1. Introduction
Clinical depression is undoubtedly part of life experience. Life as we perceive it is a chronology of events/moments that are subject to interpretations. Interpretations generate mood states. The fact that at least the initial moment of a person’s life cannot be influenced, postponed, or cancelled suggests that life as a whole must be accepted [
1].
Furthermore, life in its entirety is a sequential and synchronous running of three programs: biological, psychological, and social. The finality of the biological program is the exhaustion of the genetic program; the finality of the psychological program seems to be the acceptance of one’s own life, while the finality of the social program is the exhaustion of the person’s life scenes [
2].
Clearly, each individual/patient experiences life uniquely. The variety of interpretations given to the same stimuli/life events/contexts can be explained by the fundamental intervals of time of individuals. These intervals are capable of describing, through multiplication, the entire life horizon of all basic anatomical units and larger anatomical structures. Likewise, these intervals determine the number of life frames accessible to the individual in one second [
2].
Personalized interpretations of life events suggest that, at its core, clinical depression in patients is a personalized pattern of biological, psychological, and social interaction impairments.
Major depressive disorder (MDD) is defined as a mental disorder [
3] or as a mood disorder [
4]. To be diagnosed with MDD, according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), an individual must have five of the following symptoms: persistently low or depressed mood, anhedonia, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, suicidal thoughts. One of the five symptoms must be depressed mood or anhedonia [
5].
The prevalence of depression in different age groups has reached alarming levels. A recent study shows that 34% of adolescents aged 10–19 years are at risk of developing clinical depression [
6]. Another meta-analysis involving 72,878 older adults demonstrated that 28.4% of them screened positive for depression [
7]. The association of MDD with morbidity and mortality makes these values even more worrying [
8].
The clearest and most visible effects of MDD, interpreted as associations, are dysfunctions and abnormalities at the level of the brain. Recent studies have shown that these abnormalities are due to the impairment of complex neuroregulatory systems and neuronal circuits [
5,
9,
10,
11,
12,
13]. Other studies highlight the connection between chemical imbalance in the brain and mood disorders [
14,
15].
How does MDD manifest at the mental level? An important characteristic of MDD is reduced emotional reactivity to sad contexts [
16]. Self-compassion is often used as an adaptive emotion regulation strategy, especially by patients with high levels of depressed mood [
17]. High levels of suppression of positive or negative emotions are associated with MDD symptoms [
18]. The posibility of emotional regulation in MDD medicated patients is preserved, depending on the severity of the symptoms [
19]. These conclusions do not exclude the specific manifestations of the experiences of patients affected by clinical depression [
1].
Cognitive impairment and dysfunction are major causes of the onset and manifestation of clinical depression [
20]. Cognitive dysfunction can be determined by altering certain biochemical/physiological processes. Changes recorded in the hypothalamic–pituitary–adrenal axis and decreased serotonin levels contribute to the development of cognitive decline [
21]. There are findings that justify the importance of studying cognitive impairment because it persists despite the remission of depressive symptoms [
22,
23]. What is specific in major depression is the presence of strong connections between symptoms resulting from cognitive impairment [
24]. A major cause of impaired thinking capacity determined by major depression is the persistence of negative self-information that is strongly interconnected in the cognitive system of patients [
25]. The complicated thinking of depressed patients is influenced by the persistence of implicative dilemmas that determine cognitive conflicts [
26]. Recovery from major depression is mediated by the increase in patients’ capacity to evaluate, observe, and regulate their own cognitive processes [
27].
Assessing major depression is undoubtedly a challenging task. Here, a distinction must be made between the clinical presentation of MDD and how the illness is experienced at the patient level. The clinical presentation of the illness includes symptoms observed in patients diagnosed with clinical depression. However, DSM-5 does not accurately describe the experience of these symptoms.
Each moment of life is experienced from a biological, psychological, and social perspective. The sequential unfolding of life events elicits response reactions. These reactions are determined by fundamental life concepts through which individuals understand and interpret reality. The reactions induce experiences. Therefore, an essential presence in life is defined by the relationship between life themes and experiences. In the case of a life affected by clinical depression, studying the relationship between life themes and symptoms can offer a better understanding of the illness pattern and solutions for psychotherapeutic intervention.
The treatment of major depression involves both medication and psychotherapy. Although medication treatment usually leads to the improvement of certain physical symptoms of depression, a range of other psychological and emotional aspects such as those related to cognition and mental states may not improve adequately. In complex cases, with multiple relapses, the persistence and consistency of dysfunctional life themes are aggravating factors for the illness. Discussing certain life themes during the patient’s psychotherapy sessions to facilitate the reinterpretation of their dysfunctional life themes can lead to some symptomatic improvements. In complex cases, this approach can improve some symptoms and amplify other symptoms. An alternative solution would be to shift the patient’s focus towards other life themes with the potential to alleviate the problematic symptoms.
The research we propose is focused on identifying those categories of symptoms, both observable and less observable, that manifest at a mental level and deeply affect the quality of life of depressive patients. We consider that these categories of symptoms are major sources of relapse and exacerbation of the illness over time.
The unique manner in which the illness is experienced by the patient suggests that emphasis should be placed on the patient’s illness pattern rather than on identifying generic features of the illness that aid in diagnosis.
The observable symptoms of the depressive patient are actually the most relevant symptoms. In reality, the patient experiences a combination of symptoms, which, in our opinion, is a new symptom called the latent symptom (LS). The register of latent symptoms is often complemented by a distinct category of symptoms that intensify patients’ stress and anxiety, and also by symptoms that are experienced undistortedly. We refer to these three categories of symptoms as problematic symptoms (PSs). What we aim to demonstrate is that identifying and treating problematic symptoms is essential to understand and improve the illness.
In this regard, we designed a computing system that processes the natural language of patients to provide a personalised description of the illness pattern and suggest psychotherapeutic solutions. Natural language processing is performed through specific techniques of latent semantic analysis (LSA) [
28,
29].
To achieve a comprehensive description of the computing system, we structured this work as follows:
Section 1—Introduction;
Section 2—Related Topics, Works and Concerns;
Section 3—Presentation of the Computing System for Assessing the Relationship between Life Themes and Symptoms in Patients Diagnosed with Major Recurrent Depression;
Section 4—Testing and Validation of the Computing System;
Section 5—Discussion;
Section 6—Conclusions.
