Pregnancy, Birth, Infant, and Early Childhood Neurodevelopmental Outcomes among a Cohort of Women with Symptoms of Zika Virus Disease during Pregnancy in Three Surveillance Sites, Project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016–2018
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria and Medical Records Abstraction
2.2. Specimen Collection and Testing
2.3. Laboratory Evidence of Zika Virus Infection during Pregnancy
2.4. Zika-Associated Birth Defects and Other Pregnancy Outcomes
2.5. Early Childhood Neurodevelopmental Outcomes
2.6. Data Entry and Analysis
3. Results
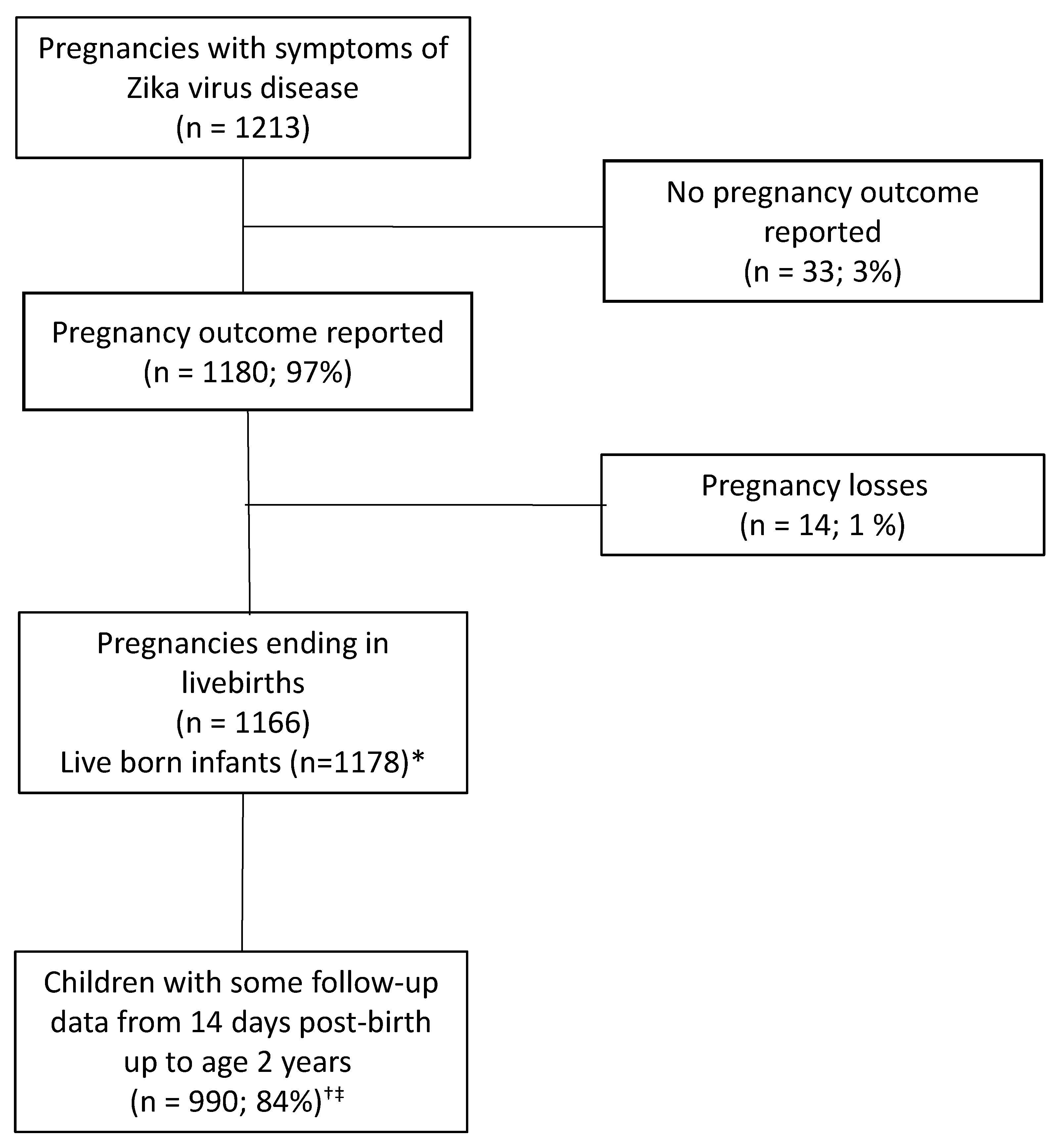
3.1. Characteristics of the Study Population
3.2. Pregnancy and Infant Outcomes including Zika-Associated Birth Defects
3.3. Zika Virus Testing Results
3.4. Early Childhood Neurodevelopmental Outcomes
4. Discussion
4.1. Limitations
4.2. Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Disclaimer
References
- Peterson, A.T.; Osorio, J.; Qiao, H.; Escobar, L.E. Zika Virus, Elevation, and Transmission Risk. PLoS Curr. 2016, 8, 8. [Google Scholar] [CrossRef]
- Calvet, G.; Aguiar, R.S.; Melo, A.S.O.; Sampaio, S.A.; de Filippis, I.; Fabri, A.; Araujo, E.S.M.; de Sequeira, P.C.; de Mendonça, M.C.L.; de Oliveira, L.; et al. Detection and sequencing of Zika virus from amniotic fluid of fetuses with microcephaly in Brazil: A case study. Lancet Infect. Dis. 2016, 16, 653–660. [Google Scholar] [CrossRef] [Green Version]
- Noronha, L.; Zanluca, C.; Azevedo, M.L.V.; Luz, K.G.; Dos Santos, C.N.D. Zika virus damages the human placental barrier and presents marked fetal neurotropism. Memórias Inst. Oswaldo Cruz 2016, 111, 287–293. [Google Scholar] [CrossRef]
- Brasil, P.; Calvet, G.A.; Siqueira, A.M.; Wakimoto, M.; De Sequeira, P.C.; Nobre, A.; Quintana, M.D.S.B.; De Mendonça, M.C.L.; Lupi, O.; De Souza, R.V.; et al. Zika Virus Outbreak in Rio de Janeiro, Brazil: Clinical Characterization, Epidemiological and Virological Aspects. PLoS Negl. Trop. Dis. 2016, 10, e0004636. [Google Scholar] [CrossRef]
- de Araújo, T.V.B.; Rodrigues, L.C.; Ximenes, R.A.D.A.; Miranda-Filho, D.D.B.; Montarroyos, U.R.; de Melo, A.P.L.; Valongueiro, S.; Albuquerque, M.D.F.P.M.D.; Souza, W.; Braga, C.; et al. Association between Zika virus infection and microcephaly in Brazil, January to May, 2016: Preliminary report of a case-control study. Lancet Infect. Dis. 2016, 16, 1356–1363. [Google Scholar] [CrossRef] [Green Version]
- Honein, M.A.; Dawson, A.L.; Petersen, E.E.; Jones, A.M.; Lee, E.H.; Yazdy, M.; Ahmad, N.; Macdonald, J.; Evert, N.; Bingham, A.; et al. Birth Defects Among Fetuses and Infants of US Women with Evidence of Possible Zika Virus Infection During Pregnancy. JAMA 2017, 317, 59–68. [Google Scholar] [CrossRef]
