Epidemiological Characteristics and Spatial-Temporal Analysis of Tuberculosis at the County-Level in Shandong Province, China, 2016–2020
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Data Source
2.3. Statistic Analysis
2.3.1. Time Series Decomposition
2.3.2. Spatial Autocorrelation Analysis
2.3.3. Spatio-Temporal Scan Analysis
3. Results
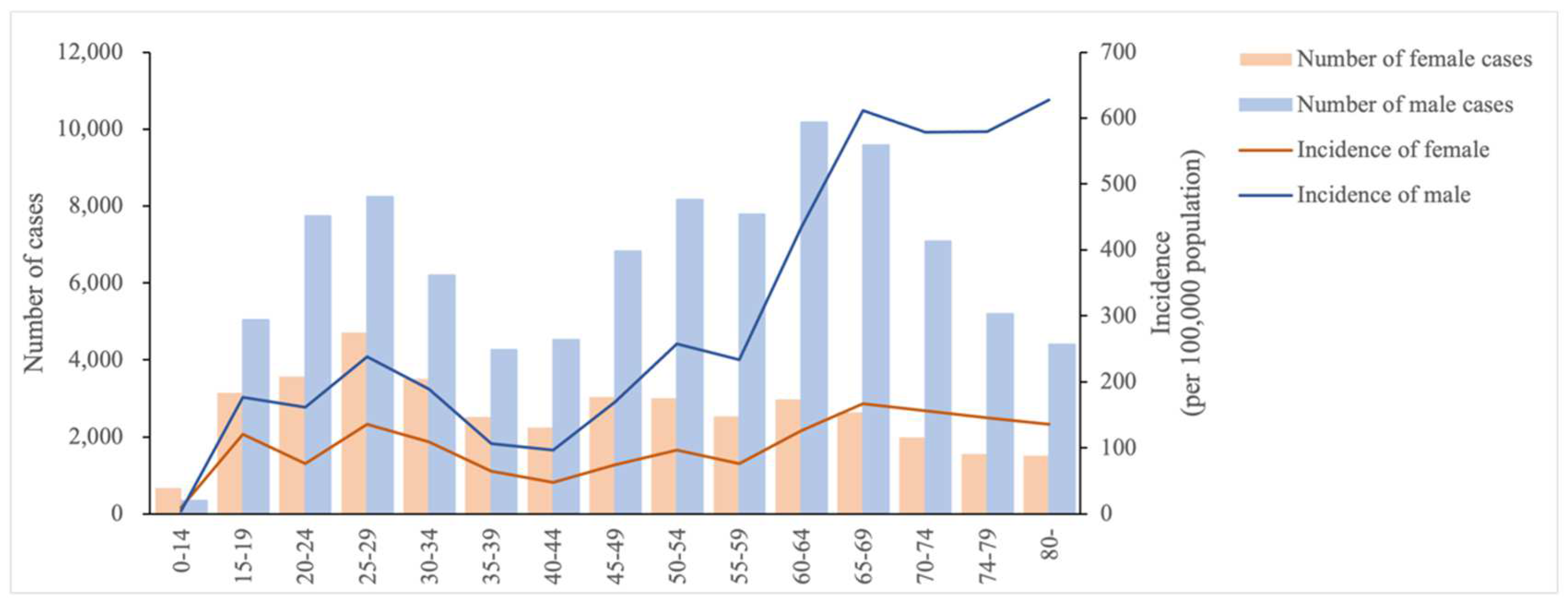
3.1. Descriptive Analysis
3.2. Temporal Pattern
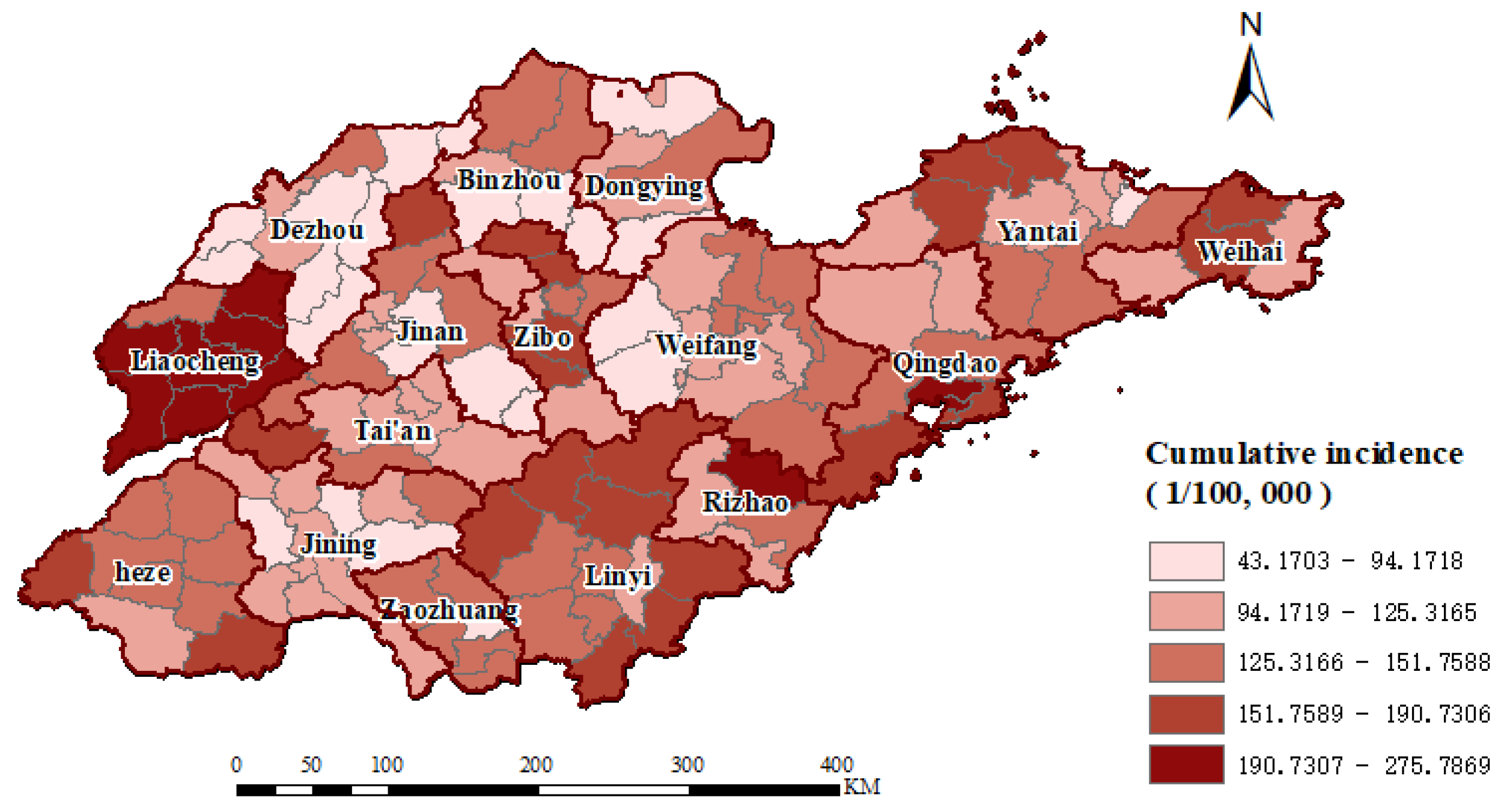
3.3. Spatial Distribution
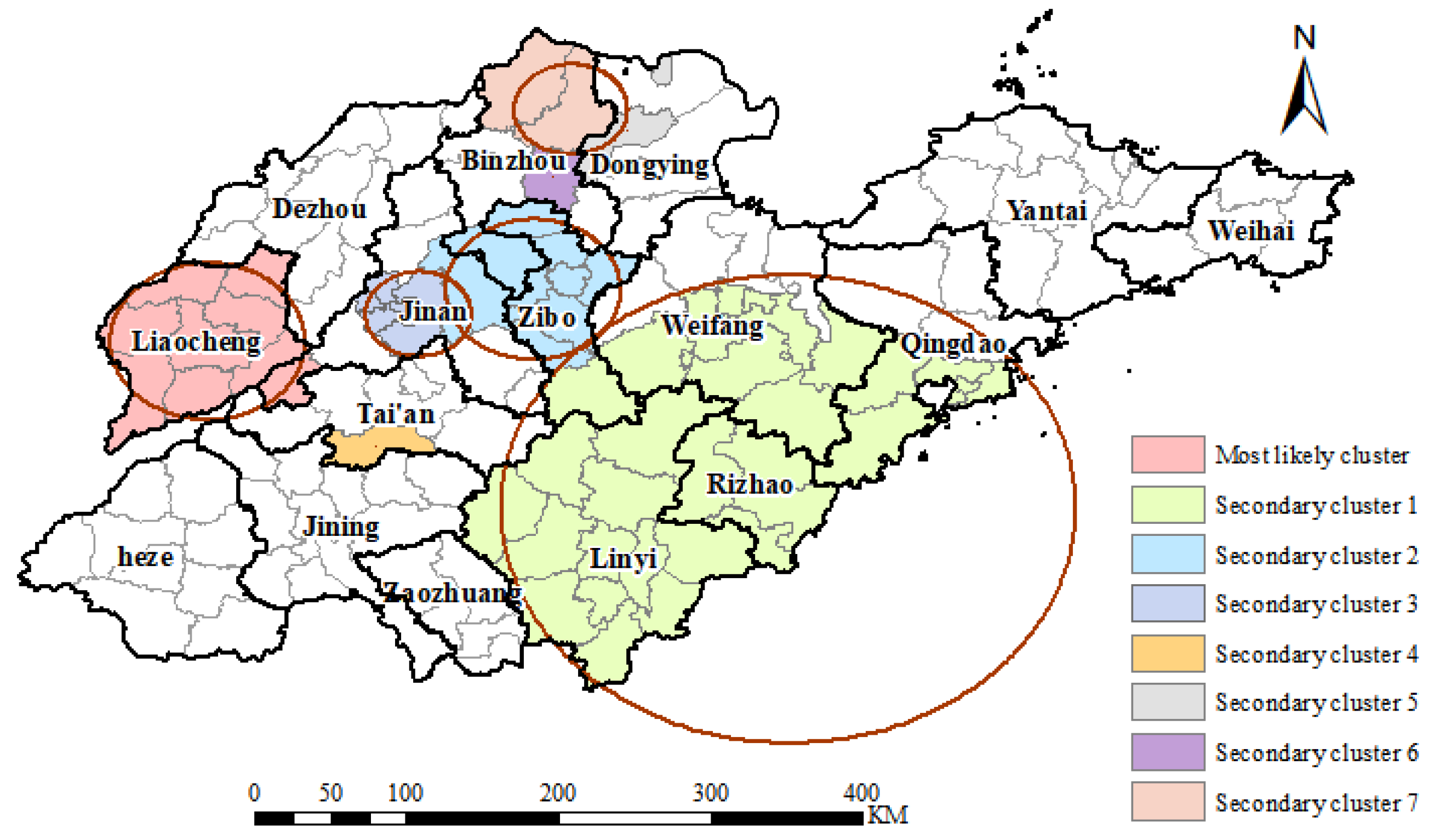
3.4. Spatio-Temporal Distribution
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dannenberg, A.M., Jr.; Rook, G.A. Pathogenesis of pulmonary tuberculosis: An interplay of tissue-damaging and macrophage-activating immune responses—Dual mechanisms that control bacillary multiplication. Tuberc. Pathog. Prot. Control 1994, 459–483. [Google Scholar]
- Behr, M.A.; Edelstein, P.H.; Ramakrishnan, L. Revisiting the timetable of tuberculosis. BMJ 2018, 362, k2738. [Google Scholar] [CrossRef] [PubMed]
- WHO. Global Tuberculosis Report 2020; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. Global Tuberculosis Report 2021: Supplementary Material; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Li, Y.W.; Cheng, J.; Wang, H.; Zhao, F.; Li, X.X.; Tao, W.W.; Bi, X.L.; Jin, J.; Ding, Y.; Geng, H. Spatial-temporal analysis of pulmonary tuberculosis in Shandong province, 2015. Zhonghua Liu Xing Bing Xue Za Zhi 2016, 37, 1257–1261. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, D.; Zhang, Y.; Xue, X.; Zhang, S.; Chen, M.; Liu, X.; Ding, G. Analysis of spatial-temporal distribution of notifiable respiratory infectious diseases in Shandong Province, China during 2005–2014. BMC Public Health 2021, 21, 1597. [Google Scholar] [CrossRef]
- Chen, D.; Lu, H.; Zhang, S.; Yin, J.; Liu, X.; Zhang, Y.; Dai, B.; Li, X.; Ding, G. The association between extreme temperature and pulmonary tuberculosis in Shandong Province, China, 2005–2016: A mixed method evaluation. BMC Infect. Dis. 2021, 21, 402. [Google Scholar] [CrossRef]
