Surveillance Quality Indicators Highlight the Need for Improving Tuberculosis Diagnostics and Monitoring in a Hyperendemic Area of the Brazilian Amazon Region
Abstract
1. Introduction
2. Materials and Methods
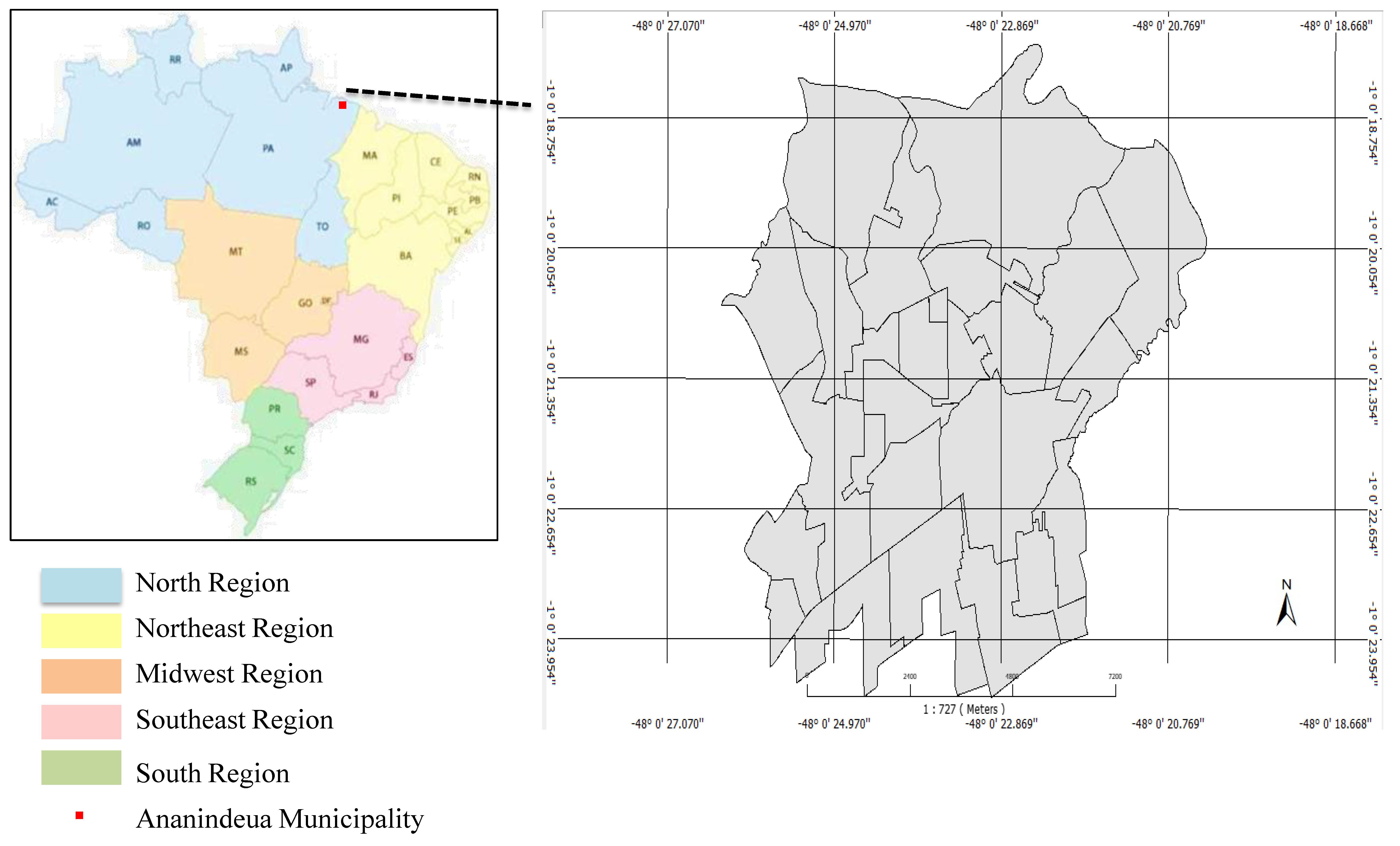
2.1. Study Design and Location
2.2. Tuberculosis Case Selection
2.3. Data Collection and Analysis
2.4. Ethical Aspects
3. Results
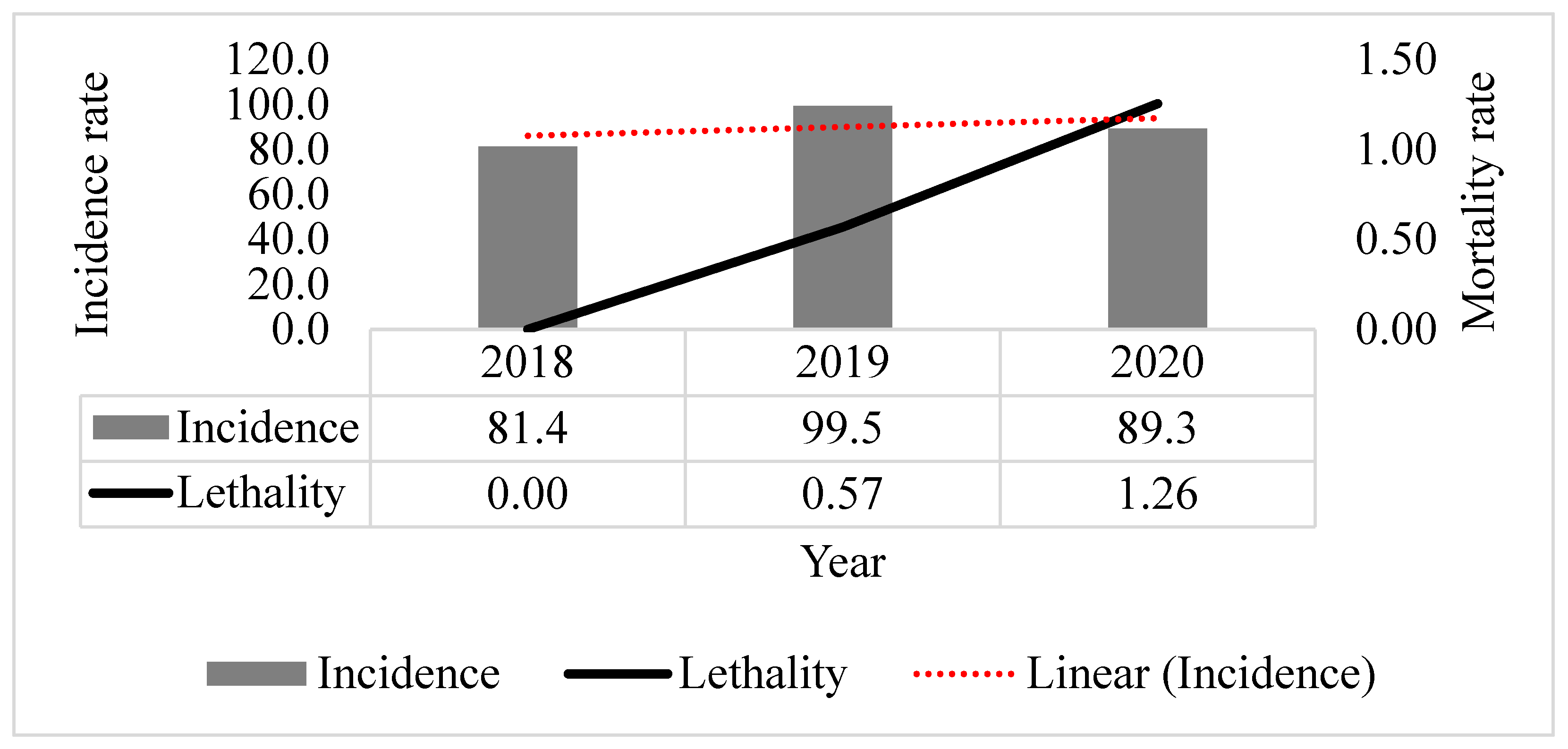
3.1. Epidemiological Indicators
3.2. Surveillance Quality Indicators
3.3. New Cases Versus Relapses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barreira, D. Os desafios para a eliminação da tuberculose no Brasil. Epidemiol. Serviços Saúde 2018, 27, e00100009. [Google Scholar] [CrossRef] [PubMed]
- Moreira, A.D.S.R.; Kritski, A.L.; Carvalho, A.C.C. Determinantes sociais da saúde e custos catastróficos associados ao diagnóstico e tratamento da tuberculose. J. Bras. Pneumol. 2020, 46, e20200015. [Google Scholar] [PubMed]
- Brasil, M.D.S. Guia de Vigilância em Saúde, 5th ed.; Secretaria de Vigilância em Saúde Coordenação-Geral de Desenvolvimento da Epidemiologia em Serviços: Brasília, Brazil, 2021. [Google Scholar]
- Brasil, M.D.S. Manual de Operação SINAN. Vigilância Saúde 2015, 1, 1–125. [Google Scholar]
- Frimpong-Mansoh, R.P.; Calys-Tagoe, B.N.L.; Therson-Coffie, E.F.; Antwi-Agyei, K.O. Evaluation of the tuberculosis surveillance system in the Ashaiman municipality, in Ghana. Pan Afr. Med. J. 2018, 31, 1–10. [Google Scholar] [CrossRef] [PubMed]
- CDC. Updated Guidelines for Evaluating Public Health Surveillance Systems 2001. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5013a1.htm (accessed on 11 November 2021).
