Coordination and Management of COVID-19 in Africa through Health Operations and Technical Expertise Pillar: A Case Study from WHO AFRO One Year into Response
Abstract
:1. Introduction
2. Methods
3. Findings
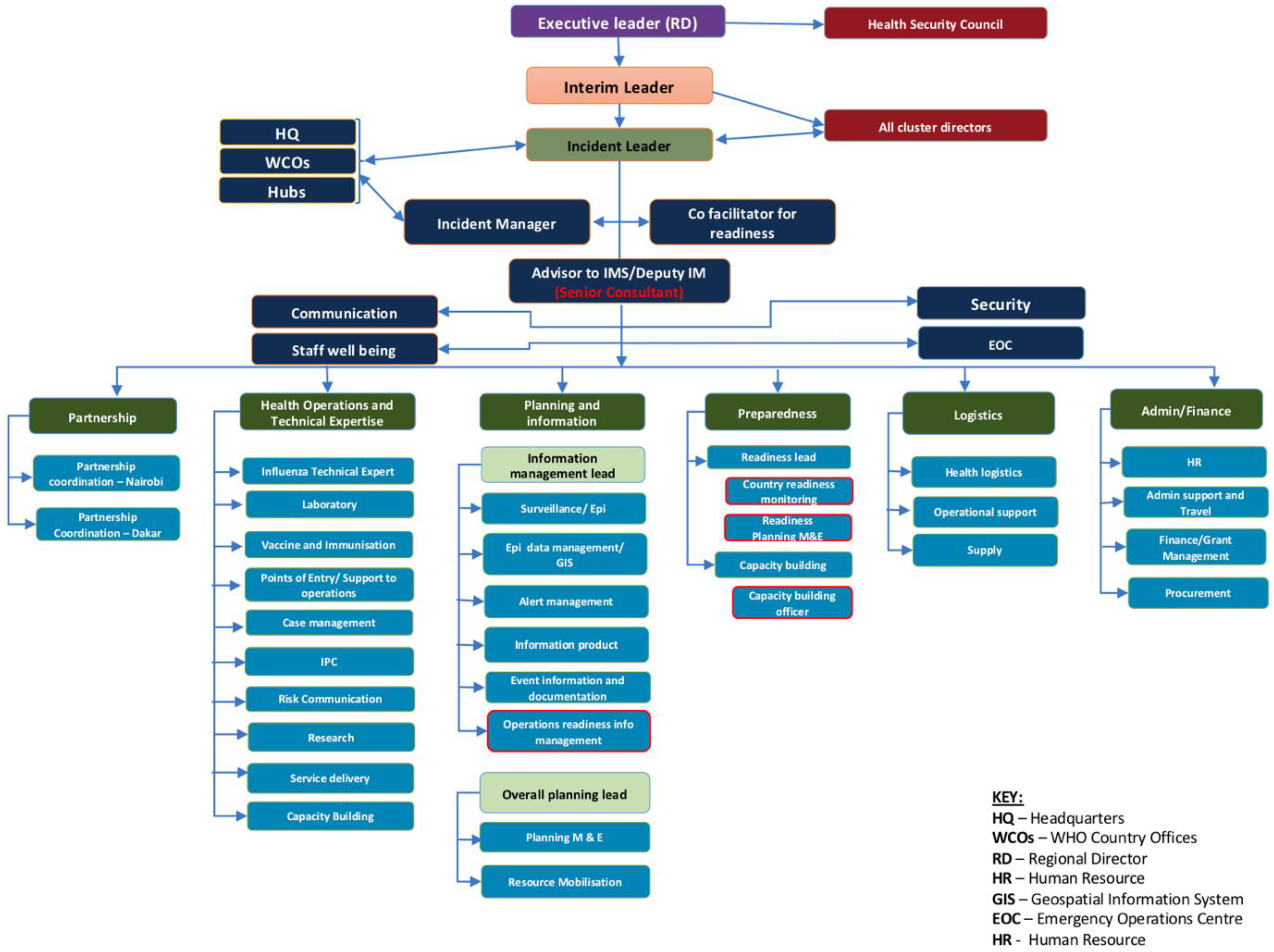
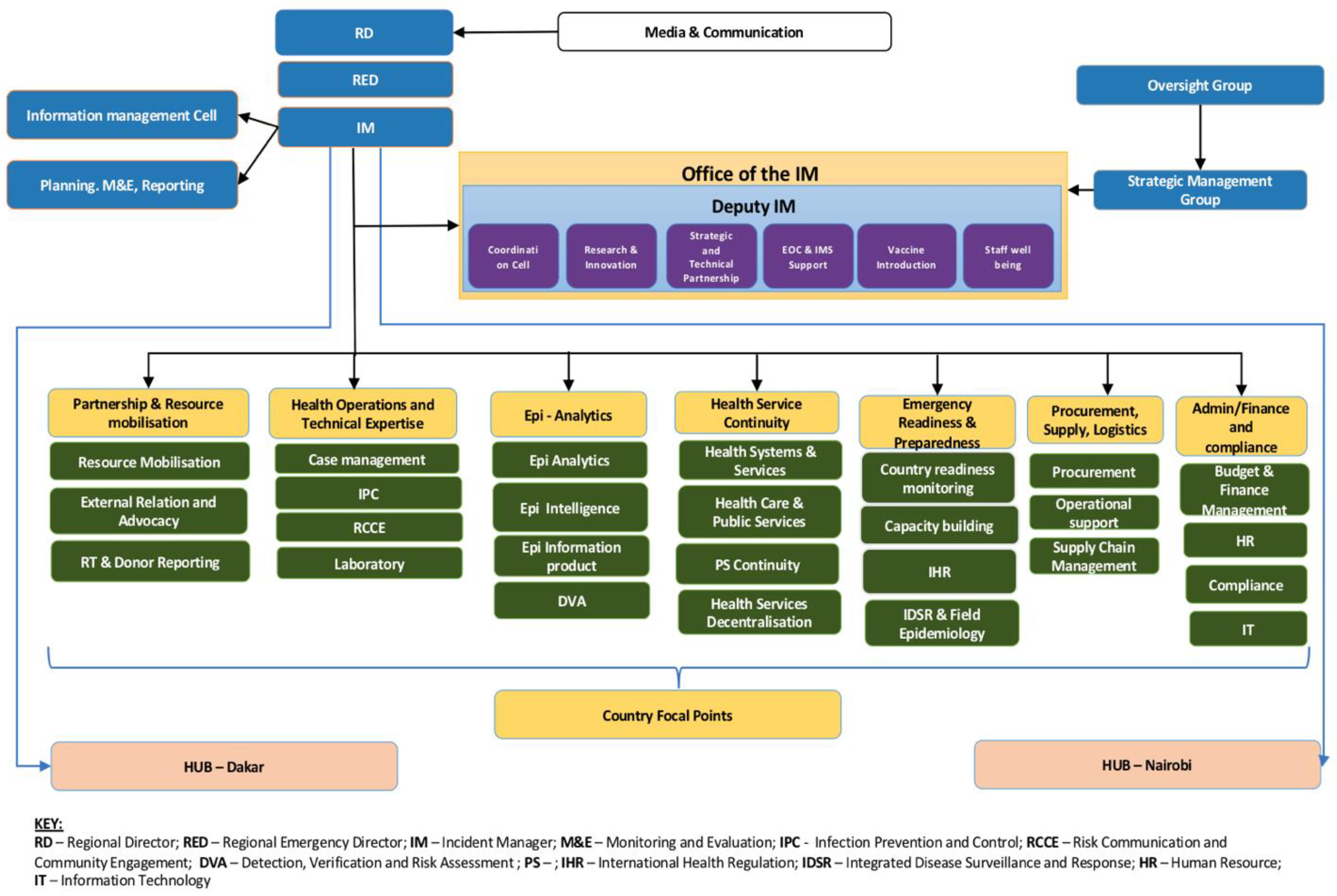
The Changes in the Organisational Structure of Health Operations and Technical Expertise Pillar during the Pandemic and the Roles of the Sub Pillars
4. Key Learnings
4.1. HOTE Intra and Extra Team Coordination
4.2. Internal and External Coordination Meetings
4.3. HOTE Collaboration with Countries
4.4. Intra-Communication among HOTE Members
4.5. Documentation and Information Management
4.6. Monitoring Objectives
5. Discussion and Conclusions
6. Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organisation. Novel Coronavirus (2019-nCoV); Situation Report—1; World Health Organisation: Geneva, Switzerland, 2020; Available online: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200121-sitrep-1-2019-ncov.pdf (accessed on 7 January 2020).
