Temporal and Spatial Analysis Techniques as Potential Tools for Combating the HIV Epidemic among Young Brazilian Amazonian People: An Ecological Study
Abstract
:1. Introduction
2. Materials and Methods
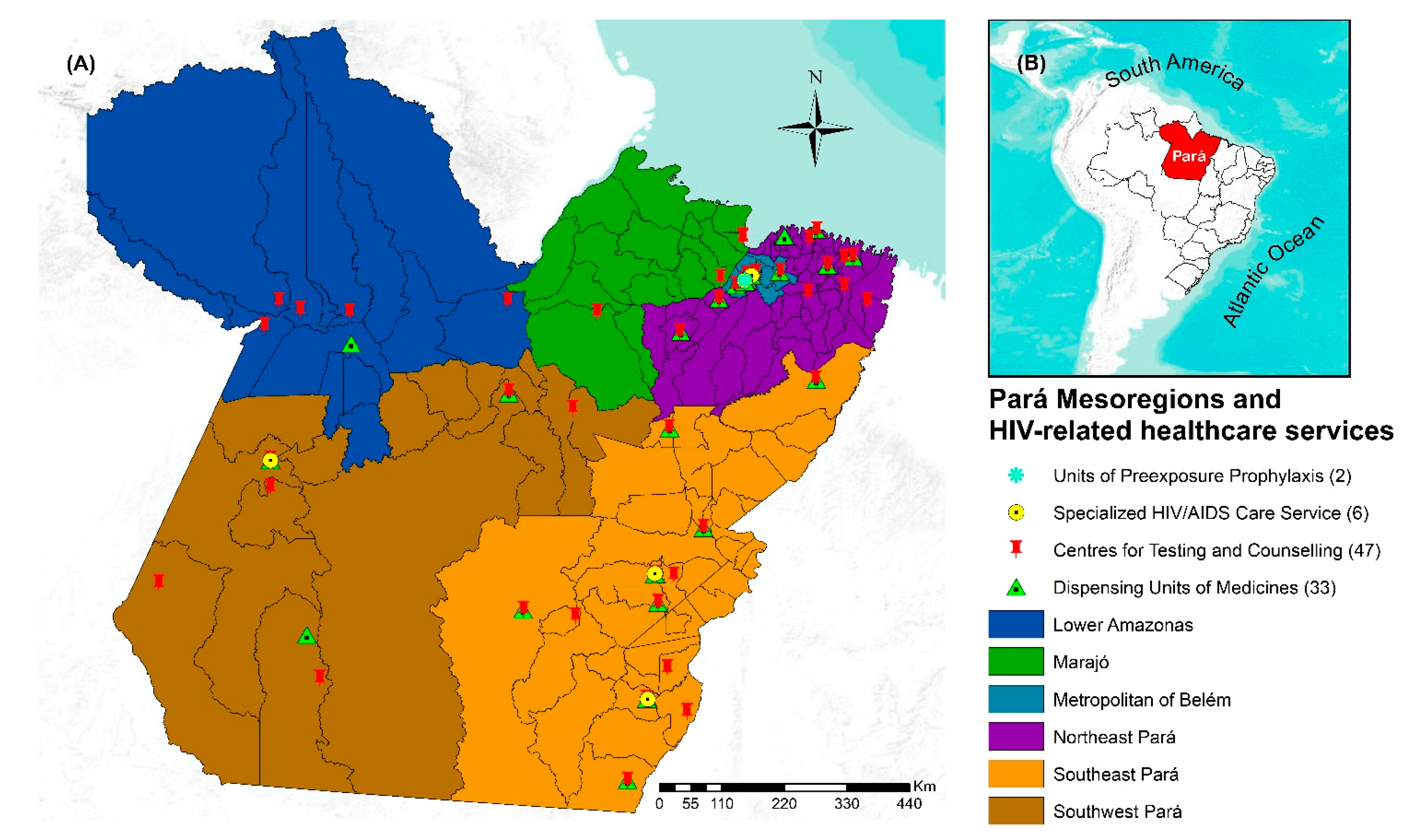
2.1. Study Settings
2.2. Study Data Set
2.3. Statistical Methods
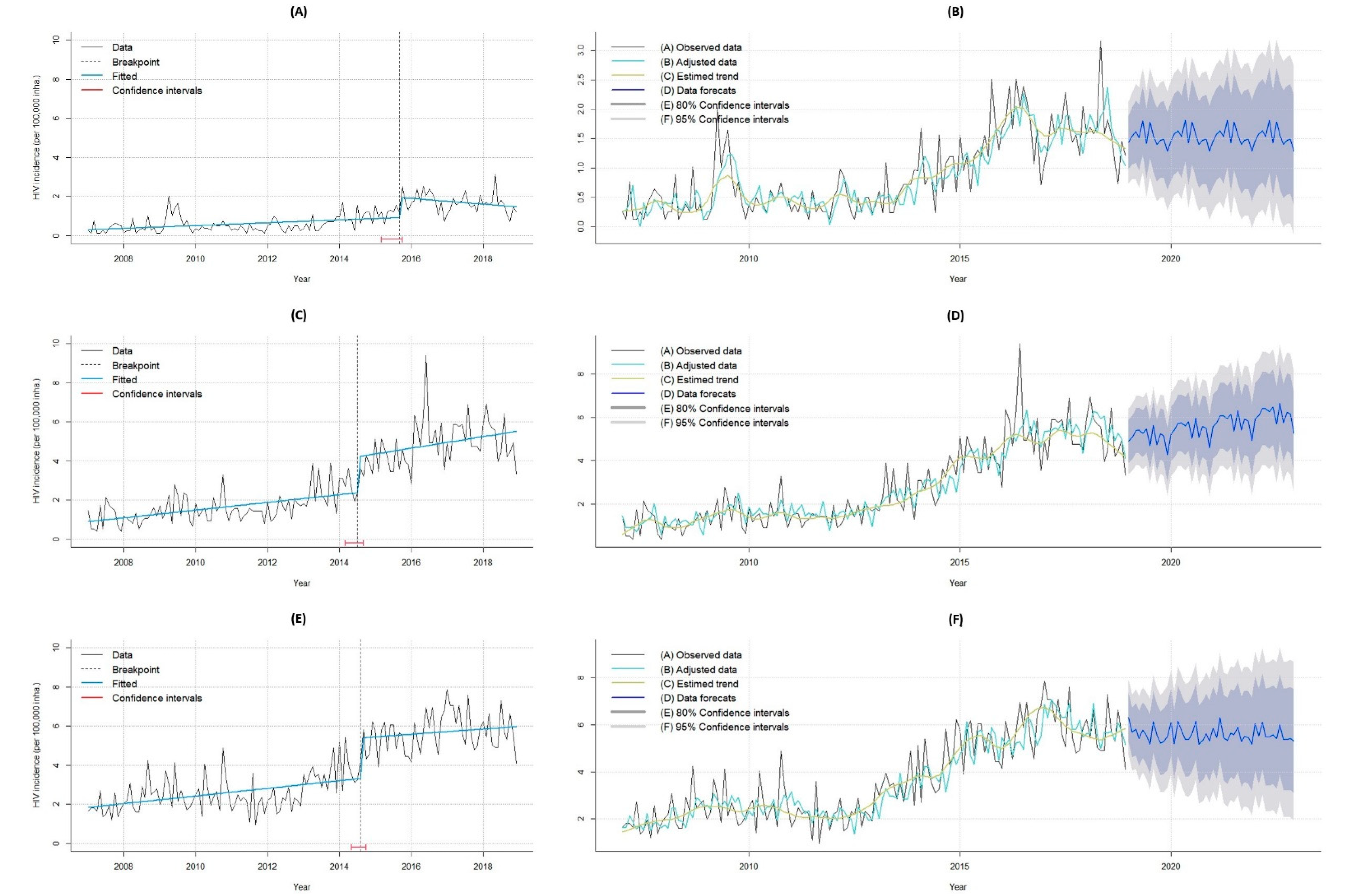
2.3.1. Temporal Analysis
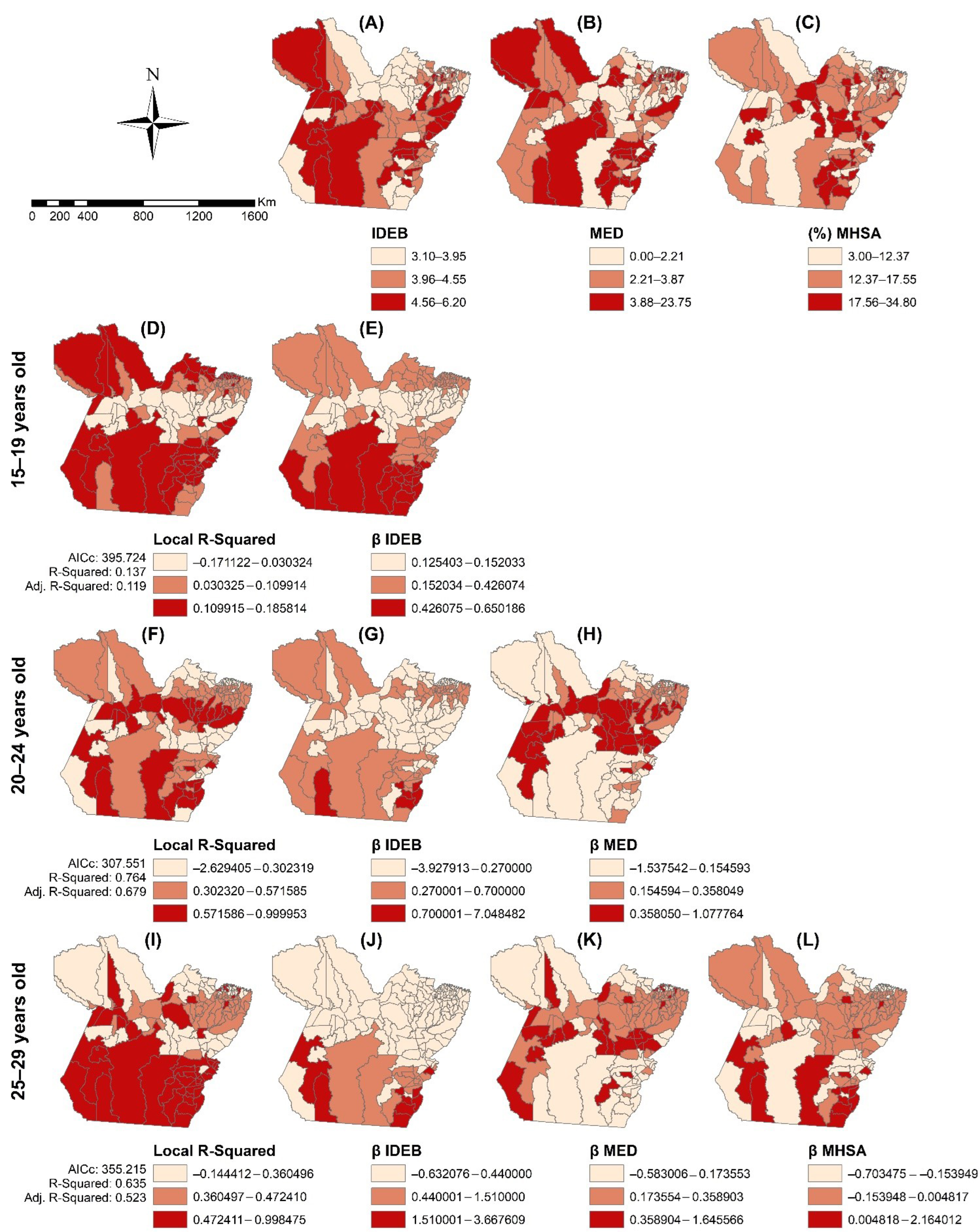
2.3.2. Spatial Analysis
2.4. Ethics
3. Results
4. Discussion
4.1. Temporal Analyses
4.2. Spatial Analyses
4.3. Study Limitation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- UNAIDS. Young People and HIV; UNAIDS: Geneva, Switzerland, 2021; Available online: https://www.unaids.org/sites/default/files/media_asset/young-people-and-hiv_en.pdf (accessed on 10 March 2022).
- UNAIDS. 90-90-90 Uma Meta Ambiciosa de Tratamento para Contribuir para o Fim da Epidemia de AIDS; UNAIDS: Geneva, Switzerland, 2015; Available online: https://unaids.org.br/wp-content/uploads/2015/11/2015_11_20_UNAIDS_TRATAMENTO_META_PT_v4_GB.pdf (accessed on 10 March 2022).
- Brazil. Presidência da República. Lei n. 12852, de 5 de Agosto de 2013. Institui o Estatuto da Juventude e Dispõe Sobre os Direitos dos Jovens, os Princípios e Diretrizes das Políticas Públicas de Juventude e o Sistema Nacional de Juventude. Diário Oficial da União, Brasília(DF) 2013 Ago 6; Seção 1. Available online: http://www.planalto.gov.br/ccivil_03/_ato2011-2014/2013/lei/l12852.htm (accessed on 10 March 2022).
