Trend of Human Schistosomiasis Japonica Prevalence in China from 1990 to 2019
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population
2.3. Data Source
2.4. Statistical Analysis
3. Results
3.1. Prevalence of Schistosomiasis in 2019
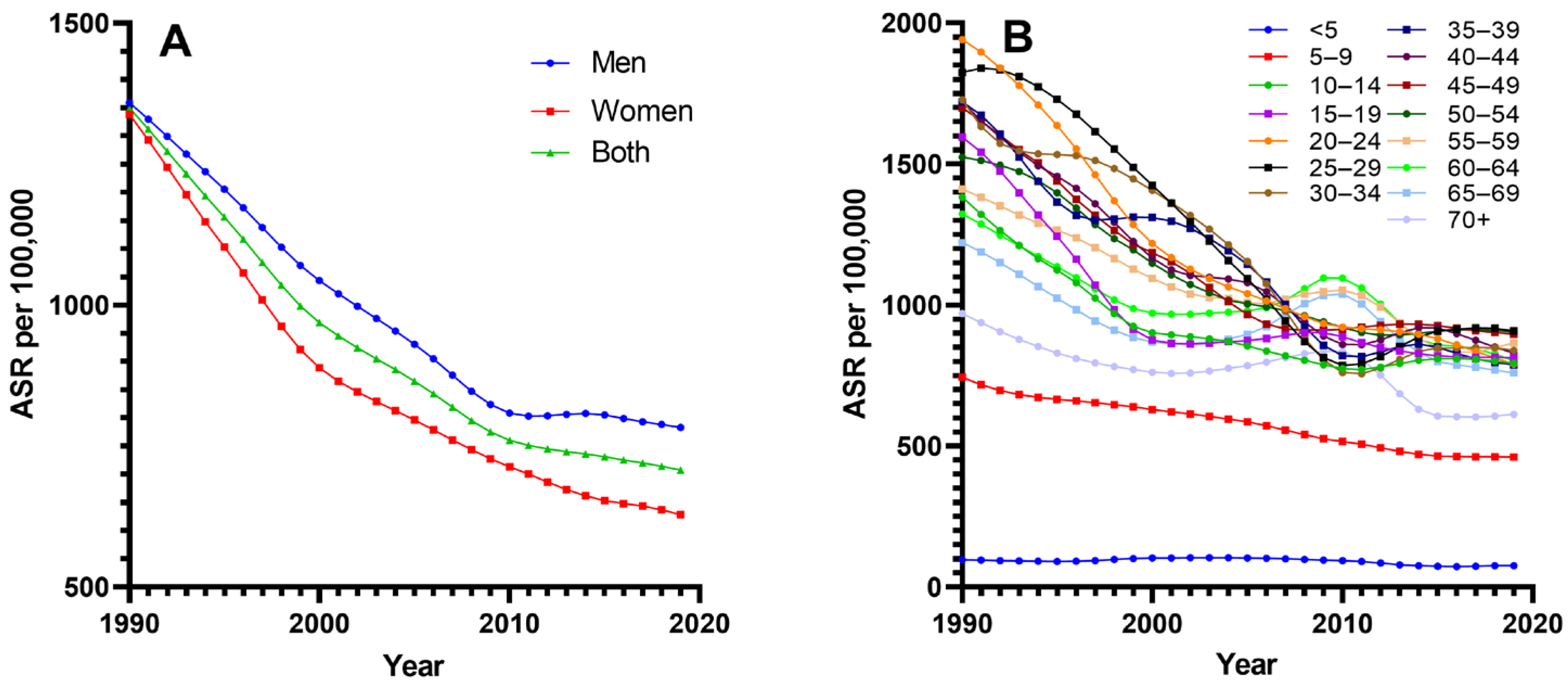
3.2. Trends in Prevalence of Schistosomiasis
3.3. Correlation between ASR and Socioeconomic, Sanitation Parameters
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ogongo, P.; Nyakundi, R.K.; Chege, G.K.; Ochola, L. The Road to Elimination: Current State of Schistosomiasis Research and Progress Towards the End Game. Front. Immunol. 2022, 13, 846108. [Google Scholar] [CrossRef] [PubMed]
- McManus, D.P.; Bergquist, R.; Cai, P.; Ranasinghe, S.; Tebeje, B.M.; You, H. Schistosomiasis—From Immunopathology to Vaccines. Semin. Immunopathol. 2020, 42, 355–371. [Google Scholar] [CrossRef] [PubMed]
- Gryseels, B.; Polman, K.; Clerinx, J.; Kestens, L. Human Schistosomiasis. Lancet 2006, 368, 1106–1118. [Google Scholar] [CrossRef] [PubMed]
- Wiegand, R.E.; Fleming, F.M.; de Vlas, S.J.; Odiere, M.R.; Kinung’hi, S.; King, C.H.; Evans, D.; French, M.D.; Montgomery, S.P.; Straily, A.; et al. Defining Elimination as a Public Health Problem for Schistosomiasis Control Programmes: Beyond Prevalence of Heavy-Intensity Infections. Lancet Glob. Health 2022, 10, e1355–e1359. [Google Scholar] [CrossRef] [PubMed]
- Colley, D.G.; Bustinduy, A.L.; Secor, W.E.; King, C.H. Human Schistosomiasis. Lancet 2014, 383, 2253–2264. [Google Scholar] [CrossRef]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990–2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- King, C.H.; Dickman, K.; Tisch, D.J. Reassessment of the Cost of Chronic Helmintic Infection: A Meta-Analysis of Disability-Related Outcomes in Endemic Schistosomiasis. Lancet 2005, 365, 1561–1569. [Google Scholar] [CrossRef]
- Utzinger, J.; Raso, G.; Brooker, S.; De Savigny, D.; Tanner, M.; Ornbjerg, N.; Singer, B.H.; N’goran, E.K. Schistosomiasis and Neglected Tropical Diseases: Towards Integrated and Sustainable Control and a Word of Caution. Parasitology 2009, 136, 1859–1874. [Google Scholar] [CrossRef]
