Seroprevalence and Associated Risk Factors of Trichinellosis and T. Solium Cysticercosis in Indigenous Pigs in Hoa Binh Province, Vietnam
Abstract
1. Introduction
2. Materials and Methods
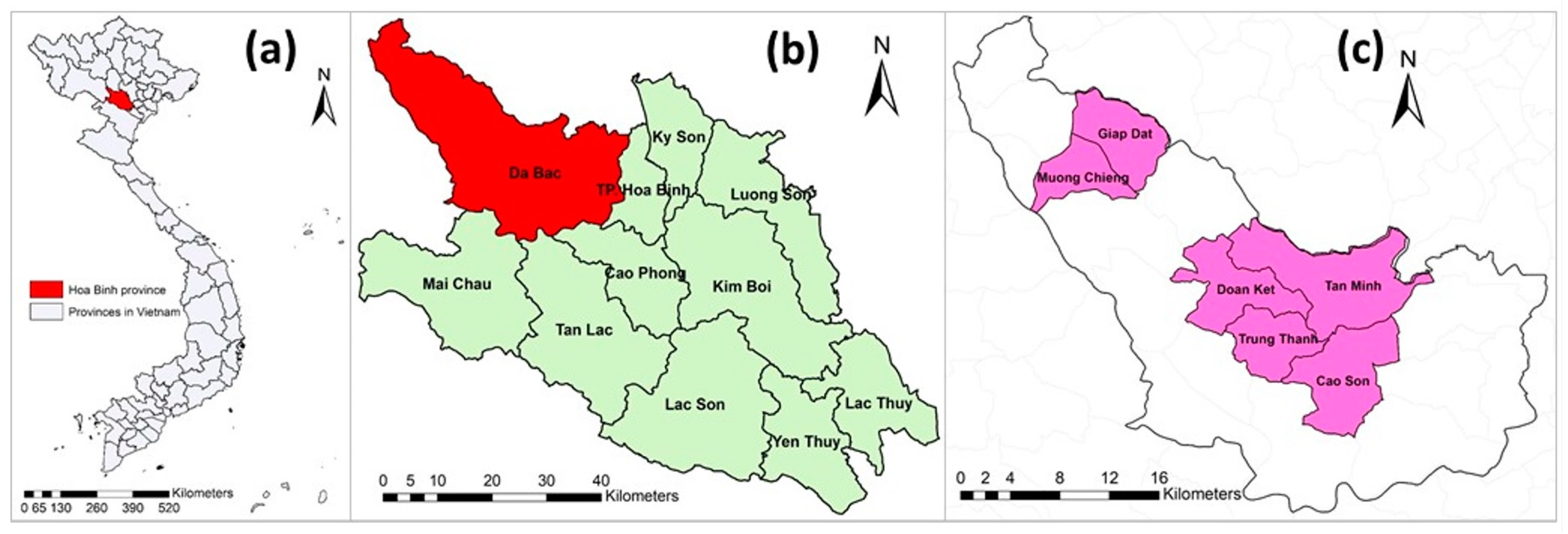
2.1. Study Sites and Design
2.2. Sample Size
2.3. Data Collection
2.3.1. Pig Samplings and Observational Checklist
2.3.2. Questionnaire
2.4. Data Management and Analysis
2.4.1. Laboratory Testing
2.4.2. On-Farm Questionnaire
2.4.3. Data Analysis
3. Results
3.1. Seroprevalence of Pig Trichinellosis and T. solium Cysticercosis in Pigs
3.2. Risk Factors Related to Seroprevalence of Trichinellosis and T. solium Cysticercosis in Pigs
3.2.1. Pig Raising Practice and Sanitation Conditions
3.2.2. Univariable Analysis
3.2.3. Multivariable Analysis
3.3. FBPDs Knowledge and Attitude and Behaviour of Eating Raw or Undercooked Pork
3.3.1. Demographic Information of Respondents
3.3.2. Knowledge
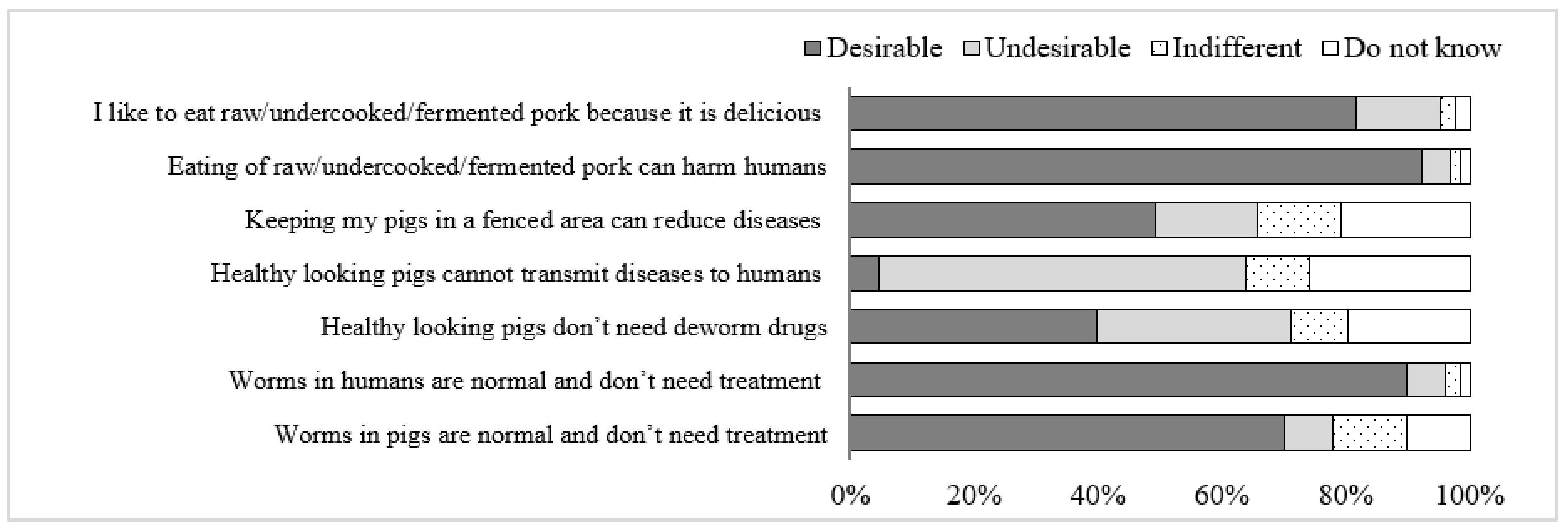
3.3.3. Attitude
3.3.4. Behavior of Eating Undercooked or Fermented Pork
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Organisation for Animal Health (OIE). Infection with Taenia solium (Porcine cysticercosis). In Terrestrial Animal Health Code; OIE: Paris, France, 2019; Chapter 15.4.; Volume 2. [Google Scholar]
- World Health Organization (WHO); Food and Agriculture Organization (FAO). Multicriteria-Based Ranking for Risk Management of Food-Borne Parasites: Report of a Joint FAO/WHO Expert Meeting, 3–7 September 2012; Microbiological Risk Assessment Series No. 23; FAO: Rome, Italy, 2014. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Parasites—Trichinellosis. Available online: https://www.cdc.gov/parasites/trichinellosis/disease.html (accessed on 10 September 2021).
- Olson, M.E.; Guselle, N. Are pig parasites a human health risk? Adv. Pork Prod. 2000, 11, 153–162. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Parasites-Cysticercosis. Available online: https://www.cdc.gov/parasites/cysticercosis/gen_info/faqs.html (accessed on 10 September 2021).