- Rasmussen, S.A.; Jamieson, D.J.; Honein, M.A.; Petersen, L.R. Zika Virus and Birth Defects—Reviewing the Evidence for Causality. N. Engl. J. Med. 2016, 374, 1981–1987. [Google Scholar] [CrossRef] [PubMed]
- Cauchemez, S.; Besnard, M.; Bompard, P.; Dub, T.; Guillemette-Artur, P.; Eyrolle-Guignot, D.; Salje, H.; Van Kerkhove, M.D.; Abadie, V.; Garel, C.; et al. Association between Zika virus and microcephaly in French Polynesia, 2013–2015: A retrospective study. Lancet 2016, 387, 2125–2132. [Google Scholar] [CrossRef] [Green Version]
- Ferreira, H.N.C.; Schiariti, V.; Regalado, I.C.R.; Sousa, K.G.; Pereira, S.A.; Fechine, C.P.N.D.S.; Longo, E. Functioning and Disability Profile of Children with Microcephaly Associated with Congenital Zika Virus Infection. Int. J. Environ. Res. Public Health 2018, 15, 1107. [Google Scholar] [CrossRef] [Green Version]
- Nielsen-Saines, K.; Brasil, P.; Kerin, T.; Vasconcelos, Z.; Gabaglia, C.R.; Damasceno, L.; Pone, M.V.D.S.; De Carvalho, L.M.A.; Pone, S.M.; Zin, A.A.; et al. Delayed childhood neurodevelopment and neurosensory alterations in the second year of life in a prospective cohort of ZIKV-exposed children. Nat. Med. 2019, 25, 1213–1217. [Google Scholar] [CrossRef]
- Mulkey, S.B.; Arroyave-Wessel, M.; Peyton, C.; Bulas, D.I.; Fourzali, Y.; Jiang, J.; Russo, S.; McCarter, R.; Msall, M.E.; Du Plessis, A.J.; et al. Neurodevelopmental Abnormalities in Children With In Utero Zika Virus Exposure without Congenital Zika Syndrome. JAMA Pediatr. 2020, 174, 269–276. [Google Scholar] [CrossRef]
- Satterfield-Nash, A.; Kotzky, K.; Allen, J.; Bertolli, J.; Moore, C.A.; Pereira, I.O.; Pessoa, A.; Melo, F.; Santelli, A.C.F.E.S.; Boyle, C.A.; et al. Health and Development at Age 19–24 Months of 19 Children Who Were Born with Microcephaly and Laboratory Evidence of Congenital Zika Virus Infection During the 2015 Zika Virus Outbreak—Brazil, 2017. MMWR. Morb. Mortal. Wkly. Rep. 2017, 66, 1347–1351. [Google Scholar] [CrossRef] [Green Version]
- Lage, M.-L.C.; De Carvalho, A.L.; Ventura, P.A.; Taguchi, T.B.; Fernandes, A.S.; Pinho, S.F.; Santos-Junior, O.T.; Ramos, C.L.; Nascimento-Carvalho, C.M. Clinical, Neuroimaging, and Neurophysiological Findings in Children with Microcephaly Related to Congenital Zika Virus Infection. Int. J. Environ. Res. Public Health 2019, 16, 309. [Google Scholar] [CrossRef] [Green Version]
- França, G.V.A.; Schuler-Faccini, L.; Oliveira, W.K.; Henriques, C.M.P.; Carmo, E.H.; Pedi, V.D.; Nunes, M.L.; Castro, M.C.; Serruya, S.; Silveira, M.F.; et al. Congenital Zika virus syndrome in Brazil: A case series of the first 1501 livebirths with complete investigation. Lancet 2016, 388, 891–897. [Google Scholar] [CrossRef] [Green Version]
- De França, T.L.B.; Medeiros, W.R.; De Souza, N.L.; Longo, E.; Pereira, S.A.; França, T.B.D.O.; Sousa, K.G. Growth and Development of Children with Microcephaly Associated with Congenital Zika Virus Syndrome in Brazil. Int. J. Environ. Res. Public Health 2018, 15, 1990. [Google Scholar] [CrossRef] [Green Version]