- McManus, D.P.; Dunne, D.W.; Sacko, M.; Utzinger, J.; Vennervald, B.J.; Zhou, X.-N. Schistosomiasis. Nat. Rev. Dis. Primers 2018, 4, 13. [Google Scholar] [CrossRef]
- Zhou, X.-N.; Wang, L.-Y.; Chen, M.-G.; Wu, X.-H.; Jiang, Q.-W.; Chen, X.-Y.; Zheng, J.; Utzinger, J. The Public Health Significance and Control of Schistosomiasis in China—Then and Now. Acta Trop. 2005, 96, 97–105. [Google Scholar] [CrossRef]
- Zhou, Y.; Chen, Y.; Jiang, Q. History of Human Schistosomiasis (Bilharziasis) in China: From Discovery to Elimination. Acta Parasitol. 2021, 66, 760–769. [Google Scholar] [CrossRef]
- Qian, M.-B.; Chen, J.; Bergquist, R.; Li, Z.-J.; Li, S.-Z.; Xiao, N.; Utzinger, J.; Zhou, X.-N. Neglected Tropical Diseases in the People’s Republic of China: Progress towards Elimination. Infect. Dis. Poverty 2019, 8, 86. [Google Scholar] [CrossRef]
- Zhang, L.J.; Xu, Z.M.; Yang, F.; He, J.Y.; Dang, H.; Li, Y.L.; Cao, C.L.; Xu, J.; Li, S.Z.; Zhou, X.N. Progress of schistosomiasis control in People’s Republic of China in 2021. Chin. J. Schistosomasis Control 2022, 34, 329–336. [Google Scholar] [CrossRef]
- Abe, E.M.; Tambo, E.; Xue, J.; Xu, J.; Ekpo, U.F.; Rollinson, D.; Yang, K.; Li, S.-Z.; Zhou, X.-N. Approaches in Scaling up Schistosomiasis Intervention towards Transmission Elimination in Africa: Leveraging from the Chinese Experience and Lessons. Acta Trop. 2020, 208, 105379. [Google Scholar] [CrossRef]
- Feng, J.; Zhang, X.; Hu, H.; Gong, Y.; Luo, Z.; Xue, J.; Cao, C.; Xu, J.; Li, S. Spatiotemporal Distribution of Schistosomiasis Transmission Risk in Jiangling County, Hubei Province, P.R. China. PLoS Negl. Trop. Dis. 2023, 17, e0011265. [Google Scholar] [CrossRef]
- Xiao, Y.; Zhong, C.H.; Wei, F.H.; Dai, L.F.; Yang, J.J.; Chen, Y.Y. Epidemiological trends for human schistosomiasis prevalence in Hubei Province from 2004 to 2018 based on Joinpoint regression analysis. Chin. J. Schistosomasis Control 2022, 34, 122–127. [Google Scholar] [CrossRef]