The established abbreviations are used in the text of the paper, while any remaining abbreviations are employed within tables or in the interpretation of the results derived from these tables.
2. Related Topics, Works, and Concerns
In a broader context, our work could be integrated into the field of artificial intelligence applied in psychiatry, clinical psychology, and psychotherapy.
Undoubtedly, the specialized literature addressing depression from the perspective of artificial intelligence is vast. Remarkable progress has been made in creating products that incorporate the experience of diagnosing depression. The emphasis is on machine learning of both symptoms and associated behaviours. However, training machine learning models with symptoms and associated behaviours is difficult. Undoubtedly, one cause could be linked to the descriptions of the illness in diagnostic manuals. With a view to extracting complex symptoms and behaviors, significant progress has been made in identifying effective solutions for unsupervised machine learning [
30,
31]. At the same time, it is crucial not to overlook the fact that each individual possesses unique biological building capabilities that determine distinct behaviors, including those related to depression.
Despite the advancements, there are opinions underscoring the limitations of artificial intelligence products [
32]. One such limitation pertains to the analysis of mood, which is essential in detecting early signs of depression and suicidal tendencies [
33]. Another major limitation is the lack of definitive medical tests for depression [
34].
The applications of LSA in clinical psychology and psychotherapy are consistent, where the focus is on identifying hidden variables that sustain cognitive impairments and dysfunctions. In our view, achievements of LSA aimed at intervention in major depression could be synthesized as follows: improving algorithms for latent semantic analysis in major depression [
35,
36,
37,
38,
39]; the role of semantic interpretations in major depression [
40,
41,
42,
43,
44,
45]; subtle computing in major depression [
46,
47,
48]; the use of latent semantic analysis in major depression [
49,
50,
51,
52,
53].
3. Presentation of the Computing System for Assessing the Relationship between Life Themes and Symptoms in Patients Diagnosed with Major Recurrent Depression
Since the computing system is focused on the patient and on the symptoms for each life theme of the patient, we opted for a strictly matrix-based approach to the relationship between life themes and symptoms.
The construction of the computing system is part of an exploratory research endeavor aimed at evaluating the ability of LSA to accurately capture the patient’s illness pattern and provide effective suggestions for psychotherapy sessions. The overall objective of the computing system is to provide the necessary information for an efficient intervention aimed to improve the patient’s illness. To achieve this goal, we set the following specific objectives: to extract the LIFE THEMES-SYMPTOMS matrix for each patient; to describe the illness pattern of the patient by identifying dysfunctional life themes (Tis), irrelevant life themes (ILTs), latent life themes (LLTs), the most relevant symptoms (MRSs) in relation to life themes, and problematic symptoms; to provide the most suitable life themes as discussion topics for the patient’s psychotherapy sessions.
To achieve these objectives, the computing system uses the representation of life themes through symptom vectors, LSA, and the correlation method. The choice of these methods is justified by their ability to extract what is less visible, but with potential to worsen the illness. Specifically, these hidden aspects are represented by latent life themes, latent symptoms, nonspecific symptoms, and irrelevant life themes.
A latent life theme defines a composite theme resulting from the statistically significant association of life themes. This theme determines, with a certain probability, the symultaneously experiencing of the associated life themes. Each life theme is experienced through a latent symptom. Latent life theme can determine the amplification of some components of latent symptoms associated or the amplification of a latent symptom.
On the other hand, the statistically significant association of symptoms also generates a latent symptom. Therefore, latent symptoms are generated by life themes or by associations between symptoms.
Extraction of latent symptoms is facilitated by using matrix dimensionality reduction [
54], often used by LSA [
55,
56,
57,
58].
In the case of our work, matrix dimensionality reduction transforms a space of higher dimensions into a space of lower dimensions, represented by the most specific (relevant) symptoms. Thus, similarities between life themes are interpreted in the new coordinates given by these symptoms, which allow the identification of hidden correlations. Additionally, LSA enables the identification of hidden semantic relationships between life themes/symptoms, which are more challenging to observe in the original space of higher dimensions. This way, LSA provides a more compact semantic representation of the data.
In a certain sense, cosine similarity can be interpreted as a correlation measure. However, what is specific to patients with severe forms of depression and multiple relapses is the strength of the associations between life themes/symptoms, especially in the case of those that present a potential threat to the integrity of the psychological system. Often, the strength of the associations between life themes/symptoms persists over time. Therefore, identifying and addressing them is essential. We used Spearman correlation applied to column vectors of an approximated matrix to capture and measure the strength and statistical significance of associations. This approximated matrix is obtained by reducing the dimensionality of the original matrix.
Representation of life themes through symptom vectors allows the identification of symptomatic noises. We define a symptomatic noise as a symptom that is present in all life themes. Thus, symptomatic noise is a nonspecific symptom. In the case of a patient diagnosed with severe depression, the presence of symptomatic noises can dramatically amplify anxiety, the burden of managing latent symptoms, and specific symptoms.
We define life themes represented exclusively by symptomatic noises as irrelevant life themes. Irrelevant life themes are major vulnerability factors for the patient, as they are impossible to manage despite being dysfunctional life themes. Since irrelevant life themes cannot be distinguished from other life themes, they must be eliminated from LSA.