- Leal, M.C.; Muniz, L.F.; Ferreira, T.S.; Santos, C.M.; Almeida, L.C.; Van Der Linden, V.; Ramos, R.C.; Rodrigues, L.C.; Neto, S.S.C. Hearing Loss in Infants with Microcephaly and Evidence of Congenital Zika Virus Infection—Brazil, November 2015–May 2016. MMWR. Morb. Mortal. Wkly. Rep. 2016, 65, 917–919. [Google Scholar] [CrossRef] [Green Version]
- Melo, A.; Gama, G.L.; Júnior, R.A.D.S.; De Assunção, P.L.; Tavares, J.S.; Da Silva, M.B.; Costa, K.N.F.S.; Vânia, M.L.; Evangelista, M.; Amorim, M. Motor function in children with congenital Zika syndrome. Dev. Med. Child Neurol. 2020, 62, 221–226. [Google Scholar] [CrossRef]
- Rice, M.E.; Galang, R.R.; Roth, N.M.; Ellington, S.R.; Moore, C.A.; Valencia-Prado, M.; Ellis, E.M.; Tufa, A.J.; Taulung, L.A.; Alfred, J.M.; et al. Vital Signs:Zika-Associated Birth Defects and Neurodevelopmental Abnormalities Possibly Associated with Congenital Zika Virus Infection—U.S. Territories and Freely Associated States, 2018. MMWR. Morb. Mortal. Wkly. Rep. 2018, 67, 858–867. [Google Scholar] [CrossRef] [Green Version]
- Einspieler, C.; Utsch, F.; Brasil, P.; Aizawa, C.Y.P.; Peyton, C.; Hasue, R.H.; Genovesi, F.F.; Damasceno, L.; Moreira, M.E.; Adachi, K.; et al. Association of Infants Exposed to Prenatal Zika Virus Infection With Their Clinical, Neurologic, and Developmental Status Evaluated via the General Movement Assessment Tool. JAMA Netw. Open 2019, 2, e187235. [Google Scholar] [CrossRef] [Green Version]
- Valdes, V.; Zorrilla, C.D.; Gabard-Durnam, L.; Muler-Mendez, N.; Rahman, Z.I.; Rivera, D.; Nelson, C.A. Cognitive Development of Infants Exposed to the Zika Virus in Puerto Rico. JAMA Netw. Open 2019, 2, e1914061. [Google Scholar] [CrossRef]
- Calle-Giraldo, J.P.; Rojas, C.A.; Hurtado, I.C.; Barco, C.; Libreros, D.; Sánchez, P.J.; López, P.; Arias, A.; Dávalos, D.M.; Lesmes, M.C.; et al. Outcomes of Congenital Zika Virus Infection During an Outbreak in Valle del Cauca, Colombia. Pediatr. Infect. Dis. J. 2019, 38, 735–740. [Google Scholar] [CrossRef]
- Cabral, J.; Faiçal, A.; Almeida, B.; Oliveira, J.; Embiruçu, E.; Ferreira, N.; Reis, L.; Salles, C.; Cabral, B.; Costa, B.; et al. Neurodevelopmental delays arising from in utero exposure to Zika virus in Salvador, Brazil. Int. J. Infect. Dis. 2018, 73, 48–49. [Google Scholar] [CrossRef]
- Hcini, N.; Kugbe, Y.; Rafalimanana, Z.H.L.; Lambert, V.; Mathieu, M.; Carles, G.; Baud, D.; Panchaud, A.; Pomar, L. Association between confirmed congenital Zika infection at birth and outcomes up to 3 years of life. Nat. Commun. 2021, 12, 3270. [Google Scholar] [CrossRef]
