Developing Feasible, Locally Appropriate Socioeconomic Support for TB-Affected Households in Nepal
Abstract
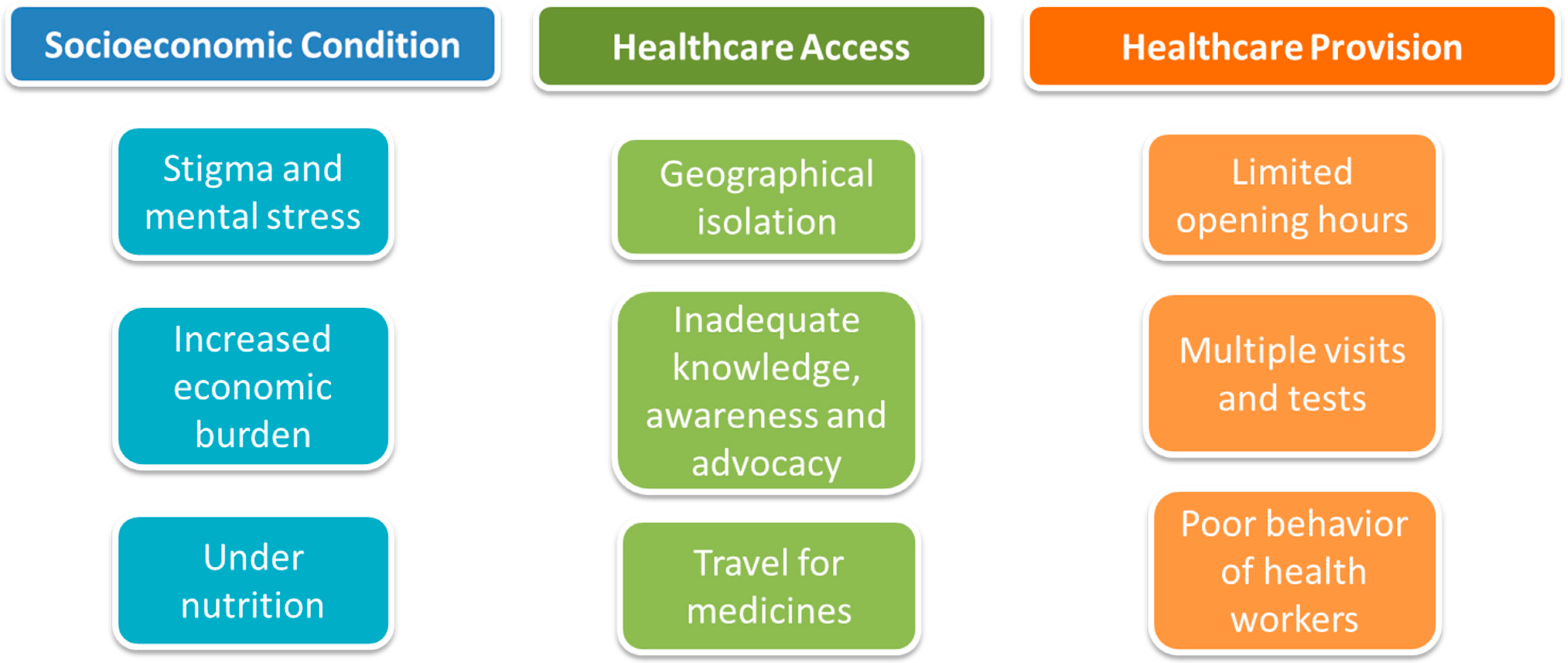
1. Introduction
2. Workshop Overview
2.1. A Review of the Existing Evidence on Socioconomic Support for TB-Affected People
2.2. Ongoing Studies Addressing the Socioeconomic Impact of TB in Nepal
2.3. Section 1 of the Workshop
2.4. Section 2 of the Workshop
(ii) Targeting of the intervention and potential funding sources
(iii) Designing and voting on the most suitable interventions for evaluation in a trial
3. Recommendations and Conclusions
- 1.
- Psychosocial support: Psychosocial counseling should be incorporated into existing NTP activities to improve mental health of all people with TB. Counseling by health workers or community volunteers at the point of TB care, OPD visits in public and private health facilities, and/or during community-based DOT and household visits, could support people with TB to cope with the psychological impact of the disease, and potentially improve TB treatment adherence and outcomes. A more detailed evaluation and assessment of mental health of people with TB is required.
