Antimicrobial Stewardship in Tropical Infectious Diseases: Focusing on Dengue and Malaria
Abstract
1. Introduction
2. Acute Undifferentiated Febrile Illness
2.1. Causes
2.2. Antibiotic Use in AUFI
2.3. Challenges in Diagnosis of AUFI Aetiology
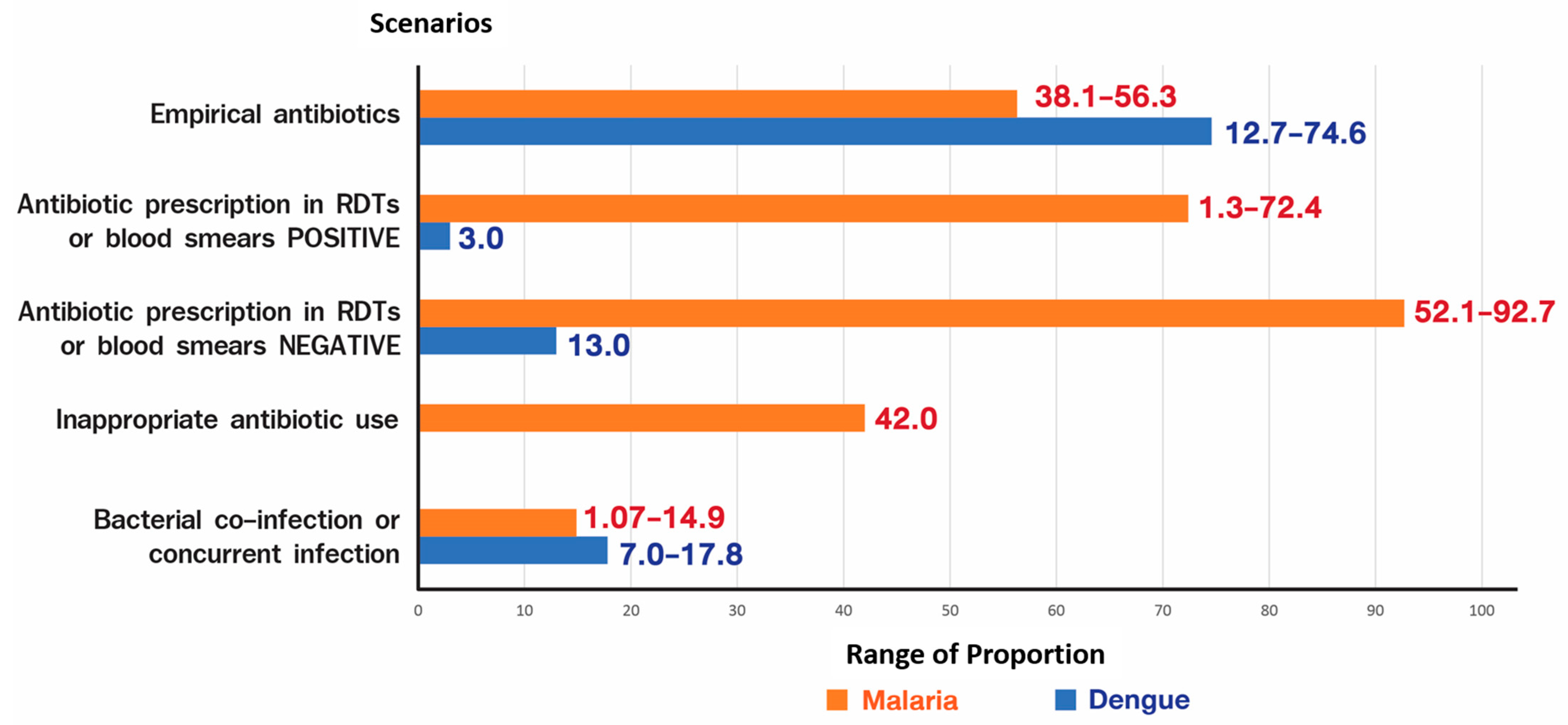
2.4. Antimicrobial Use in Malaria and Dengue
2.5. Bacterial Co-Infection in Tropical Infectious Diseases
3. Antimicrobial Stewardship
3.1. Overview of AMS
3.2. AMS in Tropical Infectious Diseases
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | Antimicrobial resistance |
| AMS | Antimicrobial stewardship |
| AUFI | Acute undifferentiated febrile illness |
| CRP | C-reactive protein |
| HIC | High-income countries |
| HIV | Human immunodeficiency virus |
| LMIC | Low- and middle-income countries |
| MDR | Multidrug resistance |
| RDTs | Rapid diagnostic tests |
| WHO | World Health Organisation |
References
- Wangdi, K.; Kasturiaratchi, K.; Nery, S.V.; Lau, C.L.; Gray, D.J.; Clements, A.C.A. Diversity of infectious aetiologies of acute undifferentiated febrile illnesses in south and Southeast Asia: A systematic review. BMC Infect. Dis. 2019, 19, 577. [Google Scholar] [CrossRef] [PubMed]
- Kularatne, S.A.; Dalugama, C. Dengue infection: Global importance, immunopathology and management. Clin. Med. 2022, 22, 9. [Google Scholar] [CrossRef] [PubMed]
- Luvira, V.; Silachamroon, U.; Piyaphanee, W.; Lawpoolsri, S.; Chierakul, W.; Leaungwutiwong, P.; Thawornkuno, C.; Wattanagoon, Y. Etiologies of Acute Undifferentiated Febrile Illness in Bangkok, Thailand. Am. J. Trop. Med. Hyg. 2019, 100, 622–629. [Google Scholar] [CrossRef]
- Stoler, J.; Awandare, G.A. Febrile illness diagnostics and the malaria-industrial complex: A socio-environmental perspective. BMC Infect. Dis. 2016, 16, 683. [Google Scholar] [CrossRef] [PubMed]
- Southeast Asia Infectious Disease Clinical Research Network. Causes and outcomes of sepsis in southeast Asia: A multinational multicentre cross-sectional study. Lancet Glob. Health 2017, 5, e157–e167. [Google Scholar] [CrossRef]