- Jiang, H.; Liu, M.; Zhang, Y.; Yin, J.; Li, Z.; Zhu, C.; Li, Q.; Luo, X.; Ji, T.; Zhang, J. Changes in incidence and epidemiological characteristics of pulmonary tuberculosis in mainland China, 2005–2016. JAMA Netw. Open 2021, 4, e215302. [Google Scholar] [CrossRef]
- Wang, Y.-S.; Zhu, W.-L.; Li, T.; Chen, W.; Wang, W.-B. Changes in newly notified cases and control of tuberculosis in China: Time-series analysis of surveillance data. Infect. Dis. Poverty 2021, 10, 16. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Tuberculosis Infection Prevention and Control: 2019 Update; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Alene, K.A.; Xu, Z.; Bai, L.; Yi, H.; Tan, Y.; Gray, D.J.; Viney, K.; Clements, A.C.A. Spatiotemporal Patterns of Tuberculosis in Hunan Province, China. Int. J. Environ. Res. Public Health 2021, 18, 6778. [Google Scholar] [CrossRef]
- Sadeq, M.; Bourkadi, J.E. Spatiotemporal distribution and predictors of tuberculosis incidence in Morocco. Infect. Dis. Poverty 2018, 7, 43. [Google Scholar] [CrossRef]
- Cleveland, R.B.; Cleveland, W.S.; McRae, J.E.; Terpenning, I. STL: A seasonal-trend decomposition. J. Off. Stat. 1990, 6, 3–73. [Google Scholar]
- Ho, C.C.; Ting, C.-Y. Time series analysis and forecasting of dengue using open data. In Proceedings of the International Visual Informatics Conference, Bangi, Malaysia, 17–19 November 2015; pp. 51–63. [Google Scholar]
- Pfeiffer, D.U.; Robinson, T.P.; Stevenson, M.; Stevens, K.B.; Rogers, D.J.; Clements, A.C. Spatial clustering of disease and global estimates of spatial clustering. In Spatial Analysis in Epidemiology; Oxford University Press: Oxford, UK, 2008; pp. 32–44. [Google Scholar]
- Moran, P.A. The interpretation of statistical maps. J. R. Stat. Society. Ser. B (Methodol.) 1948, 10, 243–251. [Google Scholar] [CrossRef]
- Ord, J.K.; Getis, A. Local spatial autocorrelation statistics: Distributional issues and an application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- M., K. SaTScan User Guide for Version 10.1. Available online: https://www.satscan.org/techdoc.html (accessed on 1 September 2022).