- Ospina, M.L.; Tong, V.T.; Gonzalez, M.; Valencia, D.; Mercado, M.; Gilboa, S.M.; Rodriguez, A.J.; Tinker, S.C.; Rico, A.; Winfield, C.M.; et al. Zika Virus Disease and Pregnancy Outcomes in Colombia. N. Engl. J. Med. 2020, 383, 537–545. [Google Scholar] [CrossRef]
- Instituto Nacional de Salud. Circular Externa 0043 de 2015; Instituto Nacional de Salud: Bogotá, Colombia, 2015; Volume 2016.
- Lanciotti, R.S.; Kosoy, O.L.; Laven, J.J.; Velez, J.O.; Lambert, A.J.; Johnson, A.J.; Stanfield, S.M.; Duffy, M.R. Genetic and Serologic Properties of Zika Virus Associated with an Epidemic, Yap State, Micronesia, 2007. Emerg. Infect. Dis. 2008, 14, 1232–1239. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Trioplex Real-Time RT-PCR Assay: For Use Under an Emergency Use Authorization only; CDC: Atlanta, GA, USA, 2017. [Google Scholar]
- Santiago, G.A.; Vázquez, J.; Courtney, S.; Matías, K.Y.; Andersen, L.E.; Colón, C.; Butler, A.E.; Roulo, R.; Bowzard, J.; Villanueva, J.M.; et al. Performance of the Trioplex real-time RT-PCR assay for detection of Zika, dengue, and chikungunya viruses. Nat. Commun. 2018, 9, 1–10. [Google Scholar] [CrossRef]
- Bhatnagar, J.; Rabeneck, D.B.; Martines, R.B.; Reagan-Steiner, S.; Ermias, Y.; Estetter, L.B.; Suzuki, T.; Ritter, J.; Keating, M.K.; Al, J.B.E.; et al. Zika Virus RNA Replication and Persistence in Brain and Placental Tissue. Emerg. Infect. Dis. 2017, 23, 405–414. [Google Scholar] [CrossRef]
- Lindsey, N.P.; Staples, J.E.; Powell, K.; Rabe, I.B.; Fischer, M.; Powers, A.M.; Kosoy, O.I.; Mossel, E.C.; Munoz-Jordan, J.L.; Beltran, M.; et al. Ability To Serologically Confirm Recent Zika Virus Infection in Areas with Varying Past Incidence of Dengue Virus Infection in the United States and U.S. Territories in 2016. J. Clin. Microbiol. 2018, 56, e01115-17. [Google Scholar] [CrossRef] [Green Version]
- Olson, S.M.; Delaney, A.; Jones, A.M.; Carr, C.P.; Liberman, R.F.; Forestieri, N.E.; Tong, V.T.; Gilboa, S.M.; Honein, M.A.; Moore, C.A.; et al. Updated baseline prevalence of birth defects potentially related to Zika virus infection. Birth Defects Res. 2019, 111, 938–940. [Google Scholar] [CrossRef] [Green Version]
- Villar, J.; Ismail, L.C.; Victora, C.G.; Ohuma, E.O.; Bertino, E.; Altman, D.G.; Lambert, A.; Papageorghiou, A.T.; Carvalho, M.; Jaffer, Y.A.; et al. International standards for newborn weight, length, and head circumference by gestational age and sex: The Newborn Cross-Sectional Study of the INTERGROWTH-21st Project. Lancet 2014, 384, 857–868. [Google Scholar] [CrossRef]
- De Onis, M.; Garza, C.; Victora, C.G.; Onyango, A.W.; Frongillo, E.A.; Martines, J. Members of the who Multicentre Growth Reference Study Group. Food Nutr. Bull. 2004, 25, S13–S14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministerio de Salud República de Colombia. Escala Abreviada de Desarrollo; Ministerio de Salud República de Colombia: Bogotá, Colombia, 1999.
