Stratification and Adaptation of Malaria Control Interventions in Chad
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Site
2.2. Data Collection
2.2.1. Malaria Data
2.2.2. Environmental Data
2.2.3. Population Data
2.2.4. Data Quality Checking
- -
- Register and MMR data mismatch rate
- -
- Data agreement rate = 100 − discrepancy rate
- -
- greater than 95% was labeled good data quality;
- -
- between 90 to 95% was labeled average data quality;
- -
- less than 90% was labeled poor data quality.
2.2.5. Data Analysis
Annual Incidence of Malaria
Scenario 1: Crude Incidence
Scenario 2: Incidence Adjusted for Biological Confirmation Rate
Scenario 3: Incidence Adjusted for Health Facility Attendance Rate
Scenario 4: Incidence Adjusted for Laboratory Diagnosis Confirmation and Attendance Rates
- -
- Very low malaria transmission zone: incidence less than 100 cases per 1000 person (or parasite prevalence < 1%).
- -
- Low malaria transmission zone: incidence between 100 to 250 cases per 1000 person (or parasite prevalence 1–10%);
- -
- Moderate malaria transmission zone: incidence between 250 to 450 cases per 1000 person (or parasite prevalence between 10–35%);
- -
- High malaria transmission zone: incidence greater than 450 cases per 1000 person (or parasite prevalence > 35%).
Prevalence of Malaria
Distribution of Malaria Parasites
Infant and Child Mortality
Meteorological Data
Entomology
- -
- Mortality < 90%: Resistance confirmed;
- -
- Mortality between 90–97%: Probable resistance;
- -
- Mortality between 98–100%: Susceptible.
Seasonality of Malaria
Targeting of Interventions by Transmission Zone
2.2.6. Statistical Tools
2.2.7. Ethical Considerations
3. Results
3.1. Malaria Incidence
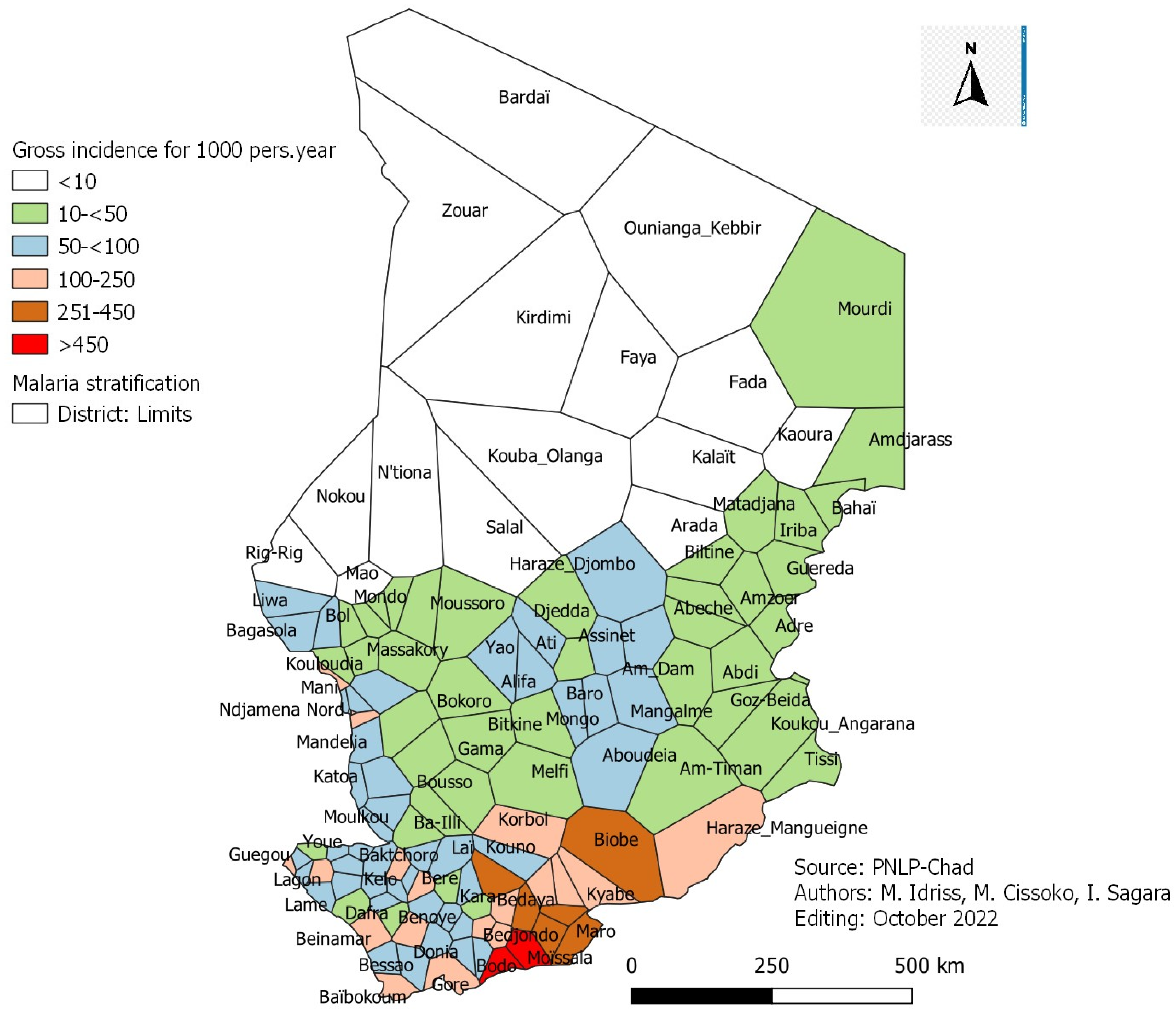
3.2. Malaria Crude Incidence
- -
- One hundred and two (102) health districts are in the very low malaria transmission zone;
- -
- Nineteen (19) health districts are in the low malaria transmission zone;
- -
- Six (6) health districts are in the moderate malaria transmission zone;
- -
- Two (2) health districts are in the high malaria transmission zone.
3.3. Incidence Adjusted for Malaria Laboratory Confirmation Rate
- -
- Eighty-seven (87) health districts are in the very low malaria transmission zone;
- -
- Twenty-nine (29) health districts are in the low malaria transmission zone;
- -
- Eleven (11) health districts are in the moderate malaria transmission zone;
- -
- Two (2) health districts are in the high malaria transmission zone.