- Wu, X.H.; Wu, J.; Xu, R.M.; Xiong, Y.; Chen, Z. Epidemiological trends of schistosomiasis in Poyang county of Jiangxi Province from 2004 to 2020 based on the Joinpoint regression model. Chin. J. Schistosomasis Control 2022, 34, 7–15. [Google Scholar] [CrossRef]
- Li, F.Y.; Tan, H.Z.; Ren, G.H.; Jiang, Q.; Wang, H.L. Research of prevalence of schistosomiasis in Hu Nan province, 1984–2015. Chin. J. Epidemiol. 2017, 38, 350–353. [Google Scholar]
- Zhou, X.N.; Wang, T.P.; Wang, L.Y.; Guo, J.G.; Yu, Q.; Xu, J.; Wang, R.B.; Chen, C.; Jia, T.W. The current states of schistosomiasis epidemics in China. Chin. J. Epidemiol. 2004, 25, 9–12. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, Regional, and National Age-Sex-Specific Mortality for 282 Causes of Death in 195 Countries and Territories, 1980–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Kim, H.J.; Chen, H.S.; Byrne, J.; Wheeler, B.; Feuer, E.J. Twenty years since Joinpoint 1.0: Two major enhancements, their justification, and impact. Stat. Med. 2022, 41, 3102–3130. [Google Scholar] [CrossRef] [PubMed]
- Vrieze, S.I. Model selection and psychological theory: A discussion of the differences between the Akaike information criterion (AIC) and the Bayesian information criterion (BIC). Psychol. Methods 2012, 17, 228–243. [Google Scholar] [CrossRef] [PubMed]
- Clegg, L.X.; Hankey, B.F.; Tiwari, R.; Feuer, E.J.; Edwards, B.K. Estimating average annual percent change in trend analysis. Stat. Med. 2009, 28, 3670–3678. [Google Scholar]
- Kim, H.; Fay, M.; Feuer, E.; Midthurne, D. Permutation Tests for Joinpoint Regression with Applications to Cancer Rates. Stat. Med. 2000, 19, 335–351. [Google Scholar] [CrossRef]
- The Central Committee of the Communist Party of China and the State Council Issued “Healthy China 2030” Program, Relevant Documents of the Central Government, Chinese Government Website. Available online: http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (accessed on 22 May 2023).