- Tango, T.; Takahashi, K. A flexibly shaped spatial scan statistic for detecting clusters. Int. J. Health Geogr. 2005, 4, 11. [Google Scholar] [CrossRef]
- Rhines, A.S. The role of sex differences in the prevalence and transmission of tuberculosis. Tuberculosis 2013, 93, 104–107. [Google Scholar] [CrossRef]
- Lin, H.-H.; Ezzati, M.; Murray, M. Tobacco smoke, indoor air pollution and tuberculosis: A systematic review and meta-analysis. PLoS Med. 2007, 4, e20. [Google Scholar] [CrossRef]
- Lönnroth, K.; Williams, B.G.; Stadlin, S.; Jaramillo, E.; Dye, C. Alcohol use as a risk factor for tuberculosis—A systematic review. BMC Public Health 2008, 8, 289. [Google Scholar] [CrossRef]
- Slama, K.; Chiang, C.; Enarson, D.; Hassmiller, K.; Fanning, A.; Gupta, P.; Ray, C. Tobacco and tuberculosis: A qualitative systematic review and meta-analysis. Int. J. Tuberc. Lung Dis. 2007, 11, 1049–1061. [Google Scholar]
- Morris, J.; Heady, J. Mortality in relation to the physical activity of work: A preliminary note on experience in middle age. Br. J. Ind. Med. 1953, 10, 245. [Google Scholar] [CrossRef]
- Cegielski, J.; McMurray, D. The relationship between malnutrition and tuberculosis: Evidence from studies in humans and experimental animals. Int. J. Tuberc. Lung Dis. 2004, 8, 286–298. [Google Scholar]
- Spence, D.P.; Hotchkiss, J.; Williams, C.S.; Davies, P.D. Tuberculosis and poverty. Br. Med. J. 1993, 307, 759–761. [Google Scholar] [CrossRef]
- Zhang, S.; Li, X.; Zhang, T.; Fan, Y.; Li, Y. The experiences of high school students with pulmonary tuberculosis in China: A qualitative study. BMC Infect. Dis. 2016, 16, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pan, D.; Lan, R.; Graviss, E.A.; Lin, D.; Liang, D.; McNeil, E.; Lin, M.; Chongsuvivatwong, V. Adolescent tuberculosis associated with tuberculosis exposure in classrooms and dorm rooms in Guangxi, China. Int. J. Infect. Dis. 2019, 78, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Li, A.; Li, D.; Liu, Y.; Du, Y.; Pei, T.; Ma, T.; Zhou, C. Difference of urban development in China from the perspective of passenger transport around Spring Festival. Appl. Geogr. 2017, 87, 85–96. [Google Scholar] [CrossRef]