- Gottstein, B.; Pozio, E.; Nockler, K. Epidemiology, diagnosis, treatment, and control of trichinellosis. Clin. Microbiol. Rev. 2009, 22, 127–145. [Google Scholar] [CrossRef] [PubMed]
- Sikasunge, C.S.; Phiri, I.K.; Phiri, A.M.; Dorny, P.; Siziya, S.; Willingham, A.L. Risk factors associated with porcine cysticercosis in selected districts of eastern and southern provinces of Zambia. Vet. Parasitol. 2007, 143, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Willingham, A.L.; Wu, H.W.; Conlan, J.; Satrija, F. Combating Taenia solium cysticercosis in Southeast Asia. In Advances in Parasitology; Elsevier: Amsterdam, The Netherlands, 2010; Volume 72, pp. 235–266. ISBN 978-0-12-381513-2. [Google Scholar]
- Dupouy-Camet, J. Trichinellosis: A Worldwide Zoonosis. Vet. Parasitol. 2000, 93, 191–200. [Google Scholar] [CrossRef]
- Murrell, K.D.; Pozio, E. Trichinellosis: The Zoonosis That Won’t Go Quietly. Int. J. Parasitol. 2000, 30, 1339–1349. [Google Scholar] [CrossRef]
- Pozio, E. World Distribution of Trichinella spp. Infections in Animals and Humans. Vet. Parasitol. 2007, 149, 3–21. [Google Scholar] [CrossRef]
- Kaewpitoon, N.; Kaewpitoon, S.J.; Pengsaa, P. Food-Borne Parasitic Zoonosis: Distribution of Trichinosis in Thailand. WJG 2008, 14, 3471. [Google Scholar] [CrossRef]
- Van De, N.; Thi Nga, V.; Ngoc Minh, P.; Vu Trung, N.; Pozio, E.; Trung Dung, D.; Dorny, P. Trichinellosis in Vietnam. Am. J. Trop. Med. Hyg. 2015, 92, 1265–1270. [Google Scholar] [CrossRef]
- Vu Thi, N.; De, N.V.; Praet, N.; Claes, L.; Gabriël, S.; Dorny, P. Seroprevalence of trichinellosis in domestic animals in northwestern Vietnam. Vet. Parasitol. 2013, 193, 200–205. [Google Scholar] [CrossRef]
- Vu Thi, N.; Trung, D.D.; Litzroth, A.; Praet, N.; Nguyen Thu, H.; Nguyen Thu, H.; Nguyen Manh, H.; Dorny, P. The Hidden Burden of Trichinellosis in Vietnam: A Postoutbreak Epidemiological Study. BioMed Res. Int. 2013, 2013, 149890. [Google Scholar] [CrossRef]
- Del Brutto, O.H.; Rajshekhar, V.; White, A.C.; Tsang, V.C.; Nash, T.E.; Takayanagui, O.M.; Schantz, P.M.; Evans, C.A.; Flisser, A.; Correa, D.; et al. Proposed Diagnostic Criteria for Neurocysticercosis. Neurology 2001, 57, 177–183. [Google Scholar] [CrossRef]
- Schantz, P.M.; Cruz, M.; Sarti, E.; Pawlowski, Z. Potential eradicability of taeniasis and cysticercosis. Bull. Pan Am. Health Organ. 1993, 27, 397–403. [Google Scholar]
- Somers, R.; Dorny, P.; Geysen, D.; Nguyen, L.A.; Thach, D.C.; Vercruysse, J.; Nguyen, V.K. Human tapeworms in north Vietnam. Trans. R. Soc. Trop. Med. Hyg. 2007, 101, 275–277. [Google Scholar] [CrossRef]
- Somers, R.; Dorny, P.; Nguyen, V.K.; Dang, T.C.T.; Goddeeris, B.; Craig, P.S.; Vercruysse, J. Taenia solium taeniasis and cysticercosis in three communities in north Vietnam. Trop. Med. Int. Health 2006, 11, 65–72. [Google Scholar] [CrossRef]
- Van De, N.; Le, T.H.; Lien, P.T.H.; Eom, K.S. Current status of taeniasis and cysticercosis in Vietnam. Korean J. Parasitol. 2014, 52, 125–129. [Google Scholar] [CrossRef]
- Doanh, N.Q.; Kim, N.T.; De, N.V.; Lung, N.N. Result of survey on taeniasis and cysticercosis humans and pigs in Bac Ninh and Bac Kan provinces. Vet. Sci. Tech. 2002, 9, 46–49. [Google Scholar]
