Can Patient Navigators Help Potential TB Patients Navigate the Diagnostic and Treatment Pathways? An Implementation Research from India
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Project Details
2.2.1. Public Sector project
Study Setting
Intervention
2.2.2. Private Sector Project
Study Setting
Intervention
2.3. Data Collection
2.4. Analysis
3. Result
3.1. Public Sector Project
3.2. Private Sector Project
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2019; Global TB Report; World Health Organization: Geneva, Switzerland, 2019; ISBN 978-92-4-156571-4. [Google Scholar]
- Cazabon, D.; Alsdurf, H.; Satyanarayana, S.; Nathavitharana, R.; Subbaraman, R.; Daftary, A.; Pai, M. Quality of Tuberculosis Care in High Burden Countries: The Urgent Need to Address Gaps in the Care Cascade. Int. J. Infect. Dis. 2017, 56, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Odone, A.; Roberts, B.; Dara, M.; van den Boom, M.; Kluge, H.; McKee, M. People- and Patient-Centred Care for Tuberculosis: Models of Care for Tuberculosis. Int. J. Tuberc. Lung Dis. 2018, 22, 133–138. [Google Scholar] [CrossRef] [PubMed]
- George, M. The Fragmentation and Weakening of Institutions of Primary Healthcare. Econ. Polit. Wkly. 2020, 55, 7. [Google Scholar]
- Yellapa, V.; Devadasan, N.; Krumeich, A.; Pant Pai, N.; Vadnais, C.; Pai, M.; Engel, N. How Patients Navigate the Diagnostic Ecosystem in a Fragmented Health System: A Qualitative Study from India. Glob. Health Action 2017, 10, 1350452. [Google Scholar] [CrossRef]
- Engel, N.; Ganesh, G.; Patil, M.; Yellappa, V.; Pant Pai, N.; Vadnais, C.; Pai, M. Barriers to Point-of-Care Testing in India: Results from Qualitative Research across Different Settings, Users and Major Diseases. PLoS ONE 2015, 10, e0135112. [Google Scholar] [CrossRef] [PubMed]
- Storla, D.G.; Yimer, S.; Bjune, G.A. A Systematic Review of Delay in the Diagnosis and Treatment of Tuberculosis. BMC Public Health 2008, 8, 15. [Google Scholar] [CrossRef]
- Bhatnagar, H. User-Experience and Patient Satisfaction with Quality of Tuberculosis Care in India: A Mixed-Methods Literature Review. J. Clin. Tuberc. Mycobact. Dis. 2019, 17, 100127. [Google Scholar] [CrossRef] [PubMed]
- Mukerji, R.; Turan, J.M. Challenges in Accessing and Utilising Health Services for Women Accessing DOTS TB Services in Kolkata, India. Glob. Public Health 2020, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Oxlade, O.; Murray, M. Tuberculosis and Poverty: Why Are the Poor at Greater Risk in India? PLoS ONE 2012, 7, e47533. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandra, A.; Kumar, R.; Kant, S.; Parthasarathy, R.; Krishnan, A. Direct and Indirect Patient Costs of Tuberculosis Care in India. Trop. Med. Int. Health 2020, 25, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Yellappa, V.; Lefèvre, P.; Battaglioli, T.; Narayanan, D.; Van der Stuyft, P. Coping with Tuberculosis and Directly Observed Treatment: A Qualitative Study among Patients from South India. BMC Health Serv. Res. 2016, 16, 283. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mason, P.H.; Roy, A.; Spillane, J.; Singh, P. Social, Historical and Cultural Dimensions of Tuberculosis. J. Biosoc. Sci. 2016, 48, 206–232. [Google Scholar] [CrossRef] [Green Version]
