Nanobody-Based Blocking of Binding ELISA for the Detection of Anti-NS1 Zika-Virus-Specific Antibodies in Convalescent Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Evaluation of Direct ELISA for Antibodies Detection of Flavivirus Immune Sera
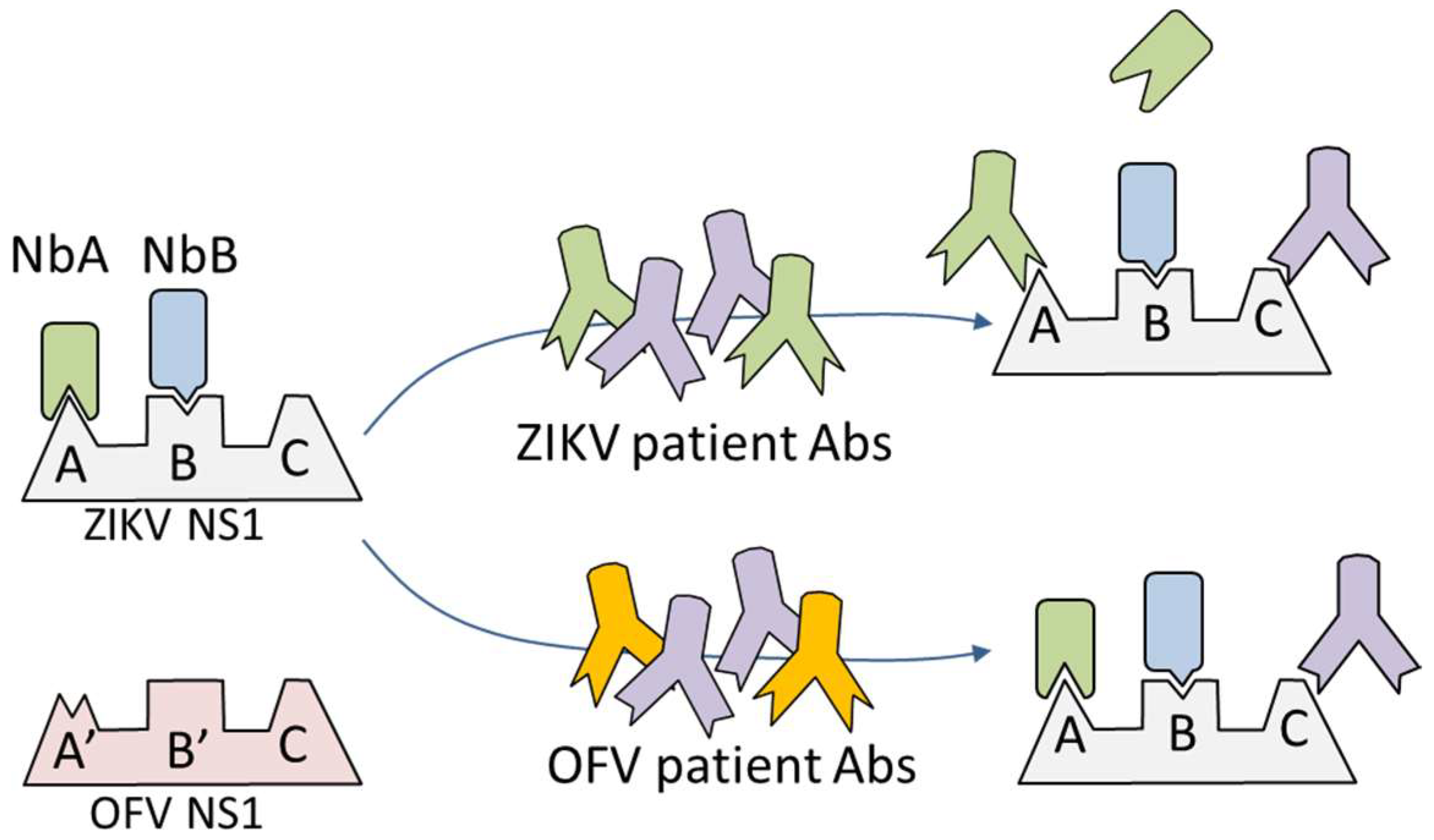
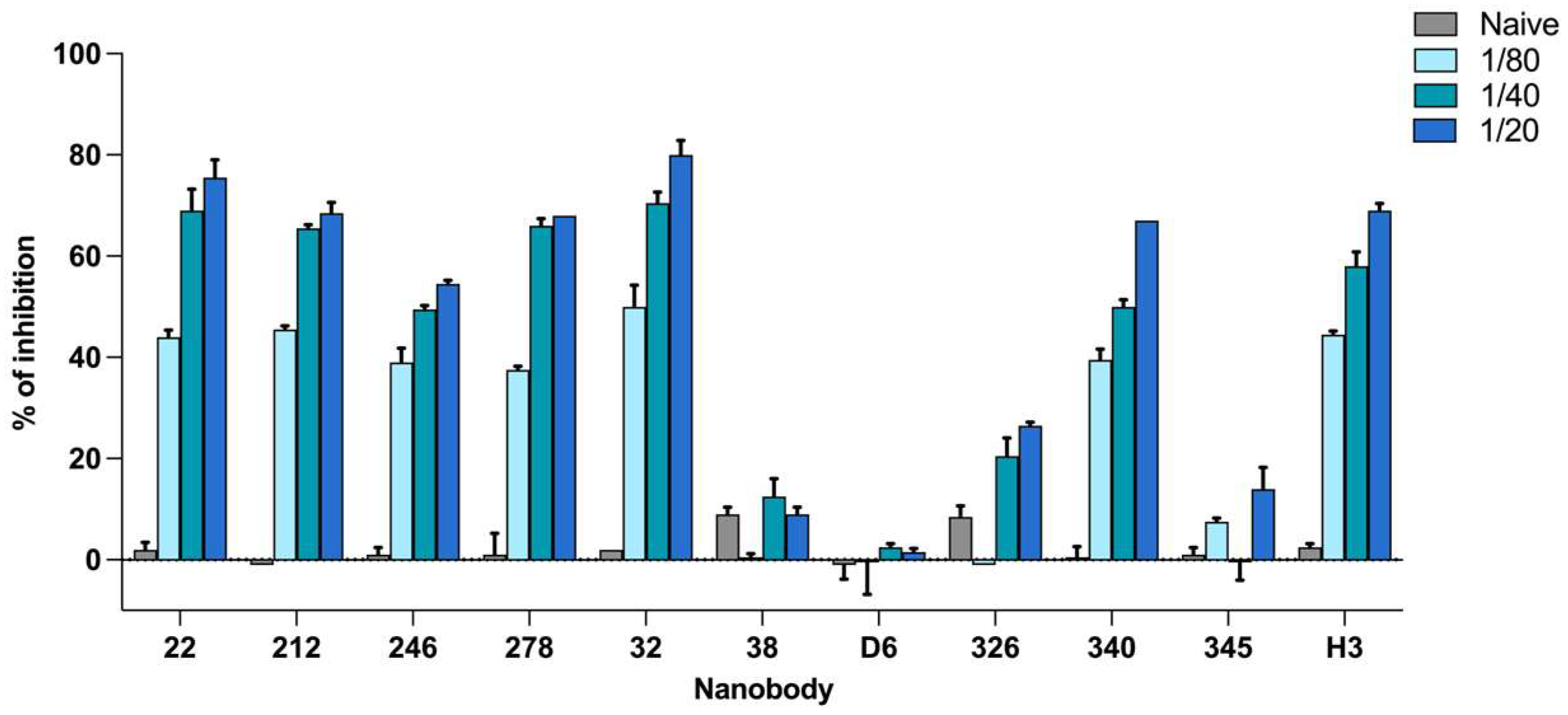
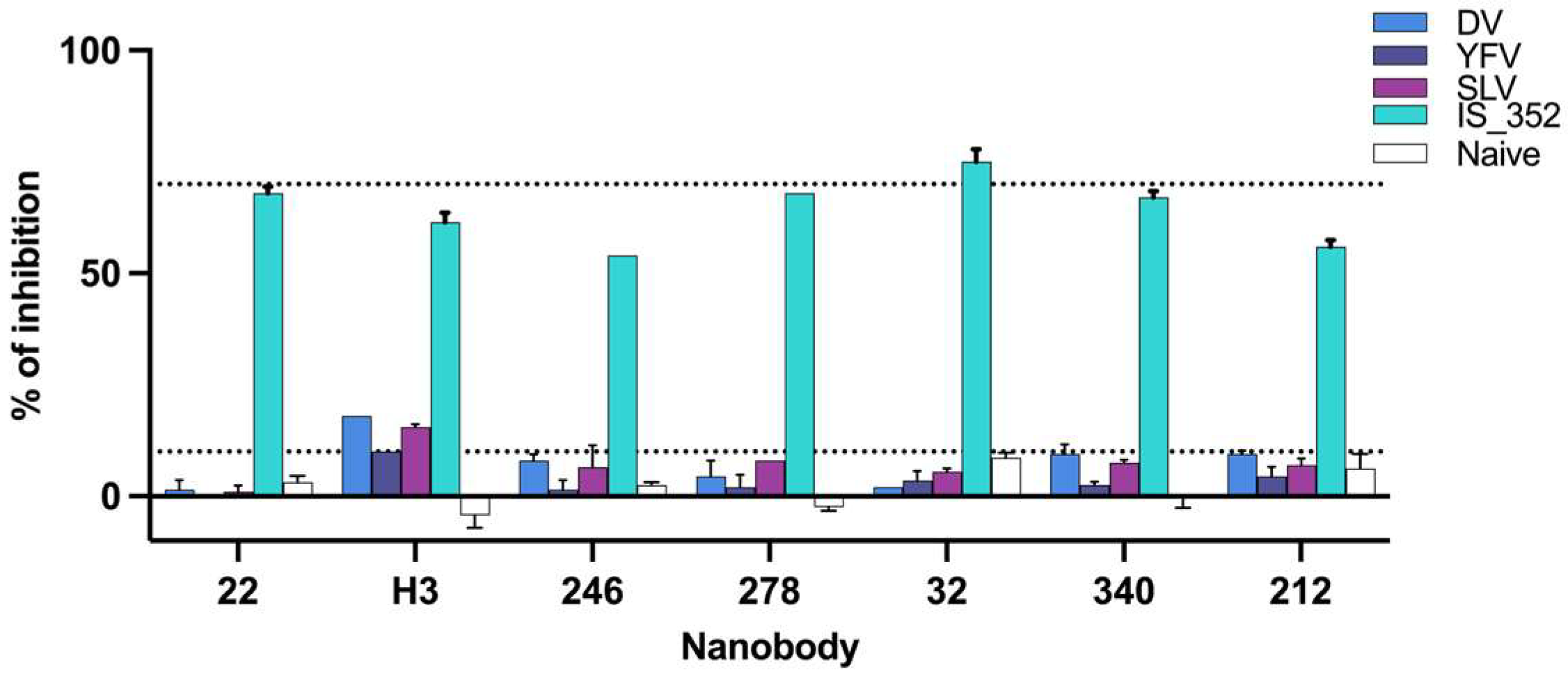
2.3. Selection of Nanobodies: Binding Inhibition and Cross-Reactivity Evaluation
2.4. Optimization of the ELISA
2.5. Study of Intra-Assay and Inter-Assay Reproducibility
3. Results
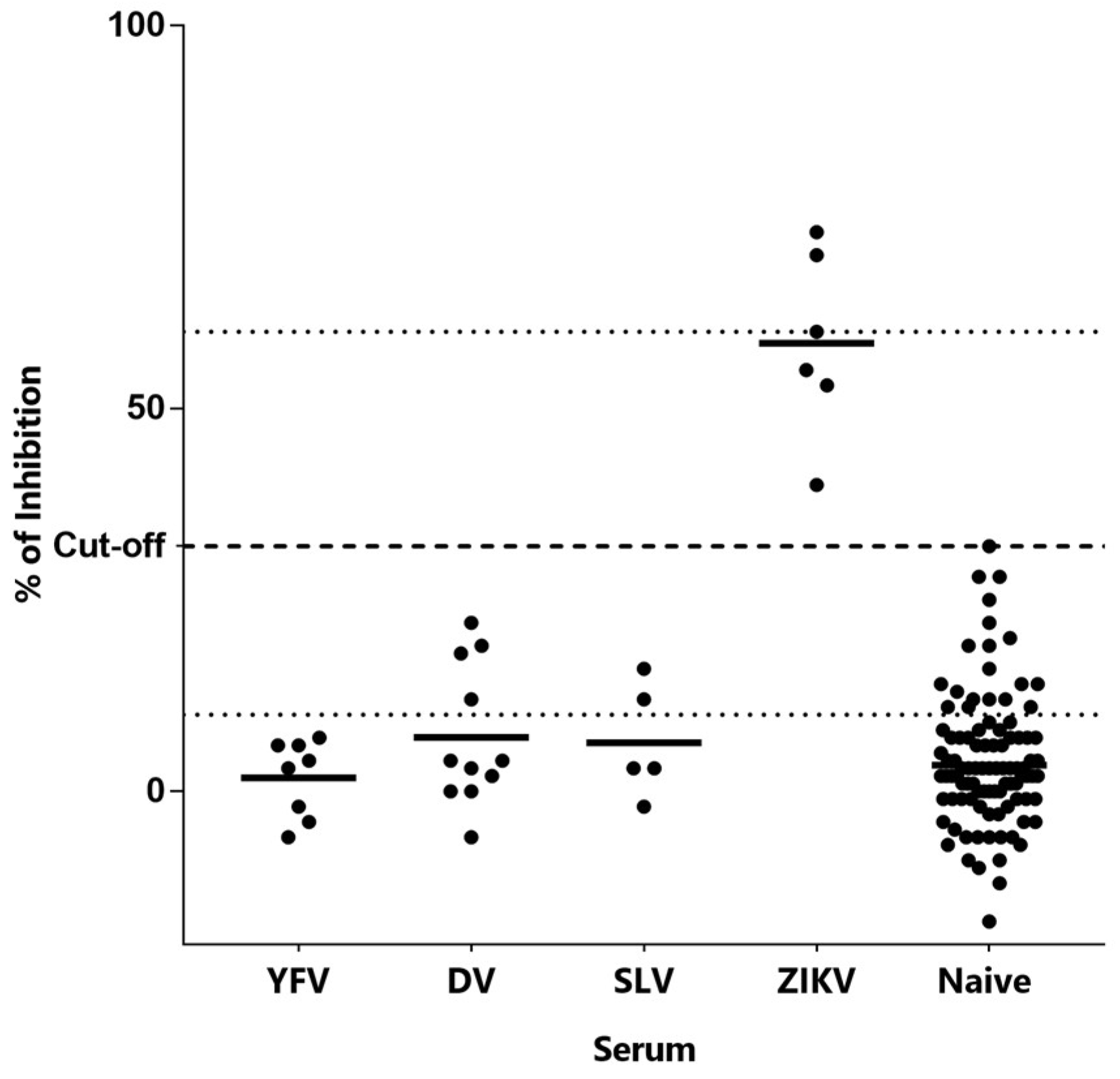
3.1. Election of Nanobodies: Binding Inhibition and Cross-Reactivity Evaluation
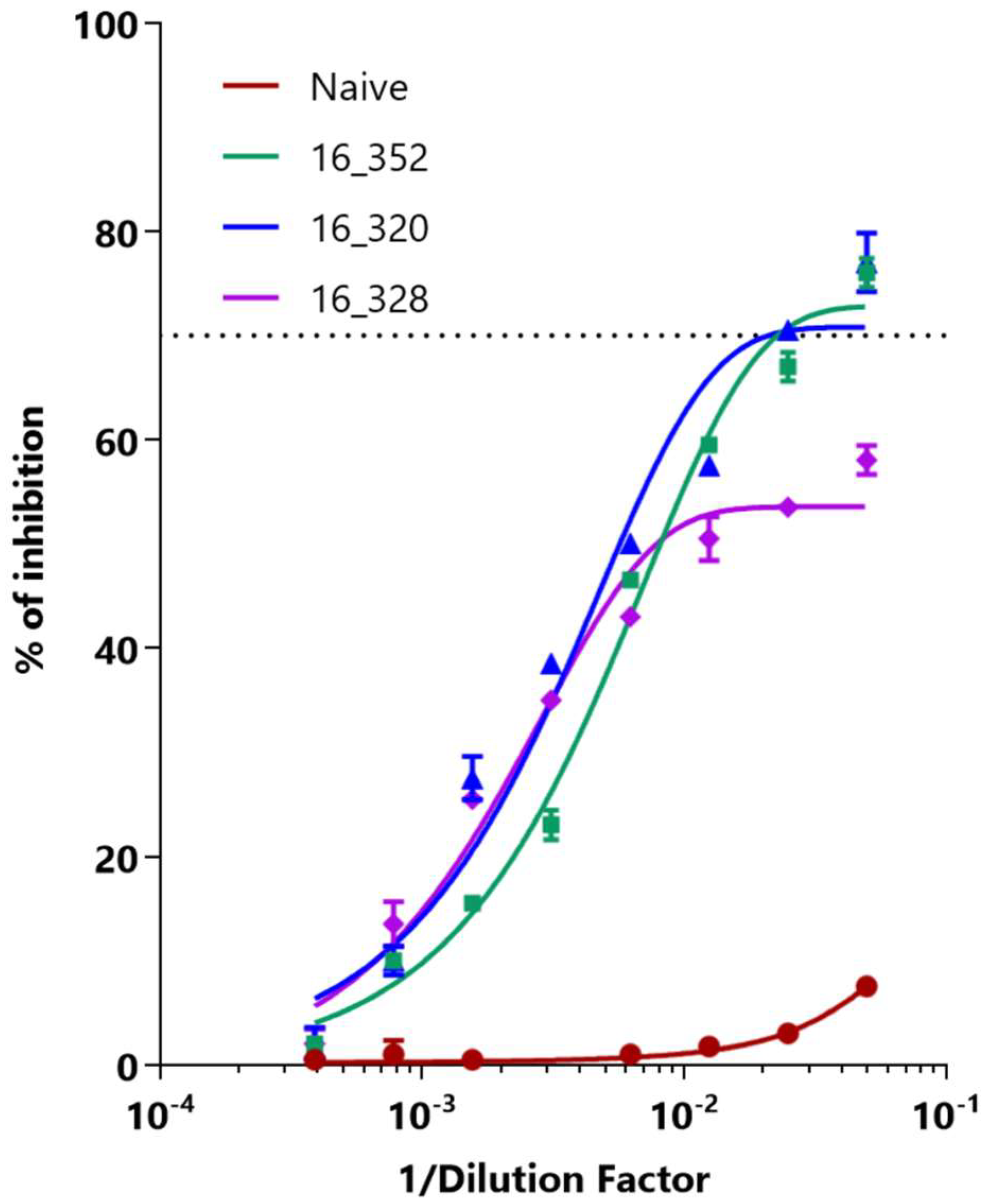
3.2. Optimization of Inhibition ELISA
3.3. Study of the Intra-Assay and Inter-Assay Reproducibility
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dick, G.W.; Kitchen, S.F.; Haddow, A.J. Zika virus (I). Isolations and serological specificity. Trans. R. Soc. Trop. Med. Hyg. 1952, 46, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Heukelbach, J.; Alencar, C.H.; Kelvin, A.A.; de Oliveira, W.K.; de Goes Cavalcanti, L.P. Zika virus outbreak in Brazil. J. Infect. Dev. Ctries. 2016, 10, 116–120. [Google Scholar] [CrossRef] [PubMed]
