, thiazide, ACE inhibitors and beta blockers. In Stage 1 hypertension, ARBs were followed by ARB + thiazide and CCB + beta blocker. ARBs were also highly prescribed in Stage 2, which was followed ARB + thiazide, CCB, and beta blocker. More than half (i.e., 61%) of the total patients in this study received two or more antihypertensive drugs [,,].
After analyzing all the prescriptions collected from different Heart care Centers of the Kathmandu Valley, we found most of the institutes followed the seventh report of the Joint National Committee. In general, our data showed that 74% of the prescriptions followed the JNC guidelines [,].
Cost analysis showed that 57% of patients were charged below 500 rupees per month for their treatment. About 33% of total patients were charged between 501 and 1000 rupees per month, and 5% of patients were charged from 1001 to 1500 and more than 1500 rupees per month [].
5. Conclusions
Based on our analysis of 100 prescriptions, the results of the current study were partly in accordance with the JNC 7 guidelines. Hence, larger extended studies are required to draw noticeable inferences.
References
- World Health Organization. Report of WHO Consultation on Xenotransplantation: Geneva, Switzerland, 28-30 October 1997; World Health Organization, Emerging and Other Communicable Diseases and Control: Geneva, Switzerland, 1998. [Google Scholar]
- James, P.A.; Oparil, S.; Carter, B.L.; Cushman, W.C.; Dennison-Himmelfarb, C.; Handler, J.; Smith, S.C. 2014 Evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014, 311, 507–520. [Google Scholar] [CrossRef] [PubMed]
- Novello, F.C.; Sprague, J.M. Benzothiadiazine dioxides as novel diuretics. J. Am. Chem. Soc. 1957, 79, 2028–2029. [Google Scholar] [CrossRef]
- Dustan, H.P.; Roccella, E.J.; Garrison, H.H. Controlling hypertension: a research success story. Arch. Intern. Med. 1996, 156, 1926–1935. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V.; Bakris, G.L.; Black, H.R.; Cushman, W.C.; Green, L.A.; Izzo, J.L., Jr.; Roccella, E.J. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003, 289, 2560–2571. [Google Scholar] [CrossRef] [PubMed]
- Mancia, G.; Laurent, S.; Agabiti-Rosei, E.; Ambrosioni, E.; Burnier, M.; Caulfield, M.J.; Erdine, S. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. Blood Press. 2009, 18, 308–347. [Google Scholar] [CrossRef] [PubMed]
- Rathnakar, U.P.; Shenoy, A.; Ullal, S.D.; Sudhakar, P.; Shastry, R.; Shoeb, A. Prescribing patterns of fixed dose combinations in hypertension, diabetes mellitus and dyslipedimia among patients attending a cardiology clinic in a tertiary care teaching hospital in india. Int. J. Compr. Pharm. 2011, 2, 1–3. [Google Scholar]
- Remesh, A.; Salim, S.; Gayathri, A.M.; Nair, U.; Retnavally, K.G. Antibiotics prescribing pattern in the in-patient departments of a tertiary care hospital. Arch. Pharm. Pract. 2013, 4, 71. [Google Scholar] [CrossRef]
- Bajaj, J.K.; Sood, M.; Singh, S.J.; Jerath, P. Prescription Patterns Of Antihypertensive Drugs And Adherence To JNC ViiGuidelines In A Tertiary Care Hospital In North India. Int. J. Med. Clin. Res. 2012, 3, 118–120. [Google Scholar]
- Dhanaraj, E.; Raval, A.; Yadav, R.; Bhansali, A.; Tiwari, P. Prescription pattern of antihypertensive agents in T2DM patients visiting tertiary care centre in North India. Int. J. Hypertens. 2012, 2012, 520915. [Google Scholar] [CrossRef] [PubMed]
- Mohd, A.H.; Mateti, U.V.; Konuru, V.; Parmar, M.Y.; Kunduru, B.R. A study on prescribing patterns of antihypertensives in geriatric patients. Perspect. Clin. Res. 2012, 3, 139. [Google Scholar] [PubMed]
- Chataut, J.; Khanal, K.; Manandhar, K. Prevalence and Associated Factors of Hypertension among Adults in Rural Nepal: A Community Based Study. Kathmandu Univ. Med. J. (KUMJ), 2015, 13, 346–350. [Google Scholar] [PubMed]
- Vaidya, A.; Pathak, R.P.; Pandey, M.R. Prevalence of hypertension in Nepalese community triples in 25 years: a repeat cross-sectional study in rural Kathmandu. Indian Heart J. 2012, 64, 128–131. [Google Scholar] [CrossRef] [PubMed]
- Kalamdani, A.R.; Bhandare, B.; Hemamalini, M.B.; Krishna, M.V. A prospective study of prescribing pattern of antihypertensive drugs in tertiary care hospital, Bangalore. J. Evol. Med. Dent. Sci. 2014, 2, 10339–10344. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).