- Hoen, B.; Schaub, B.; Funk, A.L.; Ardillon, V.; Boullard, M.; Cabié, A.; Callier, C.; Carles, G.; Cassadou, S.; Césaire, R.; et al. Pregnancy Outcomes after ZIKV Infection in French Territories in the Americas. N. Engl. J. Med. 2018, 378, 985–994. [Google Scholar] [CrossRef]
- Shapiro-Mendoza, C.K.; Rice, M.E.; Galang, R.R.; Fulton, A.C.; Vanmaldeghem, K.; Prado, M.V.; Ellis, E.; Anesi, M.S.; Simeone, R.M.; Petersen, E.E.; et al. Pregnancy Outcomes After Maternal Zika Virus Infection During—U.S. Territories, January 1, 2016–April 25, 2017. MMWR. Morb. Mortal. Wkly. Rep. 2017, 66, 615–621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Galang, R.R.; Avila, G.A.; Valencia, D.; Daza, M.; Tong, V.T.; Bermúdez, A.J.; Gilboa, S.M.; Rico, A.; Cates, J.; Pacheco, O.; et al. Etiology of Microcephaly and Central Nervous System Defects during the Zika Epidemic in Colombia. J. Pediatr. 2020, 222, 112–119.e3. [Google Scholar] [CrossRef] [PubMed]
- Departamento Administrativo Nacional de Estadística Nacimientos por Área de Ocurrencia y Sexo, Según Grupos de Edad de la Madre. Available online: https://www.dane.gov.co/index.php/estadisticas-por-tema/salud/nacimientos-y-defunciones/nacimientos/nacimientos-2018 (accessed on 26 June 2021).
- Moreira, M.E.L.; Nielsen-Saines, K.; Brasil, P.; Kerin, T.; Damasceno, L.; Pone, M.V.D.S.; Carvalho, L.M.; Pone, S.M.; Vasconcelos, Z.; Ribeiro, I.P.; et al. Neurodevelopment in Infants Exposed to Zika Virus In Utero. N. Engl. J. Med. 2018, 379, 2377–2379. [Google Scholar] [CrossRef]
- Faiçal, A.V.B.; De Oliveira, J.C.; Oliveira, J.V.V.; De Almeida, B.L.; Agra, I.A.; Alcantara, L.; Acosta, A.X.; De Siqueira, I.C. Neurodevelopmental delay in normocephalic children with in utero exposure to Zika virus. BMJ Paediatr. Open 2019, 3, e000486. [Google Scholar] [CrossRef] [PubMed]
- Cranston, J.S.; Tiene, S.F.; Nielsen-Saines, K.; Vasconcelos, Z.; Pone, M.V.D.S.; Pone, S.; Zin, A.; Salles, T.S.; Pereira, J.P.; Orofino, D.; et al. Association Between Antenatal Exposure to Zika Virus and Anatomical and Neurodevelopmental Abnormalities in Children. JAMA Netw. Open 2020, 3, e209303. [Google Scholar] [CrossRef]
- Stringer, E.M.; Martinez, E.; Blette, B.; Toval Ruiz, C.E.; Boivin, M.; Zepeda, O.; Stringer, J.S.; Morales, M.; Ortiz-Pujols, S.; Familiar, I.; et al. Neurodevelopmen-tal Outcomes of Children Following In Utero Exposure to Zika in Nicaragua. Clin. Infect. Dis. 2021, 72, e146–e153. [Google Scholar] [CrossRef] [PubMed]
- Familiar, I.; Boivin, M.; Magen, J.; Azcorra, J.A.; Phippen, C.; Barrett, E.A.; Miller, S.; Ruisenor-Escudero, H. Neurodevel-opment outcomes in infants born to women with Zika virus infection during pregnancy in Mexico. Child Care Health Dev. 2021, 47, 311–318. [Google Scholar] [CrossRef]
- Gerzson, L.R.; De Almeida, C.S.; Da Silva, J.H.; Feitosa, M.M.A.; De Oliveira, L.N.; Schuler-Faccini, L. Neurodevelopment of Nonmicrocephalic Children, After 18 Months of Life, Exposed Prenatally to Zika Virus. J. Child Neurol. 2019, 35, 278–282. [Google Scholar] [CrossRef]