- Doanh, N.Q.; Holland, W.; Vecruyce, J.; De, N.V. Results of survey on cysticercosis pig in some northern provinces in Vietnam. J. Malar. Parasite Dis. Control 2002, 6, 76–82. [Google Scholar]
- De, N.V.; Chau, L.V.; Son, D.T.; Chuyen, L.T.; Hop, N.T.; Vien, H.V.; Hien, N.T.; Dung, D.T.; Thuan, L.K. Taenia solium survey in Hanoi. J. Malar. Parasite Dis. Control 2004, 6, 93–99. [Google Scholar]
- Ng-Nguyen, D.; Noh, J.; Breen, K.; Stevenson, M.A.; Handali, S.; Traub, R.J. The epidemiology of porcine Taenia solium cysticercosis in communities of the central highlands in Vietnam. Parasites Vectors 2018, 11, 360. [Google Scholar] [CrossRef]
- Huan, L.V. Parasitic Helminths in Pigs in Several Southern Provinces and Preventative Measures; National Institute of Veterinary Research: Hanoi, Vietnam, 1994. (In Vietnamese)
- Lan, N.T.K.; Quyen, N.T.; Hoat, P.C. The correlation between the prevalence of the tapeworm Taenia hydatigena in dogs and their larvae Cysticercus tenuicollis in cattle and pigs-The effect of tapeworm treatment in dogs. Vet. Sci. Tech. 2011, 18, 60–65. [Google Scholar]
- Nguyen, T.; Dermauw, V.; Noh, J.; Chien, N.; Dao, T.; Van Hul, A.; Dorny, P. Occurrence of Taenia species in pigs in slaughterhouses in Phu Tho province, northern Vietnam. J. Helminthol. 2020, 94, e201. [Google Scholar] [CrossRef] [PubMed]
- Lemke, U.; Mergenthaler, M.; Roßler, R.; Huyen, L.; Herold, P.; Kaufmann, B.; Zarate, A.V. Pig production in Vietnam—A review. CAB Rev. Perspect. Agric. Vet. Sci. Nutr. Nat. Resour. 2008, 23, 1–15. [Google Scholar] [CrossRef]
- GSO (General Statistics Office of Vietnam). Vietnam Population and Housing Census 2009: Education in Vietnam—An Analysis of Key Indicators; GSO: Hanoi, Vietnam, 2009.
- Lan, P.; Jones, N.; Thuy, T.; Lyytikainen, M. Education for All in Vietnam: High Enrolment, but Problems of Quality Remain; University of Oxford: Oxford, UK, 2007. [Google Scholar]
- Noh, J.; Rodriguez, S.; Lee, Y.-M.; Handali, S.; Gonzalez, A.E.; Gilman, R.H.; Tsang, V.C.W.; Garcia, H.H.; Wilkins, P.P. Recombinant protein- and synthetic peptide-based immunoblot test for diagnosis of neurocysticercosis. J. Clin. Microbiol. 2014, 52, 1429–1434. [Google Scholar] [CrossRef] [PubMed]
- Tsang, V.C.W.; Brand, J.A.; Boyer, A.E. An enzyme-linked immunoelectrotransfer blot assay and glycoprotein antigens for diagnosing human cysticercosis (Taenia solium). J. Infect. Dis. 1989, 159, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Tsang, V.C.; Pilcher, J.A.; Zhou, W.; Boyer, A.E.; Kamango-Sollo, E.I.; Rhoads, M.L.; Murrell, K.D.; Schantz, P.M.; Gilman, R.H. Efficacy of the immunoblot assay for cysticercosis in pigs and modulated expression of distinct IgM/IgG activities to Taenia solium antigens in experimental infections. Vet. Immunol. Immunopathol. 1991, 29, 69–78. [Google Scholar] [CrossRef]
- Bates, D.; Maechler, M.; Bolker, B.; Walker, S.; Christensen, R.H.B.; Singmann, H.; Dai, B.; Scheipl, F.; Grothendieck, G.; Green, P.; et al. Linear Mixed-Effects Models Using ‘Eigen’ and S4. 2017. Available online: https://cran.r-project.org/web/packages/lme4/lme4.pdf (accessed on 8 August 2021).
