Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020
Abstract
:1. Introduction
2. Materials and Methods
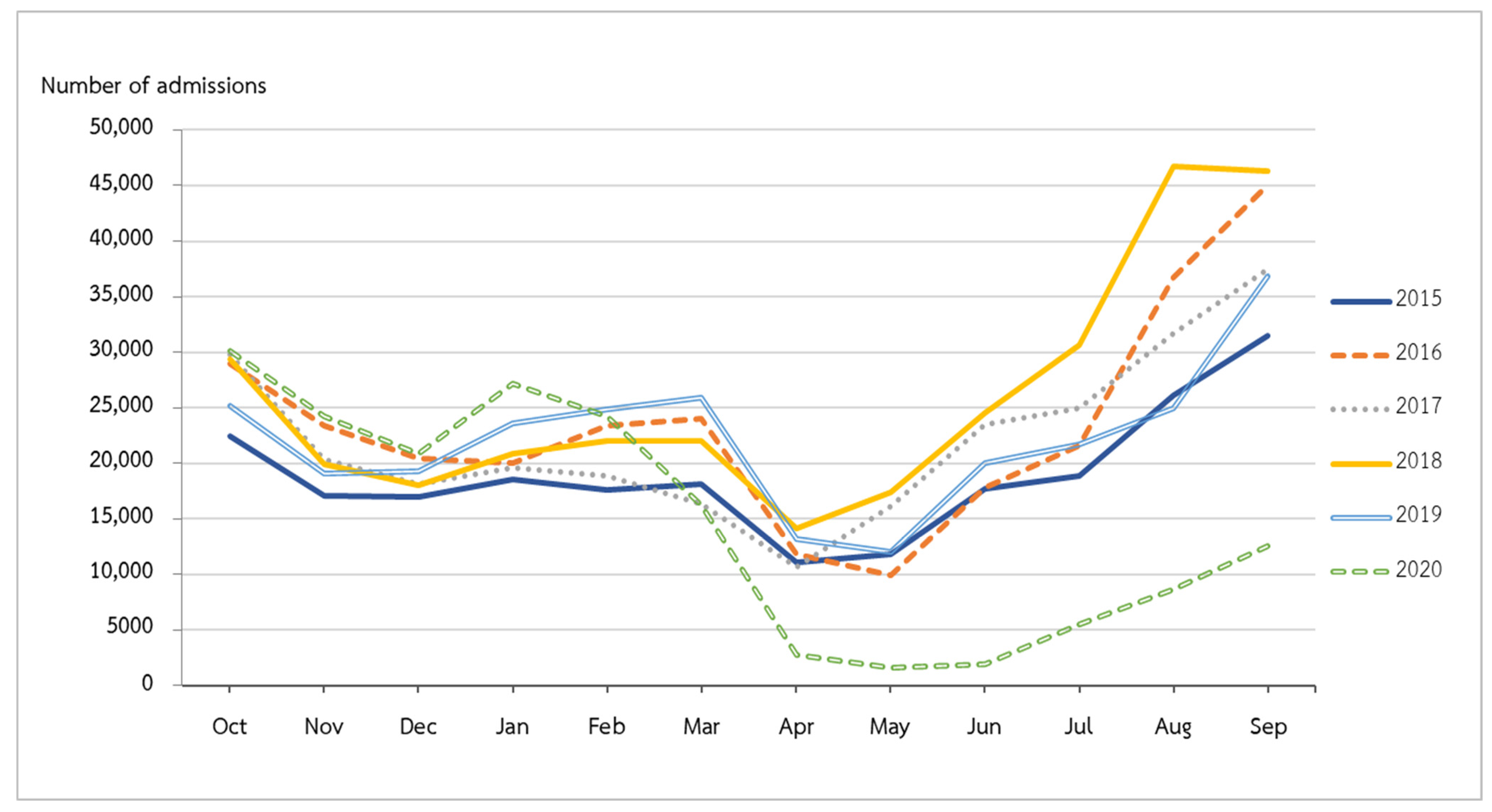
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Teeratakulpisarn, J.; Uppala, R.; Thepsuthammarat, K.; Sutra, S. Burden of Acute Lower Respiratory Infection in Children in Thailand in 2010: Have We Achieved the National Target in under-Five Morbidity and Mortality? J. Med. Assoc. Thail. 2012, 95 (Suppl. S7), S87–S96. [Google Scholar]
- Rudan, I.; O’Brien, K.L.; Nair, H.; Liu, L.; Theodoratou, E.; Qazi, S.; Lukšić, I.; Fischer Walker, C.L.; Black, R.E.; Campbell, H.; et al. Epidemiology and Etiology of Childhood Pneumonia in 2010: Estimates of Incidence, Severe Morbidity, Mortality, Underlying Risk Factors and Causative Pathogens for 192 Countries. J. Glob. Health 2013, 3, 010401. [Google Scholar] [CrossRef]
- Pneumonia. Available online: https://www.who.int/news-room/fact-sheets/detail/pneumonia (accessed on 13 June 2022).