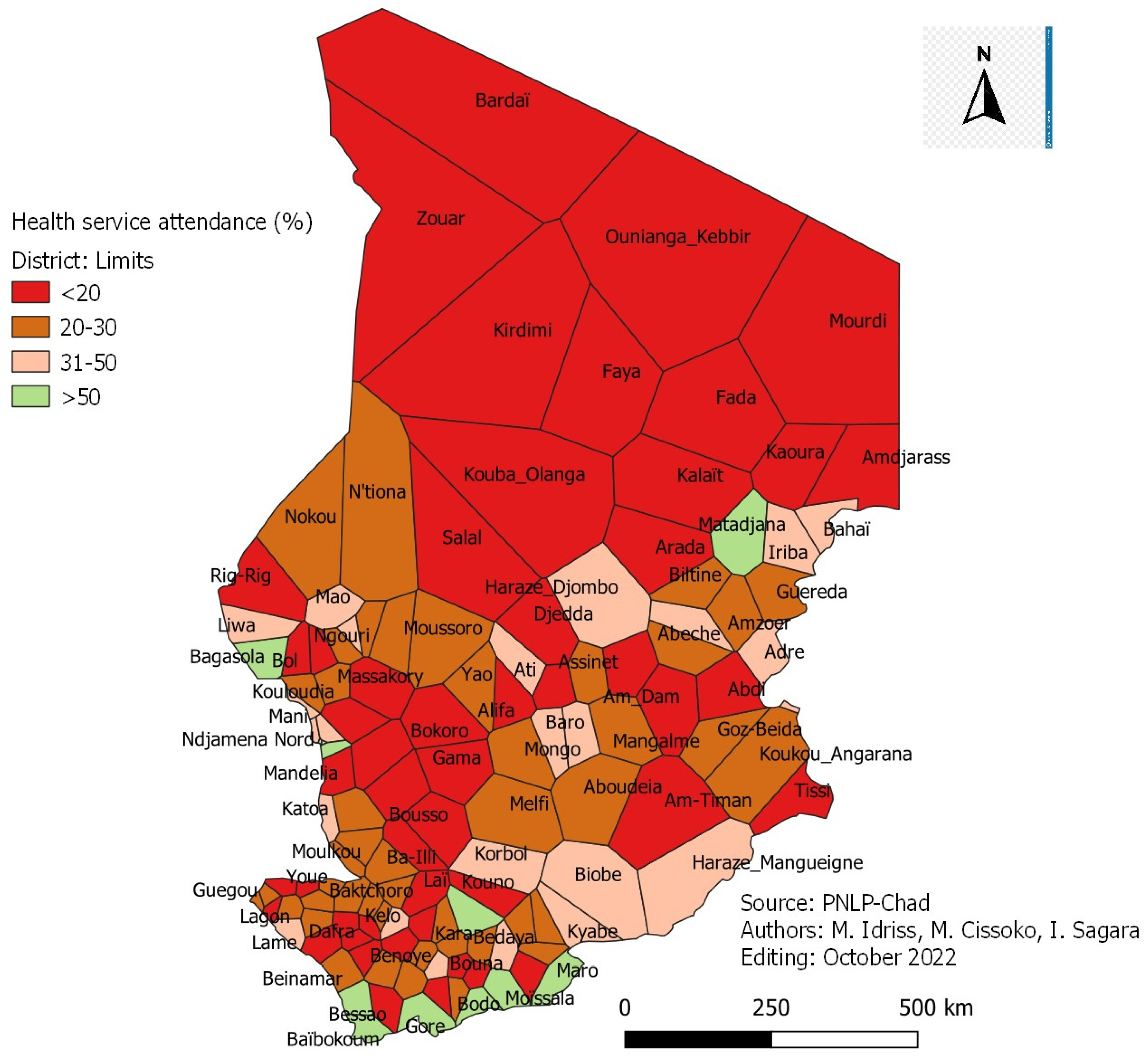
3.4. Incidence Adjusted for Attendance Rate
- -
- Twenty-eight (28) health districts are in the very low malaria transmission zone;
- -
- Thirty-nine (39) health districts are in the low malaria transmission zone;
- -
- Forty-one (41) health districts are in the moderate malaria transmission zone;
- -
- Twenty-one (21) health districts are in the high malaria transmission zone.
Accessibility to Health Services
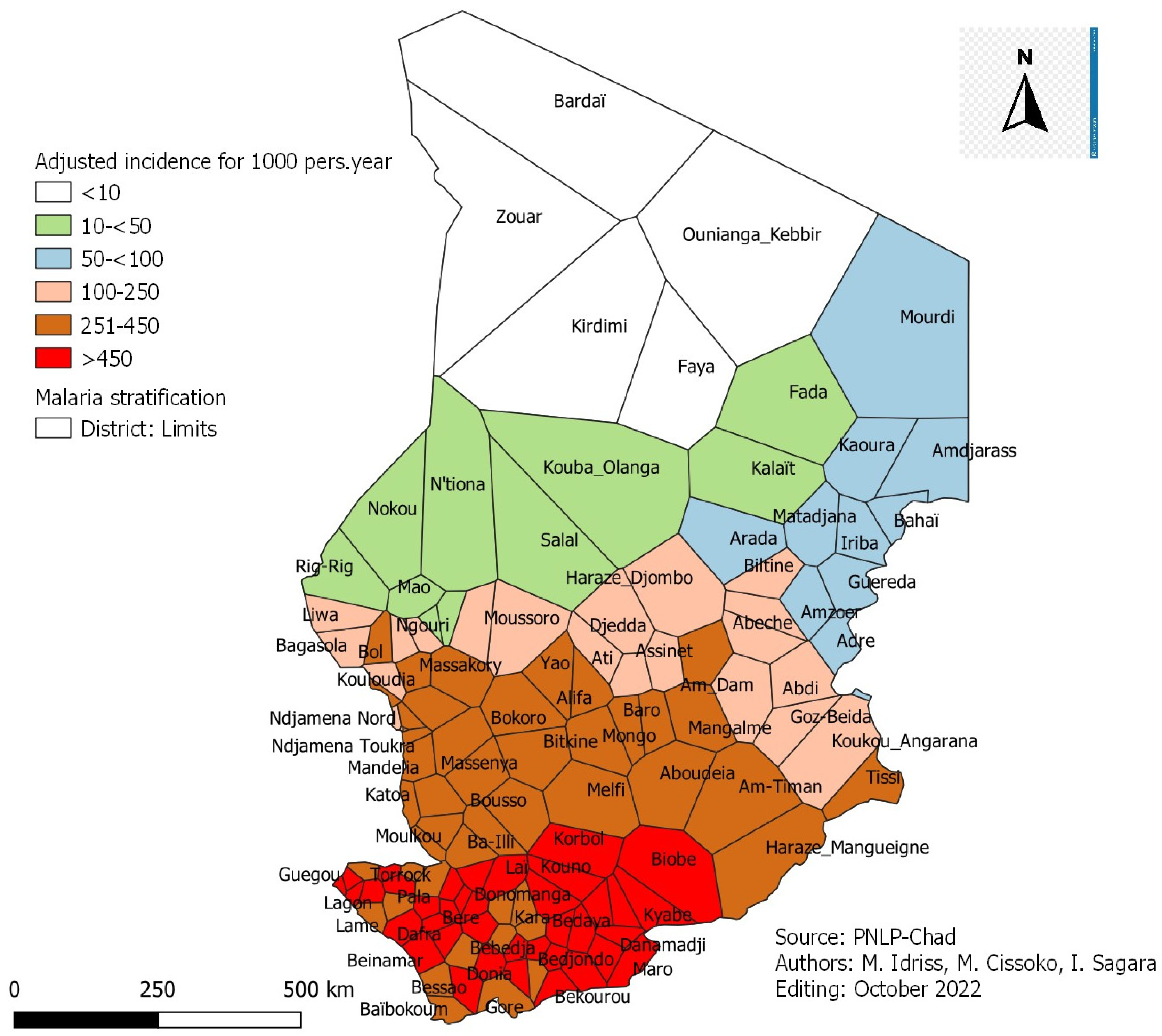
3.5. Incidence Adjusted for Malaria Laboratory Confirmation and Attendance Rates
- -
- Twenty-five (25) health districts are in the very low malaria transmission zone, including five (5) districts with an incidence <10 per 1000, nine (9) districts with an incidence between 10 and <50 per 1000 and 11 districts with an incidence between 50 and <100 cases per 1000 person;
- -
- Twenty (20) health districts are in the low malaria transmission zone;
- -
- Forty-six (46) health districts are in the moderate malaria transmission zone;
- -
- Thirty-eight (38) health districts are in the high malaria transmission zone.