- Liu, M.-Y.; Li, Q.-H.; Zhang, Y.-J.; Ma, Y.; Liu, Y.; Feng, W.; Hou, C.-B.; Amsalu, E.; Li, X.; Wang, W.; et al. Spatial and temporal clustering analysis of tuberculosis in the mainland of China at the prefecture level, 2005–2015. Infect. Dis. Poverty 2018, 7, 106. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Qiu, Y.; Yang, R.; Li, L.; Hou, J.; Lu, K.; Xu, L. The characteristics of spatial-temporal distribution and cluster of tuberculosis in Yunnan Province, China, 2005–2018. BMC Public Health 2019, 19, 1715. [Google Scholar] [CrossRef]
- Li, Y.; Zhu, L.; Lu, W.; Chen, C.; Yang, H. Seasonal variation in notified tuberculosis cases from 2014 to 2018 in eastern China. J. Int. Med. Res. 2020, 48, 0300060520949031. [Google Scholar] [CrossRef]
- Chen, R.; Yin, P.; Meng, X.; Liu, C.; Wang, L.; Xu, X.; Ross, J.A.; Tse, L.A.; Zhao, Z.; Kan, H.; et al. Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am. J. Respir. Crit. Care Med. 2017, 196, 73–81. [Google Scholar] [CrossRef]
- Fennelly, K.P.; Nardell, E.A. The relative efficacy of respirators and room ventilation in preventing occupational tuberculosis. Infect. Control Hosp. Epidemiol. 1998, 19, 754–759. [Google Scholar] [CrossRef]
- Pasco, J.A.; Henry, M.J.; Kotowicz, M.A.; Sanders, K.M.; Seeman, E.; Pasco, J.R.; Schneider, H.G.; Nicholson, G.C. Seasonal periodicity of serum vitamin D and parathyroid hormone, bone resorption, and fractures: The Geelong Osteoporosis Study. J. Bone Miner. Res. 2004, 19, 752–758. [Google Scholar] [CrossRef]
- Koh, G.C.; Hawthorne, G.; Turner, A.M.; Kunst, H.; Dedicoat, M. Tuberculosis incidence correlates with sunshine: An ecological 28-year time series study. PLoS ONE 2013, 8, e57752. [Google Scholar] [CrossRef]