- Zhu, Y.; Li, W.; Yang, B.; Qian, R.; Wu, F.; He, X.; Zhu, Q.; Liu, J.; Ni, Y.; Wang, J.; et al. Epidemiological and Virological Characteristics of Respiratory Tract Infections in Children during COVID-19 Outbreak. BMC Pediatrics 2021, 21, 195. [Google Scholar] [CrossRef] [PubMed]
- Suntronwong, N.; Vichaiwattana, P.; Klinfueng, S.; Korkong, S.; Thongmee, T.; Vongpunsawad, S.; Poovorawan, Y. Climate Factors Influence Seasonal Influenza Activity in Bangkok, Thailand. PLoS ONE 2020, 15, e0239729. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A Novel Coronavirus Outbreak of Global Health Concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef] [Green Version]
- Coronavirus Disease (COVID-19)—World Health Organization. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 13 June 2022).
- World Health Organization. Regional Office for the Western Pacific Calibrating Long-Term Non-Pharmaceutical Interventions for COVID-19: Principles and Facilitation Tools; WHO Regional Office for the Western Pacific: Manila, Philippines, 2020. [Google Scholar]
- Chu, D.K.; Akl, E.A.; Duda, S.; Solo, K.; Yaacoub, S.; Schünemann, H.J. COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors Physical Distancing, Face Masks, and Eye Protection to Prevent Person-to-Person Transmission of SARS-CoV-2 and COVID-19: A Systematic Review and Meta-Analysis. Lancet 2020, 395, 1973–1987. [Google Scholar] [CrossRef]
- Tantrakarnapa, K.; Bhopdhornangkul, B. Challenging the Spread of COVID-19 in Thailand. One Health 2020, 11, 100173. [Google Scholar] [CrossRef]
- Jefferson, T.; Del Mar, C.B.; Dooley, L.; Ferroni, E.; Al-Ansary, L.A.; Bawazeer, G.A.; van Driel, M.L.; Jones, M.A.; Thorning, S.; Beller, E.M.; et al. Physical Interventions to Interrupt or Reduce the Spread of Respiratory Viruses. Cochrane Database Syst. Rev. 2020, 11, CD006207. [Google Scholar] [CrossRef]
- Wang, X.; Li, Y.; O’Brien, K.L.; Madhi, S.A.; Widdowson, M.-A.; Byass, P.; Omer, S.B.; Abbas, Q.; Ali, A.; Amu, A.; et al. Global Burden of Respiratory Infections Associated with Seasonal Influenza in Children under 5 Years in 2018: A Systematic Review and Modelling Study. Lancet Glob. Health 2020, 8, e497–e510. [Google Scholar] [CrossRef] [Green Version]
- Nitsuwat, S.; Paoin, W. Development of ICD-10-TM Ontology for a Semi-Automated Morbidity Coding System in Thailand. Methods Inf. Med. 2012, 51, 519–528. [Google Scholar] [CrossRef] [Green Version]
- Sumriddetchkajorn, K.; Shimazaki, K.; Ono, T.; Kusaba, T.; Sato, K.; Kobayashi, N. Universal Health Coverage and Primary Care, Thailand. Bull. World Health Organ. 2019, 97, 415–422. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Lu, J.; Liu, Y.; Zhang, Z.; Luo, L. Positive Effects of COVID-19 Control Measures on Influenza Prevention. Int. J. Infect. Dis. 2020, 95, 345–346. [Google Scholar] [CrossRef]