- Faria, N.R.; Azevedo, R.D.S.D.S.; Kraemer, M.U.; Souza, R.; Cunha, M.S.; Hill, S.C. Zika virus in the Americas: Early epidemiological and genetic findings. Science 2016, 352, 345–349. [Google Scholar] [CrossRef]
- Cao-Lormeau, V.M.; Roche, C.; Teissier, A.; Robin, E.; Berry, A.L.; Mallet, H.P. Zika virus, French polynesia, South pacific, 2013. Emerg. Infect. Dis. 2014, 20, 1085–1086. [Google Scholar] [CrossRef]
- Musso, D.; Roche, C.; Robin, E.; Nhan, T.; Teissier, A.; Cao-Lormeau, V.M. Potential sexual transmission of Zika virus. Emerg. Infect. Dis. 2015, 21, 359–361. [Google Scholar] [CrossRef]
- Mlakar, J.; Korva, M.; Tul, N.; Popovic, M.; Poljsak-Prijatelj, M.; Mraz, J.; Kolenc, M.; Resman Rus, K.; Vesnaver Vipotnik, T.; Fabjan Vodusek, V.; et al. Zika Virus Associated with Microcephaly. N. Engl. J. Med. 2016, 374, 951–958. [Google Scholar] [CrossRef]
- Moore, C.A.; Staples, J.E.; Dobyns, W.B.; Pessoa, A.; Ventura, C.V.; Fonseca, E.B.; Ribeiro, E.M.; Ventura, L.O.; Neto, N.N.; Arena, J.F.; et al. Characterizing the Pattern of Anomalies in Congenital Zika Syndrome for Pediatric Clinicians. JAMA Pediatr. 2017, 171, 288–295. [Google Scholar] [CrossRef]
- Bingham, A.M.; Cone, M.; Mock, V.; Heberlein-Larson, L.; Stanek, D.; Blackmore, C.; Likos, A. Comparison of Test Results for Zika Virus RNA in Urine, Serum, and Saliva Specimens from Persons with Travel-Associated Zika Virus Disease—Florida, 2016. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 475–478. [Google Scholar] [CrossRef]