- Nguyen Van, C.; Vu Thi, N.; Nguyen, C. Result of survey and solution for trichinellosis in pigs in Bac yen district, Son La province. Vet. Sci. Tech. 2012, 19, 45–50. [Google Scholar]
- Vu Thi, N.; Dorny, P.; La Rosa, G.; To Long, T.; Nguyen Van, C.; Pozio, E. High Prevalence of Anti-Trichinella IgG in Domestic Pigs of the Son La Province, Vietnam. Vet. Parasitol. 2010, 168, 136–140. [Google Scholar] [CrossRef]
- Söderberg, R.; Lindahl, J.F.; Henriksson, E.; Kroesna, K.; Ly, S.; Sear, B.; Unger, F.; Tum, S.; Nguyen-Viet, H.; Ström Hallenberg, G. Low Prevalence of Cysticercosis and Trichinella Infection in Pigs in Rural Cambodia. Trop. Med. Infect. Dis. 2021, 6, 100. [Google Scholar] [CrossRef]
- Holt, H.R.; Inthavong, P.; Khamlome, B.; Blaszak, K.; Keokamphe, C.; Somoulay, V.; Phongmany, A.; Durr, P.; Graham, K.; Allen, J.; et al. Endemicity of Zoonotic Diseases in Pigs and Humans in Lowland and Upland Lao PDR: Identification of Socio-cultural Risk Factors. PLoS Negl. Trop. Dis. 2016, 10, e0003913. [Google Scholar] [CrossRef]
- Adenuga, A.; Mateus, A.; Ty, C.; Borin, K.; Holl, D.; San, S.; Duggan, V.; Clark, M.; Smith, G.J.D.; Coker, R.; et al. Seroprevalence and Awareness of Porcine Cysticercosis across Different Pig Production Systems in South-Central Cambodia. Parasite Epidemiol. Control 2018, 3, 1–12. [Google Scholar] [CrossRef]
- Conlan, J.V.; Vongxay, K.; Khamlome, B.; Dorny, P.; Sripa, B.; Elliot, A.; Blacksell, S.D.; Fenwick, S.; Thompson, R.C.A. A cross-sectional study of Taenia solium in a multiple taeniid-endemic region reveals competition may be protective. Am. J. Trop. Med. Hyg. 2012, 87, 281–291. [Google Scholar] [CrossRef]
- Khaing, T.A.; Bawm, S.; Wai, S.S.; Htut, Y.; Htun, L.L. Epidemiological survey on porcine cysticercosis in Nay Pyi Taw area, Myanmar. J. Vet. Med. 2015, 2015, 340828. [Google Scholar] [CrossRef][Green Version]
- Dorny, P.; Phiri, I.K.; Vercruysse, J.; Gabriel, S.; Willingham, A.L.; Brandt, J.; Victor, B.; Speybroeck, N.; Berkvens, D. A Bayesian Approach for Estimating Values for Prevalence and Diagnostic Test Characteristics of Porcine Cysticercosis. Int. J. Parasitol. 2004, 34, 569–576. [Google Scholar] [CrossRef]
- National Institute of Malariology, Parasitology and Entomology (NIMPE). Taeniasis and Cysticercosis. Rev. Work. Helminthiasis Control Act. Period 2006–2011 Implement. Work. Period 2012–2015; Ministry of Health of Vietnam: Hanoi, Vietnam, 2012.
