Issues and Controversies in the Evolution of Oral Rehydration Therapy (ORT)
Abstract
1. Introduction
2. Basic Principles of Oral Therapy Methodology
3. Home Therapy with the WHO 90 ORS Using the 2:1 Regimen
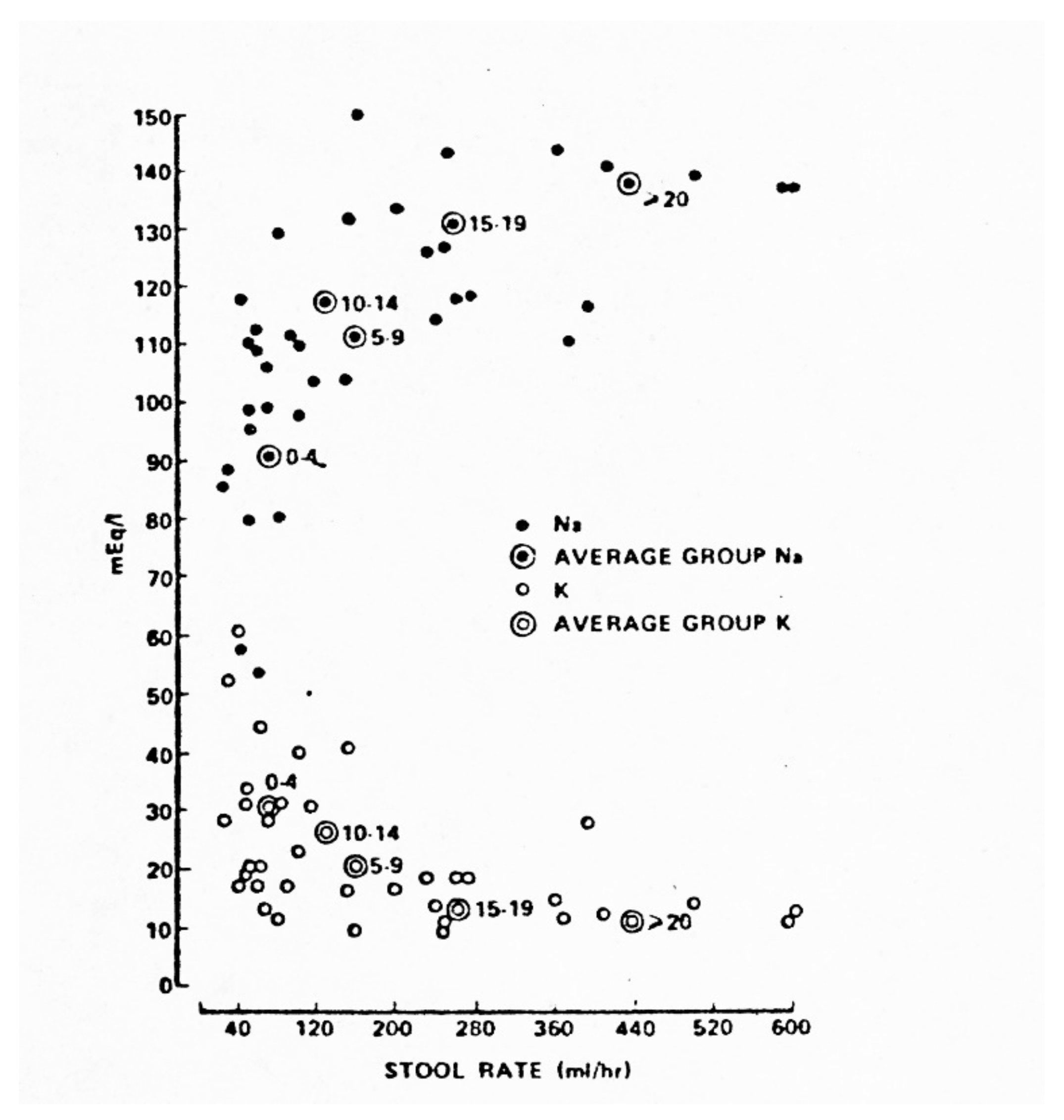
4. The Evolution of ORT and ORS
5. Major Differences in Pathophysiology of Cholera and Non-Cholera AWDs
6. Limitations of Existing Studies
7. Discussion
8. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
Abbreviations
| AWD | Acute Watery Diarhhea |
| ORS | Oral Rehydratation Solution |
| ORT | Oral Rehydratation Therapy |
| ORS75 | ORS with 75 mEq/L Sodium (Na+) |
| ORS90 | ORS With 90 mEq/L Sodium (Na+) |
| ORS120 | ORS With 120 mEq/L Sodium (Na+) |
| GDR | Gross Diarrhea Rate, ml/hr |
| NGB | Net Gut Balance (oral intake) − (stool+vomitus) in Liters |
| PNGB | Positive Net Gut Balance |
| CHOLERA | AWD Caused by Vibrio cholerae |
| ETEC | Enterotoxigenic Escherichia coli |
| NONVIBRIO CHOLERA | Severe AWD Due to ETEC or Bacteria with Cholera Toxin Analogs |
References
- WHO. Reduced Osmolarity Oral Rehydration Salts (ORS) Formulation; Department of Child and Adolescent Health and Development. Available online: https://apps.who.int/iris/handle/10665/67322 (accessed on 20 October 2020).
- Musekiwa, A.; Volmink, J.; Cochrane Infectious Diseases Group. Oral Rehydration Salt Solution for Treating Cholera: ≤270 mOs/L solutions vs. ≤310 mOsm/L Solutions. Cochrane Database Syst. Rev. 2011, 2011, CD003754. [Google Scholar] [CrossRef]
- CHOICE Study Group. Multicenter, randomized, double-blind clinical trial to evaluate the efficacy and safety of a reduced osmolarity oral rehydration salts solution in children with acute watery diarrhea. Pediatrics 2001, 107, 613–618. [Google Scholar] [CrossRef]
- Alam, S.; Afzal, K.; Maheshwari, M.; Shukla, I. Controlled trial of hypo-osmolar versus world Health Organization Oral rehydration solution. Indian Pediatrics 2000, 37, 952–960. [Google Scholar]