- Sié, A.; Ouattara, M.; Bountogo, M.; Dah, C.; Compaoré, G.; Boudo, V.; Lebas, E.; Brogdon, J.; Nyatigo, F.; Arnold, B.F.; et al. Indication for Antibiotic Prescription Among Children Attending Primary Healthcare Services in Rural Burkina Faso. Clin. Infect. Dis. 2021, 73, 1288–1291. [Google Scholar] [CrossRef] [PubMed]
- Landstedt, K.; Sharma, A.; Johansson, F.; Stålsby Lundborg, C.; Sharma, M. Antibiotic prescriptions for inpatients having non-bacterial diagnosis at medicine departments of two private sector hospitals in Madhya Pradesh, India: A cross-sectional study. BMJ Open 2017, 7, e012974. [Google Scholar] [CrossRef] [PubMed]
- Hooft, A.M.; Ndenga, B.; Mutuku, F.; Otuka, V.; Ronga, C.; Chebii, P.K.; Maina, P.W.; Jembe, Z.; Lee, J.; Vu, D.M.; et al. High Frequency of Antibiotic Prescription in Children With Undifferentiated Febrile Illness in Kenya. Clin. Infect. Dis. 2021, 73, e2399–e2406. [Google Scholar] [CrossRef]
- Godman, B.; Egwuenu, A.; Haque, M.; Malande, O.O.; Schellack, N.; Kumar, S.; Saleem, Z.; Sneddon, J.; Hoxha, I.; Islam, S.; et al. Strategies to Improve Antimicrobial Utilization with a Special Focus on Developing Countries. Life 2021, 11, 528. [Google Scholar] [CrossRef]
- Marks, F.; Liu, J.; Soura, A.B.; Gasmelseed, N.; Operario, D.J.; Grundy, B.; Wieser, J.; Gratz, J.; Meyer, C.G.; Im, J.; et al. Pathogens That Cause Acute Febrile Illness Among Children and Adolescents in Burkina Faso, Madagascar, and Sudan. Clin. Infect. Dis. 2021, 73, 1338–1345. [Google Scholar] [CrossRef]
- Kaboré, B.; Post, A.; Lompo, P.; Bognini, J.D.; Diallo, S.; Kam, B.T.D.; Rahamat-Langendoen, J.; Wertheim, H.F.L.; van Opzeeland, F.; Langereis, J.D.; et al. Aetiology of acute febrile illness in children in a high malaria transmission area in West Africa. Clin. Microbiol. Infect. 2021, 27, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Popoola, O.; Kehinde, A.; Ogunleye, V.; Adewusi, O.J.; Toy, T.; Mogeni, O.D.; Aroyewun, E.O.; Agbi, S.; Adekanmbi, O.; Adepoju, A.; et al. Bacteremia Among Febrile Patients Attending Selected Healthcare Facilities in Ibadan, Nigeria. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2019, 69, S466–S473. [Google Scholar] [CrossRef] [PubMed]