- Brazil. Ministério da Saúde. Secretaria de Vigilância em Saúde; Departamento de Vigilância. Boletim Epidemiológico HIV/Aids 2021. Brasília/DF. 2021. Available online: http://www.aids.gov.br/pt-br/taxonomy/term/595 (accessed on 10 March 2022).
- Saffier, I.P.; Kawa, H.; Harling, G. A scoping review of prevalence, incidence and risk factors for HIV infection amongst young people in Brazil. BMC Infect. Dis. 2017, 17, 675. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, H.; Zhang, L.; Zhou, Y.; Wang, K.; Zhang, X.; Wu, J.; Wang, G. The use of geosocial networking smartphone applications and the risk of sexually transmitted infections among men who have sex with men: A systematic review and meta-analysis. BMC Public Health 2018, 18, 1178. [Google Scholar] [CrossRef] [PubMed]
- Muleia, R.; Boothe, M.; Loquiha, O.; Aerts, M.; Faes, C. Spatial Distribution of HIV Prevalence among Young People in Mozambique. Int. J. Environ. Res. Public Health 2020, 17, 885. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO–World Health Organization; Commission on Social Determinants of Health. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Final Report of the Commission on Social Determinants of Health; WHO: Geneva, Switzerland, 2008.
- Qin, Q.; Guo, W.; Tang, W.; Mahapatra, T.; Wang, L.; Zhang, N.; Ding, Z.; Cai, C.; Cui, Y.; Sun, J. Spatial Analysis of the Human Immunodeficiency Virus Epidemic among Men Who Have Sex with Men in China, 2006–2015. Clin Infect Dis. 2017, 64, 956–963. [Google Scholar] [CrossRef] [Green Version]
- Boyda, D.C.; Holzman, S.B.; Berman, A.; Grabowski, M.K.; Chang, L.W. Geographic Information Systems, spatial analysis, and HIV in Africa: A scoping review. PLoS ONE 2019, 14, e0216388. [Google Scholar] [CrossRef]
- Huang, D.; Wang, J.; Yang, T. Mapping the Spatial–Temporal Distribution and Migration Patterns of Men Who Have Sex with Men in Mainland China: A Web-Based Study. Int. J. Environ. Res. Public Health 2020, 17, 1469. [Google Scholar] [CrossRef] [Green Version]
- Taquette, S.R.; Matos, H.J.; Rodrigues, A.D.O.; Bortolotti, L.R.; Amorim, E. A Epidemia de AIDS em Adolescentes de 13 a 19 Anos, No Município Do Rio de Janeiro: Descrição Espaço-Temporal. Rev. Soc. Bras. Med. Trop. 2011, 44, 467–470. Available online: https://www.scielo.br/j/rsbmt/a/5VNKCDp3qdJMRB8tpBPbKjr/?format=pdf&lang=pt (accessed on 10 July 2021). [CrossRef] [Green Version]
- Chimoyi, L.A.; Musenge, E. Spatial analysis of factors associated with HIV infection among young people in Uganda, 2011. BMC Public Health 2014, 14, 555. [Google Scholar] [CrossRef] [Green Version]
- Zhang, X.; Tang, W.; Li, Y.; Mahapatra, T.; Feng, Y.; Li, M.; Chen, F.; Li, P.; Xing, J.; Qian, S.; et al. The HIV/AIDS epidemic among young people in China between 2005 and 2012: Results of a spatial temporal analysis. HIV Med. 2017, 18, 141–150. [Google Scholar] [CrossRef]
- Khalifa, A.; Stover, J.; Mahy, M.; Idele, P.; Porth, T.; Lwamba, C. Demographic change and HIV epidemic projections to 2050 for adolescents and young people aged 15–24. Glob. Health Action 2019, 12, 1662685. [Google Scholar] [CrossRef]
- Nakazwe, C.; Michelo, C.; Sandøy, I.F.; Fylkesnes, K. Contrasting HIV prevalence trends among young women and men in Zambia in the past 12 years: Data from demographic and health surveys 2002–2014. BMC Infect. Dis. 2019, 19, 432. [Google Scholar] [CrossRef] [Green Version]
- Brazil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância. Boletim Epidemiológico HIV/Aids 2020. Brasília/DF. 2020. Available online: http://www.aids.gov.br/pt-br/taxonomy/term/595 (accessed on 10 March 2022).