- Sharp, T.M.; Fischer, M.; Muñoz-Jordán, J.L.; Paz-Bailey, G.; Staples, J.E.; Gregory, C.J.; Waterman, S.H. Dengue and Zika Virus Diagnostic Testing for Patients with a Clinically Compatible Illness and Risk for Infection with Both Viruses. MMWR Recomm. Rep. 2019, 68, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Haby, M.M.; Pinart, M.; Elias, V.; Reveiz, L. Prevalence of asymptomatic Zika virus infection: A systematic review. Bull. World Health Organ. 2018, 96, 402–413D. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.W.; Buekens, P.M.; Cafferata, M.L.; Gilboa, S.; Tomasso, G.; Tong, V. Measurement error, microcephaly prevalence and implications for Zika: An analysis of Uruguay perinatal data. Arch. Dis. Child. 2020, 105, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Harville, E.; Tong, V.; Gilboa, S.; Moore, C.; Cafferata, M.; Alger, J.; Gibbons, L.; Bustillo, C.; Callejas, A.; Castillo, M.; et al. Measurement of Head Circumference: Implications for Microcephaly Surveillance in Zika-Affected Areas. Trop. Med. Infect. Dis. 2020, 6, 5. [Google Scholar] [CrossRef] [PubMed]
| Total (N = 1180) n (%) | Laboratory Evidence of Zika Virus Infection (N = 254) n (%) | |
|---|---|---|
| Maternal age at conception (years) | ||
| <17 | 106 (9.0) | 28 (11.0) |
| 17–19 | 208 (17.6) | 41 (16.1) |
| 20–24 | 374 (31.7) | 76 (29.9) |
| 25–29 | 249 (21.1) | 55 (21.7) |
| 30–34 | 149 (12.6) | 34 (13.4) |
| ≥35 | 78 (6.6) | 17 (6.7) |
| Not reported | 16 (1.4) | 3 (1.2) |
| Maternal education | ||
| <Secondary | 120 (10.2) | 30 (11.8) |
| Secondary | 595 (50.4) | 114 (44.9) |
| Technical | 130 (11.0) | 27 (10.6) |
| Professional | 70 (5.9) | 14 (5.5) |
| Not reported | 265 (22.5) | 69 (27.2) |
| Gravidity | ||
| Primigravid | 323 (27.4) | 92 (36.2) |
| Multigravid | 668 (56.6) | 131 (51.6) |
| Not reported | 189 (16.0) | 31 (12.2) |
| Delivery method | ||
| Vaginal | 541 (45.9) | 136 (53.5) |
| Cesarean section | 622 (52.7) | 115 (45.3) |
| Not reported | 17 (1.4) | 3 (1.2) |
| Infant sex † | ||
| Male | 575 (48.2) | 124 (48.4) |
| Female | 602 (50.5) | 127 (49.6) |
| Not reported | 15 (1.3) | 5 (2.0) |
| Plurality | ||
| Singleton | 1150 (97.5) | 246 (96.9) |
| Twins | 12 (1.0) | 2 (0.8) |
| Not reported | 18 (1.5) | 6 (2.4) |
| Symptoms reported ‡ | ||
| Rash | 983 (83.3) | 211 (83.1) |
| Fever | 787 (66.7) | 149 (58.7) |
| Joint pain | 691 (58.6) | 148 (58.3) |
| Headache | 612 (51.9) | 110 (43.3) |
| Conjunctivitis | 267 (22.6) | 54 (21.3) |
| Eye pain | 116 (9.8) | 26 (10.2) |
| Diarrhea | 99 (8.4) | 21 (8.3) |
| Swollen lymph nodes | 22 (1.9) | 5 (2.0) |
| Not reported | 72 (6.1) | 20 (7.9) |
| Trimester of symptom onset | ||
| Periconception (up to 8 weeks before the estimated date of conception) | 84 (7.1) | 8 (3.2) |
| First trimester | 616 (52.2) | 124 (48.8) |
| Second trimester | 397 (33.6) | 104 (40.9) |
| Third trimester | 63 (5.3) | 13 (5.1) |
| Not reported | 20 (1.7) | 5 (2.0) |
| Total (N = 1180) n (%) | Laboratory Evidence of Zika Virus Infection (N = 254) n (%) | |
|---|---|---|