3.6. Incidence of Malaria in Children under Five (5) Years Old
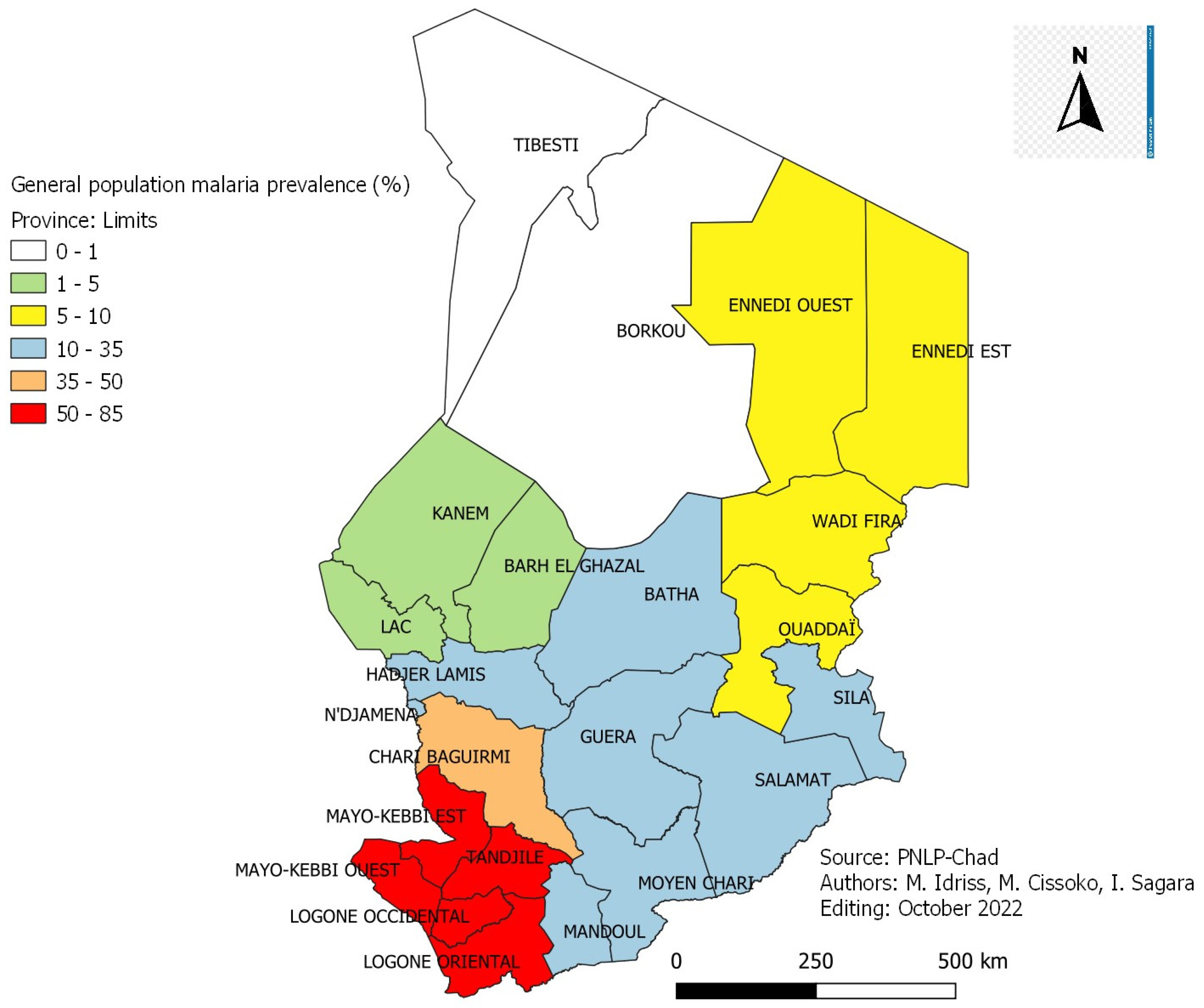
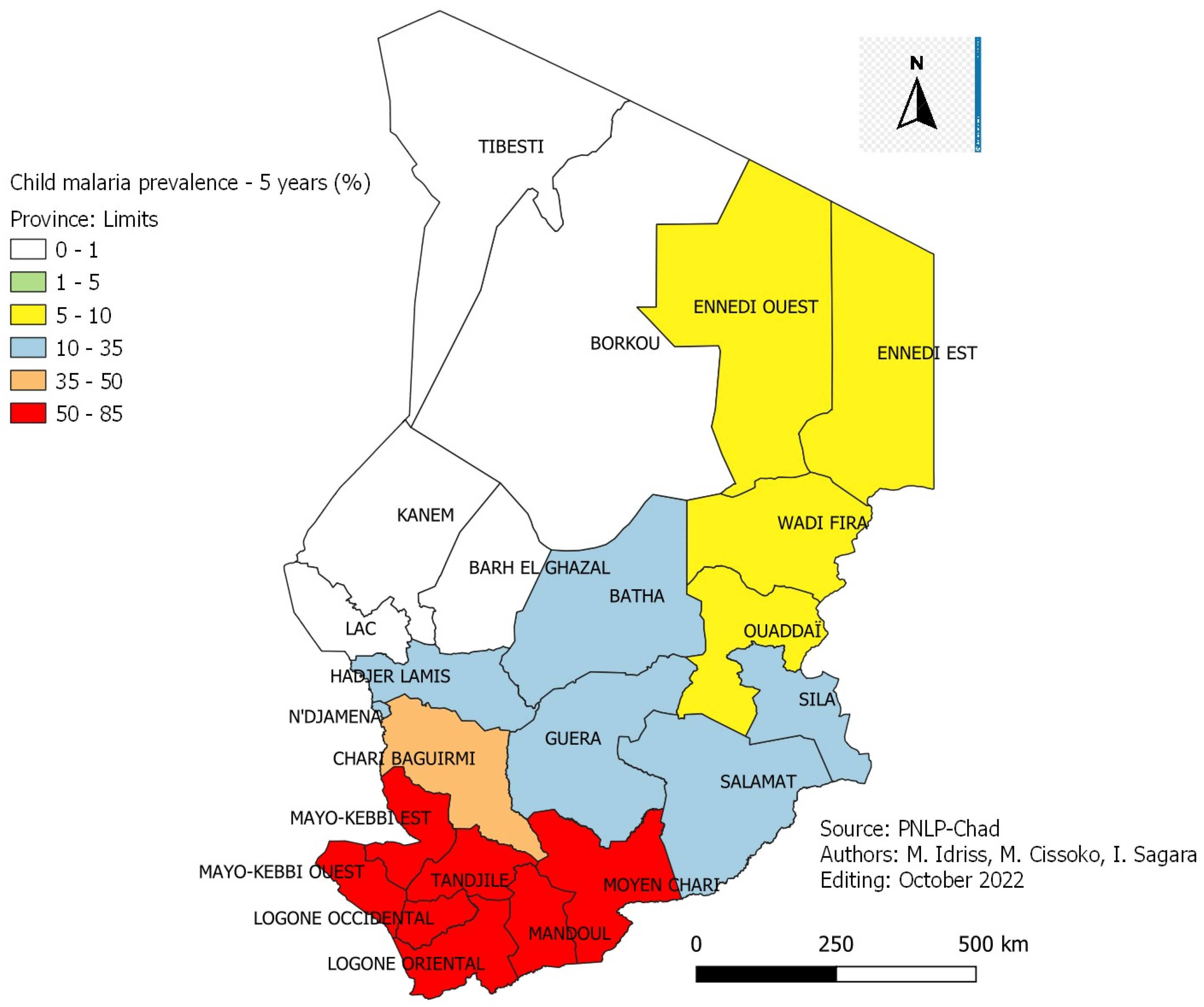
3.7. The Prevalence of Malaria
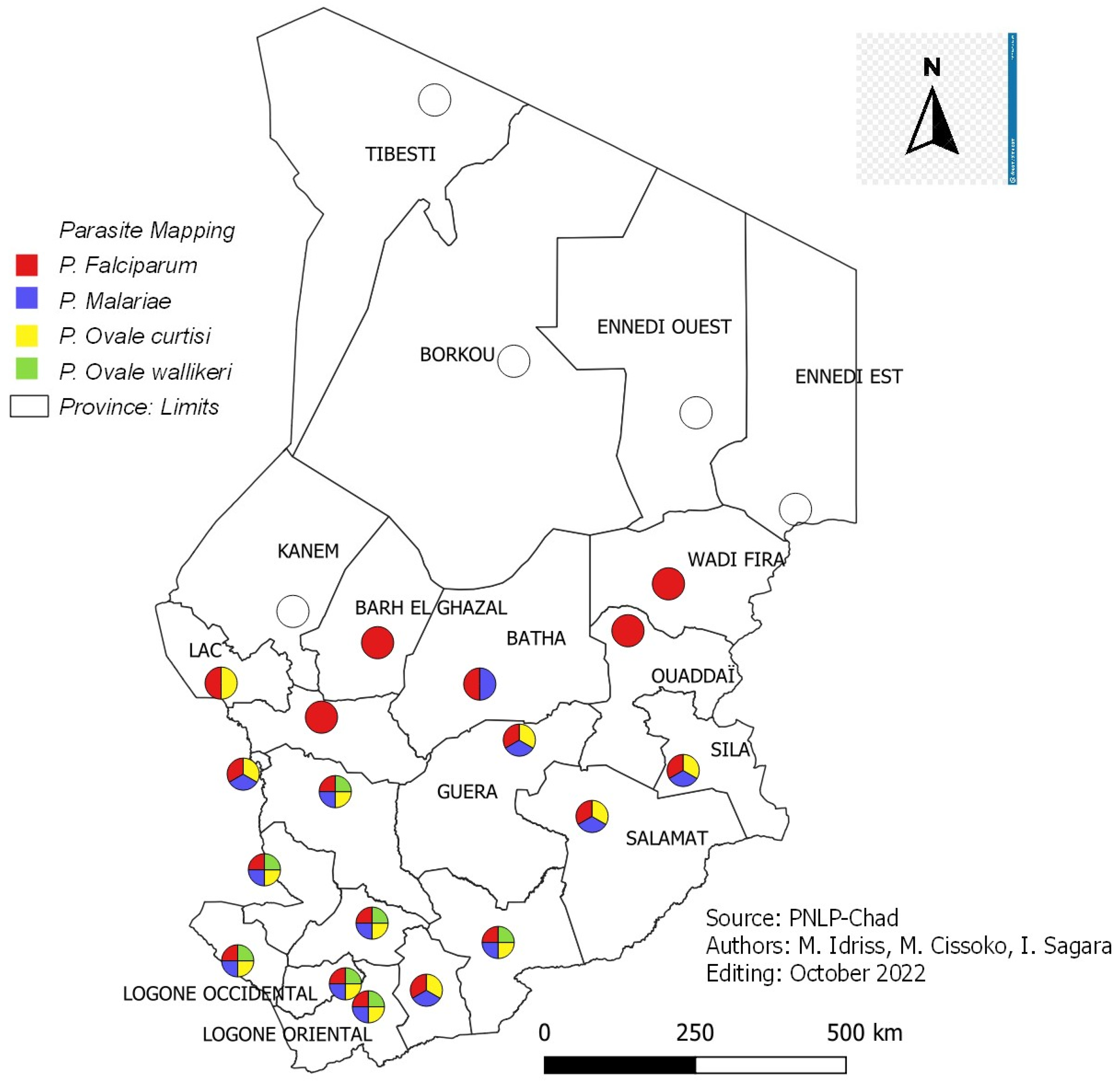
3.8. Distribution of Parasitic Species in Chad
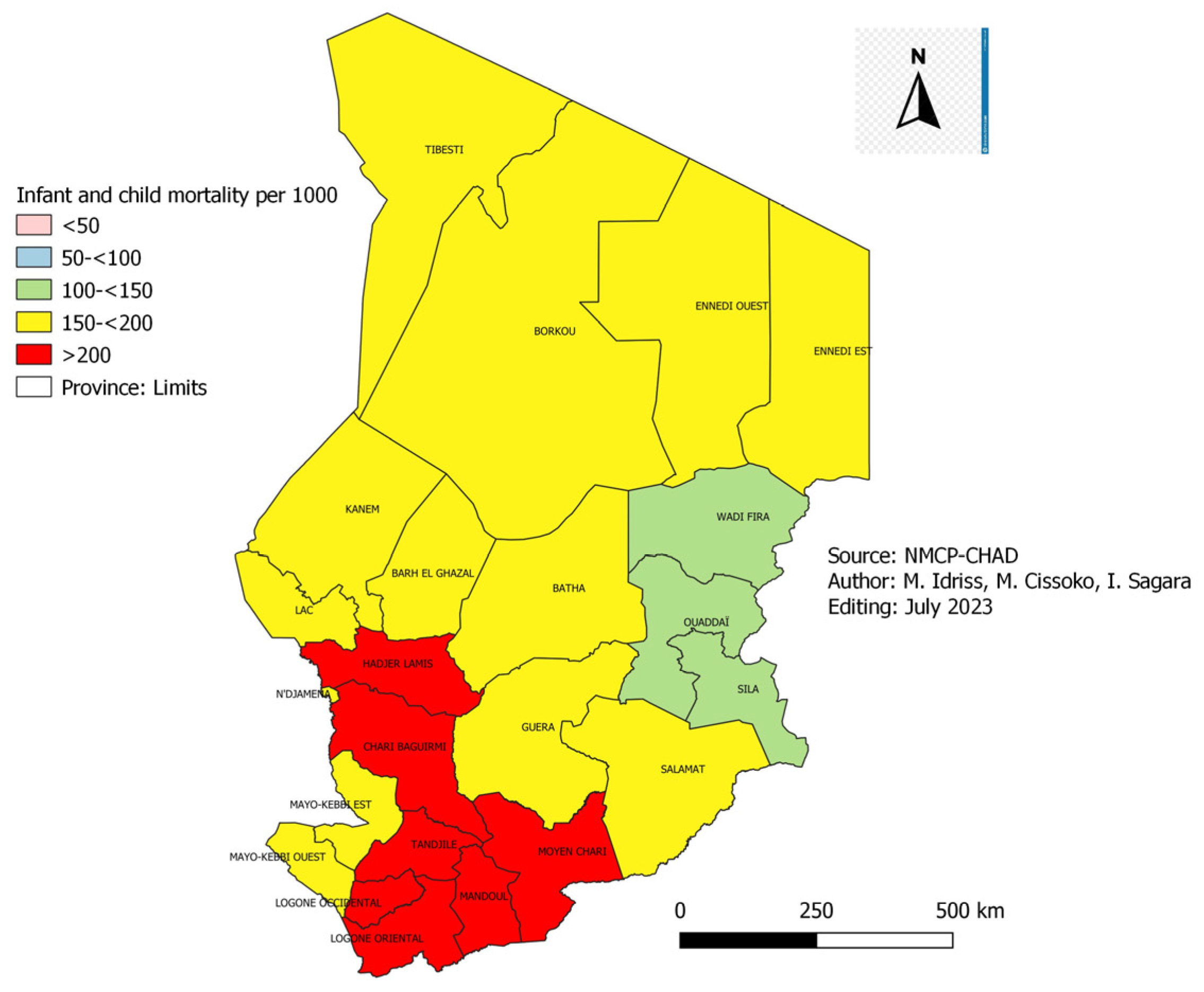
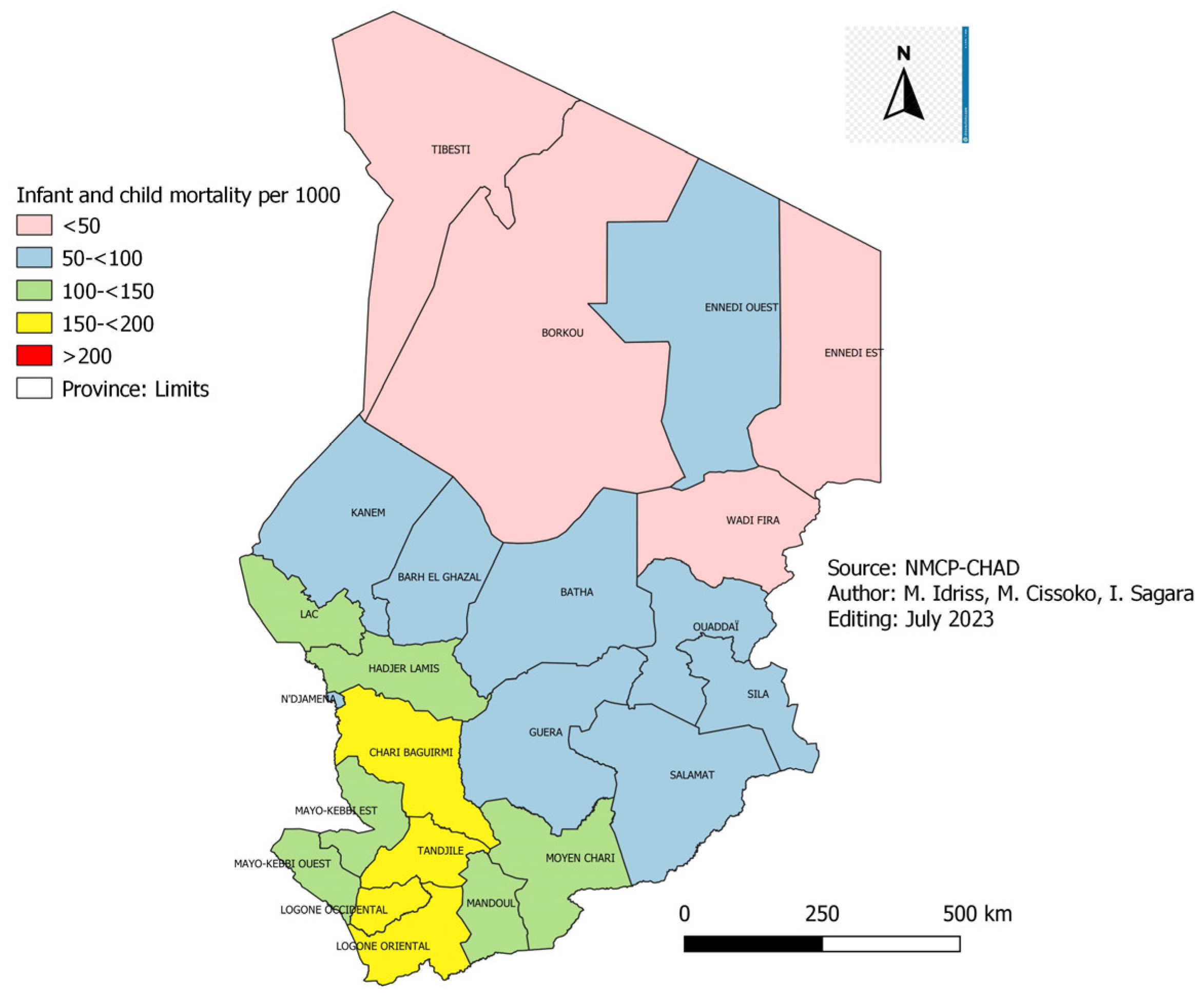
3.9. Infant and Child Mortality
3.10. Weather Factors from 2017 to 2021
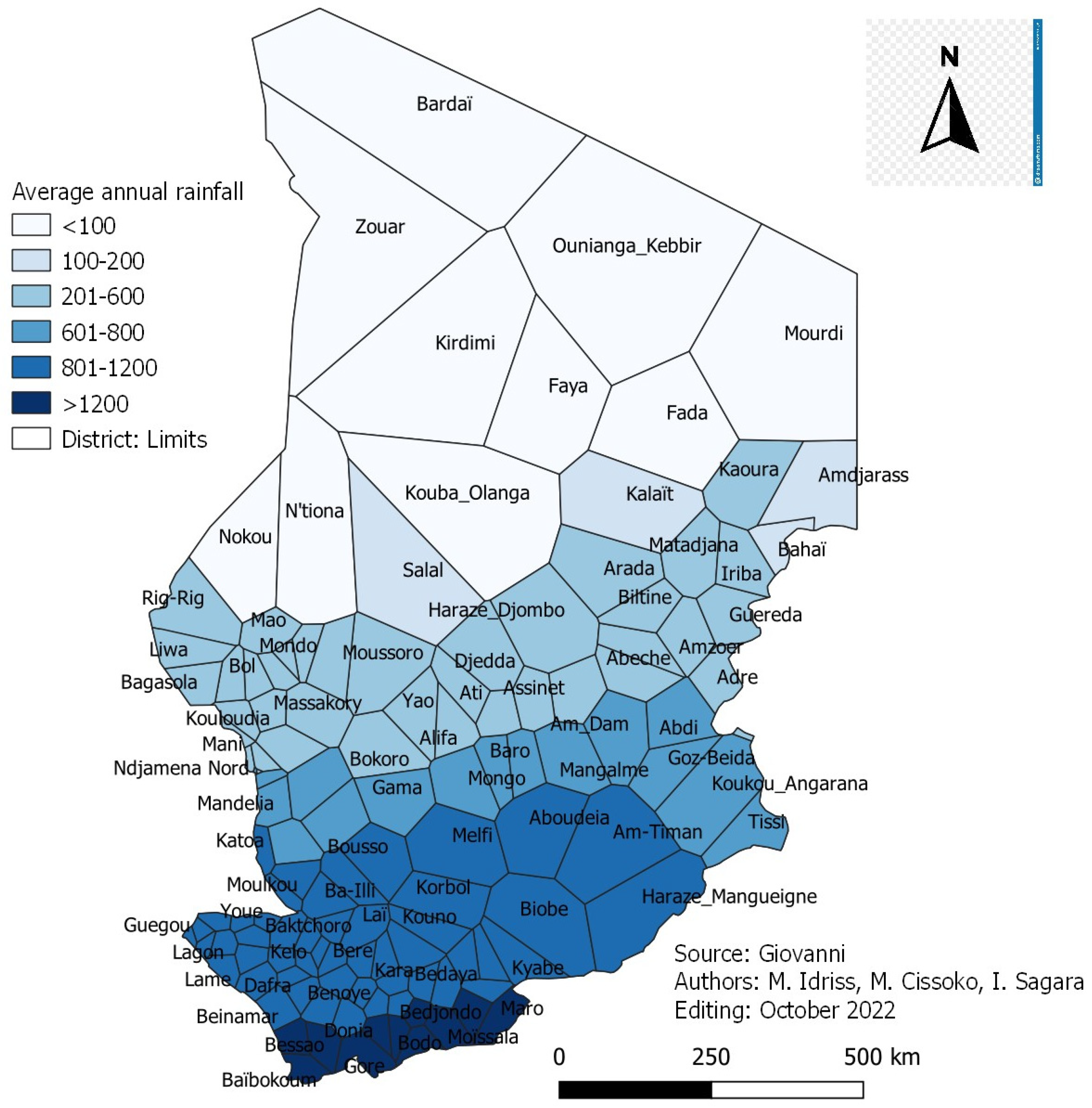
3.10.1. Rainfall Situation by Health District
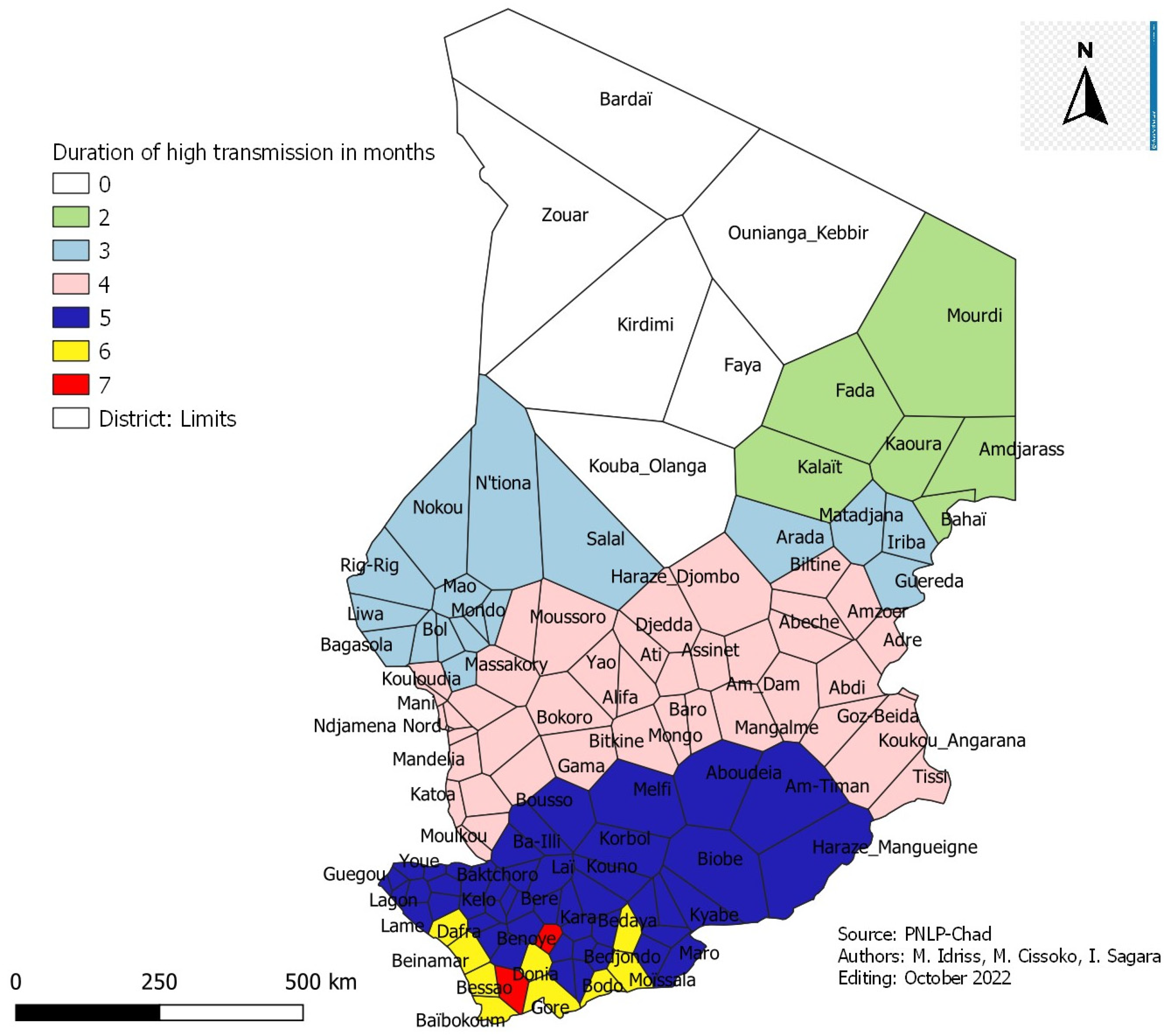
3.10.2. Health Districts and Period of High Transmission
Estimation of Malaria Seasonality in Districts
- -
- Five (5) health districts have two (2) months of high malaria transmission period;
- -
- Nineteen (19) health districts with three (3) months of high malaria transmission period;
- -