- Garg, T.; Gupta, V.; Sen, D.; Verma, M.; Brouwer, M.; Mishra, R.; Bhardwaj, M. Prediagnostic Loss to Follow-up in an Active Case Finding Tuberculosis Programme: A Mixed-Methods Study from Rural Bihar, India. BMJ Open 2020, 10, e033706. [Google Scholar] [CrossRef] [PubMed]
- Mukerji, R.; Turan, J.M. Exploring Manifestations of TB-Related Stigma Experienced by Women in Kolkata, India. Ann. Glob. Health 2018, 84, 727–735. [Google Scholar] [CrossRef] [Green Version]
- Ali-Faisal, S.F.; Colella, T.J.F.; Medina-Jaudes, N.; Benz Scott, L. The Effectiveness of Patient Navigation to Improve Healthcare Utilization Outcomes: A Meta-Analysis of Randomized Controlled Trials. Patient Educ. Couns. 2017, 100, 436–448. [Google Scholar] [CrossRef]
- Peart, A.; Lewis, V.; Brown, T.; Russell, G. Patient Navigators Facilitating Access to Primary Care: A Scoping Review. BMJ Open 2018, 8, e019252. [Google Scholar] [CrossRef]
- Calhoun, E.A.; Esparza, A. (Eds.) Patient Navigation: Overcoming Barriers to Care; Springer: New York, NY, USA, 2018; ISBN 978-1-4939-6977-7. [Google Scholar]
- Carter, N.; Valaitis, R.K.; Lam, A.; Feather, J.; Nicholl, J.; Cleghorn, L. Navigation Delivery Models and Roles of Navigators in Primary Care: A Scoping Literature Review. BMC Health Serv. Res. 2018, 18, 96. [Google Scholar] [CrossRef] [Green Version]
- Dalton, M.; Holzman, E.; Erwin, E.; Michelen, S.; Rositch, A.F.; Kumar, S.; Vanderpuye, V.; Yeates, K.; Liebermann, E.J.; Ginsburg, O. Patient Navigation Services for Cancer Care in Low-and Middle-Income Countries: A Scoping Review. PLoS ONE 2019, 14, e0223537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bernardo, B.M.; Zhang, X.; Hery, C.M.B.; Meadows, R.J.; Paskett, E.D. The Efficacy and Cost-Effectiveness of Patient Navigation Programs across the Cancer Continuum: A Systematic Review. Cancer 2019, 125, 2747–2761. [Google Scholar] [CrossRef] [Green Version]
- Sinha, P.; Shenoi, S.V.; Friedland, G.H. Opportunities for Community Health Workers to Contribute to Global Efforts to End Tuberculosis. Glob. Public Health 2019, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Blok, L.; Creswell, J.; Stevens, R.; Brouwer, M.; Ramis, O.; Weil, O.; Klatser, P.; Sahu, S.; Bakker, M.I. A Pragmatic Approach to Measuring, Monitoring and Evaluating Interventions for Improved Tuberculosis Case Detection. Int. Health 2014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Registrar General of India Census of India 2011; Office of the Registrar General Census Commissioner: New Delhi, India, 2011.
- Socio-Economic Caste Census 2011; Ministry of Rural Development, Government of India: New Delhi, India, 2011.
- Annual Health Survey 2011-12, Bihar Factsheet; Office of the Registrar General & Census Commissioner: New Delhi, India, 2011.
- International Institute for Population Sciences. NFHS 4 Factsheet Samastipur. National Family and Health Survey. International Institute for Population Sciences: Mumbai, India. p. 4. Available online: http://rchiips.org/nfhs/factsheet_nfhs-4.shtml (accessed on 3 September 2021).
- Central TB Division. India TB Report 2018: Revised National Tuberculosis Control Program—Annual Status Report; TB India; Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India: New Delhi, India, 2018; p. 156.
- Central TB Division. India TB Report 2019: Revised National Tuberculosis Control Program—Annual Status Report; TB India; Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India: New Delhi, India, 2019.