- Pulungsih, S.P.; Punjabi, N.H.; Rafli, K.; Rifajati, A.; Kumala, S.; Simanjuntak, C.H.; Yuwono Lesmana, M.; Subekti, D.; Sutoto; Fontaine, O. Standard WHO_ORS versus reduced-osmolarity ORS in the management of cholera patients. J. Health Popul. Nutr. 2006, 24, 107–112. [Google Scholar]
- Alam, N.H.; Majumder, R.N.; Fuchs, G.J.; The CHOICE study group. Efficacy and safety of oral rehydration solution with reduced osmolarity in adults with cholera: A randomized double-blind clinical trial. Lancet 1999, 354, 296–299. [Google Scholar] [CrossRef]
- Faruque, A.S.G.; Mahalanabis, D.; Hamadani, J.D.; Zetterstrom, R. Reduced osmolarity oral rehydration salt in cholera. Scan. J. Infect Dis. 1996, 28, 87–90. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharya, M.K.; Bhattacharya, S.K.; Dutta, D.; Deb, A.K.; Deb, M.; Dutta, A.; Saha, C.A.; Nair, G.B.; Mahalanabis, D. Efficacy of oral hyposmolar glucose-based and rice-based oral rehydration salt solutions in the treatment of cholera in adults. Scan. J. Gastroent. 1998, 33, 159–163. [Google Scholar] [CrossRef]
- Dutta, M.K.; Bhattacharya, M.K.; Deb, A.K.; Sarkar, A.; Chatterjee, A.; Biswas, A.B.; Chatterjee, K.; Nair, G.B.; Bhattacharya, S.K. Evaluation of oral hypo-osmolar glucose-based and rice-based oral rehydration solutions in the treatment of cholera in children. Acta Paediatr. 2000, 89, 787–790. [Google Scholar] [CrossRef]
- Alam, N.H.; Yunus, M.; Faruque, A.S.G.; Gyr, N.; Sattar, S.; Parvin, S.; Ahmed, J.U.; Salam, M.A.; Sack, D.A. Symptomatic hyponatremia during treatment of dehydrating diarrheal disease with reduced osmolarity oral rehydration solution. JAMA 2006, 296, 567–573. [Google Scholar] [CrossRef]
- Phillips, R.A. Asiatic cholera. Ann. Rev. Med. 1968, 19, 69–79. [Google Scholar] [CrossRef]
- Nalin, D.R. Oral therapy for diarrheal diseases. J. Diarrheal Dis. Res. 1987, 5, 283–292. [Google Scholar]