- Thirty-two (32) health districts with four (4) months of high malaria transmission period;
- -
- Forty-four (44) health districts have five (5) months of high malaria transmission period;
- -
- Nine (9) health districts have six (6) months of high malaria transmission period;
- -
- Two (2) health districts with seven (7) months of high malaria transmission period.
3.11. Targeting of Interventions by Stratum
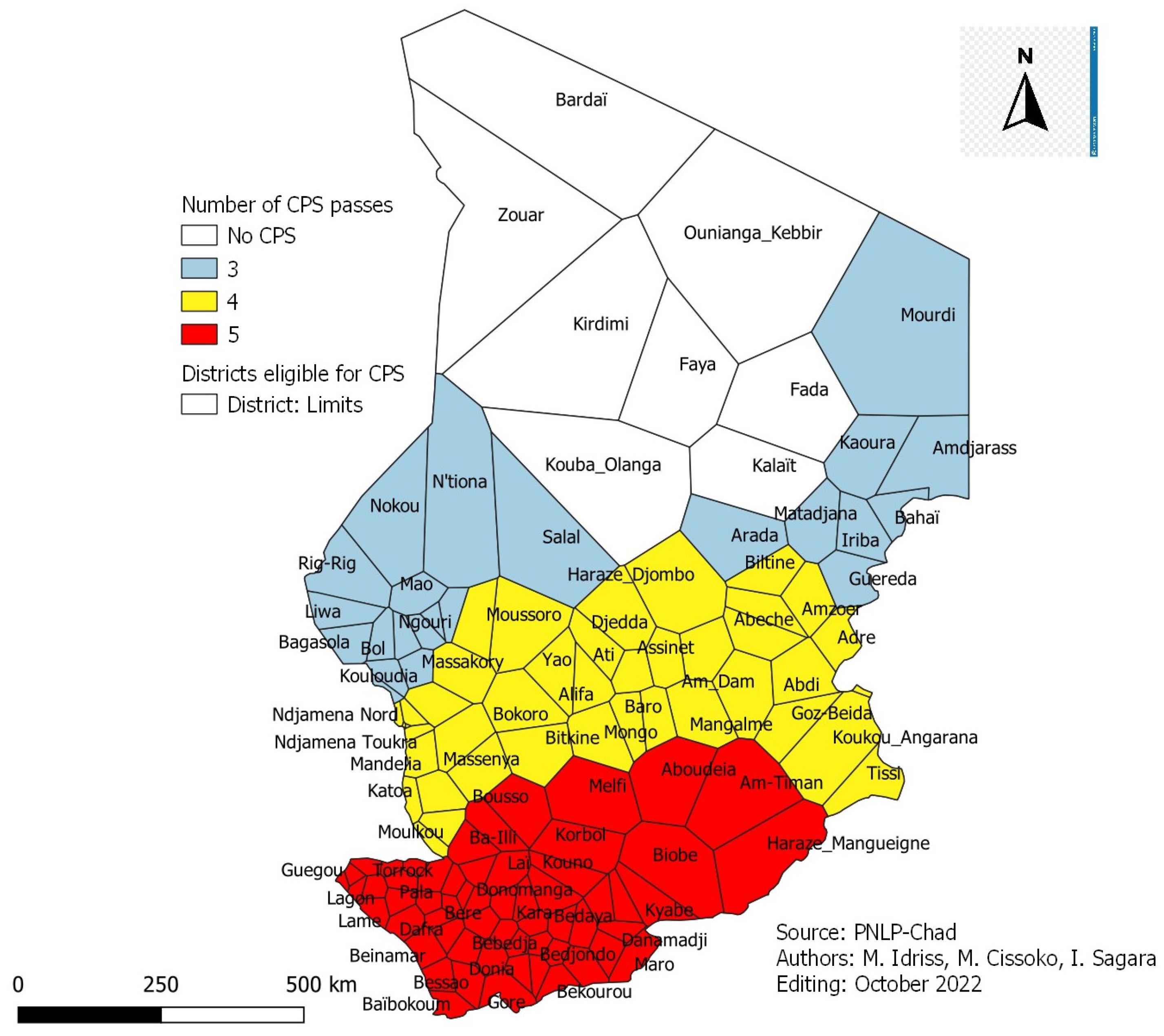
3.12. Health Districts Eligible for SMC and Number of Visits
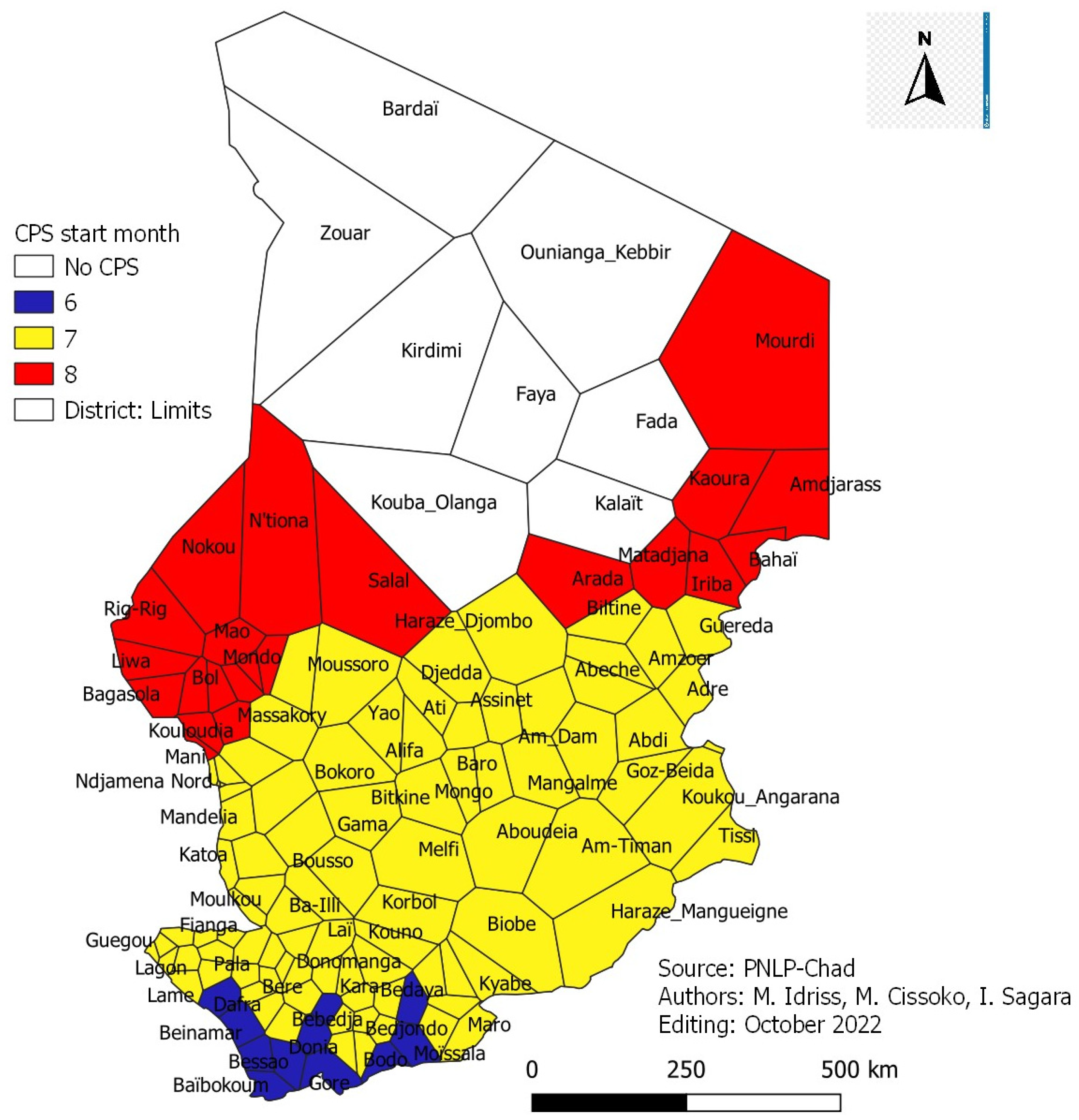
3.13. Districts Eligible for SMC and Start-Up Months
4. Discussion
4.1. Malaria Incidence
4.2. Incidence of Malaria in Children under Five (5) Years Old
4.3. Prevalence of Malaria in Children Aged 6–59 Months Old
4.4. Infant and Child Mortality
4.5. Interventions by Stratum
4.6. Seasonal Malaria Chemoprophylaxis (SMC)
5. Conclusions