- Fares, A. Seasonality of tuberculosis. J. Glob. Infect. Dis. 2011, 3, 46. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, M.; Chen, Y.; Ma, L.; Yadikaer, R.; Lu, Y.; Lou, P.; Pu, Y.; Xiang, R.; Rui, B. A study on the relationship between air pollution and pulmonary tuberculosis based on the general additive model in Wulumuqi, China. Int. J. Infect. Dis. 2020, 96, 42–47. [Google Scholar] [CrossRef]
- Liao, W.-B.; Ju, K.; Gao, Y.-M.; Pan, J. The association between internal migration and pulmonary tuberculosis in China, 2005–2015: A spatial analysis. Infect. Dis. Poverty 2020, 9, 5. [Google Scholar] [CrossRef]
- Nie, Y.; Lu, Y.; Wang, C.; Yang, Z.; Sun, Y.; Zhang, Y.; Tian, M.; Rifhat, R.; Zhang, L. Effects and Interaction of Meteorological Factors on Pulmonary Tuberculosis in Urumqi, China, 2013–2019. Front. Public Health 2022, 10, 951578. [Google Scholar] [CrossRef]
- Liu, F.; Zhang, Z.; Chen, H.; Nie, S. Associations of ambient air pollutants with regional pulmonary tuberculosis incidence in the central Chinese province of Hubei: A Bayesian spatial-temporal analysis. Environ. Health 2020, 19, 51. [Google Scholar] [CrossRef]


| Characteristics | 2016 | 2017 | 2018 | 2019 | 2020 | 2016–2020 |
|---|---|---|---|---|---|---|
| Gender | ||||||
| male | 21,327 | 20,664 | 19,512 | 18,563 | 15,489 | 95,554 |
| female | 8632 | 8504 | 8062 | 7630 | 6802 | 39,631 |
| Occupation | ||||||
| farmer | 22,226 | 21,149 | 19,252 | 17,825 | 15,065 | 95,517 |
| unemployed | 2670 | 2949 | 2867 | 2802 | 2457 | 13,745 |
| worker | 1302 | 1185 | 1216 | 1291 | 1072 | 6066 |
| student | 1178 | 1291 | 1621 | 1664 | 1420 | 7174 |
| retired | 885 | 910 | 941 | 996 | 836 | 4568 |
| others | 1698 | 1684 | 1677 | 1615 | 1441 | 8115 |
| Total | 29,959 | 29,168 | 27,574 | 26,193 | 22,291 | 135,185 |
| Year | Moran’s I | Z-Score | p-Value |
|---|---|---|---|
| 2016 | 0.245016 | 3.924002 | 0.000087 |
| 2017 | 0.348460 | 5.532868 | <0.000001 |
| 2018 | 0.526354 | 8.161494 | <0.000001 |
| 2019 | 0.341232 | 5.395392 | <0.000001 |
| 2020 | 0.336923 | 5.324681 | <0.000001 |
| 2016–2020 | 0.429948 | 6.793433 | <0.000001 |
| Cluster Type | Time Frame | N | LLR | RR | p-Value |