- World Health Organisation. Listings of WHO’s Response to COVID-19; World Health Organisation: Geneva, Switzerland, 2020; Available online: https://www.who.int/news/item/29-06-2020-covidtimeline (accessed on 7 January 2020).
- Quaife, M.; van Zandvoort, K.; Gimma, A.; Shah, K.; McCreesh, N.; Prem, K.; Barasa, E.; Mwanga, D.; Kangwana, B.; Pinchoff, J.; et al. The impact of COVID-19 control measures on social contacts and transmission in Kenyan informal settlements. BMC Med. 2020, 18, 316. [Google Scholar] [CrossRef] [PubMed]
- Diop, B.Z.; Ngom, M.; Biyong, C.P.; Biyong, J.N.P. The relatively young and rural population may limit the spread and severity of COVID-19 in Africa: A modelling study. BMJ Glob. Health. 2020, 5, e002699. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, M.; Pullano, G.; Pinotti, F.; Valdano, E.; Poletto, C.; Boëlle, P.-Y. Preparedness and vulnerability of African countries against importations of COVID-19: A modelling study. Lancet 2020, 395, 871–877. [Google Scholar] [CrossRef]
- Nkengasong, J.N.; Mankoula, W. Looming threat of COVID-19 infection in Africa: Act collectively, and fast. Lancet 2020, 395, 841–842. [Google Scholar] [CrossRef]
- Hopman, J.; Allegranzi, B.; Mehtar, S. Managing COVID-19 in low-and middle-income countries. JAMA. 2020, 323, 1549–1550. [Google Scholar] [CrossRef]
- Martinez-Alvarez, M.; Jarde, A.; Usuf, E.; Brotherton, H.; Bittaye, M.; Samateh, A.L.; Antonio, M.; Vives-Tomas, J.; D’Alessandro, U.; Roca, A. COVID-19 pandemic in west Africa. Lancet Glob. Health 2020, 8, e631–e632. [Google Scholar] [CrossRef]
- Nguimkeu, P.; Tadadjeu, S. Why is the Number of COVID-19 Cases Lower Than Expected in Sub-Saharan Africa? A Cross-Sectional Analysis of the Role of Demographic and Geographic Factors. World Dev. 2021, 138, 105251. [Google Scholar] [CrossRef]
- Doshi, P. COVID-19: Do many people have pre-existing immunity? BMJ 2020, 370, m3563. [Google Scholar] [CrossRef]
- Haider, N.; Osman, A.Y.; Gadzekpo, A.; Akipede, G.O.; Asogun, D.; Ansumana, R.; Lessells, R.J.; Khan, P.; Hamid, M.M.A.; Yeboah-Manu, D.; et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob. Health 2020, 5, e003319. [Google Scholar] [CrossRef]
- Bankole, T.O.; Omoyeni, O.B.; Oyebode, A.O.; Akintunde, D.O. Low incidence of COVID-19 in the West African sub-region: Mitigating healthcare delivery system or a matter of time? J. Public Health 2020, 30, 1179–1188. [Google Scholar] [CrossRef]
- Worldometer: Coronavirus Update (Live). Available online: https://www.worldometers.info/coronavirus/ (accessed on 26 October 2020).
- Yaya, S.; Otu, A.; Labonté, R. Globalisation in the time of COVID-19: Repositioning Africa to meet the immediate and remote challenges. Glob. Health 2020, 16, 1–7. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Operational Review of the WHO AFRO IMST to COVID-19 Pandemic Response; World Health Organisation: Brazaville, Congo, 2020. [Google Scholar]
- World Health Organization. Emergency Response Framework (ERF), 2nd ed.; World Health Organization: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/bitstream/handle/10665/258604/9789241512299-eng.pdf (accessed on 2 June 2021).