- Greco, D.B. Trinta anos de enfrentamento à epidemia da Aids no Brasil, 1985–2015. Ciênc. Saúde Colet. 2016, 21, 1553–1564. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- IBGE (Instituto Brasileiro de Geografia e Estatística). Cidades e Estados; IBGE: Rio de Janeiro, Brazil, 2022. Available online: https://www.ibge.gov.br/ (accessed on 10 March 2022).
- Pará. Fapespa. Anuário Estatístico 2021. Fapespa. 2021. Available online: https://www.fapespa.pa.gov.br/sistemas/anuario2021/ (accessed on 10 March 2022).
- Pará. Plano Estadual de Saúde 2016–2019. CONASS. Belém. 2016. Available online: https://www.conass.org.br/pdf/planos-estaduais-de-saude/PA_Plano-estadual-saude-2016-2019.pdf (accessed on 13 April 2021).
- Brazil. Ministério da Saúde. SICLOM. Sistema de Controle Logístico de Medicamentos. SICLOM. 2022. Available online: http://azt.aids.gov.br/ (accessed on 10 March 2022).
- Brazil. Ministério da Saúde. Painel de Indicadores Epidemiológicos. Aids.gov. 2022. Available online: http://aids.gov.br/indicadores (accessed on 22 March 2022).
- Hyndman, R.J.; Athanasopoulos, G. Forecasting: Principles and Practice; OTexts: Melbourne, Australia, 2018; Available online: https://otexts.com/fpp2/ (accessed on 10 March 2022).
- Box, G.E.; Jenkins, G.M.; Reinsel, G.C.; Ljung, G.M. Time Series Analysis: Forecasting and Control, 5th ed.; John Wiley & Sons: Hoboken, NJ, USA, 2015. [Google Scholar]
- Cleveland, R.B.; Cleveland, W.S.; McRae, J.E.; Terpenning, I. STL: A seasonal-trend decomposition. J. Off. Stat. 1990, 6, 3–73. [Google Scholar]
- Jushan, B.A.I. Estimating multiple breaks one at a time. Econom. Theory 1997, 13, 315–352. [Google Scholar] [CrossRef] [Green Version]
- Câmara, G.; Carvalho, M.S.; Cruz, O.G.; Correa, V. Análise Espacial de Áreas. In Análise Espacial de Dados Geográficos; EMBRAPA: Brasilia, Brazil, 2004; Available online: http://www.dpi.inpe.br/gilberto/tutoriais/analise/cap2.pdf (accessed on 12 June 2021).
- Anselin, L. Local indicators of spatial association—LISA. Geogr. Anal. 1995, 27, 93–115. [Google Scholar] [CrossRef]
- Mitchell, A. The ESRI Guide to GIS Analysis, 2nd ed.; ESRI Press: Redlands, CA, USA, 2005. [Google Scholar]
- Kulldorff, M. SaTScanTM Manual do Usuário para Versão 9.4: Versão do Original Traduzido para o Português; Pelini, ACG Tradutor: São Paulo, Brazil, 2016; Available online: http://www.satscan.org/ (accessed on 1 March 2021).
- Antunes, J.L.F.; Cardoso, M.R.A. Uso da análise de séries temporais em estudos epidemiológicos. Epidemiol. Serv. Saúde 2015, 24, 565–576. [Google Scholar] [CrossRef]
- Brunsdon, C.; Fotheringham, S.; Charlton, M. Geographically Weighted Regression. J. R. Stat. Soc. Ser. D 1998, 47, 431–443. [Google Scholar] [CrossRef]
- Assis, I.S.; Arcoverde, M.A.M.; Ramos, A.C.V.; Alves, L.S.; Berra, T.Z.; Arroyo, L.H.; Arcêncio, R.A. Social determinants, their relationship with leprosy risk and temporal trends in a tri-border region in Latin America. PLoS Negl. Trop. Dis. 2018, 12, e0006407. [Google Scholar] [CrossRef] [Green Version]
- Dias, B.R.L. Os Determinantes Sociais, a infecção pelo HIV e a Aids em uma Capital na Amazônia Brasileira: Análise Espacial e Temporal. Master’s Thesis, Faculdade de Enfermagem da Universidade Federal do Pará, Belém, Brazil, 2021. [Google Scholar]
- Brazil. Ministério da Educação. Programa Saúde na Escola. 2022. Available online: http://portal.mec.gov.br/programa-saude-da-escola/194-secretarias-112877938/secad-educacao-continuada-223369541/14578-programa-saude-nas-escolas (accessed on 22 August 2021).