- Ng-Nguyen, D.; Stevenson, M.A.; Traub, R.J. A systematic review of taeniasis, cysticercosis and trichinellosis in Vietnam. Parasites Vectors 2017, 10, 150. [Google Scholar] [CrossRef]
- Pozio, E.; Darwin Murrell, K. Systematics and epidemiology of Trichinella. In Advances in Parasitology; Elsevier: Amsterdam, The Netherlands, 2006; Volume 63, pp. 367–439. ISBN 978-0-12-031763-9. [Google Scholar]
- Agustina, K.K.; Swacita, I.B.N.; Oka, I.B.M.; Dwinata, I.M.; Traub, R.J.; Cargill, C.; Damriyasa, I.M. Reducing zoonotic and internal parasite burdens in pigs using a pig confinement system. Vet. World 2017, 10, 1347–1352. [Google Scholar] [CrossRef][Green Version]
- Lien, N. Current status of trichinosis (Trichinella spp.) in some northern provinces of Vietnam and the effectiveness of interventions (2015–2017). Ph.D Thesis, National Institute of Malariology, Parasitology and Entomology, Hanoi, Vietnam, 2019. [Google Scholar]
- Conlan, J.V.; Vongxay, K.; Khamlome, B.; Gomez-Morales, M.A.; Pozio, E.; Blacksell, S.D.; Fenwick, S.; Thompson, R.C.A. Patterns and Risks of Trichinella Infection in Humans and Pigs in Northern Laos. PLoS Negl. Trop. Dis. 2014, 8, e3034. [Google Scholar] [CrossRef]
- Dorny, P.; Somers, R.; Dang, T.C.T.; Nguyen, V.K.; Vercruysse, J. Cysticercosis in Cambodia, Laos PDR and Vietnam. Southest Asian J. Trop. Med. Public Health 2004, 35, 223–226. [Google Scholar]
- Sayasone, S.; Odermatt, P.; Vongphrachanh, P.; Keoluangkot, V.; Dupouy-Camet, J.; Newton, P.N.; Strobel, M. A Trichinellosis outbreak in Borikhamxay Province, Lao PDR. Trans. R. Soc. Trop. Med. Hyg. 2006, 100, 1126–1129. [Google Scholar] [CrossRef]
- Nhan, D.; De, N. Emergence of Trichinellosis in Tuan Giao District, Dien Bien Province. J. Malar. Parasite Dis. Control 2004, 6, 76–79. [Google Scholar]
- Taylor, W.R.J.; Tran, G.V.; Nguyen, T.Q.; Dang, D.V.; Nguyen, V.K.; Nguyen, C.T.; Nguyen, L.T.; Luong, C.Q.; Scott, T.; Thach, D.T.C.; et al. Acute Febrile Myalgia in Vietnam Due to Trichinellosis Following the Consumption of Raw Pork. Clin. Infect. Dis. 2009, 49, e79–e83. [Google Scholar] [CrossRef]
- Toan, N.; De, N.; Son, D.; Linh, P. Report of an epidemic area of trichinellosis in Tuan Giao district, Lai Chau province. J. Malar. Parasite Dis. Control. 2002, 1, 76–79. [Google Scholar]
- Zinsstag, J.; Schelling, E.; Crump, L.; Whittaker, M.; Tanner, M.; Stephen, C. One Health: The Theory and Practice of Integrated Health Approaches, 2nd ed.; CABI: Wallingford, UK, 2020. [Google Scholar]
- Okello, W.O.; Okello, A.L.; Inthavong, P.; Tiemann, T.; Phengsivalouk, A.; Devleesschauwer, B.; Shaw, A.; Allen, J. Improved methods to capture the total societal benefits of zoonotic disease control: Demonstrating the cost-effectiveness of an integrated control programme for Taenia solium, soil transmitted helminths and classical swine fever in Northern Lao PDR. PLoS Negl. Trop. Dis. 2018, 12, e0006782. [Google Scholar] [CrossRef]