- Leuzinger, K.; Roloff, T.; Gosert, R.; Sogaard, K.; Naegele, K.; Rentsch, K.; Bingisser, R.; Nickel, C.H.; Pargger, H.; Bassetti, S.; et al. Epidemiology of Severe Acute Respiratory Syndrome Coronavirus 2 Emergence Amidst Community-Acquired Respiratory Viruses. J. Infect. Dis. 2020, 222, 1270–1279. [Google Scholar] [CrossRef]
- Redlberger-Fritz, M.; Kundi, M.; Aberle, S.W.; Puchhammer-Stöckl, E. Significant Impact of Nationwide SARS-CoV-2 Lockdown Measures on the Circulation of Other Respiratory Virus Infections in Austria. J. Clin. Virol. 2021, 137, 104795. [Google Scholar] [CrossRef]
- Huang, Q.S.; Wood, T.; Jelley, L.; Jennings, T.; Jefferies, S.; Daniells, K.; Nesdale, A.; Dowell, T.; Turner, N.; Campbell-Stokes, P.; et al. Impact of the COVID-19 Non-pharmaceutical Interventions on Influenza and Other Respiratory Viral Infections in New Zealand. Nat. Commun. 2021, 12, 1001. [Google Scholar] [CrossRef] [PubMed]
- Sitthikarnkha, P.; Uppala, R.; Niamsanit, S.; Sutra, S.; Thepsuthammarat, K.; Techasatian, L.; Teeratakulpisarn, J. Epidemiology of Acute Lower Respiratory Tract Infection Hospitalizations in Thai Children: A 5-Year National Data Analysis. Influenza Other Respir. Viruses 2021, 16, 142–150. [Google Scholar] [CrossRef]
- Haddadin, Z.; Schuster, J.E.; Spieker, A.J.; Rahman, H.; Blozinski, A.; Stewart, L.; Campbell, A.P.; Lively, J.Y.; Michaels, M.G.; Williams, J.V.; et al. Acute Respiratory Illnesses in Children in the SARS-CoV-2 Pandemic: Prospective Multicenter Study. Pediatrics 2021, 148, e2021051462. [Google Scholar] [CrossRef] [PubMed]
- Kuitunen, I.; Artama, M.; Mäkelä, L.; Backman, K.; Heiskanen-Kosma, T.; Renko, M. Effect of Social Distancing Due to the COVID-19 Pandemic on the Incidence of Viral Respiratory Tract Infections in Children in Finland During Early 2020. Pediatric Infect. Dis. J. 2020, 39, e423–e427. [Google Scholar] [CrossRef] [PubMed]
- Santoli, J.M.; Lindley, M.C.; DeSilva, M.B.; Kharbanda, E.O.; Daley, M.F.; Galloway, L.; Gee, J.; Glover, M.; Herring, B.; Kang, Y.; et al. Effects of the COVID-19 Pandemic on Routine Pediatric Vaccine Ordering and Administration—United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 591–593. [Google Scholar] [CrossRef] [PubMed]
- Hartnett, K.P.; Kite-Powell, A.; DeVies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V. National Syndromic Surveillance Program Community of Practice Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, 1st January, 2019–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef]
- Chen, J.; Vullikanti, A.; Santos, J.; Venkatramanan, S.; Hoops, S.; Mortveit, H.; Lewis, B.; You, W.; Eubank, S.; Marathe, M.; et al. Epidemiological and Economic Impact of COVID-19 in the US. medRxiv 2020. medRxiv:2020.11.28.20239517. [Google Scholar] [CrossRef] [PubMed]