- Silva, G.D.M.D.; Bartholomay, P.; Cruz, O.G.; Garcia, L.P. Avaliação da qualidade dos dados, oportunidade e aceitabilidade da vigilância da tuberculose nas microrregiões do Brasil. Cien. Saude Colet. 2017, 22, 3307–3319. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Tuberkulosis Report; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Brito, A.C.D.; Silva, D.A.D.; Dell’Orti, D.G.; Arakaki, D.; Johansen, F.D.C.; Andrade, K.B.; Alves, K.C.; Fornaziere, L.S.R.; Souza, N.M.; Couto, R. M; Arakawa, T; Sanine, P.R. Tuberculose 2021 Boletim Epidemiológico Especial, 1st ed.; Secretaria de Vigilância em Saúde Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis—DCCI Coordenação Geral de Vigilância das Doenças de Transmissão Respiratória de Condições Crônicas—CGDR: Brasília, Brazil, 2021; Volume 1. [Google Scholar]
- Brasil, M.D.S. Indicadores Operacionais da Tuberculose no Brasil e a COVID-19: Análise Comparativa dos Anos de 2019 e 2020, 1st ed.; Coordenação-Geral de Vigilância das Doenças de Transmissão Respiratória de Condições Crônicas do Departamento de Doenças de Condições Crônicas e Infecções Sexualmente Transmissíveis (CGDR/DCCI/SVS): Brasília, Brazil, 2021; Volume 52. [Google Scholar]
- Secretaria de Estado de Saúde Pública. Boletim Epidemiológico Da Tuberculose—No 01. Dir. Vigilância Saúde 2021, 1, 1–15. [Google Scholar]
- Brasil, M.D.S. SINANWEB—Página Inicial. SINAN 2021. Available online: https://portalsinan.saude.gov.br/ (accessed on 11 November 2021).
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [PubMed]
- IBGE. Ananindeua (PA)|Cidades e Estados|IBGE. 2021. Available online: https://www.ibge.gov.br/cidades-e-estados/pa/ananindeua.html (accessed on 11 November 2021).
- Brasil, M.D.S. Ficha de notificação da Tuberculose. Secr Vigilância Em Saúde 2014. Available online: http://portalsinan.saude.gov.br/images/documentos/Agravos/Tuberculose/Tuberculose_v5.pdf (accessed on 11 November 2021).
- Costa, R.J.F.D.; Miranda, C.D.S.C.; Noguchi, S.K.D.T.; de Oliveira, R.A.C.; de Oliveira Santos, B.; Pinto, D.D.S. Distribuição Espaço-Temporal Da Tuberculose No Município De Ananindeua, Pará, Brasil. Rev. Inspirar Mov. Saúde 2021, 21, 1–16. [Google Scholar]
- CDC. Fact Sheets|Testing and Diagnosis|Fact Sheets—Diagnosis of Tuberculosis Disease|TB|CDC. 2021. Available online: https://www.cdc.gov/tb/publications/factsheets/testing/diagnosis.htm (accessed on 11 November 2021).