- 2.
- Economic support: To reduce the financial burden of TB, the current cash transfer amount for people with DR-TB should be increased and this economic support extended to people with DS-TB, especially the most vulnerable (e.g., the most impoverished, unemployed). It was also recommended that additional budget be provided to healthcare centers to subsidize provision of medication to treat people experiencing adverse effects of TB medication or requiring related ancillary services. A national TB Patient Costs Survey would provide more accurate estimates of out-of-pocket and lost income costs incurred during TB treatment, which would support related policy translation.
- 3.
- Social protection: Coverage of social protection packages should be expanded to other vulnerable populations that are defined by national social health insurance program to reduce the likelihood of developing TB disease.
- 4.
- Nutritional support: There is a need for nutritional support not only for people with MDR-TB but also for people with DS-TB. This recommendation was seen to align with the evidence presented during the workshop that people with TB, regardless of drug-resistant status, experienced high levels of food insecurity.
- 5.
- Education and public-private mix (PPM): A PPM approach is vital to avoid the unnecessary expenditure incurred at private health care visits for diagnostic and treatment services that are free in the public healthcare system. Educational campaigns to inform communities about TB signs, symptoms, and free NTP TB diagnostic and treatment services would complement this approach. A PPM strategy has recently been approved by the Ministry of Health and Population in June 2019 and will be crucial to make TB diagnosis and treatment affordable.
Supplementary Materials
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organisation Global Tuberculosis Report 2019; World Health Organization: Geneva, Switzerland, 2019.
- Van Helden, P.D. The economic divide and tuberculosis. Tuberculosis is not just a medical problem, but also a problem of social inequality and poverty. EMBO Rep. 2003, 4, S24–S28. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Tovar, M.A.; Datta, S.; Saunders, M.J.; Evans, C. Addressing social determinants to end tuberculosis. Lancet 2018, 391, 1129–1132. [Google Scholar] [CrossRef]
- Wingfield, T.; Tovar, M.A.; Huff, D.; Boccia, D.; Saunders, M.J.; Datta, S.; Montoya, R.; Ramos, E.; Lewis, J.J.; Gilman, R.H.; et al. Beyond pills and tests: Addressing the social determinants of tuberculosis. Clin. Med. 2016, 16, s79–s91. [Google Scholar] [CrossRef] [PubMed]
- Fields, G.S. Data for measuring poverty and inequality changes in the developing countries. J. Dev. Econ. 1994, 44, 87–102. [Google Scholar] [CrossRef]
- Lönnroth, K.; Jaramillo, E.; Williams, B.; Dye, C.; Raviglione, M. Drivers of tuberculosis epidemics: The role of risk factors and social determinants. Soc. Sci. Med. 2009, 68, 2240–2246. [Google Scholar] [CrossRef] [PubMed]
- Raviglione, M.; Krech, R. Tuberculosis: Still a social disease. Int. J. Tuberc. Lung Dis. 2011, 15 (Suppl. 2), S6–S8. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Boccia, D.; Tovar, M.; Gavino, A.; Zevallos, K.; Montoya, R.; Evans, C.A. Defining Catastrophic Costs and Comparing Their Importance for Adverse Tuberculosis Outcome with Multi-Drug Resistance: A Prospective Cohort Study, Peru. PLoS Med. 2014, 11, e1001675. [Google Scholar] [CrossRef] [PubMed]
- Reeves, A.; Basu, S.; McKee, M.; Stuckler, D.; Sandgren, A.; Semenza, J. Social protection and tuberculosis control in 21 European countries, 1995–2012: A cross-national statistical modelling analysis. Lancet Infect. Dis. 2014, 14, 1105–1112. [Google Scholar] [CrossRef]
- Siroka, A.; Ponce, N.A.; Lönnroth, K. Association between spending on social protection and tuberculosis burden: A global analysis. Lancet Infect. Dis. 2016, 473–479. [Google Scholar] [CrossRef]