- Oh, D.-Y.; Buda, S.; Biere, B.; Reiche, J.; Schlosser, F.; Duwe, S.; Wedde, M.; von Kleist, M.; Mielke, M.; Wolff, T.; et al. Trends in Respiratory Virus Circulation Following COVID-19-Targeted Nonpharmaceutical Interventions in Germany, January–September 2020: Analysis of National Surveillance Data. Lancet Reg. Health Eur. 2021, 6, 100112. [Google Scholar] [CrossRef] [PubMed]


| Fiscal Year | 2015 | 2016 | 2017 | 2018 | 2019 | 2020 | Total |
|---|---|---|---|---|---|---|---|
| Total | 235,316 | 294,436 | 281,510 | 329,657 | 282,590 | 186,651 | 1,610,160 |
| Gender, N (%) | |||||||
| Male | 140,165 (59.56) | 171,817 (58.35) | 164,619 (58.48) | 193,533 (58.71) | 164,987 (58.38) | 109,400 (58.61) | 944,521 |
| Age group, N (%) | |||||||
| <1 year | 57,903 (24.61) | 70,313 (23.88) | 64,753 (23.00) | 82,424 (25.00) | 61,280 (21.69) | 42,247 (22.63) | 378,920 |
| 1–<5 years | 141,875 (60.29) | 174,129 (59.14) | 162,349 (57.67) | 194,000 (58.85) | 157,037 (55.57) | 103,718 (55.57) | 933,108 |
| 5–<18 years | 35,538 (15.10) | 49,994 (16.98) | 54,408 (19.33) | 53,233 (16.15) | 64,273 (22.74) | 40,686 (21.80) | 298,132 |
| Principal diagnosis, N (%) | |||||||
| Pneumonia (J09–J18) | 130,943 (55.65) | 179,434 (60.94) | 176,352 (62.65) | 207,382 (62.91) | 182,446 (64.56) | 120,281 (64.44) | 996,838 |
| Bronchiolitis (J21) | 31,121 (13.23) | 31,535 (10.71) | 27,493 (9.77) | 34,037 (10.32) | 25,067 (8.87) | 16,037 (8.59) | 165,290 |
| Bronchitis (J20) | 73,252 (31.13) | 83,467 (28.35) | 77,665 (27.59) | 88,238 (26.77) | 75,077 (26.57) | 50,333 (26.97) | 448,032 |
| Region, N (%) | |||||||
| Bangkok | 10,304 (4.38) | 13,224 (4.49) | 11,839 (4.21) | 12,464 (3.78) | 10,736 (3.80) | 6371 (3.41) | 64,938 |
| Central | 45,402 (19.29) | 58,494 (19.87) | 55,588 (19.75) | 64,445 (19.55) | 55,122 (19.51) | 34,669 (18.57) | 313,720 |
| East | 13,827 (5.88) | 16,947 (5.76) | 16,609 (5.90) | 18,719 (5.68) | 15,492 (5.48) | 8922 (4.78) | 90,516 |
| Northeast | 83,335 (35.41) | 111,398 (37.83) | 105,592 (37.51) | 125,414 (38.04) | 98,332 (34.80) | 68,684 (36.80) | 592,755 |
| North | 20,424 (8.68) | 23,906 (8.12) | 22,609 (8.03) | 28,562 (8.66) | 26,815 (9.49) | 18,428 (9.87) | 140,744 |
| West | 12,360 (5.25) | 15,735 (5.34) | 14,435 (5.13) | 18,356 (5.57) | 15,730 (5.57) | 10,162 (5.44) | 86,778 |
| South | 49,664 (21.11) | 54,732 (18.59) | 54,838 (19.48) | 61,697 (18.72) | 60,363 (21.36) | 39,415 (21.12) | 320,709 |
| Level of hospital, N (%) | |||||||
| Primary | 16,299 (6.93) | 21,319 (7.24) | 20,683 (7.35) | 25,926 (7.86) | 21,032 (7.44) | 14,049 (7.53) | 119,308 |
| Secondary | 173,335 (73.66) | 215,586 (73.22) | 208,757 (74.16) | 246,822 (74.87) | 212,567 (75.22) | 142,217 (76.19) | 1,199,284 |
| Tertiary | 37,898 (16.11) | 47,275 (16.06) | 43,263 (15.37) | 48,288 (14.65) | 40,856 (14.46) | 25,748 (13.79) | 243,328 |
| Private | 7784 (3.31) | 10,256 (3.48) | 8807 (3.13) | 8621 (2.62) | 8135 (2.88) | 4637 (2.48) | 48,240 |