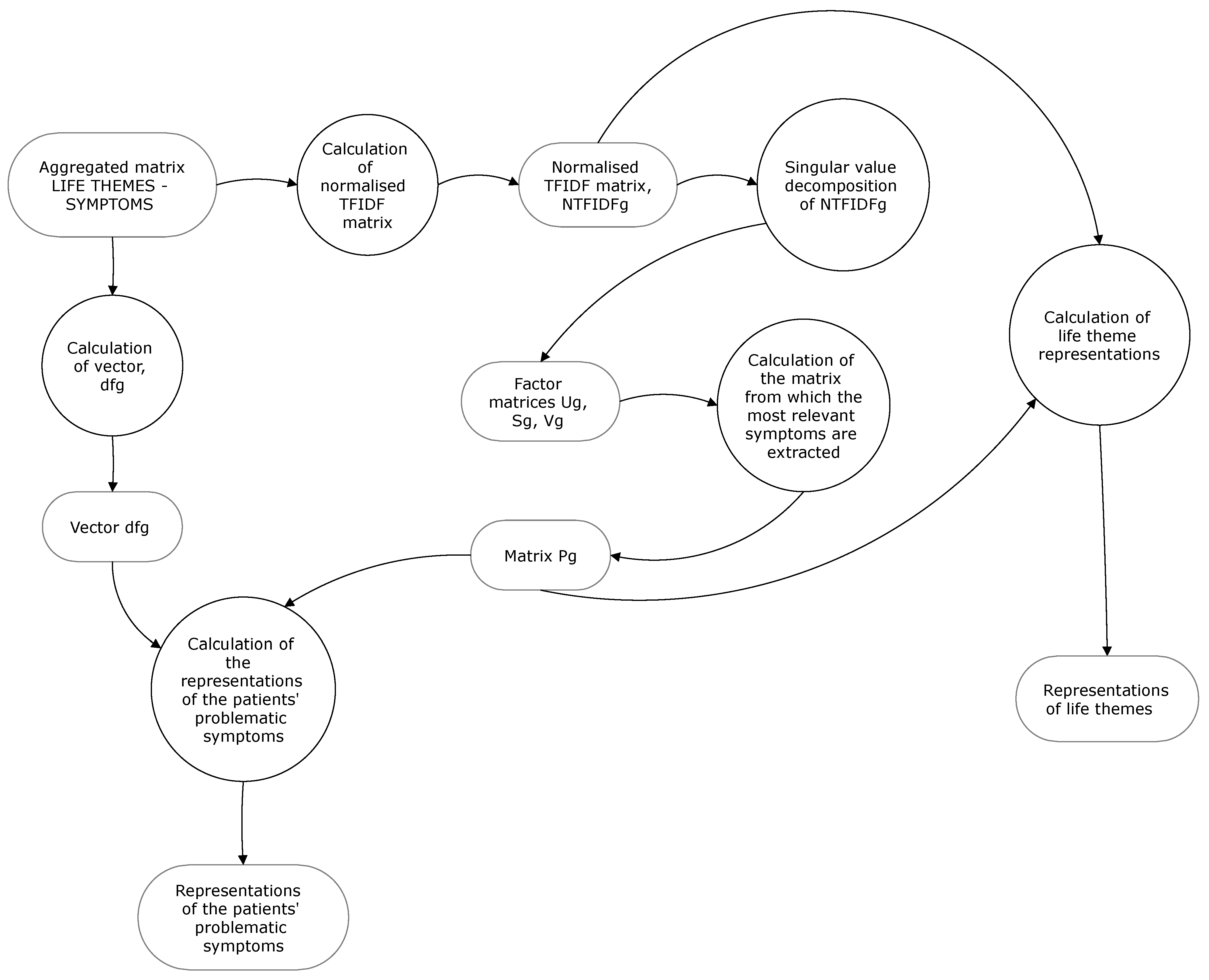
The block diagram of the computing system is described in
Figure 1.
The life themes of the patient diagnosed with major recurrent depression are dysfunctional ones associated with problematic symptoms. Redirecting the patient’s attention to other life themes involves identifying them from a more extensive source of themes. We identified this source within the patient group. This is the reason for the presence of the module for aggregating the patients’ matrices into a matrix of the group of patients.
Illness patterns and solutions for alleviating problematic symptoms, as outputs of the computing system, result exclusively from the processing of patients’ natural language. The natural language, as input to the computing system, is not subjected to manipulation or control to generate specific types of outputs. The system’s inputs and outputs are not treated as variables. Essentially, the entire research is based on the collection and processing of patients’ natural language using LSA techniques.
All modules are defined through data flow diagrams, except for the Processing Module of the Narrative, for which we provided a procedural presentation. Each diagram is described by processes, external entities, and arrows. The specific calculations for each process are performed in MATLAB R2024a.
3.1. Modules of the Computing System
3.1.1. Processing Module of the Narrative
The purpose of this module is to transform the patient’s narrative into a matrix in which the columns (life themes) are represented by the vectors of symptoms (see the first specific objective). Practically, through this matrix model, the patient’s experiences (symptoms) are linked to their dysfunctional sources (life themes).
Correct identification of life themes and symptoms is crucial for understanding the depression pattern at patient level. Their extraction must result from accurately interpretating text corpora by treating physicians/psychologists.
The thematic method [
59] is used by this module to extract life themes. It is useful to employ the content analysis method to identify the symptomatic content of each life theme [
1,
60].
We now present the procedure used in this module. Each patient investigated is asked to present concisely, within a maximum of one page, the happiest, the unhappiest and also some daily events. What is the premise of this request? [
1].
The absence of future perspective experienced in major depression (MD) engages the patient in a costly strategy of comparing an unfavorable present with a past unaffected by this absence. The reason behind such a strategy may lie in the need to sustain a state of seeking answers that justify and enable the acceptance of the traumatic event. In our opinion, the mood of patients is maintained by comparing the unhappiness and happiness themes, as well as by the presence of a daily theme encompassing activities, concerns, and so on necessary for managing the current psychological state [
1].
The happiest events are grouped into the theme of happiness, the unhappiest events into the theme of unhappiness, and the daily events into the theme of everyday life [
1]. Each of the three themes has to be divided into life subthemes [
1]. Each life subtheme is a life theme (Ti). The life subthemes need to be validated by a group of experts.
Each life subtheme is divided into groups of meaningful words. Each group is described based on the symptom that the patient experiences at the time of the request. For this purpose, each patient is asked to select one of the following symptoms (Sis): anxiety, apathy, zest for life, fury, tranquility, regret, gratitude, low self-esteem, high self-esteem, fatigue, euphoria, sadness, happiness, and other symptoms [
1]. The selection of this list was performed in accordance with the content of the three themes, which include positive/negative mental states.
All these symptoms are explained to the patients beforehand. To ensure that the patient accurately chooses Si, we ask them to justify their choice [
1]. Additionally, patients need to be aware that selecting the option other symptoms involves specifying and justifying them. By providing the option other symptoms, we make sure that the patients can mention symptoms that are not included in the list.
The unique symptoms gathered from all the life themes of the patients investigated are coded. The symptom code indicates the position of the symptom in the life theme vectors. All the life themes are represented by column vectors of the same size, containing the associated values of the presence of all the symptoms. These associated values contain the summed values of the occurrence of each symptom in the life theme.