- Garg, T.; Bhardwaj, M.; Deo, S. Role of Community Health Workers in Improving Cost Efficiency in an Active Case Finding Tuberculosis Programme: An Operational Research Study from Rural Bihar, India. BMJ Open 2020, 10, e036625. [Google Scholar] [CrossRef] [PubMed]
- Office of the Registrar General, India. SRS Bulletin, Sample Registration System; Vital Statistics Division, Office of the Registrar General, India: New Delhi, India, 2020. [Google Scholar]
- Office of the Registrar General, India. Special Bulletin on Maternal Mortality in India 2015-17, Sample Registration System; Office of the Registrar General & Census Commissioner, India: New Delhi, India, 2019. [Google Scholar]

| Indicators | 2017 | 2018 | Total | ||||
|---|---|---|---|---|---|---|---|
| Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | ||
| Number of people screened | 1964 | 2846 | 3431 | 2993 | 3187 | 2483 | 16,904 |
| Number of people identified with TB symptoms | 1590 | 2539 | 3126 | 2641 | 2817 | 2119 | 14,832 |
| Number of people identified with TB symptoms tested for TB | 861 | 1468 | 1933 | 1603 | 1597 | 1161 | 8623 |
| Number of people with microbiologically confirmed TB (Bac+) | 137 | 144 | 184 | 172 | 147 | 104 | 888 |
| Number of people diagnosed with TB (all forms) | 284 | 302 | 324 | 327 | 256 | 157 | 1650 |
| Number of Bac+ TB patients started on treatment | 135 | 142 | 180 | 162 | 143 | 100 | 862 |
| Number of all forms TB patients started on treatment | 279 | 296 | 316 | 311 | 250 | 148 | 1600 |
| Number of Bac+ TB patients successfully treated | 130 | 127 | 172 | 149 | 134 | 87 | 799 |
| Number of all forms TB patients successfully treated | 273 | 279 | 308 | 293 | 235 | 131 | 1519 |
| % tested of those with TB symptoms | 54% | 58% | 62% | 61% | 57% | 55% | 58% |
| Pre-treatment lost to follow-up (All Forms) | 2% | 2% | 2% | 5% | 2% | 6% | 3% |
| Treatment Success Rate (All Forms) | 98% | 94% | 97% | 94% | 94% | 89% | 95% |
| TB Case | Historical Baseline Notifications | Implementation Period Notifications | Additional Cases | Change from BASELINE (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2017 | 2018 | |||||||||||
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | |||
| All Forms | 141 | 170 | 121 | 100 | 116 | 131 | 228 | 266 | 283 | 304 | 292 | 136 | 730 | 94% |
| Microbiologically-confirmed | 66 | 66 | 59 | 44 | 55 | 50 | 74 | 97 | 98 | 142 | 110 | 86 | 267 | 79% |
| Indicators | Intervention | Total | |
|---|---|---|---|
| Diagnostic Hub | Private Provider | ||
| Number of people identified with TB symptoms | 12,041 | 0 | 12,041 |