- World Health Organisation. Report on the Strategic Response to COVID-19 in the WHO African Region: February–December 2020; WHO Regional Office for Africa: Brazzavile, Congo, 2020. [Google Scholar]
- World Health Organisation. Strategic Response Plan for the WHO African Region: February–December 2020 (Update 4 May 2020); World Health Organisation: Brazzavile, Congo, 2020; Available online: https://www.afro.who.int/sites/default/files/2021-04/SPRP%20BUDGET%200520_01.pdf (accessed on 30 July 2021).
- Yin, K.R. Case Study Research and Applications: Design and Methods, 6th ed.; SAGE Publications: Thousand Oaks, CA, USA, 2018. [Google Scholar]
- World Health Organisation. Health Operation and Technical Expertise; Pillar Progressive Report for COVID-19; World Health Organisation: Geneva, Switzerland, 2020. [Google Scholar]
- Heale, R.; Forbes, D. Understanding triangulation in research. Evid. Based Nurs. 2013, 16, 98. [Google Scholar] [CrossRef] [PubMed]
- Bowen, G.A. Document analysis as a qualitative research method. Qual. Res. J. 2009, 9, 27–40. [Google Scholar] [CrossRef]
- Uneke, C.J.; Langlois, E.V.; Uro-Chukwu, H.C.; Chukwu, J.; Ghaffar, A. Fostering access to and use of contextualised knowledge to support health policy-making: Lessons from the Policy Information Platform in Nigeria. Health Res. Policy Syst. 2019, 17, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Cohn, K.H. Developing effective communication skills. J. Oncol. Pract. 2007, 3, 314–317. [Google Scholar]
- Forman, R.; Atun, R.; McKee, M.; Mossialos, E. 12 Lessons learned from the management of the coronavirus pandemic. Health Policy 2020, 124, 577–580. [Google Scholar] [CrossRef]
- Savoia, E.; Massin-Short, S.B.; Rodday, A.M.; Aaron, L.A.; Higdon, M.A.; Stoto, M.A. Public health systems research in emergency preparedness: A review of the literature. Am. J. Prev. Med. 2009, 37, 150–156. [Google Scholar] [CrossRef]
- World Health Organisation. Managing Epidemics: Key Facts About Major Deadly Diseases; World Health Organisation: Geneva, Switzerland, 2018; Available online: https://www.who.int/emergencies/diseases/managing-epidemics-interactive.pdf (accessed on 23 March 2021).
- Hung, K.; Mashino, S.; Chan, E.; MacDermot, M.; Balsari, S.; Ciottone, G.; Della Corte, F.; Dell’Aringa, M.; Egawa, S.; Evio, B.; et al. Health Workforce Development in Health Emergency and Disaster Risk Management: The Need for Evidence-Based Recommendations. Int. J. Environ. Res. Public Health 2021, 18, 3382. [Google Scholar] [CrossRef]
- Margherita, A.; Elia, G.; Klein, M. Managing the COVID-19 emergency: A coordination framework to enhance response practices and actions. Technol. Forecast. Soc. Chang. 2021, 166, 120656. [Google Scholar] [CrossRef]
- Olu, O.O.; Lamunu, M.; Chimbaru, A.; Adegboyega, A.; Conteh, I.; Nsenga, N.; Sempiira, N.; Kamara, K.-B.; Dafae, F.M. Incident management systems are essential for effective coordination of large disease outbreaks: Perspectives from the coordination of the Ebola outbreak response in Sierra Leone. Front. Public Health 2016, 4, 254. [Google Scholar] [CrossRef]
- Hernantes, J.; Rich, E.; Laugé, A.; Labaka, L.; Sarriegi, J.M. Learning before the storm: Modeling multiple stakeholder activities in support of crisis management, a practical case. Technol. Forecast. Soc. Chang. 2013, 80, 1742–1755. [Google Scholar] [CrossRef]

| Pillar/Sub-Pillar | Interventions | Activities |
|---|---|---|
| Pillar Lead (1) | - Provide guidance and leadership of the pillar. | - Coordinate the operations of the five sub-pillars - Represents the pillar in the cross-pillar meetings at the IMST strategic meeting - The lead represents the voice of the pillar and communicates all their needs to the management. |