At the level of each patient, the matrix LIFE THEMES-SYMPTOMS contains all the column vectors of the life themes identified.
Algorithm 1 for generating the LIFE THEMES-SYMPTOMS matrix at the patient level is presented below.
| Algorithm 1 Pseudocode for generating the LIFE THEMES-SYMPTOMS matrix |
| Input: |
| 1: Vectors of symptom occurrences for each life theme in patient i |
| Output: The matrix LIFE THEMES-SYMPTOMS in patient i, Ai |
| 2: procedure for Ai construction |
| 3: Initialize the matrix Ai |
| 4: for each life theme vector do |
| 5: for each symptom do |
| 6: Sum up the occurrences of each symptom |
| 7: end for | |
| 8: Write the transposed vector of the life theme in Ai |
| 9: end for |
| 10: return Ai |
| 11: end procedure |
Example 1. Life themes T1, T3, T20, T2, and T6 are identified in patient i. Each theme corresponds to a vector of symptom occurrences. These vectors are [3,3,3,4], [1,2,7,7,7], [4,3,3,1], [1,1,1,1,3,3,2,2,2,2,7,6,7,8], [1,3,3,2,4,4,4,4,4,4]. The components of the vectors are represented by symptom labels. For example, 4 is symptom number 4 and also the fourth component of the symptom vector. The procedure for obtaining these vectors is the one described above. Assuming that twenty symptoms are recorded at the level of the patient group to which patient i belongs, the LIFE THEMES-SYMPTOMS matrix for this patient is the one presented in Table 1.
3.1.2. Computing Module (CM)
CM processes the matrices LIFE THEMES-SYMPTOMS of the patients investigated. It contributes to achieving the second specific objective.
The data flow diagram for this module is presented in
Figure 2.
The process Calculation of Normalized TFIDF Matrices requires, for each matrix Ai, the calculation of the number of life themes, where the presence of symptom i is signaled, df(i), the knowledge of the frequency of symptom i in life theme j, f(i,j), the number N of the life themes of the patient, and the column-wise normalization of TFIDF matrices. To compute df, we use the procedure outlined in Algorithm 2.
| Algorithm 2 Pseudocode for computing df |
| Input: |
| 1: Ai |
| Output: df
|
| 2: procedure for computing df |
| 3: Initialize df |
| 4: for each line k of Ai do |
| 5: Calculate the total number of non-zero components, df(k) |
| 6: end for |
| 7: return df |
| 8: end procedure |
CM uses relation (1) [
61] to calculate the specificity of symptom i within life theme j:
The specificity score is higher, as f(i, j) increases and df(i) decreases. The notation log2(…) is used in MATLAB R2024a and represents the base-2 logarithm of (…). Relation (1) transforms matrix Ai into matrix TFIDF.
To mitigate the impact of large variations in symptom specificities on the statistical correlations, we use column-wise normalization of the TFIDF matrix and Euclidean norm [
62]. To normalize a TFIDF matrix, we use the following formula:
For each matrix, CM uses the MATLAB command [U,S,V]=svd(TFIDF_normalised_ matrix) for the process of Decomposition of the Singular Value of Normalized TFIDF Matrices. The decomposition formula is [
61,
63]
where A is the normalized TFIDF matrix, S is a diagonal matrix containing n singular values of matrix A sorted in a descending order, and U and V are orthogonal matrices that contain eigenvectors.
For the process of Calculation of the Matrices From Which the Most Relevant Symptoms are Extracted, we need the number of the most relevant symptoms for each patient. This number, r, is deduced from , where is the singular value i. The equality indicates the amount of information retained after eliminating irrelevant symptoms. r is used to extract the most relevant symptoms and to calculate the approximated TFIDF matrix. To extract the most relevant symptoms, CM calculates, for each patient i, matrix , where and are the truncated matrices of S and U.
For the process of Extraction of the Most Relevant Symptoms of the Patients Investigated, we use Algorithm 3 and the abbreviated form of these symptoms. The most relevant symptoms of patient i are represented by a vector of labels associated with the highest absolute values of matrix Pi.
| Algorithm 3 Pseudocode for extracting MRS of the patients investigated |
| Input: |
| 1: Pi |
| Output: MRS of the patients investigated |
| 2: procedure for extracting MRS of the patients |
| 3: for each Pi do |
| 4: for each row k of Pi do |
| 5: Identify the largest absolute value and MRS(k) |
| 6: end for |
| 7: end for |
| 8: return MRS of the patients investigated |
| 9: end procedure |
For the process of Approximation of Normalized TFIDF Matrices, CM uses formula [
61]
where
is the approximated matrix obtained by the dimensionality reduction in A; U(:,1:r) is the matrix that contains all rows and the first r columns; S(1:r,1:r) is the matrix that includes the first r rows and the first r columns; V(1:r,:) is the matrix that includes the first r rows and all columns.
For the process of Calculation of the Spearman Correlations Between Symptoms, CM employs the formula for the Spearman correlation coefficient [
64,
65],
where
is the difference between the ranks of a pair of observations and n is the number of pairs of observations.
For the process of Calculation of the Spearman Correlations Between Life Themes, we also use relation (5).
The process of Calculation of Transposed Matrices from Approximated Matrices is carried out, for each matrix, by using the MATLAB command, transpose_matrix = transpose(matrix).
For the process of Identification of Symptomatic Noises, we use Algorithm 4 for each matrix Ai. Here, S is a vector of labels, and Sk is the label taken from the kth row of matrix Ai.
| Algorithm 4 Pseudocode for extracting symptomatic noises from Ai |
| Input: |
| 1: Ai |
| Output: Symptomatic noises, S |
| 2: procedure for extracting S |
| 3: for each row k of Ai do |
| 4: Calculate the number of non-zero components of row k |
| 5: if the number of nonzero components is equal to the number of columns of Ai |
| 6: add Sk to S |
| 7: end if |
| 8: end for |
| 9: return S |
| 10: end procedure |
In the case of the module of Extraction of Latent Symptoms From Life Themes Present in Approximated Matrices, the approximated matrices contain relevant dysfunctional life themes whose components are updated by taking into consideration the most relevant symptoms. Each life theme has its own latent symptom. The latent symptom contains the labels of the component symptoms associated with the positive values in the life theme vector.