- Hirschhorn, N.; Kinzie, J.I.; Sachar, D.B.; Northrup, R.S.; Taylor, J.O.; Ahmad, S.Z.; Philllips, R.A. Decrease in net stool output in cholera during intestinal perfusion with glucose-containing solutions. NEJM 1968, 279, 176–181. [Google Scholar] [CrossRef]
- Nalin, D.R.; Levine, M.M.; Hornick, R.; Bergquist, E.; Hoover, D.; Holley, H.P.; Waterman, D.; Van Blerk, J.; Matheny, S.; Sotman, S.; et al. The problem of emesis during oral glucose-electrolytes therapy given from the onset of severe cholera. Trans. Roy. Soc. Trop. Med. Hyg. 1979, 73, 10–14. [Google Scholar] [CrossRef]
- Cash, R.A.; Nalin, D.R.; Toaha, K.M.M.; Huq, Z. Acetate in the correction of acidosis secondary to diarrhea. Lancet 1969, 294, 302–303. [Google Scholar] [CrossRef]
- Harvey, R.M.; Enson, Y.; Lewis, M.L.; Greenough, W.B.; Ally, K.; Panno, R.A. Hemodynamic studies on cholera, Effects of hypovolemia and acidosis. Circulation 1968, 37, 709–728. [Google Scholar] [CrossRef]
- Nalin, D.R.; Cash, R.A.; Islam, R.; Molla, M.; Phillips, R.A. Oral maintenance therapy for cholera in adults. Lancet 1968, 292, 370–373. [Google Scholar] [CrossRef]
- El-Mougi, M.; Hendaw, A.; Koura, H.; Hegazi, E.; Fontain, O.; Pierce, N.F. Efficacy of standard glucose-based and reduced-osmolarity maltodextrin-based oral rehyration solutions: Effect of sugar malabsorption. Bull. WHO 1996, 74, 471–477. [Google Scholar]
- Lifschitz, F.; Coello-Ramirez, P.; Gutierrez, L.L.C. Monosaccharide intolerance and hypoglycemia in infants with diarrh74, 471-477.ea: Metabolic studies in 23 infants. J. Peds 1970, 77, 604–612. [Google Scholar] [CrossRef]
- Hirschhorn, N.; Nalin, D.R.; Cash, R.A. CHOICE Study Group Trial. Pediatrics 2002, 109, 713–715. [Google Scholar] [CrossRef]
- Saniel, M.C.; Zimicki, S.; Carlos, C.C.; Maria, A.C.S.; Balis, A.C.; Malacad, C. J. Diarrhoeal Dis. Res. 1997, 15, 47–52.