6. Ethical Considerations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Vincent, R.; Obert, J.P.; Chippraux, D.L. Malaria in West Africa: Entomological and Epidemiological Studies in Rice-Growing Areas and in Urban Areas; ORSTOM: Paris, France, 1991; Available online: https://horizon.documentation.ird.fr/exl-doc/pleins_textes/pleins_textes_2/etudes_theses/34309.pdf (accessed on 3 October 2022).
- World Health Organization: World Malaria Report: Key Messages. WHO/UCN/GMP/2021; p. 24. Available online: https://cdn.who.int/media/docs/default-source/malaria/world-malaria-reports/world-malaria-report-2021-global-briefing-kit-eng.pdf?sfvrsn=8e5e915_23&download=true (accessed on 3 October 2022).
- Chad National Malaria Control Program, National Institute of Statistics, Economic and Demographic Studies. National Survey on Malaria Indicators in Chad. 2017. Available online: https://www.inseed.td/index.php/blog-with-right-sidebar/communique/155-l-enquete-nationale-sur-les-indicators-du-paludisme-au-tchad-from-2017-SMI-2017 (accessed on 12 October 2022).
- Carnevale, P.; Robert, V.; Boudin, C.; Halna, J.M.; Pazart, L.; Gazin, P.; Richard, A.; Mouchet, J. Control of malaria using mosquito nets impregnated with pyrethroids in Burkina Faso Faso. Bull. Société Pathol. Exot. Fil. 1988, 81, 832–846. [Google Scholar]
- Carnevale, P.; Guillet, P.; Robert, V.; Fontenille, D.; Doannio, J.; Coosemans, M.; Mouchet, J. Diversity of malaria in rice growing areas of the Afrotropical region. Parasitology 1999, 41, 273–276. [Google Scholar]
- Kerah-Hinzoumbé, C.; Péka, M.; Nwane, P.; Donan-Gouni, I.; Etang, J.; Samè-Ekobo, A.; Simard, F. Insecticide resistance in Anopheles gambiae from south-western Chad, Central Africa. Malar. J. 2008, 7, 192. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Framework for Malaria Elimination, 2017, Geneva, License: CC BY-NC-SA 3.0 IGO. Available online: http://apps.who.int/iris.consulted (accessed on 12 October 2022).
- Dumont, G.-F. Geopolitics and Populations in Chad. Overland. In European Review of Geopolitic; Ghazipur Publications: Ghazipur, India, 2008; pp. 263–288. Available online: https://halshs.archives-ouvertes.fr/halshs-00768368/document (accessed on 5 October 2022).
- World Health Organization. Global Technical Strategy for Malaria 2016–2030, 2017, Geneva 27. Available online: https://apps.who.int/iris/bitstream/handle/10665/176720/9789242564990_fre.pdf?sequence=1 (accessed on 5 October 2022).
- US President’s Malaria Initiative Senegal. Malaria Operational Plan FY. 2020. Available online: https://d1u4sg1s9ptc4z.cloudfront.net/uploads/2021/03/fy-2020-senegal-malaria-operational-plan.pdf (accessed on 6 October 2022).