- Parsons, L.M.; Somoskövi, Á.; Gutierrez, C.; Lee, E.; Paramasivan, C.N.; Abimiku, A.; Spector, S.; Roscigno, G.; Nkengasong, J. Laboratory Diagnosis of Tuberculosis in Resource-Poor Countries: Challenges and Opportunities. Clin. Microbiol. Rev. 2011, 24, 314–350. [Google Scholar] [CrossRef] [PubMed]
- Bartholomay, P.; Pelissari, D.M.; de Araujo, W.N.; Yadon, Z.E.; Heldal, E. Quality of tuberculosis care at different levels of health care in Brazil in 2013. Rev. Panam. Salud Pública 2016, 39, 3–11. [Google Scholar] [PubMed]
- Rocha, M.S.; Oliveira, G.P.D.; Guillen, L.C.T.; Coeli, C.M.; Saraceni, V.; Pinheiro, R.S. Uso de linkage entre diferentes bases de dados para qualificação de variáveis do Sinan-TB e a partir de regras de scripting. Cad. Saude Publica 2019, 35, e00074318. [Google Scholar] [CrossRef] [PubMed]
- Santos, N.P.D.; Lírio, M.; Passos, L.A.R.; Kritski, J.P.D.A.L.; Galvão-Castro, B.; Grassi, M.F.R. Completeness of tuberculosis reporting forms in five Brazilian capitals with a high incidence of the disease. J. Bras. Pneumol. 2013, 39, 221–225. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Farias, R.C.; Rodrigues, I.L.A.; Nogueira, L.M.V.; da Silva, F.O.; Conacci, B.J.; dos Santos, C.B. Indicadores Operacionais do Controle da Tuberculose No Município de Belém-Pará. Cogitare Enferm. 2020, 25, e70880. [Google Scholar] [CrossRef]
- Pelissari, D.M.; Rocha, M.S.; Bartholomay, P.; Sanchez, M.N.; Duarte, E.C.; Arakaki-Sanchez, D.; Dantas, C.O.; Jacobs, M.G.; Andrade, K.B.; Codenotti, S.; et al. Identifying socioeconomic, epidemiological and operational scenarios for tuberculosis control in Brazil: An ecological study. BMJ Open 2018, 8, e018545. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.M.; Harries, A.D.; Satyanarayana, S.; Thekkur, P.; Shewade, H.D.; Zachariah, R. What is operational research and how can national tuberculosis programmes in low- and middle-income countries use it to end TB? Indian J. Tuberc. 2020, 67, S23–S32. [Google Scholar] [CrossRef] [PubMed]
- Arakawa, T.; Magnabosco, G.T.; Lopes, L.M.; Arnaez, M.A.A.; Gavín, M.A.O.; Gallardo, M.D.P.S.; Monroe, A.A.; Villa, T.C.S. Avaliação de desempenho de Programas de Controle de Tuberculose no contexto brasileiro e espanhol: Uma revisão integrativa da literatura. Cien. Saude Colet. 2015, 20, 3877–3889. [Google Scholar] [CrossRef] [PubMed]
- Millet, J.P.; Orcau, À.; De Olalla, P.G.; Casals, M.; Rius, C.; Caylà, J.A. Tuberculosis recurrence and its associated risk factors among successfully treated patients. J. Epidemiol. Community Health 2009, 63, 799–804. [Google Scholar] [CrossRef] [PubMed]
- Crofts, J.P.; Andrews, N.J.; Barker, R.D.; Delpech, V.; Abubakar, I. Risk factors for recurrent tuberculosis in England and Wales, 1998–2005. Thorax 2010, 65, 310–314. [Google Scholar] [CrossRef] [PubMed]
- Imtiaz, S.; Shield, K.D.; Roerecke, M.; Samokhvalov, A.V.; Lönnroth, K.; Rehm, J. Alcohol consumption as a risk factor for tuberculosis: Meta-analyses and burden of disease. Eur. Respir. J. 2017, 50, 1700216. [Google Scholar] [CrossRef] [PubMed]