- Isolauri, E. Evaluation of an oral rehydration solution with Na+ 60 mmol/L. in infants hospitalized for acute diarrhea or treated as outpatients. Acta Paediatr. Scand 1985, 74, 643–649. [Google Scholar] [CrossRef]
- Nalin, D.R.; Levine, M.M.; Mata, L.; de Cespedes, C.; Vargas, W.; Lizano, C.; Loria, A.R.; Simhon, A.; Mohs, E. Oral rehydration and maintenance of children with rotavirus and bacterial diarrheas. Bull. WHO 1979, 57, 453–459. [Google Scholar]
- Snyder, J.D.; Merson, M.H. The magnitude of the problem of acute diarrheal disease: A review of active surveillance data. Bull. WHO 1982, 60, 506–513. [Google Scholar]
- GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional and national morbidity, mortality and aetiologies of diarrhea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 18, 1211–1228. [Google Scholar] [CrossRef]
- Ruxin, J. Magic Bullet: The history of oral rehydration therapy. Med. Hist. 1994, 38, 363–397. [Google Scholar] [CrossRef] [PubMed]
- Cash, R.A.; Nalin, D.R.; Forrest, J.; Abrutyn, E. Rapid correction of the acidosis and dehydration of cholera with an oral solution. Lancet 1970, 296, 549–550. [Google Scholar] [CrossRef]
- Nalin, D.R.; Cash, R.A. Oral or nasogastric maintenance therapy for diarrheas of unknown etiology resembling cholera. Trans. Roy. Soc. Trop. Med. Hyg. 1970, 64, 769–771. [Google Scholar] [CrossRef]
- Greenough, W.B.; Gordon, R.S., Jr.; Rosenberg, I.S.; David, B.I.; Benenson, A.H. Tetracycline in the treatment of cholera. Lancet 1964, 1, 335–337. [Google Scholar] [CrossRef]
- Cash, R.A.; Nalin, D.R.; Rochat, R.; Reller, B.; Haque, E.; Rahman, M. A clinical trial of oral therapy in a rural cholera treatment center. Am. J. Trop. Med. Hyg. 1970, 19, 653–656. [Google Scholar] [CrossRef]
- Nalin, D.R.; Cash, R.A. Sodium content in oral therapy for diarrhea. Lancet 1976, 2, 957. [Google Scholar] [CrossRef]
- Pierce, N.F.; Banwell, J.G.; Mitra, R.C.; Caranasos, G.J.; Keimowitz, R.I.; Mondal, A.; Manji, P.M. Effect of intragastric glucose-electrolyte infusion upon water and electrolyte balance in Asiatic cholera. Gastroenterology 1968, 55, 333–344. [Google Scholar] [CrossRef]
- Nalin, D.R. Oral Cholera Therapy. Ann. Intern. Med. 1970, 72, 288–289. [Google Scholar] [CrossRef]
- Molla, A.M.; Ahmed, S.M.; Greenough, W.B., III. Rice-based oral rehydration solution decreases the stool volume in acute diarrhea. Bull. WHO 1985, 63, 751–756. [Google Scholar]
- Roy, S.K.; Rabbani, G.H.; Black, R.E. Oral rehydration solution safely used in breast-fed children without additional water. J. Trop. Med. Hyg. 1984, 87, 11–13. [Google Scholar] [PubMed]
- Nalin, D.R.; Levine, M.M.; Mata, L.; de Cespedes, C.; Vargas, W.; Lizano, C.; Loria, A.R.; Simhon, A.; Mohs, E. Comparison of sucrose with glucose in oral therapy of infant diarrheas. Lancet 1978, 312, 277–279. [Google Scholar] [CrossRef]