- Lin, D.D.; Wu, H.W.; Wu, G.L.; Zhou, X.N. Review and evaluation on optimal combined strategies for schistosomiasis control in China. Chin. J. Schistosomasis Control 2007, 234–237. [Google Scholar] [CrossRef]
- Li, Y.F.; Lin, D.D. Process and prospect of schistosomiasis control in Jiangxi Province. J. Trop. Dis. Parasitol. 2019, 17, 125–130. [Google Scholar] [CrossRef]
- Luo, T.P.; Li, Y.L.; Zhang, X.Q.; Fang, W. Evaluation on world band load schistosomiasis control programme in Yunnan province from 1992–2000. Chin. J. Schistosomasis Control 2002, 85, 142–143. [Google Scholar] [CrossRef]
- Cai, K.P.; Li, Y.Y.; Li, X.Y.; Jiang, Q. Effectiveness of world bank loan schistosomiasis control project in 9 years, in Hunan province. Chin. J. Schistosomasis Control 2003, 30, 41–44. [Google Scholar] [CrossRef]
- Wang, R.B.; Wang, T.P.; Wang, L.Y.; Guo, J.G.; Yu, Q.; Xu, J.; Gao, F.H.; Yin, Z.C.; Zhou, X.N. Study on the re-emerging situation of schistosomiasis epidemics in areas already under control and interruption. Chin. J. Epidemiol. 2004, 25, 18–21. [Google Scholar] [CrossRef]
- Lin, D.D.; Hu, F.; Liu, Y.M.; Chen, H.G. Analysis of Schistosomiasis Epidemic Situation after World Bank Loan in Poyang Lake District and Its Control Countermeasures. Chin. J. Epidemiol. 2004, 25, 33–35. [Google Scholar] [CrossRef]
- Wang, L.-D.; Chen, H.-G.; Guo, J.-G.; Zeng, X.-J.; Hong, X.-L.; Xiong, J.-J.; Wu, X.-H.; Wang, X.-H.; Wang, L.-Y.; Xia, G.; et al. A Strategy to Control Transmission of Schistosomasis Japonicum in China. N. Engl. J. Med. 2009, 360, 121–128. [Google Scholar] [CrossRef]
- Li, Y.F.; Hang, C.Q.; Hu, F.; Yuan, M.; Gu, X.N.; Lu, S.B.; Zeng, X.J.; Lin, D.D. Role of new strategy in transmission control of schistosomiasis in Poyang Lake region. Chin. J. Schistosomasis Control 2017, 29, 689–694. [Google Scholar] [CrossRef]
- Wang, L.D.; Zhou, X.N.; Chen, H.G.; Guo, J.G.; Zeng, X.J.; Hong, X.L.; Xiong, J.J.; Wu, X.H.; Wang, L.Y.; Xia, G.; et al. A new strategy to control transmission of Schistosomasis japonicum. Strateg. Study CAE 2009, 11, 37–43. [Google Scholar] [CrossRef]
- Li, H.M.; Zheng, J.X.; Qian, Y.J.; Lv, S.; Xia, S.; Zhou, X.N. Comparison of the disease burden of schistosomiasis globally and in China and Zimbabwe. Chin. J. Schistosomasis Control 2023, 35, 128–154. [Google Scholar] [CrossRef]
- LoVerde, P.T. Schistosomiasis. Adv. Exp. Med. Biol. 2019, 1154, 45–70. [Google Scholar] [CrossRef]
- Dong, X.Q.; Feng, X.G.; Dong, Y.; Xiong, M.T.; Jiang, H.; Shen, M.F.; Zhang, Y.; Yang, G.C.; Shao, Z.T.; Wu, X. Epidemiological characteristics and control strategies of schistosomiasis in mountainous areas of Yunnan Province. Chin. J. Schistosomasis Control 2008, 20, 135–137. [Google Scholar] [CrossRef]