| Number of people identified with TB symptoms tested for TB | 12,041 | 0 | 12,041 |
| Number of people with microbiologically confirmed TB (Bac+) | 2193 | 947 | 3140 |
| Number of people diagnosed with TB (all forms) | 2403 | 3362 | 5765 |
| Number of Bac+ TB patients started on treatment | 2193 | 947 | 3140 |
| Number of all forms TB patients started on treatment | 2403 | 3362 | 5765 |
| Number of Bac+ TB patients successfully treated # | 891 | 168 | 1059 |
| Number of all forms TB patients successfully treated # | 1791 | 716 | 2507 |
| % tested of those with TB symptoms | 100% | - | 100% |
| Pre-treatment lost to follow-up (All Forms) | 0% | 0% | 0% |
| Treatment Success Rate (All Forms) # | 75% | 21% | 43% |
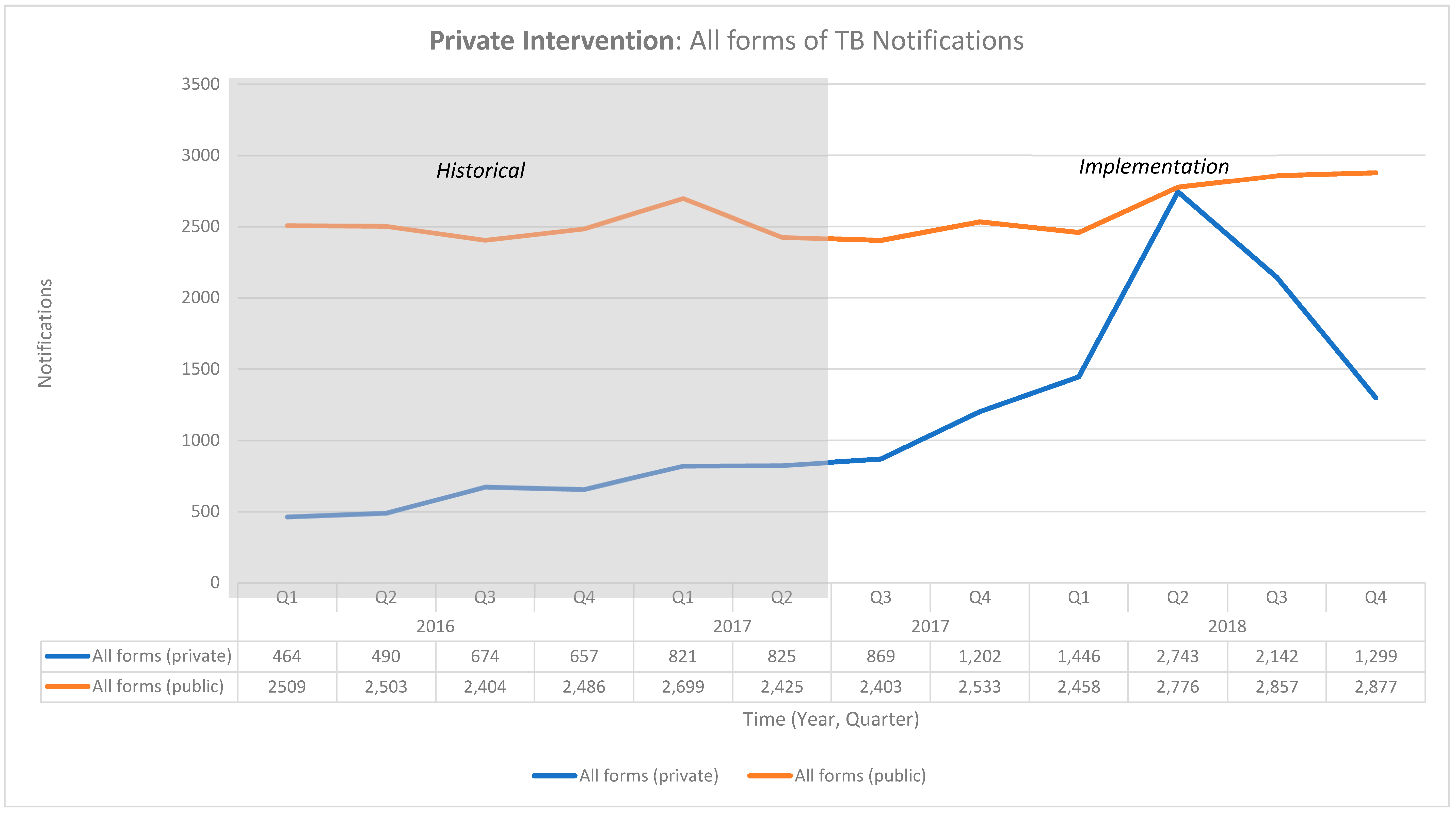
| Historical Baseline Notifications | Implementation Period Notifications | Additional Cases | Change from BASELINE (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2017 | 2018 | |||||||||||
| Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | Q1 | Q2 | Q3 | Q4 | |||
| All forms (private) | 464 | 490 | 674 | 657 | 821 | 825 | 869 | 1202 | 1446 | 2743 | 2142 | 1299 | 5770 | 147% |
| All forms (public) | 2509 | 2503 | 2404 | 2486 | 2699 | 2425 | 2403 | 2533 | 2458 | 2776 | 2857 | 2877 | 878 | 6% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garg, T.; Panibatla, V.; Carel, J.P.; Shanta, A.; Bhardwaj, M.; Brouwer, M. Can Patient Navigators Help Potential TB Patients Navigate the Diagnostic and Treatment Pathways? An Implementation Research from India. Trop. Med. Infect. Dis. 2021, 6, 200. https://doi.org/10.3390/tropicalmed6040200
Garg T, Panibatla V, Carel JP, Shanta A, Bhardwaj M, Brouwer M. Can Patient Navigators Help Potential TB Patients Navigate the Diagnostic and Treatment Pathways? An Implementation Research from India. Tropical Medicine and Infectious Disease. 2021; 6(4):200. https://doi.org/10.3390/tropicalmed6040200
Chicago/Turabian StyleGarg, Tushar, Vikas Panibatla, Joseph P. Carel, Achanta Shanta, Manish Bhardwaj, and Miranda Brouwer. 2021. "Can Patient Navigators Help Potential TB Patients Navigate the Diagnostic and Treatment Pathways? An Implementation Research from India" Tropical Medicine and Infectious Disease 6, no. 4: 200. https://doi.org/10.3390/tropicalmed6040200
APA StyleGarg, T., Panibatla, V., Carel, J. P., Shanta, A., Bhardwaj, M., & Brouwer, M. (2021). Can Patient Navigators Help Potential TB Patients Navigate the Diagnostic and Treatment Pathways? An Implementation Research from India. Tropical Medicine and Infectious Disease, 6(4), 200. https://doi.org/10.3390/tropicalmed6040200