- Song, H.; Qi, J.; Haywood, J.; Shi, Y.; Gao, G.F. Zika virus NS1 structure reveals diversity of electrostatic surfaces among flaviviruses. Nat. Struct. Mol. Biol. 2016, 23, 456–458. [Google Scholar] [CrossRef]
- Dejnirattisai, W.; Supasa, P.; Wongwiwat, W.; Rouvinski, A.; Barba-Spaeth, G.; Duangchinda, T.; Sakuntabhai, A.; Cao-Lormeau, V.M.; Malasit, P.; Rey, F.A.; et al. Dengue virus sero-cross-reactivity drives antibody-dependent enhancement of infection with zika virus. Nat. Immunol. 2016, 17, 1102–1108. [Google Scholar] [CrossRef] [PubMed]
- Priyamvada, L.; Quicke, K.M.; Hudson, W.H.; Onlamoon, N.; Sewatanon, J.; Edupuganti, S.; Pattanapanyasat, K.; Chokephaibulkit, K.; Mulligan, M.J.; Wilson, P.C.; et al. Human antibody responses after dengue virus infection are highly cross-reactive to Zika virus. Proc. Natl. Acad. Sci. USA 2016, 113, 7852–7857. [Google Scholar] [CrossRef] [PubMed]
- Rockstroh, A.; Barzon, L.; Kumbukgolla, W.; Su, H.X.; Lizarazo, E.; Vincenti-Gonzalez, M.F.; Tami, A.; Ornelas, A.M.M.; Aguiar, R.S.; Cadar, D.; et al. Dengue Virus IgM Serotyping by ELISA with Recombinant Mutant Envelope Proteins. Emerg. Infect. Dis. 2019, 25, 1111–1115. [Google Scholar] [CrossRef] [PubMed]