Example 2. Let us assume that the approximated matrix contains three life themes and five symptoms presented in Table 2.
The latent symptom associated with T1 is S1S4S5, the latent symptom associated with T2 is S1S2S3S4S5, and the latent symptom associated with T3 is S1S3S4S5.
For the module of Extraction of Latent Symptoms and Symptoms Experienced Undistorted from the Significant Associations Between Symptoms, it is essential to specify that latent symptoms result from the significant positive associations between symptoms. In contrast, the symptoms experienced undistortedly result from the significant negative associations between symptoms.
For example, for correlation S2–S3, , where is the value of the Spearman correlation coefficient and p is the p-value corresponding to , the symptom experienced undistortedly is S2 or S3, if and only if neither of the two symptoms is involved in a perfect positive association. In the case of significant positive associations between symptoms, identifying the latent symptom is straightforward. For example, for correlation S2–S3, , the latent symptom is S2S3. Life themes experienced undistortedly are extracted similarly.
3.1.3. Aggregation Module of All Matrices LIFE THEMES-SYMPTOMS
The inputs of this module are the matrices LIFE THEMES-SYMPTOMS of all the patients investigated. The output is represented by the aggregated matrix. The data flow diagram is presented in
Figure 3.
For the process of Aggregation of Matrices, we use Algorithm 5.
| Algorithm 5 Pseudocode for generating the aggregated matrix |
| Input: |
| 1: The matrices LIFE THEMES-SYMPTOMS of all patients, Ais |
| Output: Aggregated matrix LIFE THEMES-SYMPTOMS, A_group |
| 2: procedure for generating A_group |
| 3: Concatenate Ais horizontally, A_concatenated |
| 4: for each life theme in A_concatenated do |
| 5: Identify the positions where the life theme is present in A_concatenated |
| 6: if the life theme is unique in A_concatenated |
| 7: Write the life theme vector in A_group |
| 8: end if |
| 9: if the life theme appears at multiple positions in A_concatenated |
| 10: Sum up the column vectors corresponding to the positions identified |
| 11: Write the result in A_group |
| 12: end if |
| 13: end for |
| 14: return A_group |
| 15: end procedure |
The result of aggregating matrices Ais is presented in
Table A45.
3.1.4. Computing Module on the Aggregated Matrix
The input of this module is the aggregated matrix LIFE THEMES-SYMPTOMS. The outputs are the representations of patients’ life themes and problematic symptoms. The data flow diagram is presented in
Figure 4.
All the processes of this module, except for two, are similar to those presented in CM. The two processes are described below.
First is the calculation of Life Theme Representations, for which we apply formula [
61]
where LTg, Pg, and NTFIDFg are matrices at the level of the group of patients. LTg contains the representations of life themes through column vectors calculated in relation to the most relevant symptoms extracted from Pg.
Second is the calculation of the Representations of the Patients’ Problematic Symptoms, for which we apply formula [
61]
where PSg is the representation of the column vector of the problematic symptom at the level of the group of patients and SPSg is the vector of the specificity of the problematic symptom at the level of the group of patients.
For example, for a total of N = 26 life themes, the vector of the specificity for S2S3, where dfg(2) = 3 and dfg(3) = 4, takes the form .
3.1.5. Query Module
The function of this module is to provide discussion topics for the patient’s psychotherapy sessions. This module ensures the achievement of the third specific objective.
The inputs of this module are the outputs of the Computing Module on the Aggregated Matrix presented in
Section 3.1.4. The output is represented by a set of discussion topics with the potential to improve problematic symptoms in each patient.
To fulfill its function, the module uses cosine similarity calculation between two vectors. The vectors must have the same dimension. The cosine similarities are calculated between each problematic symptom and each life theme recorded at the level of the group of patients. Since the components of the life theme vectors are represented by symptoms extracted from matrix Pg, the problematic symptom vectors must have the same components. This way, we obtain an alternative representation of the patient’s problematic symptoms at the level of the group of patients.
The alternative representation of the problematic symptom is not the same as the representation of the patient’s problematic symptom. The patient’s problematic symptom is represented based on the most relevant symptoms extracted from matrix Ai, whereas the alternative representation takes into account the most relevant symptoms extracted from matrix A_group.
The criterion used to assess the symptomatic improvement potential of a life theme is the similarity one. Dissimilarity leads to symptomatic improvement, while similarity leads to symptomatic preservation or exacerbation.
For cosine similarity calculation, we use formula [
61]
where
and
are two vectors.
In order for a life theme to be considered dissimilar in relation to a problematic symptom, it is necessary for the application of Formula (8) to lead to a negative result.
The data flow diagram for this module is presented in
Figure 5.
The process of Calculation of Similarities applies Algorithm 6.
| Algorithm 6 Pseudocode for calculating the similarities of life themes in relation to problematic symptoms
|
| Input: |
| 1: Representations of life themes |
| 2: Representations of the patients’ problematic symptoms |
| Output: Problematic symptoms as column vectors of life theme similarities |
| 3: procedure for calculating the similarity of life themes in relation to problematic symptoms |
| 4: Initialize the vectors of problematic symptoms |
| 5: for each vector of the problematic symptom do |
| 6: for each vector of the life theme do |
| 7: Calculate the similarity between the two vectors |
| 8: Add the similarity value to the vector of the similarities of life themes in relation to the |
| problematic symptom |
| 9: end for |
| 10: end for |
| 11: return Problematic symptoms as column vectors of life theme similarities |
| 12: end procedure |
Applying Algorithm 6 leads to the results presented in
Table A51.