- Pizarro, D.; Possada, G.; Villavicencio, N.; Mohs, E.; Levine, M.M. Hypernatremic and hyponatremic diarrheal dehydration. Treatment with oral glucose-electrolyte solution. Am. J. Dis. Child. 1983, 137, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Nalin, D.R.; Harland, E.; Ramlal, A.; Swaby, D.; McDonald, J.; Gangarosa, R.; Levine, M.; Akierman, A.; Antonine, M.; Mackenzie, K.; et al. Comparison of low and high sodium and potassium content in oral rehydration solutions. J. Pediatr. 1980, 97, 848–853. [Google Scholar] [CrossRef]
- Clancy, B.M.; Czech, M.P. Hexose transport stimulation and membrane redistribution of glucose transporter isoforms in response to cholera toxin, dibutyryl cyclic AMP and insulin in3T3-L1 adipocytes. J. Biol. Chem. 1990, 265, 12434–12443. [Google Scholar] [CrossRef]
- Nath, S.K.; Rautureau, M.; Heyman, H. Emergence of Na+-glucose cotransport in an epithelial secretory cell line sensitive to cholera toxin. Am. J. Physiol. 1989, 1069, G335–G341. [Google Scholar] [CrossRef]
- Moule, S.K.; Bradford, N.M.; McGivan, J.D. Short-term stimulation of Na+-dependent amino acid transport by dibutryl cyclic AMP in hepatocytes. Characteristics and partial mechanism. Biochem. J. 1987, 241, 737–743. [Google Scholar] [CrossRef]
- Tai, Y.H.; Perez, E.; Desjeux, J.F. Cholera toxin and cyclic AMP stimulate D-glucose absorption in rat ileum. In Ion Gradient-Coupled Transport; Alverado, F., Van Os, C.H., Eds.; Elsevier: Amsterdam, The Netherlands, 1986; pp. 403–406. [Google Scholar]
- Wright Em Hirsh, J.R.; Loo, D.D.; Zampighi, G.A. Regulation of Na+/glucose cotransporters. J. Exp. Biol. 1997, 200, 287–293. [Google Scholar]
- Flach, C.F.; Lange, S.; Jennische, E.; Lonnroth, I. Cholera toxin induces expression of ion channels and carriers in small intestinal mucosea. FEBS Lett. 2004, 561, 122–126. [Google Scholar] [CrossRef]
- Schiller, L.E.; Santa Ana, C.; Porter, J.; Fortran, J.S. Glucose-stimulated sodium transport by the human intestine during experimental cholera. Gastroenterology 1997, 112, 1529–1535. [Google Scholar] [CrossRef]
- Nalin, D.R.; Cash, R.A.; Rahaman, M.; Yunus, M. Effect of glycine and glucose on sodium and water absorption in patients with cholera. Gut 1970, 11, 768–772. [Google Scholar] [CrossRef] [PubMed]
- Patra, F.C.; Mahalanabis, D.; Jalan, K.N.; Sen, A.; Banerjee, P. In search of a super solution:controlled trial of glycine-glucose oral rehydration solution in infantile diarrhea? Acta Pediatr. Scand 1984, 73, 18. [Google Scholar] [CrossRef] [PubMed]
- Patra, F.C.; Sack, D.A.; Islam, A.; Alam, A.N.; Mazumder, R.N. Oral rehydration formula containing alanine and glucose for treatment of diarrhea: A controlled trial. BMJ 1989, 298, 1353–1356. [Google Scholar] [CrossRef] [PubMed]
- Punjabi, N.H.; Kumala, S.; Rasidi, C.; Witham, N.D.; Pulungsih, S.P.; Rivai, A.R.; Sukri, N.; Burr, D.H.; Lesmana, M. Improving the ORS: Does glutamine have a role? Am. J. Trop. Med. Hyg. 1991, 45, 114–115. [Google Scholar]