- Liang, B.; Guida, J.P.; Costa Do Nascimento, M.L.; Mysorekar, I.U. Host and viral mechanisms of congenital Zika syndrome. Virulence 2019, 10, 768–775. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.H.; Wey, J.J.; Sun, Y.C.; Chin, C.; Chien, L.J.; Wu, Y.C. Antibody responses to an immunodominant nonstructural 1 synthetic peptide in patients with dengue fever and dengue hemorrhagic fever. J. Med. Virol. 1999, 57, 1–8. [Google Scholar] [CrossRef]
- Shu, P.Y.; Chen, L.K.; Chang, S.F.; Su, C.L.; Chien, L.J.; Chin, C.; Lin, T.H.; Huang, J.H. Dengue virus serotyping based on envelope and membrane and nonstructural protein NS1 serotype-specific capture immunoglobulin M enzyme-linked immunosorbent assays. J. Clin. Microbiol. 2004, 42, 2489–2494. [Google Scholar] [CrossRef]
- Felix, A.C.; Souza, N.C.S.; Figueiredo, W.M.; Costa, A.A.; Inenami, M.; da Silva, R.M.G.; Levi, J.E.; Pannuti, C.S.; Romano, C.M. Cross reactivity of commercial anti-dengue immunoassays in patients with acute Zika virus infection. J. Med. Virol. 2017, 89, 1477–1479. [Google Scholar] [CrossRef]
- Zaidi, M.B.; Cedillo-Barron, L.; Gonzalez, Y.A.M.E.; Garcia-Cordero, J.; Campos, F.D.; Namorado-Tonix, K.; Perez, F. Serological tests reveal significant cross-reactive human antibody responses to Zika and Dengue viruses in the Mexican population. Acta Trop. 2020, 201, 105201. [Google Scholar] [CrossRef]