- Afshar, B.; Carless, J.; Roche, A.; Balasegaram, S.; Anderson, C. Surveillance of tuberculosis (TB) cases attributable to relapse or reinfection in London, 2002–2015. PLoS ONE 2019, 14, e0211972. [Google Scholar] [CrossRef] [PubMed]

| Variable | Total 1434 | % | p-Value |
|---|---|---|---|
| Sex | |||
| Female | 565 | 39.40 | <0.001 |
| Male | 869 | 60.60 | |
| Age Group | |||
| <1 | 21 | 1.46 | <0.001 |
| 1 to 19 | 155 | 10.81 | |
| 20 to 39 | 628 | 43.79 | |
| 40 to 59 | 438 | 30.54 | |
| >60 | 192 | 13.39 | |
| Race | |||
| White | 163 | 11.37 | <0.001 |
| Black | 139 | 9.69 | |
| Yellow | 4 | 0.28 | |
| Parda | 1090 | 76.01 | |
| Indigenous | 1 | 0.07 | |
| Ignored | 37 | 2.58 | |
| Education | |||
| Illiterate | 17 | 1.19 | <0.001 |
| 1st to 4th incomplete elementary school | 143 | 9.97 | |
| 2nd to 4th complete elementary school | 66 | 4.60 | |
| 5th to 8th incomplete elementary school | 222 | 15.48 | |
| Complete elementary school | 100 | 6.97 | |
| Incomplete high school | 165 | 11.51 | |
| Complete high school | 286 | 19.94 | |
| Incomplete undergraduate education | 46 | 3.21 | |
| Complete undergraduate education | 53 | 3.70 | |
| Ignored | 269 | 18.76 | |
| Data does not apply | 67 | 4.67 | |
| Entry Type | |||
| New case | 1242 | 86.61 | <0.001 |
| Relapse | 71 | 4.95 | |
| Re-entry after abandonment | 35 | 2.44 | |
| Uncrown | 5 | 0.35 | |
| Transference | 81 | 5.65 | |
| Tuberculosis Type | |||
| Pulmonary | 1275 | 88.91 | <0.001 |
| Extrapulmonary | 141 | 9.83 | |
| Pulmonary + Extrapulmonary | 18 | 1.26 | |
| Chest X-ray | |||
| Suspect | 990 | 69.04 | <0.001 |
| Normal | 42 | 2.93 | |
| Other pathology | 11 | 0.77 | |
| Not performed | 391 | 27.26 | |
| Extrapulmonary Type | |||
| Pleural | 76 | 5.30 | |
| Others | 12 | 0.84 | |
| Peripheral ganglion | 43 | 3.00 | |
| Bone | 10 | 0.70 | <0.001 |
| Ocular | 1 | 0.07 | |
| Miliary | 9 | 0.63 | |
| Meningoencephalocele | 4 | 0.28 | |
| Cutaneous | 2 | 0.14 | |
| Laryngeal | 2 | 0.14 |
| Surveillance Quality Indicators | N | % | p-Value |
|---|---|---|---|
| Sputum Smear | |||
| Positive | 812 | 56.6 | <0.001 |
| Negative | 274 | 19.1 | |
| Not performed | 299 | 20.9 | |
| Does not apply | 49 | 3.4 | |
| Rapid Molecular Test | |||
| Detectable-Rifampicin susceptible | 285 | 19.9 | <0.001 |
| Detectable-Rifampicin resistant | 13 | 0.9 | |
| Undatable | 24 | 1.7 | |
| Inconclusive | 34 | 2.4 | |
| Not performed | 1074 | 74.9 | |
| Not filled | 4 | 0.3 | |
| Drug Susceptible Test | |||
| Not filled | 1329 | 92.7 | <0.001 |
| Resistant to other first-line drugs | 1 | 0.1 | |
| Susceptible | 6 | 0.4 | |
| Ongoing | 7 | 0.5 | |
| Not performed | 91 | 6.3 | |
| Culture | |||
| Positive | 103 | 7.2 | <0.001 |
| Negative | 58 | 4.0 | |
| Ongoing | 57 | 4.0 | |
| Not performed | 1216 | 84.8 | |
| Sputum Baciloscopy (6 Months) | |||