The process of Searching for Suitable Discussion Themes to Alleviate Problematic Symptoms applies Algorithm 7. For each patient, this process filters the life themes recorded at the level of the group of patients from their dysfunctional life themes (see
Table A1,
Table A2,
Table A3,
Table A4,
Table A5,
Table A6,
Table A7,
Table A8,
Table A9,
Table A10 and
Table A11) and also from similar life themes in relation to their problematic symptoms. The output of Algorithm 7 is represented by a vector of the life theme labels for each patient.
| Algorithm 7 Pseudocode for generating the most suitable discussion themes for patients’ psychotherapy sessions
|
| Input: |
| 1: Problematic symptoms as column vectors of life theme similarities |
| 2: Patients’ dysfunctional life themes |
| Output: Discussion themes for the patients’ psychotherapy sessions |
| 3: procedure for extracting the discussion themes for the patients’ psychotherapy sessions |
| 4: for each patient do |
| 5: for each vector of the problematic symptom do |
| 6: for each row k of the vector of the problematic symptom do |
| 7: if life theme k is dissimilar in relation to the patient’s problematic symptom |
| 8: if life theme k is not one of the patient’s dysfunctional life themes |
| 9: add life theme k to life themes dissimilar in relation to the problematic symptom of the patient and also distinct in relation to the life themes of the patient |
| 10: end if |
| 11: end if |
| 12: end for |
| 13: end for |
| 14: end for |
| 15: return Discussion themes for the patients’ psychotherapy sessions |
| 16: end procedure |
4. Testing and Validation of the Computing System
The computing system was subjected to testing on a group of eleven patients diagnosed with major recurrent depression. Each of these patients experienced at least three relapses and attended psychotherapy sessions for six months. These sessions focused on discussing the life topics suggested by the computing system. Additionally, the conduct of the psychotherapy sessions took into account the patients’ illness patterns.
The procedure for testing the computing system consisted of two phases:
4.1. The Application Phase
The testing of the computing system took place at a psychiatric hospital in Romania. The Ethics Committee of Lucian Blaga University of Sibiu, Romania approved the research and use of data for research purposes (decision no. 27 dated 10 May 2023). All the patients selected for our study were individually informed about how the study would be conducted. They provided informed consent for the anonymous use of data for scientific purposes [
1]. The data subject to confidentiality are those related to identity and reports about one’s own life. Also, the ethics report specifies the task of maintaining data confidentiality even after completing the research.
4.1.1. Selection of Participants
The computing system was designed to capture the specificities of depression patterns regardless of the age of the patients investigated. The patients were selected based on the following inclusion/exclusion criteria [
1]:
Inclusion criteria
Exclusion criteria
Initially, twenty-four patients with a diagnosis of major recurrent depression who met the inclusion criteria were selected. The application of the exclusion criteria led to the elimination of two patients with unstable mental status under medication, six patients with a history of seizures, and five patients diagnosed with alcohol dependence in the last six months. Only patients without secondary affective disorders induced by substances or medical conditions directly affecting the brain were included in the study [
1].
We considered relevant for the analysis of the system’s ability to extract the essence from the patients’ illness model the presentation of the following data of the patients selected for the study: the average age of the eleven patients was 47.73 years (SD = 3.25; range = 37–49 years). In total, 45.5% were females with the average age of 48.13 years (SD = 2.97; range = 39–51 years), while 55.5% were males with the average age of 46.67 years (SD = 4.01; range = 39–50 years). Further, 36.4% were married, 36.4% were unmarried, and 27.2% were divorced. Regarding employment status, 45.5% were employed, and 54.5% were retired due to illness. Finally, 36.4% obtained higher education, and 63.64% completed high school.
4.1.2. The Results Generated by the Computing System
The content analysis of the patients’ themes of happiness, unhappiness, and daily life led to the identification of twenty-six life themes and seven symptoms coded in
Table 3 [
1].
Implementation of CM for each patient resulted in the outcomes presented in
Table A12,
Table A13,
Table A14,
Table A15,
Table A16,
Table A17,
Table A18,
Table A19,
Table A20,
Table A21,
Table A22,
Table A23,
Table A24,
Table A25,
Table A26,
Table A27,
Table A28,
Table A29,
Table A30,
Table A31,
Table A32,
Table A33,
Table A34,
Table A35,
Table A36,
Table A37,
Table A38,
Table A39,
Table A41,
Table A42,
Table A43 and
Table A44.
The synthesis of the illness pattern for each patient, inferred from the results obtained (see
Table A1,
Table A2,
Table A3,
Table A4,
Table A5,
Table A6,
Table A7,
Table A8,
Table A9,
Table A10,
Table A11,
Table A23,
Table A24,
Table A25,
Table A26,
Table A27,
Table A28,
Table A29,
Table A30,
Table A31,
Table A32,
Table A33,
Table A34,
Table A35,
Table A36,
Table A37,
Table A38,
Table A39,
Table A41,
Table A42,
Table A43,
Table A44 and
Table A50), is presented in
Table 4.
The solutions for improving the problematic symptoms generated by the computing system (as a result of applying Algorithm 7) are presented in
Table 5.
4.2. The System Performance Evaluation Phase
Before the implementation of the computing system, all patients attended two psychotherapy sessions per month for two months. The applied psychotherapy was the cognitive behavioral one. At initial assessment, all patients presented Beck scores (PSYS0) corresponding to a severe level of depression. The efficiency of each psychotherapy session (PSYSi) was analyzed in relation to the previous one by comparing the Beck scores of the eleven patients (see
Table 6).
The sign test was used to assess the efficiency of each session. The
p-values (see
Table 7) and the number of positive differences between the Beck scores recorded (PSYSi−PSYSi + 1) show that statistically, the depression levels of the eleven patients remained unchanged.
The Beck scores of the last psychotherapy session became the initial levels of depression in the testing procedure of the computing system.
Our intention was to test the efficiency of the computing system for two months, during which each patient received two psychotherapy sessions per month. The results obtained showed that the computing system was efficient. Consequently, we continued the testing procedure for the next four months, during which patients additionally received eight psychotherapy sessions. The results obtained are presented in
Table 8,
Table 9 and
Table 10. The overall effect of efficiency was measured by comparing the Beck scores corresponding to the first and last evaluations of all the patients.
The medians of the 13 columns presented in
Table 9 confirm the trend of improvement in the illness.
The
p-values below 0.05 presented in
Table 10 confirm that, over the period of the six months of psychotherapy, the solutions provided by the computing system proved to be effective. The comparison of the results obtained by all patients at the initial and final evaluation confirms a clear improvement in the illness. At the end of the six months of psychotherapy, all patients recorded Beck scores corresponding to the level of moderate depression. However, there were two instances where the efficiency of the computing system solutions recorded a plateau. This demonstrates, at least in the case of the patients investigated, that the impact of applying computing system solutions becomes significant over time.