|---|---|---|---|---|---|
| Most likely cluster | 1 May 2016–31 October 2018 | 9 | 904.75 | 1.72 | <0.001 |
| Secondary cluster 1 | 1 March 2016–31 August 2018 | 32 | 568.65 | 1.29 | <0.001 |
| Secondary cluster 2 | 1 March 2016–30 June 2018 | 9 | 92.58 | 1.24 | <0.001 |
| Secondary cluster 3 | 1 January 2019–31 January 2019 | 5 | 84.57 | 2.85 | <0.001 |
| Secondary cluster 4 | 1 July 2016–31 December 2016 | 1 | 73.76 | 2.34 | <0.001 |
| Secondary cluster 5 | 1 November 2016–31 December 2016 | 1 | 34.98 | 4.00 | <0.001 |
| Secondary cluster 6 | 1 July 2018–31 August 2018 | 1 | 21.18 | 2.44 | <0.001 |
| Secondary cluster 7 | 1 January 2016–31 December 2017 | 2 | 18.22 | 1.29 | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duan, Y.; Cheng, J.; Liu, Y.; Fang, Q.; Sun, M.; Cheng, C.; Han, C.; Li, X. Epidemiological Characteristics and Spatial-Temporal Analysis of Tuberculosis at the County-Level in Shandong Province, China, 2016–2020. Trop. Med. Infect. Dis. 2022, 7, 346. https://doi.org/10.3390/tropicalmed7110346
Duan Y, Cheng J, Liu Y, Fang Q, Sun M, Cheng C, Han C, Li X. Epidemiological Characteristics and Spatial-Temporal Analysis of Tuberculosis at the County-Level in Shandong Province, China, 2016–2020. Tropical Medicine and Infectious Disease. 2022; 7(11):346. https://doi.org/10.3390/tropicalmed7110346
Chicago/Turabian StyleDuan, Yuqi, Jun Cheng, Ying Liu, Qidi Fang, Minghao Sun, Chuanlong Cheng, Chuang Han, and Xiujun Li. 2022. "Epidemiological Characteristics and Spatial-Temporal Analysis of Tuberculosis at the County-Level in Shandong Province, China, 2016–2020" Tropical Medicine and Infectious Disease 7, no. 11: 346. https://doi.org/10.3390/tropicalmed7110346
APA StyleDuan, Y., Cheng, J., Liu, Y., Fang, Q., Sun, M., Cheng, C., Han, C., & Li, X. (2022). Epidemiological Characteristics and Spatial-Temporal Analysis of Tuberculosis at the County-Level in Shandong Province, China, 2016–2020. Tropical Medicine and Infectious Disease, 7(11), 346. https://doi.org/10.3390/tropicalmed7110346