| Record not completed | 492 | 34.3 | <0.001 |
| Negative | 378 | 26.4 | |
| Not performed | 421 | 29.4 | |
| Not applied | 143 | 10.0 | |
| Sputum Baciloscopy (After 6 Months) | |||
| Record not completed | 876 | 61.1 | <0.001 |
| Negative | 145 | 10.1 | |
| Not performed | 270 | 18.8 | |
| Not applied | 143 | 10.0 | |
| Outcome Situation | |||
| Record not completed | 289 | 20.2 | <0.001 |
| Cure | 849 | 59.2 | |
| Primary Abandonment | 1 | 0.1 | |
| Abandonment | 132 | 9.2 | |
| Death by TB | 9 | 0.6 | |
| Death by other causes | 30 | 2.1 | |
| Transference | 101 | 7.0 | |
| Diagnostic change | 13 | 0.9 | |
| TB-DR | 8 | 0.6 | |
| Mudança de Esquema | 2 | 0.1 | |
| Variables | New Cases (1242) | % | Relapses (71) | % | * p-Value | # OR | & CI |
|---|---|---|---|---|---|---|---|
| Sex | 0.648 | ||||||
| Female | 498 | 40.10 | 26 | 36.62 | |||
| Male | 744 | 59.90 | 45 | 63.38 | |||
| Age Group | |||||||
| <1 | 20 | 1.61 | 0 | 0.00 | 0.520 | ||
| 1 to 19 | 138 | 11.11 | 4 | 5.63 | 0.123 | ||
| 20 to 39 | 530 | 42.67 | 35 | 49.30 | 0.331 | ||
| 40 to 59 | 380 | 30.60 | 23 | 32.39 | 0.851 | ||
| >60 | 174 | 14.01 | 9 | 12.68 | 0.889 | ||
| Race | |||||||
| White | 147 | 11.84 | 7 | 9.86 | 0.754 | ||
| Black | 117 | 9.42 | 8 | 11.27 | 0.758 | ||
| Yellow | 3 | 0.24 | 0 | 0.00 | 0.482 | ||
| Parda | 944 | 76.01 | 53 | 74.65 | 0.906 | ||
| Indigenous | 1 | 0.08 | 0 | 0.00 | 0.207 | ||
| Ignored | 30 | 2.42 | 3 | 4.23 | 0.597 | ||
| Education | |||||||
| Illiterate | 15 | 1.21 | 0 | 0.00 | 0.702 | ||
| Incomplete Elementary School: 1st to 4th series | 124 | 9.98 | 9 | 12.68 | 0.597 | ||
| Complete Elementary School: 2nd to 4th series | 49 | 3.95 | 6 | 8.45 | 0.164 | ||
| Incomplete Elementary School: 5th to 8th series | 180 | 14.49 | 19 | 26.76 | 0.009 | 2.1558 | 1.2454–3.7315 |
| Complete Elementary School | 92 | 7.41 | 5 | 7.04 | 0.905 | ||
| Incomplete High School | 150 | 12.08 | 6 | 8.45 | 0.465 | ||
| Complete High School | 252 | 20.29 | 12 | 16.90 | 0.589 | ||
| Incomplete Undergrad | 40 | 3.22 | 2 | 2.82 | 0.876 | ||
| Complete Undergrad | 51 | 4.11 | 2 | 2.82 | 0.818 | ||
| Ignored | 266 | 21.42 | 10 | 14.08 | 0.185 | ||
| Not applied | 23 | 1.85 | 0 | 0.00 | 0.435 | ||
| Form | |||||||
| Pulmonary | 1116 | 89.86 | 66 | 92.96 | 0.519 | ||
| Extrapulmonary | 112 | 9.02 | 5 | 7.04 | 0.723 | ||
| Pulmonary + Extrapulmonary | 14 | 1.13 | 0 | 0.00 | 0.746 | ||
| Chest X-ray | |||||||
| Suspect | 878 | 70.69 | 42 | 59.15 | 0.053 | 0.6021 | 0.3693–0.9815 |
| Normal | 38 | 3.06 | 1 | 1.41 | 0.646 | ||
| Other pathology | 9 | 0.72 | 1 | 1.41 | 0.954 | ||
| Not performed | 317 | 25.52 | 27 | 38.03 | 0.028 | 1.7906 | 1.0906–2.9399 |
| Extrapulmonary Types | |||||||
| Pleural | 63 | 5.07 | 1 | 1.41 | 0.215 | ||
| Other | 9 | 0.72 | 0 | 0.00 | 0.984 | ||
| Peripheral ganglion | 34 | 2.74 | 3 | 4.23 | 0.722 | ||
| Bone | 7 | 0.56 | 0 | 0.00 | 0.846 | ||
| Ocular | 0 | 0.00 | 1 | 1.41 | 0.207 | ||
| Miliary | 8 | 0.64 | 0 | 0.00 | 0.918 | ||