- Balmaseda, A.; Stettler, K.; Medialdea-Carrera, R.; Collado, D.; Jin, X.; Zambrana, J.V.; Jaconi, S.; Cameroni, E.; Saborio, S.; Rovida, F.; et al. Antibody-based assay discriminates Zika virus infection from other flaviviruses. Proc. Natl. Acad. Sci. USA 2017, 114, 8384–8389. [Google Scholar] [CrossRef]
- Hamers-Casterman, C.; Atarhouch, T.; Muyldermans, S.; Robinson, G.; Hamers, C.; Songa, E.B.; Bendahman, N.; Hamers, R. Naturally occurring antibodies devoid of light chains. Nature 1993, 363, 446–448. [Google Scholar] [CrossRef]
- Muyldermans, S. Nanobodies: Natural single-domain antibodies. Annu. Rev. Biochem. 2013, 82, 775–797. [Google Scholar] [CrossRef]
- Gonzalez-Sapienza, G.; Rossotti, M.A.; Tabares-da Rosa, S. Single-Domain Antibodies As Versatile Affinity Reagents for Analytical and Diagnostic Applications. Front. Immunol. 2017, 8, 977. [Google Scholar] [CrossRef] [PubMed]
- van der Linden, R.H.; Frenken, L.G.; de Geus, B.; Harmsen, M.M.; Ruuls, R.C.; Stok, W.; de Ron, L.; Wilson, S.; Davis, P.; Verrips, C.T. Comparison of physical chemical properties of llama VHH antibody fragments and mouse monoclonal antibodies. Biochim. Biophys. Acta 1999, 