- Hopkins, H.; Bruxvoort, K.J.; Cairns, M.E.; Chandler, C.I.R.; Leurent, B.; Ansah, E.K.; Baiden, F.; Baltzell, K.A.; Björkman, A.; Burchett, H.E.D.; et al. Impact of introduction of rapid diagnostic tests for malaria on antibiotic prescribing: Analysis of observational and randomised studies in public and private healthcare settings. BMJ 2017, 356, j1054. [Google Scholar] [CrossRef] [PubMed]
- Piedrahita, L.D.; Agudelo, I.Y.; Trujillo, A.I.; Ramírez, R.E.; Osorio, J.E.; Restrepo, B.N. Evaluation of commercially available assays for diagnosis of acute dengue in schoolchildren during an epidemic period in Medellin, Colombia. Am. J. Trop. Med. Hyg. 2016, 95, 315e21. [Google Scholar] [CrossRef]
- Lee, J.; Kim, Y.E.; Kim, H.Y.; Sinniah, M.; Chong, C.K.; Song, H.O. Enhanced performance of an innovative dengue IgG/IgM rapid diagnostic test using an anti-dengue EDI monoclonal antibody and dengue virus antigen. Sci. Rep. 2015, 5, 18077. [Google Scholar] [CrossRef]
- Pal, S.; Dauner, A.L.; Valks, A.; Forshey, B.M.; Long, K.C.; Thaisomboonsuk, B.; Sierra, G.; Picos, V.; Talmage, S.; Morrison, A.C.; et al. Multicountry prospective clinical evaluation of two enzyme-linked immunosorbent assays and two rapid diagnostic tests for diagnosing dengue fever. J. Clin. Microbiol. 2015, 53, 1092e102. [Google Scholar] [CrossRef]
- Badiane, A.; Thwing, J.; Williamson, J.; Rogier, E.; Diallo, M.A.; Ndiaye, D. Sensitivity and specificity for malaria classification of febrile persons by rapid diagnostic test, microscopy, parasite DNA, histidine-rich protein 2, and IgG: Dakar, Senegal 2015. Int. J. Infect. Dis. 2022, 121, 92–97. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Rapid Influenza Diagnostic Tests; Rapid Influenza Diagnostic Tests|CDC; U.S. Department of Health and Human Services: Atlanta, GA, USA, 2016.