- Kloos, H. Human Behavior, Health education and schistosomiasis control: A Review. Soc. Sci. Med. 1995, 40, 1497–1511. [Google Scholar] [CrossRef]
- He, J.C.; Zheng, B.Q.; Fang, G.R.; Wan, S.K.; Zhang, X.G.; Xia, C.G.; Wang, Q.Z.; Dong, X.Z.; Wu, W.Z.; Ge, J.H. Evaluation on the cost-effectiveness of two chemotherapy strategies for schistosomiasis control in medium endemic area. Chin. J. Parasit. Dis. Con. 2000, 13, 55–58. [Google Scholar] [CrossRef]
- Feng, J.X.; Gong, Y.F.; Luo, Z.W.; Wang, X.Y.; Cao, C.L.; Zhang, X.; Zhang, J.F.; Li, H.R.; Hu, H.H.; Xu, J.; et al. A survey on the current situation of schistosomiasis prevention and control knowledge and belief among adults in Jiangling county. Mod. Prev. Med. 2022, 49, 3426–3430. [Google Scholar] [CrossRef]
- Engels, D.; Zhou, X.-N. Neglected Tropical Diseases: An Effective Global Response to Local Poverty-Related Disease Priorities. Infect. Dis. Poverty 2020, 9, 10. [Google Scholar] [CrossRef]
- Zheng, J. Achievements and challenges in schistosomiasis control in China. Chin. J. Parasitol. Parasit. Dis. Oct. 2009, 27, 398–401. [Google Scholar]
- Wang, L.D. The key to controlling the prevalence of schistosomiasis in China is to manage human and animal faeces well. Chin. J. Epidemiol. 2005, 26, 929–930. [Google Scholar] [CrossRef]
- Miranda, G.S.; Rodrigues, J.G.M.; Silva, J.K.A.d.O.; Camelo, G.M.A.; Silva-Souza, N.; Neves, R.H.; Machado-Silva, J.R.; Negrão-Corrêa, D.A. New Challenges for the Control of Human Schistosomiasis: The Possible Impact of Wild Rodents in Schistosomasis Mansoni Transmission. Acta Trop. 2022, 236, 106677. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | ASR (95% UI), 1990 | ASR (95% UI), 2019 | Change Value, 1990–2019 | Change Percentage, 1990–2019 | |
|---|---|---|---|---|---|
| Total | 1349.55 (1146.35–1903.31) | 707.09 (621.43–929.13) | 642.46 (524.92–974.18) | 47.61 (45.79–51.18) | |
| Sex | male | 1358.67 (1150.60–1919.85) | 782.99 (685.74–1031.48) | 575.68 (464.87–888.37) | 42.37 (40.40–46.27) |
| female | 1338.43 (1142.10–1893.13) | 628.37 (555.40–808.37) | 710.07 (586.71–1084.76) | 53.05 (51.37–57.30) | |
| Age | <5 | 97.30 (42.84–195.48) | 75.19 (50.47–109.37) | 22.11 (−7.63–86.11) | 22.72 (−17.80–44.05) |
| 5–9 | 743.28 (470.16–1177.23) | 461.00 (330.97–620.99) | 282.29 (139.19–556.24) | 37.98 (29.60–47.25) | |
| 10–14 | 1381.90 (898.55–2049.57) | 793.04 (582.94–1062.67) | 588.86 (315.60–986.90) | 42.61 (35.12–48.15) | |
| 15–19 | 1594.78 (1060.00–2312.52) | 813.74 (616.87–1113.20) | 781.04 (443.13–1199.31) | 48.97 (41.80–51.86) | |