| Pregnancy outcome | ||
| Live birth | 1166/1180 (98.8) | 250/254 (98.4) |
| Pregnancy loss <20 weeks’ gestation | 6/1180 (0.5) | 1/254 (0.4) |
| Pregnancy loss ≥20 weeks’ gestation | 8/1180 (0.7) | 3/254 (1.2) |
| Zika-associated birth defects | ||
| Total with any Zika-associated birth defect | 50/1180 (4.2) | 22/254 (8.7) |
| Selected brain abnormalities with or without microcephaly | 29/1180 (2.5) | 14/254 (5.5) |
| Selected eye anomalies | 14/1180 (1.2) | 6/254 (2.4) |
| Microcephaly only at birth | 19/1180 (1.6) | 7/254 (2.8) |
| Postnatal-onset microcephaly | 17/1180 (1.4) | 4/254 (1.6) |
| Other adverse outcomes † | ||
| Preterm delivery ‡ | 106/1099 (9.7) | 21/226 (9.3) |
| Low birth weight ‡ | 76/1099 (6.9) | 19/226 (8.4) |
| Small for gestational age ‡ | 50/1099 (4.6) | 8/226 (3.5) |
| Death in the first year of life (among live-born infants) | 16/1178 (1.4) | 9/252 (3.6) |
| Total (N = 1160) * | Periconception (N = 84) | 1st Trimester (N = 616) | 2nd Trimester (N = 397) | 3rd Trimester (N = 63) | |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Pregnancy outcome | |||||
| Live birth | 1149/1160 (99.1) | 81/84 (96.4) | 610/616 (99.0) | 395/397 (99.5) | 63/63 (100.0) |
| Pregnancy loss <20 weeks’ gestation | 4/1160 (0.3) | 1/84 (1.2) | 3/616 (0.5) | 0/397 (0) | 0/63 (0) |
| Pregnancy loss ≥20 weeks’ gestation | 7/1160 (0.6) | 2/84 (2.4) | 3/616 (0.5) | 2/397 (0.5) | 0/63 (0) |
| Zika-associated birth defects | |||||
| Total with any Zika-associated birth defect | 49/1160 (4.2) | 4/84 (4.8) | 29/616 (4.7) | 13/397 (3.3) | 3/63 (4.8) |
| Selected brain abnormalities with or without microcephaly | 28/1160 (2.4) | 2/84 (2.4) | 19/616 (3.1)† | 4/397 (1.0)† | 3/63 (4.8) |
| Selected eye anomalies | 14/1160 (1.2) | 0/84 (0) | 11/616 (1.8) | 2/397 (0.5) | 1/63 (1.6) |
| Microcephaly only at birth | 19/1160 (1.6) | 2/84 (2.4) | 9/616 (1.5) | 8/397 (2.0) | 0/63 (0) |
| Postnatal-onset microcephaly | 17/1160 (1.5) | 3/84 (3.6) | 7/616 (1.1) | 6/397 (1.5) | 1/63 (1.6) |
| Other adverse outcomes ‡ | |||||
| Preterm delivery § | 105/1082 (9.7) | 10/75 (13.3) | 65/573 (11.3) | 26/375 (6.9) | 4/59 (6.8) |
| Low birth weight § | 75/1082 (6.9) | 10/75 (13.3) | 41/573 (7.2) | 21/375 (5.6) | 3/59 (5.1) |
| Small for gestational age § | 50/1082 (4.6) | 3/75 (4.0) | 23/573 (4.0) | 20/375 (5.3) | 4/59 (6.8) |
| Death in the first year of life (among live births) | 14/1149 (1.2) | 0/81 (0) | 10/614 (1.6) | 3/395 (0.8) | 1/63 (1.6) |
| Total (N = 990) | Laboratory Evidence of Zika Virus Infection (N = 223) | |||
|---|---|---|---|---|
| Neurodevelopmental Sequelae | Zika-Associated Birth Defects ‡ or Postnatal onset Microcephaly (N = 58) n (%) | No Zika-Associated Birth Defects (N = 932) n (%) | Zika-Associated Birth Defects or Postnatal onset Microcephaly (N = 20) n (%) | No Zika-Associated Birth Defects (N = 203) n (%) |
| Seizures | 12 (20.7) | 5 (0.5) | 4 (20.0) | 2 (1.0) |
| Tone abnormality | 19 (32.8) | 71 (7.6) | 8 (40.0) | 44 (21.7) |
| Movement abnormality | 13 (22.4) | 6 (0.6) | 4 (20.0) | 2 (1.0) |