- Robinson, M.L.; Kadam, D.; Kagal, A.; Khadse, S.; Kinikar, A.; Valvi, C.; Basavaraj, A.; Bharadwaj, R.; Marbaniang, I.; Kanade, S.; et al. Antibiotic Utilization and the Role of Suspected and Diagnosed Mosquito-borne Illness Among Adults and Children With Acute Febrile Illness in Pune, India. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2018, 66, 1602–1609. [Google Scholar] [CrossRef]
- Anand Paramadhas, B.D.; Tiroyakgosi, C.; Mpinda-Joseph, P.; Morokotso, M.; Matome, M.; Sinkala, F.; Gaolebe, M.; Malone, B.; Molosiwa, E.; Shanmugam, M.G.; et al. Point prevalence study of antimicrobial use among hospitals across Botswana; findings and implications. Expert Rev. Anti-Infect. Ther. 2019, 17, 535–546. [Google Scholar] [CrossRef]
- Okoth, C.; Opanga, S.; Okalebo, F.; Oluka, M.; Baker Kurdi, A.; Godman, B. Point prevalence survey of antibiotic use and resistance at a referral hospital in Kenya: Findings and implications. Hosp. Pract. 2018, 46, 128–136. [Google Scholar] [CrossRef]
- Guterres, H.; Nelwan, E.J.; Chen, L.K.; Nugroho, P. Point prevalence survey of antibiotics use among inpatient in national referral hospital in Indonesia. Int. J. Infect. Dis. 2020, 101, 93. [Google Scholar] [CrossRef]
- Alothman, A.; Al Thaqafi, A.; Al Ansary, A.; Zikri, A.; Fayed, A.; Khamis, F.; Al Salman, J.; Al Dabal, L.; Khalife, N.; AlMusawi, T.; et al. Prevalence of infections and antimicrobial use in the acute-care hospital setting in the Middle East: Results from the first point-prevalence survey in the region. Int. J. Infect. Dis. 2020, 101, 249–258. [Google Scholar] [CrossRef]
- Akhloufi, H.; Streefkerk, R.H.; Melles, D.C.; de Steenwinkel, J.E.; Schurink, C.A.; Verkooijen, R.P.; van der Hoeven, C.P.; Verbon, A. Point prevalence of appropriate antimicrobial therapy in a Dutch university hospital. Eur. J. Clin. Microbiol. Infect. Dis. 2015, 34, 1631–1637. [Google Scholar] [CrossRef]
- Atif, M.; Azeem, M.; Saqib, A.; Scahill, S. Investigation of antimicrobial use at a tertiary care hospital in Southern Punjab, Pakistan using WHO methodology. Antimicrob. Resist. Infect. Control. 2017, 6, 41. [Google Scholar] [CrossRef]
- Baig, M.T.; Sial, A.A.; Huma, A.; Ahmed, M.; Shahid, U.; Syed, N. Irrational antibiotic prescribing practice among children in critical care of tertiary hospitals. Pak. J. Pharm. Sci. 2017, 30, 1483–1489. [Google Scholar]
- Dumartin, C.; L’Hériteau, F.; Péfau, M.; Bertrand, X.; Jarno, P.; Boussat, S.; Angora, P.; Lacavé, L.; Saby, K.; Savey, A.; et al. Antibiotic use in 530 French hospitals: Results from a surveillance network at hospital and ward levels in 2007. J. Antimicrob. Chemother 2010, 65, 2028–2036. [Google Scholar] [CrossRef]
- Ngamprasertchai, T.; Hanboonkunupakarn, B.; Piyaphanee, W. Rickettsiosis in Southeast Asia: Summary for International Travellers during the COVID-19 Pandemic. Trop. Med. Infect. Dis. 2022, 7, 18. [Google Scholar] [CrossRef]
- Patangia, D.V.; Ryan, C.A.; Dempsey, E.; Ross, R.P.; Stanton, C. Impact of antibiotics on the human microbiome and consequences for host health. MicrobiologyOpen 2022, 11, e1260. [Google Scholar] [CrossRef]