- Amankwah, E.N.; Adu, E.; Barimah, V.M.J.; Van Twisk, C. Amino acid profiles of some varieties of rice, soybean and groundnut grown in Ghana. J. Food Process. Technol. 2015, 6, 420–423. [Google Scholar]
- Vesikari, T.; Isolauri, E. Glycine supplemented oral rehydration solutions for diarrhea. Arch. Dis. Child. 1986, 61, 372–376. [Google Scholar] [CrossRef]
- Pizarro, D.; Levine, M.M.; Posada, G.; Sandi, L. Comparison of glucose/electrolyte and glucose/glycine/electrolyte oral rehydration solutions in hospitalized children with diarrhea in Costa Rica. J. Pediatr. Gastroenterol. Nutr. 1988, 7, 411–416. [Google Scholar] [CrossRef]
- Ribiero, H.D.C., Jr.; Lifshitz, F. Alanine-based oral rehydration therapy for infants with acute diarrhea. J. Pediatr. 1991, 118, S86–S90. [Google Scholar]
- Gutierrez, C.; Villa, S.; Mota, F.R.; Calva, J.J. Does an L-glutamine-containing, glucose–free, oral rehydration solution reduce stool output and time to rehydrate in children with acute diarrhea? A double-blind randomized clinical trial. J. Health Popul. Nutr. 2007, 3, 278–284. [Google Scholar]
- Gore, S.M.; Fontaine, O.; Pierce, N. Impact of rice based oral rehydration solution on stool output and duration of diarrhea:meta-analysis of 13 clinical trials. BMJ 1992, 304, 28791. [Google Scholar] [CrossRef] [PubMed]
- Mahalanabis, D.; Faruque, A.G.; Hoque, S.S.; Faruque, S.M. Hypotonic oral rehydration solution in acute diarrhea: A controlled clinical trial. Acta Pediatr. 1995, 84, 289–293. [Google Scholar] [CrossRef] [PubMed]
- Davidson, G.P.; Barnes, G.L. Structural and functional abnormalities of the small intestine in infants and young children with rotavirus enteritis. Acta Paediatr. 1979, 68, 181–186. [Google Scholar] [CrossRef]
- Navarro, H.; Arruebo, M.P.; Alcalde, A.I.; Sorribas, V. Effect of erythromycin on D-galactose absorption and sucrose activity in rabbit jejunum. Can. J. Physiol. Pharmacol. 1993, 71, 191–194. [Google Scholar] [CrossRef] [PubMed]
- Rhoads, J.M.; MacLeod, R.J.; Hamilton, J.R. Diminished brush border membrane sodium-dependent L-alanine transport in acute viral enteritis in piglets. J. Pediatr. Gastroenterol. Nutr. 1989, 9, 225–231. [Google Scholar] [CrossRef]
- Nalin, D.R.; Ally, K.; Hare, K.; Hare, R. Effects of cholera enterotoxin on jejunal osmoregulation of mannitol solutions in dogs. J. Infect. Dis. 1972, 125, 528–532. [Google Scholar]
- Gray, G.M.; Ingelfinger, F.J. Intestinal absorption of sucrose in man: The site of hydrolysis and absorption. JCI 1965, 44, 399098. [Google Scholar] [CrossRef]
- Mathews, C.J.; MacLeod, R.J.; Zheng, S.X.; Hanrahan, J.W.; Bennett, H.P.; Hamilton, J.R. Characterization of the inhibitory effect of boiled rice on intestinal chloride secretion in guinea pig crypt cells. Gastroenterology 1999, 116, 1342–1347. [Google Scholar] [CrossRef]
- Macleod, R.; Bennett, H.; Hamilton, J. inhibition of intestinal secretion by rice. Lancet 1995, 346, 90–92. [Google Scholar] [CrossRef]