- Ouedraogo, B.; Inoue, Y.; Kambiré, A.; Sallah, K.; Dieng, S.; Tine, R.; Rouamba, T.; Herbreteau, V.; Sawadogo, Y.; Ouedraogo, L.S.L.W.; et al. Spatio-temporal dynamics of malaria in Ouagadougou, Burkina Faso, 2011–2015. Malar. J. 2018, 17, 138. [Google Scholar] [CrossRef] [PubMed]
- Ateba, F.F.; Sagara, I.; Sogoba, N.; Touré, M.; Konaté, D.; Diawara, S.I.; Diakité, S.A.S.; Diarra, A.; Coulibaly, M.D.; Dolo, M.; et al. Spatio-temporal dynamics of malaria incidence: A comparison of two ecological zones in Mali. Int. J. Environ. Res. Public Health 2020, 17, 4698. [Google Scholar] [CrossRef] [PubMed]
- Cissoko, M.; Sagara, I.; Sankaré, M.H.; Dieng, S.; Guindo, A.; Doumbia, Z.; Allasseini, B.; Traore, D.; Fomba, S.; Bendiane, M.K.; et al. Geo-Epidemiology of Malaria at the Health Area Level, Dire Health District, Mali, 2013–2017. Int. J. Environ. Res. Public Health 2020, 17, 3982. [Google Scholar] [CrossRef] [PubMed]
- Abiodun, G.J.; Makinde, O.S.; Adeola, A.M.; Njabo, K.Y.; Witbooi, P.J.; Djidjou-Demasse, R.; Botai, J.O. A Dynamical and Zero-Inflated Negative Binomial Regression Modeling of Malaria Incidence in Limpopo Province, South Africa. Int. J. Environ. Res. Public Health 2019, 16, 2000. [Google Scholar] [CrossRef] [PubMed]
- Rouamba, T.; Nakanabo-Diallo, S.; Derra, K.; Rouamba, E.; Kazienga, A.; Inoue, Y.; Ouédraogo, E.K.; Waongo, M.; Dieng, S.; Guindo, A.; et al. Socioeconomic and environmental factors associated with malaria hotspots in the Nanoro demographic surveillance area, Burkina Faso, 2019. BMC Public Health 2019, 19, 249. [Google Scholar] [CrossRef] [PubMed]
- Andry, H.A.; Emma, R.; Chiarella, M.; Thomas, K.; Dolores, P.; Christophe, R. Dimensions of malaria-related vulnerability in two areas of Madagascar: Contributions of a mixed approach. Pop. Vulnérables 2019, 5, 129–156. [Google Scholar] [CrossRef]
- National Institute of Statistics (INSTAT); Planning and Statistics Unit, Health Sector, Social Development and Family Promotion (SMC/SS-DS-PF); ICF. Mali Demographic and Health Survey 2018: Summary Report; INSTAT, SMC/SSDS-PF: Bamako, Mali; ICF: Rockville, MD, USA, 2019. [Google Scholar]
- National Agency for Statistics and Demography (ANSD) [Senegal]; ICF. Senegal Malaria Indicator Survey, 2020–2021; ANSD and ICF: Rockville, MD, USA, 2021. [Google Scholar]
- National Institute of Statistics and Demography (INSD), Demographic and Health Survey (EDSBF), Burkina Faso in 1993; p.136. Available online: https://www.dhsprogram.com/pubs/pdf/FR53/FR53.pdf (accessed on 6 October 2022).
- Dayananda, K.K.; Achur, R.N.; Gowda, D.C. Epidemiology, drug resistance, and pathophysiology of Plasmodium vivax malaria. J. Vector Borne Dis. 2018, 55, 1–8. [Google Scholar] [PubMed]
- Erdman, L.K.; Kain, K.C. Molecular diagnostic and surveillance tools for global malaria control. Travel. Med. Infect. Dis. 2008, 6, 82–99. [Google Scholar] [CrossRef] [PubMed]
- Tandina, F.; Doumbo, O.; Yaro, A.S.; Traoré, S.F.; Parola, P.; Robert, V. Mosquitoes (Diptera: Culicidae) and mosquito-borne diseases in Mali, West Africa. Parasite Vectors 2018, 11, 467. [Google Scholar] [CrossRef] [PubMed]
- Wagman, J.; Cissé, I.; Kone, D.; Fomba, S.; Eckert, E.; Mihigo, J.; Bankineza, E.; Bah, M.; Diallo, D.; Gogue, C.; et al. Combining next -generation indoor residual spraying and drug-based malaria control strategies: Observational evidence of a combined effect in Mali. Malar. J. 2020, 19, 293. [Google Scholar] [CrossRef] [PubMed]
- Bhavnan, D.; Espinosa, B.G.; Baird, M.; Presley, N.; Menach, A.; Bradley, C.; Outten, M.; Gonzalez, O. Malaria surveillance and case management in remote and indigenous communities in Panama: Results of a community health worker pilot project. Malar. J. 2022, 21, 297. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.A.; Jones, C.O. A critical review of behavioral issues related to malaria control in sub-Saharan Africa: What contributions have social scientists made? Soc. Sci. Med. 2004, 59, 501–523. [Google Scholar] [CrossRef] [PubMed]
- Cisse, A. Effect of a 5th Round of Chemoprevention of Seasonal Malaria in Children Aged 5–14 Years in the Village of Dangassa, Health District of Ouelessebougou in Mali. Ph.D. Thesis, Université des Sciences, des Techniques et des Technologies de Bamako, Bamako, Mali, 2021. Available online: https://www.bibliosante.ml/handle/123456789/5453 (accessed on 3 November 2022).
- World Health Organization: Seasonal Malaria Chemoprevention to Control Plasmodium Falciparum Malaria in Areas of High Seasonal Transmission in the Sahel Subregion of Africa. 2021. Available online: https://www.malariaconsortium.org/mediadownloads/218/Chimiopr%C3%A9vention%20of%20seasonal%20malaria (accessed on 3 November 2022).
- World Health Organization: Optimizing the Impact of Seasonal Malaria Chemoprevention: Improving Delivery and Building Capacity for Evaluation (OPT-SMC). 2022. Available online: https://mesamalaria.org/mesa-track/optimizing-impact-seasonal-malaria-chemoprevention-improving-delivery-and-building (accessed on 3 November 2022).
| Strata | Incidence Level | Interventions |
|---|---|---|
| Very low transmission | Incidence <10 cases per 1000 | Case management, passive case detection, Active case detection, IPTp, Routine LLINs, IRS, Survence |
| Incidence between 10 and <50 cases per 1000 | Case management, IPTp, Routine LLINs, IRS: Reponse to epidemics | |
| Incedence between 50 and <100 cases per 1000 | Case management, IPTp, Routine and campaign LLINs, IRS: Reponse to epidemics, SMC | |
| Low transmission | Incidence between 100 and <250 cases per 1000 | Case management, IPTp, Routine and campaign LLIN-PBO, SMC, IRS: Reponse to epidemics |
| Moderate transmission | Incidence between 250 and <450 cases per 1000 | Case management, iCCM, IPTp, Routine and campaign LLIN-PBO, SMC |
| Strong transmission | Incidence greater than 450 cases per 1000 | Case management, iCCM, IPTp, Routine and campaign LLIN-PBO, SMC, IRS |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Djaskano, M.I.; Cissoko, M.; Diar, M.S.I.; Israel, D.K.; Clément, K.H.; Ali, A.M.; Dormbaye, M.; Souleymane, I.M.; Batrane, A.; Sagara, I. Stratification and Adaptation of Malaria Control Interventions in Chad. Trop. Med. Infect. Dis. 2023, 8, 450. https://doi.org/10.3390/tropicalmed8090450
Djaskano MI, Cissoko M, Diar MSI, Israel DK, Clément KH, Ali AM, Dormbaye M, Souleymane IM, Batrane A, Sagara I. Stratification and Adaptation of Malaria Control Interventions in Chad. Tropical Medicine and Infectious Disease. 2023; 8(9):450. https://doi.org/10.3390/tropicalmed8090450
Chicago/Turabian StyleDjaskano, Mahamat Idriss, Mady Cissoko, Mahamat Saleh Issakha Diar, Demba Kodindo Israel, Kerah Hinzoumbé Clément, Aicha Mohamed Ali, Makido Dormbaye, Issa Mahamat Souleymane, Adam Batrane, and Issaka Sagara. 2023. "Stratification and Adaptation of Malaria Control Interventions in Chad" Tropical Medicine and Infectious Disease 8, no. 9: 450. https://doi.org/10.3390/tropicalmed8090450
APA StyleDjaskano, M. I., Cissoko, M., Diar, M. S. I., Israel, D. K., Clément, K. H., Ali, A. M., Dormbaye, M., Souleymane, I. M., Batrane, A., & Sagara, I. (2023). Stratification and Adaptation of Malaria Control Interventions in Chad. Tropical Medicine and Infectious Disease, 8(9), 450. https://doi.org/10.3390/tropicalmed8090450