- Nunthavichitra, S.; Prapaso, S.; Luvira, V.; Muangnoicharoen, S.; Leaungwutiwong, P.; Piyaphanee, W. Case Report: COVID-19 Presenting as Acute Undifferentiated Febrile Illness-A Tropical World Threat. Am. J. Trop. Med. Hyg. 2020, 103, 83–85. [Google Scholar] [CrossRef]
- Iroh Tam, P.-Y.; Obaro, S.K.; Storch, G. Challenges in the Etiology and Diagnosis of Acute Febrile Illness in Children in Low- and Middle-Income Countries. J. Pediatric. Infect. Dis. Soc. 2016, 5, 190–205. [Google Scholar] [CrossRef]
- Grundy, B.S.; Houpt, E.R. Opportunities and challenges to accurate diagnosis and management of acute febrile illness in adults and adolescents: A review. Acta Trop. 2022, 227, 106286. [Google Scholar] [CrossRef] [PubMed]
- Cooke, J.; Butler, C.; Hopstaken, R.; Dryden, M.S.; McNulty, C.; Hurding, S.; Moore, M.; Livermore, D.M. Narrative review of primary care point-of-care testing (POCT) and antibacterial use in respiratory tract infection (RTI). BMJ Open Respir. Res. 2015, 2, e000086. [Google Scholar] [CrossRef] [PubMed]
- Wangrangsimakul, T.; Althaus, T.; Mukaka, M.; Kantipong, P.; Wuthiekanun, V.; Chierakul, W.; Blacksell, S.D.; Day, N.P.; Laongnualpanich, A.; Paris, D.H. Causes of acute undifferentiated fever and the utility of biomarkers in Chiangrai, northern Thailand. PLOS Negl. Trop. Dis. 2018, 12, e0006477. [Google Scholar] [CrossRef] [PubMed]
- Thanachartwet, V.; Desakorn, V.; Sahassananda, D.; Jittmittraphap, A.; Oer-Areemitr, N.; Osothsomboon, S.; Surabotsophon, M.; Wattanathum, A. Serum Procalcitonin and Peripheral Venous Lactate for Predicting Dengue Shock and/or Organ Failure: A Prospective Observational Study. PLoS Negl. Trop. Dis. 2016, 10, e0004961. [Google Scholar] [CrossRef] [PubMed]
- Tello-Cajiao, M.E.; Osorio, L. Impact of Dengue Rapid Diagnostic Tests on the Prescription of Antibiotics and Anti-Inflammatory Drugs by Physicians in an Endemic Area in Colombia. Am. J. Trop. Med. Hyg. 2019, 101, 696–704. [Google Scholar] [CrossRef]
- Leslie, T.; Mikhail, A.; Mayan, I.; Anwar, M.; Bakhtash, S.; Nader, M.; Chandler, C.; Whitty, C.J.M.; Rowland, M. Overdiagnosis and mistreatment of malaria among febrile patients at primary healthcare level in Afghanistan: Observational study. BMJ Br. Med. J. 2012, 345, e4389. [Google Scholar] [CrossRef]
- D’Acremont, V.; Kahama-Maro, J.; Swai, N.; Mtasiwa, D.; Genton, B.; Lengeler, C. Reduction of anti-malarial consumption after rapid diagnostic tests implementation in Dar es Salaam: A before-after and cluster randomized controlled study. Malar. J. 2011, 10, 107. [Google Scholar] [CrossRef]
- Bienvenu, A.-L.; Djimdé, A.; Picot, S. Antimalarial stewardship programs are urgently needed for malaria elimination: A perspective. Parasite 2019, 26, 16. [Google Scholar] [CrossRef]
- Njozi, M.; Amuri, M.; Selemani, M.; Masanja, I.; Kigahe, B.; Khatib, R.; Kajungu, D.; Abdula, S.; Dodoo, A.N. Predictors of antibiotics co-prescription with antimalarials for patients presenting with fever in rural Tanzania. BMC Public Health 2013, 13, 1097. [Google Scholar] [CrossRef]
- Severe Malaria. Trop. Med. Int. Health 2014, 19 (Suppl. 1), 7–131. [CrossRef]