- Alam, V.A.; Ahmed, T.; Khatum; Molla, A.M. Effect of food with two or four rehydration therapies: A randomized controlled clinical trial. Gut 1992, 33, 560–562. [Google Scholar]
- Santosham, M.; Fyad, I.; Hashem, M.; Goepp, J.G.; Refaf, M.; Sack, B. A comparison of rice-based oral rehydration solute and early feeding for the treatment of acute diarrhea in infants. J. Pediatr. 1990, 116, 868–875. [Google Scholar] [CrossRef]
- Clarke, A.M.; Miller, M.; Shields, R. Intestinal transport of sodium, potassium and water in the dog during sodium depletion. Gastroenteritis 1967, 52, 846–858. [Google Scholar] [CrossRef]
- Houston, K.A.; Gibb, J.G.; Maitland, K. Oral rehydration of malnourished children with diarrhea: A systematic review (version 3). Wellcome Open Res. 2017, 2, 66. [Google Scholar] [CrossRef] [PubMed]
- Arieff, A.I.; Ayus, J.C.; Fraser, C.I. Hyponatremia and death or permanent brain damage in healthy children. BMV 1992, 304, 1218–1222. [Google Scholar]
- Rondon-Berrios, H.; Berl, T. Mild chronic hyponatremia in the ambulatory setting: Significance and management. Clin. J. Am. Soc. Nephrol. 2015, 10, 2268–2278. [Google Scholar] [CrossRef] [PubMed]
- Shahrin, L.; Chistri, M.J.; Huq, S.; Nishath, T.; Christy, M.D.; Hannan, A.; Ahmed, T. Clinical manifestations of hyponatremia and hypernatremia in under-five diarrheal children in a diarrhea hospital. J. Trop. Pediatr. 2016, 62, 206–212. [Google Scholar] [CrossRef]
- Khan, W.A.; Dhar, U.; Salam, M.A.; Griffiths, J.K.; Rand, W.; Bennish, M.L. Central nervous system manifestations of childhood shigellosis: Prevalence, risk factors and outcome. Pediatrics 1999, 103, E18. [Google Scholar] [CrossRef] [PubMed]
- Mitra, A.K.; Khan, M.R.; Alam, A.N. Complications and outcome of disease in patients admitted to the intensive care unit of a diarrhoeal diseases hospital in Bangladesh. Trans. Roy. Soc. Trop. Med. Hyg. 1991, 85, 685–687. [Google Scholar] [CrossRef]
- Chisti, M.J.; Pietroni, M.A.; Smith, J.H.; Bardhan, P.K.; Salam, M.A. Predictors of death in under-five chidren with diarrhea admitted to a critical care ward in an urban hospital in Bangladesh. Acta Paediatr. 2011, 100, e275–e279. [Google Scholar] [CrossRef] [PubMed]
- Samadi, A.R.; Wahed, M.A.; Islam, M.R.; Ahmed, S.M. Consequences of hyponatraemia and hypernatraemia in children with acute diarrhea in Bangladesh. BMJ Clin. Res. Ed. 1983, 286, 671–673. [Google Scholar] [CrossRef]
- Sazawal, S.; Black, R.E.; Bhan, M.K.; Bhandari, N.; Sinha, A.; Jalla, S. Zinc supplementation in young children with acute diarrhea in India. NEJM 1995, 333, 839–844. [Google Scholar] [CrossRef] [PubMed]
- Phillips, R.A. Cholera in the perspective of 1966. Ann. Int. Med. 1966, 65, 922–930. [Google Scholar] [CrossRef] [PubMed]
- Available online: www.alibaba.com/amino-acid-glycine-price (accessed on 18 December 2020).
- Available online: www.alibaba.com/glucosepowder (accessed on 18 December 2020).