The evaluation phase of the computing system’s efficiency also included its ability to accurately capture the illness patterns of the patients. The symptoms observed by the attending physicians/psychologists were compared to those inferred by the computing system. Essentially, the symptoms deduced from clinical observation were compared to those obtained from the patients’ narratives (see
Table A1,
Table A2,
Table A3,
Table A4,
Table A5,
Table A6,
Table A7,
Table A8,
Table A9,
Table A10 and
Table A11). All symptoms resulting from the application of the computing system were fully confirmed by the attending physicians/psychologists.
In addition to these symptoms, the computing system generated other characteristics of the illness pattern that could not be noticed by specialists. These include irrelevant life themes, latent life themes, problematic symptoms, and the most relevant symptoms. Assessing these characteristics contributes to a deeper understanding of each patient’s illness pattern.
It is important to mention that the medication administered to each patient remained unchanged throughout the attendance of the psychotherapy sessions. This period also includes the two months of psychotherapy prior to the implementation of the computing system. Of course, the effect of the medication administered to the eleven patients contributed to achieving these results over time. A comparative analysis of the Beck scores recorded before and after using the computing system shows us that some of these results are due to the solutions provided by this system to alleviate the problematic symptoms of the patients.
5. Discussion
The specialized literature addresses topics related to our research studying the relationships between life themes and severe depression or between life events and depressive symptoms [
66,
67,
68,
69]. In these works, the focus is directed towards identifying the causes that trigger and sustain severe depression.
The purpose of our work was to test the ability of LSA to describe personalized patterns of severe depression and generate illness improvement solutions. The testing of LSA was conducted through a computing system applied in a six-month longitudinal study. Future patient psychotherapy used the results provided by the computing system.
Applications and concerns regarding the use of computing techniques in psychiatry, clinical psychology, and psychotherapy are numerous [
70,
71,
72,
73].
The way these techniques are used requires adaptations, according to the context pursued. In our research, we attempted to adapt LSA techniques in such a way that they correctly identify the patient’s illness pattern. We were not interested in finding similarities between patients’ illness patterns because, in our opinion, they lack utility. In the classical approach to LSA and related to our paper, both the symptoms and their sources, represented by life themes, are treated globally to identify semantic relationships between them. Here, the interest is directed towards finding generic features of the illness. We attempted to directly relate the patient’s symptoms to their life themes. Thus, one of the adaptations of LSA used in capturing the illness pattern consisted in using the matrix LIFE THEMES-SYMPTOMS for each patient, instead of using a single matrix LIFE THEMES-SYMPTOMS for all the patients investigated. This adaptation is useful as it facilitates, strictly at the patient level, the calculation of correlations between life themes/symptoms from which latent and undistorted symptoms can be extracted. The calculation of correlations uses the column vectors of the approximated matrices of normalized TFIDF matrices, obtained through dimensionality reduction. Also, these patient-specific matrices allow the identification of the presence of symptomatic noises, which are another category of symptoms with the potential to exacerbate the illness. Additionally, extracting solutions for improving each patient’s illness require exclusively the adaptation of some matrix calculation techniques. These aspects are some of the many reasons why we opted for a numerically adapted approach of LSA instead of LSA performed by its specialized module.
For each patient, MATLAB calculation programmes were run using the algorithms presented in the paper. Alternatively, other programming environments (R, Python, Mathematica) can be used.
Teamwork significantly reduces the time to generate results for all patients investigated. As shown in the architecture of the calculation system, generated results for each patient involve, additionally, the performance of calculations at the level of the group of patients. The time for generating all results, including the time for data input, validation, data checking, and the calculations, was approximately 135 min, with the involvement of five specialists.
Severe cases of clinical depression with many relapses require new, specific approaches capable of capturing and treating what is difficult to capture in the illness. We sought to extract the patient’s illness pattern (see
Table 4) by including both observable sources of dysfunctionality and some less visible ones that may lead to negative illness progression. In these cases, all life themes are dysfunctional and generate an entire life history dominated by morbid experiences. The fact that psychotherapy sessions did not show progress in alleviating the illness prior to the implementation of the computing system led us to the idea that addressing the observed symptoms by discussing the patient’s life themes might not be the most suitable option. Therefore, we sought to identify the problematic symptoms of the patient defined in the paper and the appropriate discussion topics distinct from their life themes but with the potential to alleviate their problematic symptoms. The choice of these different life themes aims to break the link between the problematic symptoms and the dysfunctional life themes of patients.
The results in improving the illness after the application of the computing system indicate that problematic symptoms should be prioritized for treatment, and also that a distinction should be made between the problematic symptoms and those observed. For patient 4, the computing system identified thematic solution T13 for improving all problematic symptoms (see
Table 5). For the other patients, multiple solutions corresponding to groups of problematic symptoms were identified. These multiple solutions show us that thematic solutions can be dissimilar to certain problematic symptoms and similar to other problematic symptoms. Since thematic solutions are distinct from dysfunctional life themes, which are linked to problematic symptoms, the likelihood of activating these symptoms is virtually zero. Why? Distinct life themes determine new experiences that are different from the dysfunctional symptoms of the patients. The similarity between the thematic solution chosen by the computing system and its latent experience is higher than the similarity between the same thematic solution and each of the problematic symptoms targeted for improvement. Therefore, the effect of distinct life themes manifests in deactivating problematic symptoms, which results in their improvement. To alleviate all problematic symptoms, the solutions generated by the computing system must be discussed in the same psychotherapy session. Where there are multiple solutions for the same symptoms it is sufficient to choose one of them.
As mentioned above, we addressed the objective of finding the most suitable discussion topics for psychotherapy sessions from the perspective of similarity/dissimilarity. The higher the dissimilarity between a life theme vector and a problematic symptom vector, the lower the likelihood of the patient experiencing the problematic symptom. Consequently, the dysfunctional experience can be replaced by a new experience. A life theme similar to a specific problematic symptom sustains the patient’s temptation to experience the dysfunctional symptom. A possible explanation could be the inability of the life theme to distract the patient from their dysfunctional concerns. Thus, there is an exacerbation of the problematic symptom over time.