- Abuya, T.O.; Mutemi, W.; Karisa, B.; Ochola, S.A.; Fegan, G.; Marsh, V. Use of over-the-counter malaria medicines in children and adults in three districts in Kenya: Implications for private medicine retailer interventions. Malar. J. 2007, 6, 57. [Google Scholar] [CrossRef]
- Premaratna, R.; Dissanayake, D.; Silva, F.H.; Dassanayake, M.; de Silva, H.J. Secondary bacteraemia in adult patients with prolonged dengue fever. Ceylon Med. J. 2015, 60, 10–12. [Google Scholar] [CrossRef]
- Lee, I.K.; Liu, J.W.; Yang, K.D. Clinical characteristics and risk factors for concurrent bacteremia in adults with dengue hemorrhagic fever. Am. J. Trop. Med. Hyg. 2005, 72, 221–226. [Google Scholar] [CrossRef]
- Sunil, T.; Alexandra, B.; Tanu, M.; Ali, M.M.; Neha, A.; Navin, B. Bacterial sepsis in dengue fever—A paediatric perspective. Trop. Doct. 2021, 51, 371–375. [Google Scholar] [CrossRef]
- Adrizain, R.; Setiabudi, D.; Chairulfatah, A. The inappropriate use of antibiotics in hospitalized dengue virus-infected children with presumed concurrent bacterial infection in teaching and private hospitals in Bandung, Indonesia. PLoS Negl. Trop. Dis. 2019, 13, e0007438. [Google Scholar] [CrossRef]
- See, K.C.; Phua, J.; Yeo, L.; Yip, H.S.; Lim, T.K. Identification of Concurrent Bacterial Infection in Adult Patients with Dengue. Am. J. Trop. Med. Hyg. 2013, 89, 804–810. [Google Scholar] [CrossRef]
- Phu, N.H.; Day, N.P.J.; Tuan, P.Q.; Mai, N.T.H.; Chau, T.T.H.; Van Chuong, L.; Vinh, H.; Loc, P.P.; Sinh, D.X.; Hoa, N.T.T.; et al. Concomitant Bacteremia in Adults With Severe Falciparum Malaria. Clin. Infect. Dis. 2020, 71, e465–e470. [Google Scholar] [CrossRef]
- Aung, N.M.; Nyein, P.P.; Htut, T.Y.; Htet, Z.W.; Kyi, T.T.; Anstey, N.M.; Kyi, M.M.; Hanson, J. Antibiotic Therapy in Adults with Malaria (ANTHEM): High Rate of Clinically Significant Bacteremia in Hospitalized Adults Diagnosed with Falciparum Malaria. Am. J. Trop. Med. Hyg. 2018, 99, 688–696. [Google Scholar] [CrossRef]
- Nyein, P.P.; Aung, N.M.; Kyi, T.T.; Htet, Z.W.; Anstey, N.M.; Kyi, M.M.; Hanson, J. High Frequency of Clinically Significant Bacteremia in Adults Hospitalized With Falciparum Malaria. Open Forum. Infect. Dis. 2016, 3, ofw028. [Google Scholar] [CrossRef]
- Yan, J.; Li, N.; Wei, X.; Li, P.; Zhao, Z.; Wang, L.; Li, S.; Li, X.; Wang, Y.; Li, S.; et al. Performance of two rapid diagnostic tests for malaria diagnosis at the China-Myanmar border area. Malar. J. 2013, 12, 73. [Google Scholar] [CrossRef]
- Mbabazi, P.; Hopkins, H.; Osilo, E.; Kalungu, M.; Byakika-Kibwika, P.; Kamya, M.R. Accuracy of two malaria rapid diagnostic tests (RDTS) for initial diagnosis and treatment monitoring in a high transmission setting in Uganda. Am. J. Trop. Med. Hyg. 2015, 92, 530–536. [Google Scholar] [CrossRef] [PubMed]
- Luo, R.; Fongwen, N.; Kelly-Cirino, C.; Harris, E.; Wilder-Smith, A.; Peeling, R.W. Rapid diagnostic tests for determining dengue serostatus: A systematic review and key informant interviews. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2019, 25, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Stewardship—APIC. Available online: https://apic.org/professional-practice/practice-resources/antimicrobial-stewardship/ (accessed on 23 July 2022).