- Fontes, M.B.; Crivelaro, R.C.; Scartezini, A.M.; Lima, D.D.; Garcia, A.D.A.; Fujioka, R.T. Fatores determinantes de conhecimentos, atitudes e práticas em DST/Aids e hepatites virais, entre jovens de 18 a 29 anos, no Brazil. Ciênc. Saúde Colet. 2017, 22, 1343–1352. [Google Scholar] [CrossRef] [Green Version]
- Mittler, J.E.; Murphy, J.T.; Stansfield, S.E.; Peebles, K.; Gottlieb, G.S.; Abernethy, N.F.; Herbeck, J.T. Large benefits to youth-focused HIV treatment-as-prevention efforts in generalized heterosexual populations: An agent-based simulation model. PLoS Comput. Biol. 2019, 15, e1007561. [Google Scholar] [CrossRef] [Green Version]
- Pereira, G.F.M.; Sabidó, M.; Caruso, A.; Benzaken, A.S. Decline in reported AIDS cases in Brazil after implementation of the test and treat initiative. BMC Infect. Dis. 2019, 19, 570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shaorong, W.; Junjie, W.; Peng, X.; Wanting, L.; Mengjie, H. Spatial Analysis of HIV/AIDS Cases among Out-of-School Youth Aged 15–24 Years—China, 2010–2020. China CDC Weekly 2021, 3, 1015–1017. [Google Scholar] [CrossRef]
- Leon, C.; Koosed, T.; Philibert, B. HIV/AIDS health services in Manaus, Brazil: Patient perception of quality and its influence on adherence to antiretroviral treatment. BMC Health Serv. Res. 2019, 19, 344. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.; Zhang, B.; Dai, Z.; Zheng, Q.; Duan, Z.; He, Q.; Zhu, C. Impact of immediate initiation of antiretroviral therapy among men who have sex with men infected with HIV in Chengdu, southwest China: Trends analysis, 2008–2018. BMC Public Health 2021, 21, 689. [Google Scholar] [CrossRef]
- Ooms, G.; Kruja, K. The integration of the global HIV/AIDS response into universal health coverage: Desirable, perhaps possible, but far from easy. Global Health 2019, 15, 1–15. [Google Scholar] [CrossRef]
- Mitzel, L.D.; Vanable, P.A.; Carey, M.P. HIV-related stigmatization and medication adherence: Indirect effects of disclosure concerns and depression. Stigma Health 2019, 4, 282–292. [Google Scholar] [CrossRef] [PubMed]
- Logie, C.H.; Okumu, M.; Kibuuka Musoke, D.; Hakiza, R.; Mwima, S.; Kyambadde, P.; Abela, H.; Gittings, L.; Musinguzi, J.; Mbuagbaw, L.; et al. Intersecting stigma and HIV testing practices among urban refugee adolescents and youth in Kampala, Uganda: Qualitative findings. J. Int. AIDS Soc. 2021, 24, e25674. [Google Scholar] [CrossRef] [PubMed]
- Carneiro, V.B.; Maia, C.R.M.; Ramos, E.M.L.S.; Castelo-Branco, S. Tecobé no Marajó: Tendência de indicadores de monitoramento da atenção primária antes e durante o Programa Mais Médicos para o Brasil. Ciênc. Saúde Colet. 2018, 23, 2413–2422. [Google Scholar] [CrossRef] [Green Version]
- IER. Instituto Edson Royer. Novo Progresso. 2022. Available online: https://prosas.com.br/empreendedores/52946-instituto-edson-royer?locale=en (accessed on 17 March 2022).