A distinction should be made between what is noticed in the illness and reality. Extremely rarely does a patient experience a particular symptom undistorted. If this happens, the experience is extremely intense, bordering on unbearable. Candidates for these symptoms are those involved in significant negative correlations. In reality, the symptoms observed are the most intense symptoms of a more extensive corpus of symptoms at a given moment. Usually, at any given moment, the patient or person experiences a combination of symptoms that we call a latent symptom. Latent symptoms differ from the observed symptoms in that they are much more complex. Another symptom, distinct from those observed, is symptomatic noise (see Algorithm 4). This is a symptom that maintains a background of anxiety and stress for the patient. Symptomatic noise can be a favoring factor in exacerbating the illness in the case of irrelevant life themes whose symptomatic content includes exclusively symptomatic noises. These themes are dysfunctional because they are experienced nonspecifically. All these aspects suggest that the three categories of symptoms hold significant potential for exacerbating the illness.
The symptoms extracted by LSA as the most relevant symptoms are semantic structures extracted from a truncated space. More clearly, in the context of the paper, a symptom extracted from the matrix Pi (see Algorithm 3) is semantically associated with the context represented by the life themes of the patient; it appears in similar contexts in the life themes of the patient, and it has a vector similar to the vectors associated with life themes. In a particular sense, we can say that the dysfunctional thematic context of the patient is best represented by the symptoms extracted by LSA.
The analysis of the results generated by the computing system highlights several interesting aspects. Although the illness levels of all patients investigated are significantly reduced after six months of psychotherapy, cognitive impairments continue to manifest. These predominantly take the form of negative self-evaluations and self-deprecating thoughts, which can be significant sources of relapse. The specialized literature confirms this possibility [
22,
23,
74,
75,
76].
A specific characteristic of clinical depression refers to the frequency of symptoms. The specialized literature indicates that, in severe depressive illness, the most common symptoms are anxiety and sadness [
77,
78,
79]. The analysis of
Table A1,
Table A2,
Table A3,
Table A4,
Table A5,
Table A6,
Table A7,
Table A8,
Table A9,
Table A10 and
Table A11 confirms the findings of the specialized literature in the case of patients 3 and 4. The symptom of sadness records higher frequencies compared to other symptoms in patients 3, 4, 6, 7, and 11. The high scores recorded for symptomatic noises represented by fury, regret, and low self-esteem are noteworthy in the case of patient 1. We consider that the differences from the findings recorded in the specialized literature are due to the specificity of the illness.
Another important characteristic refers to the presence, in all patients, of complex latent symptoms that induce combinations of morbid experiences. The difference between a latent symptom in a depressive patient and a latent experience in a balanced person lies in the content of the experience, which, in the case of the depressive patient, is exclusively morbid.
In the same context, some latent life themes amplify latent symptoms (see
Table A34,
Table A35,
Table A36,
Table A37,
Table A38,
Table A39,
Table A41,
Table A42,
Table A43,
Table A44 and
Table A50). A latent life theme amplifies a latent symptom if the vectors of life themes associated contain positive values of the same components. This is the case of patient 1, where the latent life themes T1T19, T1T17, and T17T19 amplify the latent symptom S1S2S6S7; of patient 5, where the latent theme T1T8 amplifies the latent symptom S1S2S5S6; of patient 6, where the latent theme T1T2 amplifies the latent symptom S1S2S3S4; and of patient 10, where the latent theme T14T15 amplifies the latent symptom S1S2S3S5S7.
Another interesting aspect, inferred from the same table, refers to the possibility of the simultaneous, distorted experiencing of multiple life themes. This aspect is noticed in the case of life themes T1, T19, T17, and T5 in patient 1, respectively, in the case of life themes T3, T14, and T15 in patient 5. Also, the analysis of correlations between these themes suggests the possibility of the existence of mechanisms capable of generating dysfunctional thematic cycles.
The same table indicates the possibility of experiencing life themes/symptoms in a pure, undistorted manner. We identified these experiences in the case of patient 1, where the results indicate a high probability of undistorted experiencing of symptom S7, and in the case of patient 2, where the results also indicate a high probability of undistorted experiencing of symptoms S4, S6, and S7. Also, there is a high likelihood of undistorted experiencing of life theme T6 in patient 2.
The suggestion of the same life topics for all psychotherapy sessions is explained by the fact that no changes occurred over time in the structure of the patients’ dysfunctional life themes. Thus, at least in the cases analyzed, we can speak about a closed set of life themes. At the same time, the improvement of the illness can be explained by the perspectives determined by the discussion of the life topics selected by the computing system, which leads to a functional reinterpretation of the patient’s dysfunctional life topics or by focusing attention on other life themes.
The computing system continues to be tested on patients with encouraging results. Although it has demonstrated its effectiveness on the patients investigated, we believe that a more significant number of improved illness cases could strengthen confidence in the system’s ability to extract what is essential in the illness and provide solutions for improving the illness. On the other hand, the sustainability of the effectiveness of the psychotherapeutic approach suggested by the computing system has not been tested for periods longer than two weeks. However, we consider it necessary for patients to continue psychotherapy sessions, at least to alleviate and eliminate cognitive impairments.
Theoretically, a limitation of the method proposed may be the system’s inability to generate discussion topics capable of leading to symptomatic improvement in patients. In such situations, it is necessary to increase the number of patients investigated to identify life themes distinct from the patient’s themes and dissimilar to their problematic symptoms. At the same time, the computing system does not perform psychotherapy. But the results of psychotherapy applied to the patients investigated validated the effectiveness of the computing system.
Using the research framework presented, we aim to continue applying the computing system to obtain many illness patterns associated with symptomatic relief solutions.
Another objective aims to identify the mechanisms of rumination and transition from one dysfunctional life theme to another. We aim to apply the theory of algebraic groups to non-numeric structures. In the hypothesis of identifying compelling theories, proven by reality, we intend to integrate these mechanisms in describing depression patterns in patients.
6. Conclusions
The proposed computing system is primarily intended for use in cases of severe depression. The computing system serves a dual purpose: to provide a model of the patient’s illness and to offer solutions for improving the illness. The key element revealed by the computing system in improving the patient’s illness is the substitution of dysfunctional life themes with other themes that keep problematic symptoms inactive or alleviate them.
Compared to other similar/related research, our study addresses severe depression from the perspective of semantic relationships between dysfunctional life themes and symptoms, latent life themes and symptoms, irrelevant life themes, symptomatic noise, distorted/undistorted experienced symptoms, and life themes with potential for symptomatic improvement/exacerbation.
The results obtained show that the computational system and medication treatment can be successfully used in alleviating complex cases of illness.