- Dyar, O.J.; Huttner, B.; Schouten, J.; Pulcini, C. What is antimicrobial stewardship? Clin. Microbiol. Infect. 2017, 23, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Goff, D.A. Antimicrobial stewardship: Bridging the gap between quality care and cost. Curr. Opin. Infect. Dis. 2011, 24 (Suppl. 1), S11–S20. [Google Scholar] [CrossRef]
- Tattevin, P.; Levy Hara, G.; Toumi, A.; Enani, M.; Coombs, G.; Voss, A.; Wertheim, H.; Poda, A.; Daoud, Z.; Laxminarayan, R.; et al. Advocacy for Increased International Efforts for Antimicrobial Stewardship Actions in Low-and Middle-Income Countries on Behalf of Alliance for the Prudent Use of Antimicrobials (APUA), Under the Auspices of the International Society of Antimicrobial Chemotherapy (ISAC). Front. Med. 2020, 7, 503. [Google Scholar] [CrossRef]
- Cox, J.A.; Vlieghe, E.; Mendelson, M.; Wertheim, H.; Ndegwa, L.; Villegas, M.V.; Gould, I.; Levy Hara, G. Antibiotic stewardship in low- and middle-income countries: The same but different? Clin. Microbiol. Infect. 2017, 23, 812–818. [Google Scholar] [CrossRef]
- Ashiru-Oredope, D.; Budd, E.L.; Bhattacharya, A.; Din, N.; McNulty, C.A.M.; Micallef, C.; Ladenheim, D.; Beech, E.; Murdan, S.; Hopkins, S.; et al. Implementation of antimicrobial stewardship interventions recommended by national toolkits in primary and secondary healthcare sectors in England: TARGET and Start Smart Then Focus. J. Antimicrob. Chemother. 2016, 71, 1408–1414. [Google Scholar] [CrossRef]
- Kpokiri, E.E.; Taylor, D.G.; Smith, F.J. Development of Antimicrobial Stewardship Programmes in Low and Middle-Income Countries: A Mixed-Methods Study in Nigerian Hospitals. Antibiotics 2020, 9, 204. [Google Scholar] [CrossRef]
- Adegbite, B.R.; Edoa, J.R.; Schaumburg, F.; Alabi, A.S.; Adegnika, A.A.; Grobusch, M.P. Knowledge and perception on antimicrobial resistance and antibiotics prescribing attitude among physicians and nurses in Lambaréné region, Gabon: A call for setting-up an antimicrobial stewardship program. Antimicrob. Resist. Infect. Control. 2022, 11, 44. [Google Scholar] [CrossRef]
- Krezanoski, P.J.; Roh, M.E.; Rek, J.; Nankabirwa, J.I.; Arinaitwe, E.; Staedke, S.G.; Nayiga, S.; Hsiang, M.S.; Smith, D.; Kamya, M.; et al. Marked reduction in antibiotic usage following intensive malaria control in a cohort of Ugandan children. BMC Med. 2021, 19, 294. [Google Scholar] [CrossRef]
- Means, A.R.; Weaver, M.R.; Burnett, S.M.; Mbonye, M.K.; Naikoba, S.; McClelland, R.S. Correlates of Inappropriate Prescribing of Antibiotics to Patients with Malaria in Uganda. PLoS ONE 2014, 9, e90179. [Google Scholar] [CrossRef]
- Rammohan, S.; Bhandare, B.; Adarsh, E.A.; Satyanarayana, V. The prescribing pattern for the management of dengue fever in pediatric patients of a tertiary care hospital: An observational study. Int. J. Basic Clin. Pharmacol. 2018, 7, 2384–2388. [Google Scholar] [CrossRef][Green Version]
- Rani, U.; Kamath, S.G.; Varun, H.V.; Aithal, S.; Patil, U. Prescribing patterns in Dengue fever in paediatric patients in a tertiary care hospital: A retrospective cross sectional study. Int. J. Pharm. Sci. Rev. Res. 2014, 24, 112–118. [Google Scholar]