| Commune | Number of Indigenous Pigs | Number of Pigs Sampled | Number of Households Interviewed |
|---|---|---|---|
| Cao Son | 1001 | 76 | 26 |
| Giap Dat | 890 | 68 | 24 |
| Tan Minh | 790 | 60 | 24 |
| Doan Ket | 787 | 60 | 23 |
| Muong Chieng | 647 | 50 | 18 |
| Trung Thanh | 494 | 38 | 16 |
| Total | 4609 | 352 | 131 |
| Commune | Number of Households * | Number of Pigs | ||||
|---|---|---|---|---|---|---|
| N | Seropositive with trichinellosis n (%) | Seropositive with T. Solium Cysticercosis n (%) | N | Seropositive with trichinellosis n (%) | Seropositive with T. Solium Cysticercosis n (%) | |
| Tan Minh | 24 | 11 (45.8) | 0 (0) | 60 | 13 (21.7) | 0 (0) |
| Cao Son | 26 | 9 (34.6) | 1 (3.8) | 76 | 10 (13.2) | 1 (1.3) |
| Giap Dat | 24 | 8 (33.3) | 2 (8.3) | 68 | 10 (14.7) | 2 ** (2.9) |
| Doan Ket | 23 | 5 (21.7) | 2 (8.7) | 60 | 7 (11.7) | 3 (5.0) |
| Muong Chieng | 18 | 5 (27.8) | 0 (0) | 50 | 5 (10.0) | 0 (0) |
| Trung Thanh | 16 | 2 (12.5) | 0 (0) | 38 | 3 (7.9) | 0 (0) |
| Total | 131 | 40 (30.5) | 5 (3.8) | 352 | 48 (13.6) | 6 (1.7) |
| Individual Pig Level (n = 352) | Pig Farm Level (n = 131) | |||||
|---|---|---|---|---|---|---|
| Variable | Number of Positive Pigs/n | ORadj (95% CI) | p-Value | Number of Positive Farms/n | ORadj (95% CI) | p-Value |
| Sex of pigs | ||||||
| Female | 35/205 | Ref | - | |||
| Male | 13/147 | 0.5 (0.2–0.9) | 0.04 | |||
| Age groups | ||||||
| ≤6 months | 19/199 | Ref | - | |||
| 7–12 months | 16/105 | 1.8 (0.8–4.1) | 0.18 | |||
| >12 months | 13/47 | 4.2 (1.6–11) | 0.003 | |||
| Weight of pigs | ||||||
| ≤15 kg | 22/209 | Ref | ||||
| >15 kg | 26/143 | 2.0 (1.0–4.0) | 0.07 | |||
| Farm scale | ||||||
| ≥10 pigs/farm | 12/84 | Ref | - | 29/102 | Ref | - |
| <10 pigs/farm | 36/268 | 0.9 (0.4–2.3) | 0.84 | 11/29 | 0.65 (0.42–1.01) | 0.33 |
| Pig raising system | ||||||
| Fenced | 15/123 | Ref | - | 12/45 | Ref | - |
| Free roaming | 11/53 | 2.2 (0.7–6.6) | 0.18 | 9/21 | 2.06 (1.18–3.59) | 0.19 |
| Semi | 22/176 | 1.0 (0.4–2.5) | 0.92 | 19/65 | 1.14 (0.74–1.75) | 0.76 |
| Toilet type | ||||||
| Pit latrine | 36/297 | Ref | - | 31/111 | Ref | - |
| Flushing | 12/55 | 2.3 (0.9–6.1) | 0.09 | 9/20 | 2.17 (1.3–3.63) | 0.13 |
| Pig dewormed recently | ||||||
| >1 month | 31/215 | Ref | - | 35/108 | Ref | - |
| ≤1 month | 17/137 | 0.8 (0.4–1.8) | 0.64 | 5/23 | 1.73 (1.00–2.99) | 0.32 |
| Keeping dog at farm | ||||||
| No | 7/86 | Ref | - | 6/33 | Ref | - |
| Yes | 41/266 | 2.1 (0.8–5.8) | 0.13 | 33/98 | 1.90 (1.17–3.08) | 0.18 |
| Keeping cat at farm | ||||||
| No | 24/192 | Ref | - | 17/57 | Ref | - |
| Yes | 24/160 | 1.3 (0.6–2.7) | 0.55 | 23/74 | 1.21 (0.82–1.77) | 0.62 |