1431, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Delfin-Riela, T.; Rossotti, M.A.; Echaides, C.; Gonzalez-Sapienza, G. A nanobody-based test for highly sensitive detection of hemoglobin in fecal samples. Anal. Bioanal. Chem. 2020, 412, 389–396. [Google Scholar] [CrossRef] [PubMed]
- Rossotti, M.A.; Pirez, M.; Gonzalez-Techera, A.; Cui, Y.; Bever, C.S.; Lee, K.S.; Morisseau, C.; Leizagoyen, C.; Gee, S.; Hammock, B.D.; et al. Method for Sorting and Pairwise Selection of Nanobodies for the Development of Highly Sensitive Sandwich Immunoassays. Anal. Chem. 2015, 87, 11907–11914. [Google Scholar] [CrossRef] [PubMed]
- Delfin-Riela, T.; Rossotti, M.; Alvez-Rosado, R.; Leizagoyen, C.; González-Sapienza, G. Highly Sensitive Detection of Zika Virus Nonstructural Protein 1 in Serum Samples by a Two-Site Nanobody ELISA. Biomolecules 2020, 10, 1652. [Google Scholar] [CrossRef]
- Morillas, P.P.; Terra, A.I.; Uribe, C.; Mastromonaco, G.; Prieto, J.L.; Torres, M. Guía Eurachem: La Adecuación al uso de los Métodos Analíticos—Una Guía de Laboratorio Para la Validación de Métodos y Temas Relacionados; EURACHEM, Eurolab EspañaT: Madrid, Spain, 2016. [Google Scholar]
| Intra-Day Precision | Inter-Day Precision | |
|---|---|---|
| Replicates | 5 | 5 |
| Mean Value (% inhibition) | 68 | 65 |