- Sandopa, D.; Nethi, S.K.; Sreeram, S.C.; Vijay, N.K.G.; Biradavolu, V.; Kakimani, J.V. Prescribing antibiotics to pediatric dengue: Increasing risk of bacterial resistance. Paediatr. Indones. 2018, 58, 53. [Google Scholar] [CrossRef]
- Chilongola, J.; Msoka, E.; Juma, A.; Kituma, E.; Kwigizile, E.; Nyombi, B. Antibiotics prescription practices for provisional malaria cases in three hospitals in Moshi, northern Tanzania. Tanzan. J. Health Res. 2015, 17. [Google Scholar] [CrossRef]
- Ndhlovu, M.; Nkhama, E.; Miller, J.M.; Hamer, D.H. Antibacterial prescribing practices for patients with fever in the transition from presumptive treatment of malaria to “confirm and treat” in Zambia: A cross sectional study. Trop. Med. Int. Health 2015, 20, 1696–1706. [Google Scholar] [CrossRef]
- Batwala, V.; Magnussen, P.; Nuwaha, F. Antibiotic use among patients with febrile illness in a low malaria endemicity setting in Uganda. Malar. J. 2011, 10, 377. [Google Scholar] [CrossRef]
- Bonko, M.D.A.; Kiemde, F.; Tahita, M.; Lompo, P.; Some, A.M.; Tinto, H.; Van Hensbroek, M.B.; Mens, P.F.; Schallig, H.D.F.H. The effect of malaria rapid diagnostic tests results on antimicrobial prescription practices of health care workers in Burkina Faso. Ann. Clin. Microbiol. Antimicrob. 2019, 18, 5. [Google Scholar] [CrossRef]
| Diseases | Laboratory Diagnosis (CDC) | Rapid Diagnostic Tests (RDTs) | Specific Treatment | |
|---|---|---|---|---|
| Sensitivity | Specificity | |||
| Dengue [14,15,16] |
| 26.9–96.7 | 58.3–100 | None |
| Malaria [17] |
| 98.37–99.10 | 45.47–93.33 | Antimalarial agents |
| Influenza [18] |
| 10–80 | 85–100 | Antiviral agents |
| Diagnosis |
|---|
|
| Treatment |
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siribhadra, A.; Ngamprasertchai, T.; Rattanaumpawan, P.; Lawpoolsri, S.; Luvira, V.; Pitisuttithum, P. Antimicrobial Stewardship in Tropical Infectious Diseases: Focusing on Dengue and Malaria. Trop. Med. Infect. Dis. 2022, 7, 159. https://doi.org/10.3390/tropicalmed7080159
Siribhadra A, Ngamprasertchai T, Rattanaumpawan P, Lawpoolsri S, Luvira V, Pitisuttithum P. Antimicrobial Stewardship in Tropical Infectious Diseases: Focusing on Dengue and Malaria. Tropical Medicine and Infectious Disease. 2022; 7(8):159. https://doi.org/10.3390/tropicalmed7080159
Chicago/Turabian StyleSiribhadra, Ashley, Thundon Ngamprasertchai, Pinyo Rattanaumpawan, Saranath Lawpoolsri, Viravarn Luvira, and Punnee Pitisuttithum. 2022. "Antimicrobial Stewardship in Tropical Infectious Diseases: Focusing on Dengue and Malaria" Tropical Medicine and Infectious Disease 7, no. 8: 159. https://doi.org/10.3390/tropicalmed7080159
APA StyleSiribhadra, A., Ngamprasertchai, T., Rattanaumpawan, P., Lawpoolsri, S., Luvira, V., & Pitisuttithum, P. (2022). Antimicrobial Stewardship in Tropical Infectious Diseases: Focusing on Dengue and Malaria. Tropical Medicine and Infectious Disease, 7(8), 159. https://doi.org/10.3390/tropicalmed7080159