| IPC (7) | - Strengthen patients’ treatment and prevent transmission to staff, all patients/visitors, and the community against COVID-19 infection by reviewing, updating, and disseminating existing and interim IPC protocols, including triage. | - Build capacity of health care workers on IPC for COVID-19 and SARIs (staff, training, supplies-PPEs, and equipment) for member states. - Provide strategic guidance to countries on all aspects of the pandemic response relating to the IPC component - Provide countries with the technical recommendations and tools necessary for their application - Strengthen the capacities of countries in the implementation of interventions, as well as in monitoring and evaluation - Strengthen the activities carried out by the other sub-pillars because of their transversal nature |
| RCCE (6) | - Strengthen public awareness through an integrated risk communication and community engagement approach on the COVID-19, including a psycho-social component in 47 Member States. | - Strengthen the identification of RCCE actions towards specific population groups and settings to address knowledge, rumours, and misinformation in 47 Member states. |
| CM (5) | - Improve clinical care for COVID-19 patients through slowing and stopping transmission, finding, isolating, and testing every suspected case, and provide timely, appropriate care to affected patients. | - Support clinical CM for COVID-19 patients in Member States’ treatment facilities through training, developing guidance and SOPs, assessments for screening/isolation capacity, ICU units, and related medical supplies access. |
| Laboratory (5) | - Strengthen and maintain regional and country surveillance systems to gather data on alerts, suspected cases and confirmed COVID-19 cases in collaboration with partners. | - Provide laboratory support at National and Sub-national levels, including reagents and other supplies to the Member States. |
| EMT (2) | - Strengthen and establish the regional training centre; and the national EMTs | - Enhance collaboration/coordination with Member states, Africa CDC, Regional Economic Communities, National and International NGOs and UN resident coordinators (RCs) to mobilise experts and safe deployment to support the response. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ngoy, N.; Conteh, I.N.; Oyugi, B.; Abok, P.; Kobie, A.; Phori, P.; Hamba, C.; Ejiofor, N.E.; Fitzwanga, K.; Appiah, J.; et al. Coordination and Management of COVID-19 in Africa through Health Operations and Technical Expertise Pillar: A Case Study from WHO AFRO One Year into Response. Trop. Med. Infect. Dis. 2022, 7, 183. https://doi.org/10.3390/tropicalmed7080183
Ngoy N, Conteh IN, Oyugi B, Abok P, Kobie A, Phori P, Hamba C, Ejiofor NE, Fitzwanga K, Appiah J, et al. Coordination and Management of COVID-19 in Africa through Health Operations and Technical Expertise Pillar: A Case Study from WHO AFRO One Year into Response. Tropical Medicine and Infectious Disease. 2022; 7(8):183. https://doi.org/10.3390/tropicalmed7080183
Chicago/Turabian StyleNgoy, Nsenga, Ishata Nannie Conteh, Boniface Oyugi, Patrick Abok, Aminata Kobie, Peter Phori, Cephas Hamba, Nonso Ephraim Ejiofor, Kaizer Fitzwanga, John Appiah, and et al. 2022. "Coordination and Management of COVID-19 in Africa through Health Operations and Technical Expertise Pillar: A Case Study from WHO AFRO One Year into Response" Tropical Medicine and Infectious Disease 7, no. 8: 183. https://doi.org/10.3390/tropicalmed7080183
APA StyleNgoy, N., Conteh, I. N., Oyugi, B., Abok, P., Kobie, A., Phori, P., Hamba, C., Ejiofor, N. E., Fitzwanga, K., Appiah, J., Edwin, A., Fawole, T., Kamara, R., Cihambanya, L. K., Mzozo, T., Ryan, C., Braka, F., Yoti, Z., Kasolo, F., ... Gueye, A. S. (2022). Coordination and Management of COVID-19 in Africa through Health Operations and Technical Expertise Pillar: A Case Study from WHO AFRO One Year into Response. Tropical Medicine and Infectious Disease, 7(8), 183. https://doi.org/10.3390/tropicalmed7080183