| Meningoencephalic | 1 | 0.08 | 0 | 0.00 | 0.207 | ||
| Cutaneous | 2 | 0.16 | 0 | 0.00 | 0.360 | ||
| Laryngeal | 2 | 0.16 | 0 | 0.00 | 0.360 |
| Variables | New Cases (1242) | % | Relapses (71) | % | * p-Value | # OR | & CI |
|---|---|---|---|---|---|---|---|
| HIV | 106 | 8.53 | 8 | 11.27 | 0.563 | ||
| Diabetes | 160 | 12.88 | 6 | 8.45 | 0.363 | ||
| Mental disease | 21 | 1.69 | 2 | 2.82 | 0.817 | ||
| Alcoholism | 126 | 10.14 | 11 | 15.49 | 0.217 | ||
| Others | 104 | 8.37 | 5 | 7.04 | 0.860 | ||
| Drugs | 78 | 6.28 | 8 | 11.27 | 0.192 | ||
| Smoking | 137 | 11.03 | 9 | 12.68 | 0.818 | ||
| Deprived of liberty | 52 | 4.19 | 9 | 12.68 | 0.002 | 3.3220 | 1.5656–7.0486 |
| Street situation | 7 | 0.56 | 0 | 0.00 | 0.846 | ||
| Immigrants | 4 | 0.32 | 0 | 0.00 | 0.588 | ||
| Health professionals | 23 | 1.85 | 0 | 0.00 | 0.435 | ||
| + DOT not performed | 853 | 68.68 | 63 | 88.73 | 0.001 | 3.5913 | 1.7043–7.5676 |
| Cure | 749 | 60.31 | 39 | 54.93 | 0.438 | ||
| Abandonment | 110 | 8.86 | 9 | 12.68 | 0.380 | ||
| Death by TB | 9 | 0.72 | 0 | 0.00 | 0.984 | ||
| TB-DR | 5 | 0.40 | 1 | 1.41 | 0.768 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garcez, J.C.D.; Sardinha, D.M.; Conceição, E.C.; Costa, G.F.; Sousa, I.F.R.; Mesquita, C.R.; Carmo, W.C.d.; Rodrigues, Y.C.; Lima, L.N.G.C.; Lima, K.V.B. Surveillance Quality Indicators Highlight the Need for Improving Tuberculosis Diagnostics and Monitoring in a Hyperendemic Area of the Brazilian Amazon Region. Trop. Med. Infect. Dis. 2022, 7, 165. https://doi.org/10.3390/tropicalmed7080165
Garcez JCD, Sardinha DM, Conceição EC, Costa GF, Sousa IFR, Mesquita CR, Carmo WCd, Rodrigues YC, Lima LNGC, Lima KVB. Surveillance Quality Indicators Highlight the Need for Improving Tuberculosis Diagnostics and Monitoring in a Hyperendemic Area of the Brazilian Amazon Region. Tropical Medicine and Infectious Disease. 2022; 7(8):165. https://doi.org/10.3390/tropicalmed7080165
Chicago/Turabian StyleGarcez, Juliana Conceição Dias, Daniele Melo Sardinha, Emilyn Costa Conceição, Gabriel Fazzi Costa, Ianny Ferreira Raiol Sousa, Cristal Ribeiro Mesquita, Wellington Caldas do Carmo, Yan Corra Rodrigues, Luana Nepomuceno Gondim Costa Lima, and Karla Valéria Batista Lima. 2022. "Surveillance Quality Indicators Highlight the Need for Improving Tuberculosis Diagnostics and Monitoring in a Hyperendemic Area of the Brazilian Amazon Region" Tropical Medicine and Infectious Disease 7, no. 8: 165. https://doi.org/10.3390/tropicalmed7080165
APA StyleGarcez, J. C. D., Sardinha, D. M., Conceição, E. C., Costa, G. F., Sousa, I. F. R., Mesquita, C. R., Carmo, W. C. d., Rodrigues, Y. C., Lima, L. N. G. C., & Lima, K. V. B. (2022). Surveillance Quality Indicators Highlight the Need for Improving Tuberculosis Diagnostics and Monitoring in a Hyperendemic Area of the Brazilian Amazon Region. Tropical Medicine and Infectious Disease, 7(8), 165. https://doi.org/10.3390/tropicalmed7080165