- De Souza, D.P.; da Silva, W.R.S.; Cervinski, G.C.; dos Santos, B.D.; de Assis Comarú, F.; Trigoso, F.B.M. Desenvolvimento urbano e saúde pública: Impactos da construção da UHE de Belo Monte. Desenvolv. Meio Ambiente 2018, 46, 154–173. [Google Scholar] [CrossRef]
- Boyce, M.R.; Katz, R.; Standley, C.J. Risk factors for infectious diseases in urban environments of sub-Saharan Africa: A systematic review and critical appraisal of evidence. Trop. Med. Infect. Dis. 2019, 4, 123. [Google Scholar] [CrossRef]
- Nutor, J.J.; Duah, H.O.; Agbadi, P.; Duodu, P.A.; Gondwe, K.W. Spatial analysis of factors associated with HIV infection in Malawi: Indicators for effective prevention. BMC Public Health 2020, 20, 1167. [Google Scholar] [CrossRef] [PubMed]
- Kikvidze, T.; Butsashvili, M.; Kamkamidze, G.; Kajaia, M.; DeHovitz, J.; McNutt, L.A. HIV and sti risk factors among Georgian youth. Georgian Med. News 2022, 322, 7–12. [Google Scholar]
- Chan, C.T.; Olivieri-Mui, B.L.; Mayer, K.H. Associations between State-Level High School HIV Education Policies and Adolescent HIV Risk Behaviors. J. Sch. Health 2021, 92, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Havlir, D.; Lockman, S.; Ayles, H.; Larmarange, J.; Chamie, G.; Gaolathe, T.; UT3 Consortium. What do the Universal Test and Treat trials tell us about the path to HIV epidemic control? J. Int. AIDS Soc. 2020, 23, e25455. [Google Scholar] [CrossRef] [Green Version]
- Richards, P.; VanWey, L. Where Deforestation Leads to Urbanization: How Resource Extraction is Leading to Urban Growth in the Brazilian Amazon. Ann. Assoc. Am. Geogr. 2015, 105, 806–823. [Google Scholar] [CrossRef] [Green Version]
- Waterfield, K.C.; Shah, G.H.; Etheredge, G.D. Consequences of COVID-19 crisis for persons with HIV: The impact of social determinants of health. BMC Public Health 2021, 21, 299. [Google Scholar] [CrossRef]
- Brazil. Ministério da Saúde. Departamento de Doenças Crônicas e Infecções Sexualmente Transmissíveis. Painel de monitoramento de dados de HIV durante a pandemia da COVID-19. 2022. Available online: http://www.aids.gov.br/pt-br/painelcovidHIV (accessed on 10 March 2022).



| Variables | 15–19 Years | 20–24 Years | 25–29 Years | 15–29 Years | ||||
|---|---|---|---|---|---|---|---|---|
| (n = 1055) | % | (n = 3182) | % | (n = 3906) | % | (n = 8143) | % | |
| Gender | ||||||||
| Male | 595 | 56.40 | 2185 | 68.67 | 2632 | 67.38 | 5412 | 66.46 |
| Female | 459 | 43.51 | 996 | 31.30 | 1272 | 32.57 | 2727 | 33.49 |
| unanswered | 1 | 0.09 | 1 | 0.03 | 2 | 0.05 | 4 | 0.05 |
| Race/skin color | ||||||||
| White | 103 | 9.76 | 305 | 9.59 | 356 | 9.11 | 764 | 9.38 |
| Black | 42 | 3.98 | 159 | 5.00 | 232 | 5.94 | 433 | 5.32 |
| Yellow | 15 | 1.42 | 20 | 0.63 | 15 | 0.38 | 50 | 0.61 |
| Blown | 825 | 78.20 | 2440 | 76.68 | 3001 | 76.83 | 6266 | 76.95 |
| Native Indian | 3 | 0.28 | 17 | 0.53 | 17 | 0.44 | 37 | 0.45 |
| Unanswered | 67 | 6.35 | 241 | 7.57 | 285 | 7.30 | 593 | 7.28 |
| Schooling | ||||||||
| Elementary | 427 | 40.47 | 1088 | 34.19 | 1438 | 36.82 | 2953 | 36.26 |
| High School | 341 | 32.32 | 1062 | 33.37 | 1143 | 29.26 | 2546 | 31.27 |
| Graduation | 39 | 3.70 | 325 | 10.22 | 421 | 10.78 | 785 | 9.64 |
| Unanswered | 248 | 23.51 | 707 | 22.22 | 904 | 23.14 | 1859 | 22.83 |
| Living zone | ||||||||
| Urban | 912 | 86.45 | 2742 | 86.17 | 3284 | 84.08 | 6938 | 85.20 |
| Rural | 88 | 8.34 | 272 | 8.55 | 384 | 9.83 | 744 | 9.14 |