| CV% | 2.7 | 7.7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Delfin-Riela, T.; Rossotti, M.A.; Mattiuzzo, G.; Echaides, C.; González-Sapienza, G. Nanobody-Based Blocking of Binding ELISA for the Detection of Anti-NS1 Zika-Virus-Specific Antibodies in Convalescent Patients. Trop. Med. Infect. Dis. 2023, 8, 55. https://doi.org/10.3390/tropicalmed8010055
Delfin-Riela T, Rossotti MA, Mattiuzzo G, Echaides C, González-Sapienza G. Nanobody-Based Blocking of Binding ELISA for the Detection of Anti-NS1 Zika-Virus-Specific Antibodies in Convalescent Patients. Tropical Medicine and Infectious Disease. 2023; 8(1):55. https://doi.org/10.3390/tropicalmed8010055
Chicago/Turabian StyleDelfin-Riela, Triana, Martín A. Rossotti, Giada Mattiuzzo, César Echaides, and Gualberto González-Sapienza. 2023. "Nanobody-Based Blocking of Binding ELISA for the Detection of Anti-NS1 Zika-Virus-Specific Antibodies in Convalescent Patients" Tropical Medicine and Infectious Disease 8, no. 1: 55. https://doi.org/10.3390/tropicalmed8010055
APA StyleDelfin-Riela, T., Rossotti, M. A., Mattiuzzo, G., Echaides, C., & González-Sapienza, G. (2023). Nanobody-Based Blocking of Binding ELISA for the Detection of Anti-NS1 Zika-Virus-Specific Antibodies in Convalescent Patients. Tropical Medicine and Infectious Disease, 8(1), 55. https://doi.org/10.3390/tropicalmed8010055