| 20–24 | 1940.93 (1395.68–2835.54) | 790.77 (600.24–1063.67) | 1150.16 (795.44–1771.87) | 59.26 (56.99–62.49) | |
| 25–29 | 1824.70 (1402.95–2591.64) | 907.46 (708.06–1187.07) | 917.24 (694.89–1404.57) | 50.27 (49.53–54.20) | |
| 30–34 | 1727.47 (1287.28–2426.92) | 839.54 (656.00–1114.66) | 887.94 (631.28–1312.26) | 51.40 (49.04–54.07) | |
| 35–39 | 1719.96 (1395.59–2428.44) | 788.68 (637.94–1050.40) | 931.28 (757.65–1378.03) | 54.15 (54.29–56.75) | |
| 40–44 | 1719.72 (1349.48–2498.32) | 829.23 (656.49–1103.03) | 890.49 (692.99–1395.29) | 51.78 (51.35–55.85) | |
| 45–49 | 1698.29 (1389.96–2385.33) | 895.87 (744.42–1168.40) | 802.42 (645.54–1216.93) | 47.25 (46.44–51.02) | |
| 50–54 | 1524.51 (1260.89–2118.96) | 904.08 (762.07–1170.62) | 620.42 (498.82–948.35) | 40.70 (39.56–44.76) | |
| 55–59 | 1411.01 (1096.41–1944.08) | 865.09 (702.68–1140.23) | 545.92 (393.73–803.85) | 38.69 (35.91–41.35) | |
| 60–64 | 1323.04 (1000.82–1819.36) | 801.92 (634.73–1048.41) | 521.12 (366.09–770.95) | 39.39 (36.58–42.37) | |
| 65–69 | 1220.82 (980.84–1731.00) | 759.47 (631.25–986.80) | 461.35 (349.60–744.20) | 37.79 (35.64–42.99) | |
| 70+ | 969.16 (770.83–1382.70) | 612.94 (512.32–807.15) | 356.22 (258.51–575.55) | 36.76 (33.54–41.62) | |
| Characteristics | Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | Trend 6 | Full Range | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | Years | APC | AAPC | ||
| Total | 1990–1994 | −2.99 * | 1994–2000 | −3.50 * | 2000–2004 | −2.14 * | 2004–2010 | −2.59 * | 2010–2019 | −0.73 * | −2.20 * | |||
| Sex | male | 1990–1995 | −2.35 * | 1995–1999 | −2.99 * | 1999–2005 | −2.30 * | 2005–2010 | −2.92 * | 2010–2014 | 0.20 * | 2014–2019 | −0.63 * | −1.89 * |
| female | 1990–1994 | −3.75 * | 1994–2000 | −4.29 * | 2000–2010 | −2.13 * | 2010–2014 | −1.88 * | 2014–2019 | −0.96 * | −2.57 * | |||
| Age | <5 | 1990–1995 | −1.58 * | 1995–2000 | 2.83 * | 2000–2005 | 0.17 | 2005–2010 | −2.04 * | 2010–2015 | −5.12 * | 2015–2019 | 1.11 * | −0.87 * |
| 5–9 | 1990–1993 | −2.84 * | 1993–1998 | −0.96 * | 1998–2005 | −1.37 * | 2005–2009 | −2.70 * | 2009–2015 | −2.12 * | 2015–2019 | −0.08 | −1.62 * | |
| 10–14 | 1990–1996 | −4.00 * | 1996–1999 | −5.14 * | 1999–2005 | −1.16 * | 2005–2010 | −2.16 * | 2010–2015 | 1.08 * | 2015–2019 | −0.46 * | −1.87 * | |
| 15–19 | 1990–1994 | −4.57 * | 1994–2000 | −7.10 * | 2000–2009 | 0.54 * | 2009–2014 | −1.78 * | 2014–2019 | −0.25 | −2.33 * | |||
| 20–24 | 1990–1995 | −3.34 * | 1995–2000 | −6.00 * | 2000–2003 | −3.37 * | 2003–2009 | −2.57 * | 2009–2015 | −0.92 * | 2015–2019 | −2.78 * | −3.08 * | |
| 25–29 | 1990–1995 | −0.99 * | 1995–2003 | −4.25 * | 2003–2010 | −6.64 * | 2010–2015 | 3.50 * | 2015–2019 | 0.02 | −2.40 * | |||