- Khin-Maung-U; Bolin, T.D.; Duncombe, V.M.; Myo-Khin; Nyunt-Nyunt-Wai; Pereira, S.P.; Linklater, J.M. Epidemiology of small bowel bacterial overgrowth and rice carbohydrate malabsorption in Burmese (Myanmar) village children. Am. J. Trop. Med. Hyg. 1992, 47, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Khinmaungu; Nyuntnyuntwai; Myokhin; Mumukhin; Tinu; Thanetoe. Effect of boiled-rice feeding in childhood cholera on clinical outcome. Hum. Nutr. Clin. Nutr. 1986, 40, 249–254. [Google Scholar]
- Fontaine, O.; Gore, S.M.; Pierce, N.F. Rice-based oral rehydration solution for treating diarrhea. Cochrane Database Syst. Rev. 1998, CD001264. [Google Scholar] [CrossRef]
- Eldridge, D.; Ledoux, M. Needs more salt: Old hydration habits are hard to break. Lancet 2014, 385, 1159–1160. [Google Scholar] [CrossRef]
- Duke, T.; Molyneux, E.M. Intravenous fluids for seriously ill children: Time to reconsider. Lancet 2003, 362, 1320–1323. [Google Scholar] [CrossRef]
- McNab, S.; Duke, T.; South, M.; Babl, F.E.; Lee, K.j.; Arnup, S.J.; Young, S.; Turner, H.; Davidson, A. 140 mmol/L of sodium versus 77 mmol/L. of sodium in maintenance intravenous fluid therapy for children in hospital (PIMS): A randomized controlled double-blind trial. Lancet 2015, 385, 1190–1197. [Google Scholar] [CrossRef]
- Friedman, J.N.; Beck, C.E.; DeGroot, J.; Geary, D.F.; Sklansky, D.J.; Freedman, S.B. Comparison of isotonic and hypotonic intravenous maintenance fluids: A randomized clinical trial. JAMA Pediatr. 2015, 169, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Bhattachariya, S.K.; Dutta, P.; Dutta, D.; Chakraborti, M.K. Super ORS. Indian J. Public Health 1990, 34, 35–37. [Google Scholar]
- Nalin, D.R. A spoonful of sugar. Lancet 1978, 2, 264. [Google Scholar] [CrossRef]
- Nalin, D.R.; Cash, R.A. Oral or nasogastric maintenance for cholera patients in all age groups. Bull. WHO 1970, 43, 361–363. [Google Scholar]







| Na+ Losses in Cholera Patient Given (ORS75 vs. ORS90) | ||
|---|---|---|
| ADULTS | CHILDREN | |
| Stool Na+ (mEq/L) | 140 | 101 |
| ORS Na+ | 75 vs. 90 | 75 vs. 90 |
| Na+ Loss | −65 vs. −50 | −26 vs. −10 |
| Stool Vol. (L) | 25 | 8 |
| Total Na+ loss (mEq) * | −1625 vs. −1250 | −208 vs. −80 |
| Recommended Safety Studies of 75 ORS in Cholera Patients | |
|---|---|
| STUDIES | PURPOSE |
| Na+ Balance | Determine size of Na+ deficite |
| Clinical Sequelae | R/O acute sequelae using standard tests |
| Follow-up Studies | R/O developmental deficits and excess post-convalescent mortality |
| ORS Suitable for Cholera Patients | |
|---|---|
| Dissolve 4 Packets of 90 ORS in 3 L Water | Resulting ORS Concentrations |
| Na+ 120 * | |
| K+ 27 * | |
| Cl− 107 * | |
| Citrate 13@ | |
| Glucose 147@ | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nalin, D. Issues and Controversies in the Evolution of Oral Rehydration Therapy (ORT). Trop. Med. Infect. Dis. 2021, 6, 34. https://doi.org/10.3390/tropicalmed6010034
Nalin D. Issues and Controversies in the Evolution of Oral Rehydration Therapy (ORT). Tropical Medicine and Infectious Disease. 2021; 6(1):34. https://doi.org/10.3390/tropicalmed6010034
Chicago/Turabian StyleNalin, David. 2021. "Issues and Controversies in the Evolution of Oral Rehydration Therapy (ORT)" Tropical Medicine and Infectious Disease 6, no. 1: 34. https://doi.org/10.3390/tropicalmed6010034
APA StyleNalin, D. (2021). Issues and Controversies in the Evolution of Oral Rehydration Therapy (ORT). Tropical Medicine and Infectious Disease, 6(1), 34. https://doi.org/10.3390/tropicalmed6010034