| Peri-urban | 16 | 1.52 | 16 | 0.50 | 35 | 0.90 | 67 | 0.82 |
| Unanswered | 39 | 3.70 | 152 | 4.78 | 203 | 5.20 | 394 | 4.84 |
| Exposure category | ||||||||
| Homosexual | 311 | 29.48 | 1028 | 32.31 | 971 | 24.86 | 2310 | 28.37 |
| Bisexual | 83 | 7.87 | 272 | 8.55 | 293 | 7.50 | 648 | 7.96 |
| Heterosexual | 524 | 49.67 | 1612 | 50.66 | 2295 | 58.76 | 4431 | 54.41 |
| Blood | - | 0.00 | 7 | 0.22 | 10 | 0.26 | 17 | 0.21 |
| Perinatal | 31 | 2.94 | 52 | 1.63 | 57 | 1.46 | 140 | 1.72 |
| Unanswered | 106 | 10.05 | 211 | 6.63 | 280 | 7.17 | 597 | 7.33 |
| Test | 15–19 Years | 20–24 Years | 25–29 Years |
|---|---|---|---|
| Test Statistic p-Value | |||
| Ljung–Box | 0.04 | <0.01 | 0.06 |
| Box–Pierce | 0.86 | 0.91 | 0.99 |
| Rank test | 0.78 | 0.81 | 0.78 |
| Turning Point | 0.14 | 0.59 | 0.02 |
| Lilliefors (Kolmogorov–Smirnov) | <0.01 | 0.02 | <0.01 |
| Shapiro–Wilk normality test | <0.01 | <0.01 | <0.01 |
| F test | 0.04 | 0.86 | 0.79 |
| Model | STL + ARIMA(2,1,1) | STL + ARIMA(0.1,1) with drift | STL + ARIMA(2,1,3) |
| MAPE | 45.61464 | 26.4993 | 19.18589 |
| MAE | 0.6170666 | 0.560686 | 0.6170666 |
| RMSE | 0.3519083 | 0.7553249 | 0.7946913 |
| Analysis | Age Group | ||
|---|---|---|---|
| 15–19 Years | 20–24 Years | 25–29 Years | |
| OLS | |||
| AICc | 1521.203 | 1653.173 | 1637.290 |
| R2 | 0.071 | 0.185 | 0.246 |
| Adjusted R2 | 0.064 | 0.173 | 0.230 |
| OLS residues | |||
| Moran’s Index | 0.029337 | 0.053157 | 0.068410 |
| z-score | 1.2472656 | 1.501993 | 1.590206 |
| p-value | 0.21 | 0.13 | 0.11 |
| GRW | |||
| AICc | 395.724 | 307.551 | 355.215 |
| R2 | 0.137 | 0.764 | 0.635 |
| Adjusted R2 | 0.119 | 0.679 | 0.523 |
| GWR residues | |||
| Moran’s Index | 0.023757 | −0.006620 | 0.070442 |
| z-score | 1.041916 | −0.275607 | 1.570456 |
| p-value | 0.29 | 0.78 | 0.11 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedroso, A.O.; Gomes, D.; Sousa, S.M.L.; Ferreira, G.R.O.N.; Ramos, A.M.P.C.; Polaro, S.H.I.; Nogueira, L.M.V.; Botelho, E.P. Temporal and Spatial Analysis Techniques as Potential Tools for Combating the HIV Epidemic among Young Brazilian Amazonian People: An Ecological Study. Trop. Med. Infect. Dis. 2022, 7, 137. https://doi.org/10.3390/tropicalmed7070137
Pedroso AO, Gomes D, Sousa SML, Ferreira GRON, Ramos AMPC, Polaro SHI, Nogueira LMV, Botelho EP. Temporal and Spatial Analysis Techniques as Potential Tools for Combating the HIV Epidemic among Young Brazilian Amazonian People: An Ecological Study. Tropical Medicine and Infectious Disease. 2022; 7(7):137. https://doi.org/10.3390/tropicalmed7070137
Chicago/Turabian StylePedroso, Andrey Oeiras, Dulce Gomes, Sara Melissa Lago Sousa, Glenda Roberta Oliveira Naiff Ferreira, Aline Maria Pereira Cruz Ramos, Sandra Helena Isse Polaro, Laura Maria Vidal Nogueira, and Eliã Pinheiro Botelho. 2022. "Temporal and Spatial Analysis Techniques as Potential Tools for Combating the HIV Epidemic among Young Brazilian Amazonian People: An Ecological Study" Tropical Medicine and Infectious Disease 7, no. 7: 137. https://doi.org/10.3390/tropicalmed7070137
APA StylePedroso, A. O., Gomes, D., Sousa, S. M. L., Ferreira, G. R. O. N., Ramos, A. M. P. C., Polaro, S. H. I., Nogueira, L. M. V., & Botelho, E. P. (2022). Temporal and Spatial Analysis Techniques as Potential Tools for Combating the HIV Epidemic among Young Brazilian Amazonian People: An Ecological Study. Tropical Medicine and Infectious Disease, 7(7), 137. https://doi.org/10.3390/tropicalmed7070137