| 30–34 | 1990–1992 | −4.78 * | 1992–1998 | −0.64 * | 1998–2005 | −3.49 * | 2005–2010 | −8.73 * | 2010–2015 | 2.77 * | 2015–2019 | −0.24 | −2.43 * | |
| 35–39 | 1990–1996 | −4.65 * | 1996–2001 | −0.07 | 2001–2005 | −3.08 * | 2005–2010 | −6.88 * | 2010–2014 | 1.68 * | 2014–2019 | −1.90 * | −2.72 * | |
| 40–44 | 1990–1997 | −3.24 * | 1997–2001 | −4.82 * | 2001–2005 | −0.61 * | 2005–2010 | −4.72 * | 2010–2015 | 1.60 * | 2015–2019 | −2.71 * | −2.47 * | |
| 45–49 | 1990–1994 | −3.02 * | 1994–1998 | −4.33 * | 1998–2001 | −3.02 * | 2001–2007 | −3.95 * | 2007–2014 | 0.49 * | 2014–2019 | −0.88 * | −2.19 * | |
| 50–54 | 1990–1994 | −1.37 * | 1994–2002 | −3.78 * | 2002–2012 | −1.76 * | 2012–2017 | 0.54 * | 2017–2019 | −0.6 | −1.80 * | |||
| 55–59 | 1990–1996 | −2.18 * | 1996–2002 | −2.92 * | 2002–2005 | −0.81 | 2005–2011 | 0.65 * | 2011–2015 | −5.59 * | 2015–2019 | 0.64 * | −1.71 * | |
| 60–64 | 1990–2000 | −3.19 * | 2000–2006 | 0.44 * | 2006–2010 | 3.18 * | 2010–2014 | −5.78 * | 2014–2019 | −1.72 * | −1.70 * | |||
| 65–69 | 1990–2000 | −3.56 * | 2000–2004 | 0.59 | 2004–2010 | 3.15 * | 2010–2015 | −5.52 * | 2015–2019 | −1.04 * | −1.64 * | |||
| 70+ | 1990–1997 | −2.86 * | 1997–2002 | −0.87 * | 2002–2010 | 1.53 * | 2010–2015 | −6.76 * | 2015–2019 | 0.47 * | −1.56 * | |||
| Time Periods | Index | ASR | |
|---|---|---|---|
| r | p Value | ||
| 1990–2019 | GDP | −0.799 ** | <0.01 |
| PPMS | −0.892 ** | <0.01 | |
| 1990–1999 | GDP | −0.978 ** | <0.01 |
| PPMS | NA | - | |
| 2000–2009 | GDP | −0.956 ** | <0.01 |
| PPMS | −0.985 ** | <0.01 | |
| 2010–2019 | GDP | −0.991 ** | <0.01 |
| PPMS | −0.994 ** | <0.01 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; He, T.; Xie, J.; Lv, S.; Li, Z.; Yuan, M.; Hu, F.; Lin, D. Trend of Human Schistosomiasis Japonica Prevalence in China from 1990 to 2019. Trop. Med. Infect. Dis. 2023, 8, 344. https://doi.org/10.3390/tropicalmed8070344
Li Y, He T, Xie J, Lv S, Li Z, Yuan M, Hu F, Lin D. Trend of Human Schistosomiasis Japonica Prevalence in China from 1990 to 2019. Tropical Medicine and Infectious Disease. 2023; 8(7):344. https://doi.org/10.3390/tropicalmed8070344
Chicago/Turabian StyleLi, Yifeng, Tingting He, Jingzi Xie, Shangbiao Lv, Zongguang Li, Min Yuan, Fei Hu, and Dandan Lin. 2023. "Trend of Human Schistosomiasis Japonica Prevalence in China from 1990 to 2019" Tropical Medicine and Infectious Disease 8, no. 7: 344. https://doi.org/10.3390/tropicalmed8070344
APA StyleLi, Y., He, T., Xie, J., Lv, S., Li, Z., Yuan, M., Hu, F., & Lin, D. (2023). Trend of Human Schistosomiasis Japonica Prevalence in China from 1990 to 2019. Tropical Medicine and Infectious Disease, 8(7), 344. https://doi.org/10.3390/tropicalmed8070344