| 2015–2019 | 2020 | p Value | |
|---|---|---|---|
| Total | 1,423,509 (88.41) | 186,651 (11.59) | |
| Principal diagnosis, N (%) | <0.001 | ||
| Pneumonia (J09–J18) | 876,557 (61.58) | 120,281 (64.44) | |
| Bronchiolitis (J21) | 149,253 (10.48) | 16,037 (8.59) | |
| Bronchitis (J20) | 397,699 (27.94) | 50,333 (26.97) | |
| Sex, N (%) | 0.786 | ||
| Male | 835,121 (58.67) | 109,400 (58.61) | |
| Female | 588,388 (41.33) | 77,251 (41.39) | |
| Age group, N (%) | <0.001 | ||
| <1 year | 336,673 (23.65) | 42,247 (22.63) | |
| 1–<5 years | 829,390 (58.26) | 103,718 (55.57) | |
| 5–<18 years | 257,446 (18.09) | 40,686 (21.80) | |
| Region, N (%) | <0.001 | ||
| Bangkok | 58,567 (4.11) | 6371 (3.41) | |
| Central | 279,051 (19.60) | 34,669 (18.57) | |
| East | 81,594 (5.73) | 8922 (4.78) | |
| Northeast | 524,071 (36.82) | 68,684 (36.80) | |
| North | 122,316 (8.59) | 18,428 (9.87) | |
| West | 76,616 (5.38) | 10,162 (5.44) | |
| South | 281,294 (19.76) | 39,415 (21.12) | |
| Hospital level, N (%) | <0.001 | ||
| Primary | 105,259 (7.39) | 14,049 (7.53) | |
| Secondary | 1,057,067 (74.26) | 142,217 (76.19) | |
| Tertiary | 217,580 (15.28) | 25,748 (13.79) | |
| Private | 43,603 (3.06) | 4637 (2.48) |
| Principal Diagnosis | 2015–2019 | 2020 | IRR (95%CI) |
|---|---|---|---|
| Pneumonia (J09–J18) | 12.77 | 9.16 | 0.72 (0.71, 0.72) |
| Bronchitis (J20) | 5.79 | 3.84 | 0.66 (0.65, 0.67) |
| Bronchiolitis (J21) | 2.17 | 1.22 | 0.56 (0.55, 0.57) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uppala, R.; Sitthikarnkha, P.; Niamsanit, S.; Sutra, S.; Thepsuthammarat, K.; Techasatian, L.; Anantasit, N.; Teeratakulpisarn, J. Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020. Trop. Med. Infect. Dis. 2022, 7, 151. https://doi.org/10.3390/tropicalmed7080151
Uppala R, Sitthikarnkha P, Niamsanit S, Sutra S, Thepsuthammarat K, Techasatian L, Anantasit N, Teeratakulpisarn J. Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020. Tropical Medicine and Infectious Disease. 2022; 7(8):151. https://doi.org/10.3390/tropicalmed7080151
Chicago/Turabian StyleUppala, Rattapon, Phanthila Sitthikarnkha, Sirapoom Niamsanit, Sumitr Sutra, Kaewjai Thepsuthammarat, Leelawadee Techasatian, Nattachai Anantasit, and Jamaree Teeratakulpisarn. 2022. "Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020" Tropical Medicine and Infectious Disease 7, no. 8: 151. https://doi.org/10.3390/tropicalmed7080151
APA StyleUppala, R., Sitthikarnkha, P., Niamsanit, S., Sutra, S., Thepsuthammarat, K., Techasatian, L., Anantasit, N., & Teeratakulpisarn, J. (2022). Effect of the COVID-19 Pandemic on Lower Respiratory Tract Infection Determinants in Thai Hospitalized Children: National Data Analysis 2015–2020. Tropical Medicine and Infectious Disease, 7(8), 151. https://doi.org/10.3390/tropicalmed7080151