| Swallowing abnormality | 11 (19.0) | 7 (0.8) | 3 (15.0) | 4 (2.0) |
| Arthrogryposis | 1 (1.7) | 0 (0) | 1 (5.0) | 0 (0) |
| Visual impairment | 12 (20.7) | 12 (1.3) | 6 (30.0) | 3 (1.5) |
| Hearing abnormality | 3 (5.2) | 22 (2.4) | 2 (10.0) | 3 (1.5) |
| Any neurodevelopmental sequela | 26 (44.8) | 100 (10.7) | 11 (55.0) | 51 (25.1) |
| Escala Abreviada de Desarrollo(EAD-1) § alert scores | ||||
| Gross motor domain | 18 (31.0) | 159 (17.1) | 4 (20.0) | 21 (10.3) |
| Fine motor domain | 16 (27.6) | 142 (15.2) | 4 (20.0) | 19 (9.4) |
| Personal and social domain | 14 (24.1) | 152 (16.3) | 4 (20.0) | 17 (8.4) |
| Hearing and language domain | 16 (27.6) | 151 (16.2) | 4 (20.0) | 16 (7.9) |
| Any EAD-1 alert | 20 (34.5) | 202 (21.7) | 4 (20.0) | 30 (14.8) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mercado-Reyes, M.; Gilboa, S.M.; Valencia, D.; Daza, M.; Tong, V.T.; Galang, R.R.; Winfield, C.M.; Godfred-Cato, S.; Benavides, M.; Villanueva, J.M.; et al. Pregnancy, Birth, Infant, and Early Childhood Neurodevelopmental Outcomes among a Cohort of Women with Symptoms of Zika Virus Disease during Pregnancy in Three Surveillance Sites, Project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016–2018. Trop. Med. Infect. Dis. 2021, 6, 183. https://doi.org/10.3390/tropicalmed6040183
Mercado-Reyes M, Gilboa SM, Valencia D, Daza M, Tong VT, Galang RR, Winfield CM, Godfred-Cato S, Benavides M, Villanueva JM, et al. Pregnancy, Birth, Infant, and Early Childhood Neurodevelopmental Outcomes among a Cohort of Women with Symptoms of Zika Virus Disease during Pregnancy in Three Surveillance Sites, Project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016–2018. Tropical Medicine and Infectious Disease. 2021; 6(4):183. https://doi.org/10.3390/tropicalmed6040183
Chicago/Turabian StyleMercado-Reyes, Marcela, Suzanne M. Gilboa, Diana Valencia, Marcela Daza, Van T. Tong, Romeo R. Galang, Christina M. Winfield, Shana Godfred-Cato, Mónica Benavides, Julie M. Villanueva, and et al. 2021. "Pregnancy, Birth, Infant, and Early Childhood Neurodevelopmental Outcomes among a Cohort of Women with Symptoms of Zika Virus Disease during Pregnancy in Three Surveillance Sites, Project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016–2018" Tropical Medicine and Infectious Disease 6, no. 4: 183. https://doi.org/10.3390/tropicalmed6040183
APA StyleMercado-Reyes, M., Gilboa, S. M., Valencia, D., Daza, M., Tong, V. T., Galang, R. R., Winfield, C. M., Godfred-Cato, S., Benavides, M., Villanueva, J. M., Thomas, J. D., Daniels, J., Zaki, S., Reagan-Steiner, S., Bhatnagar, J., Schiffer, J., Steward-Clark, E., Ricaldi, J. N., Osorio, J., ... Ospina Martinez, M. L. (2021). Pregnancy, Birth, Infant, and Early Childhood Neurodevelopmental Outcomes among a Cohort of Women with Symptoms of Zika Virus Disease during Pregnancy in Three Surveillance Sites, Project Vigilancia de Embarazadas con Zika (VEZ), Colombia, 2016–2018. Tropical Medicine and Infectious Disease, 6(4), 183. https://doi.org/10.3390/tropicalmed6040183