| Presence of rodents at farm | ||||||
| No | 3/34 | Ref | - | 3/12 | Ref | - |
| Yes | 42/299 | 1.7 (0.4–7.9) | 0.47 | 34/112 | 1.35 (0.66–2.75) | 0.67 |
| Household members consume raw pork * | ||||||
| No | 33/250 | Ref | - | 28/94 | Ref | - |
| Yes | 15/102 | 1.1 (0.5–2.6) | 0.79 | 12/37 | 1.14 (0.74–1.75) | 0.76 |
| Characteristics | Male (n = 91) | Female (n = 40) | Total (n = 131) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age group | ||||||
| 18–30 | 10 | 11.0 | 8 | 20.0 | 18 | 13.7 |
| 31–45 | 45 | 49.4 | 16 | 40.0 | 61 | 46.6 |
| 46–60 | 32 | 35.2 | 8 | 20.0 | 40 | 30.5 |
| >60 | 4 | 4.4 | 8 | 20.0 | 12 | 9.2 |
| Ethnic group | ||||||
| Tay | 81 | 89.0 | 33 | 82.5 | 114 | 87.0 |
| Dao | 9 | 9.9 | 5 | 12.5 | 14 | 10.7 |
| Muong | 0 | 0 | 2 | 5.0 | 2 | 1.5 |
| Kinh | 1 | 1.1 | 0 | 0 | 1 | 0.8 |
| Occupation | ||||||
| Farmer | 90 | 99.0 | 39 | 97.5 | 129 | 98.5 |
| Other | 1 | 1.0 | 1 | 2.5 | 2 | 1.5 |
| Education | ||||||
| Primary school or less | 24 | 26.4 | 17 | 42.5 | 41 | 31.3 |
| Secondary school | 34 | 37.4 | 16 | 40.0 | 50 | 38.2 |
| High school or higher | 33 | 36.2 a | 7 | 17.5 b | 40 | 30.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Le, T.T.-H.; Vu-Thi, N.; Dang-Xuan, S.; Nguyen-Viet, H.; Pham-Duc, P.; Nguyen-Thanh, L.; Pham-Thi, N.; Noh, J.; Mayer-Scholl, A.; Baumann, M.; et al. Seroprevalence and Associated Risk Factors of Trichinellosis and T. Solium Cysticercosis in Indigenous Pigs in Hoa Binh Province, Vietnam. Trop. Med. Infect. Dis. 2022, 7, 57. https://doi.org/10.3390/tropicalmed7040057
Le TT-H, Vu-Thi N, Dang-Xuan S, Nguyen-Viet H, Pham-Duc P, Nguyen-Thanh L, Pham-Thi N, Noh J, Mayer-Scholl A, Baumann M, et al. Seroprevalence and Associated Risk Factors of Trichinellosis and T. Solium Cysticercosis in Indigenous Pigs in Hoa Binh Province, Vietnam. Tropical Medicine and Infectious Disease. 2022; 7(4):57. https://doi.org/10.3390/tropicalmed7040057
Chicago/Turabian StyleLe, Trang Thi-Huyen, Nga Vu-Thi, Sinh Dang-Xuan, Hung Nguyen-Viet, Phuc Pham-Duc, Luong Nguyen-Thanh, Ngoc Pham-Thi, John Noh, Anne Mayer-Scholl, Maximilian Baumann, and et al. 2022. "Seroprevalence and Associated Risk Factors of Trichinellosis and T. Solium Cysticercosis in Indigenous Pigs in Hoa Binh Province, Vietnam" Tropical Medicine and Infectious Disease 7, no. 4: 57. https://doi.org/10.3390/tropicalmed7040057
APA StyleLe, T. T.-H., Vu-Thi, N., Dang-Xuan, S., Nguyen-Viet, H., Pham-Duc, P., Nguyen-Thanh, L., Pham-Thi, N., Noh, J., Mayer-Scholl, A., Baumann, M., Meemken, D., & Unger, F. (2022). Seroprevalence and Associated Risk Factors of Trichinellosis and T. Solium Cysticercosis in Indigenous Pigs in Hoa Binh Province, Vietnam. Tropical Medicine and Infectious Disease, 7(4), 57. https://doi.org/10.3390/tropicalmed7040057