- De Vries, S.G.; Cremers, A.L.; Heuvelings, C.C.; Greve, P.F.; Visser, B.J.; Belard, S.; Janssen, S.; Spijker, R.; Shaw, B.; Hill, R.A.; et al. Barriers and facilitators to the uptake of tuberculosis diagnostic and treatment services by hard-to-reach populations in countries of low and medium tuberculosis incidence: A systematic review of qualitative literature. Lancet Infect. Dis. 2017, 17, e128–e143. [Google Scholar] [CrossRef]
- Tanimura, T.; Jaramillo, E.; Weil, D.; Raviglione, M.; Lönnroth, K. Financial burden for tuberculosis patients in low- And middle-income countries: A systematic review. Eur. Respir. J. 2014, 43, 1763–1775. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Tovar, M.A.; Huff, D.; Boccia, D.; Montoya, R.; Ramos, E.; Lewis, J.J.; Gilman, R.H.; Evans, C.A. The economic effects of supporting tuberculosis-affected households in Peru. Eur. Respir. J. 2016, 48, 1396–1410. [Google Scholar] [CrossRef] [PubMed]
- Saunders, M.J.; Wingfield, T.; Tovar, M.A.; Baldwin, M.R.; Datta, S.; Zevallos, K.; Montoya, R.; Valencia, T.R.; Friedland, J.S.; Moulton, L.H.; et al. A score to predict and stratify risk of tuberculosis in adult contacts of tuberculosis index cases: A prospective derivation and external validation cohort study. Lancet Infect. Dis. 2017, 17, 1190–1199. [Google Scholar] [CrossRef]
- Laurence, Y.V.; Griffiths, U.K.; Vassal, A. Costs to Health Services and the Patient of Treating Tuberculosis: A Systematic Literature Review. Pharmacoeconomics 2015, 33, 939–955. [Google Scholar] [CrossRef] [PubMed]
- Foster, N.; Vassall, A.; Cleary, S.; Cunnama, L.; Churchyard, G.; Sinanovic, E. The economic burden of TB diagnosis and treatment in South Africa. Soc. Sci. Med. 2015, 130, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Fullman, N.; Barber, R.M.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Allah, F.A.; Abdulkader, R.S.; Abdulle, A.M.; Abera, S.F.; et al. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: An analysis from the Global Burden of Disease Study 2016. Lancet 2017, 390, 1423–1459. [Google Scholar] [CrossRef]
- The End TB Strategy; World Health Organisation: Geneva, Switzerland, 2015.
- Viney, K.; Islam, T.; Hoa, N.B.; Morishita, F.; Lönnroth, K. The Financial Burden of Tuberculosis for Patients in the Western-Pacific Region. Trop. Med. Infect. Dis. 2019, 4, 94. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization. R202—Social Protection Floors Recommendation, 2012 (No. 202). Available online: https://www.ilo.org/dyn/normlex/en/f?p=NORMLEXPUB:12100:0::NO::P12100_ILO_CODE:R202 (accessed on 20 October 2019).
- Boccia, D.; Hargreaves, J.; Lönnroth, K.; Jaramillo, E.; Weiss, J.; Uplekar, M.; Porter, J.D.H.; Evans, C.A. Cash transfer and microfinance interventions for tuberculosis control: Review of the impact evidence and policy implications. Int. J. Tuberc. Lung Dis. 2011, 15, 1–21. [Google Scholar] [CrossRef]
- Rocha, C.; Montoya, R.; Zevallos, K.; Curatola, A.; Ynga, W.; Franco, J.; Fernandez, F.; Becerra, N.; Sabaduche, M.; Tovar, M.A.; et al. The Innovative Socio-economic Interventions Against Tuberculosis (ISIAT) project: An operational assessment. Int. J. Tuberc. Lung Dis. 2011, 15, S50–S57. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). The World Health Organisation’s Global Health Expenditure Database. Available online: www.apps.who.int/nha/database (accessed on 23 October 2019).
- Hone, T.; Mirelman, A.J.; Rasella, D.; Paes-Sousa, R.; Barreto, M.L.; Rocha, R.; Millett, C. Effect of economic recession and impact of health and social protection expenditures on adult mortality: A longitudinal analysis of 5565 Brazilian municipalities. Lancet Glob. Health 2019, 7, e1575–e1583. [Google Scholar] [CrossRef]
- United Nations. United Nations Social Development Report 2019. Available online: https://www.unstats.un.org/sdgs/report/2019 (accessed on 23 October 2019).
- Richterman, A.; Steer-massaro, J.; Jarolimova, J.; Nguyen, L.B.L.; Werdenberg, J.; Ivers, L.C. Systematic reviews Cash interventions to improve clinical outcomes for pulmonary tuberculosis: Systematic review and meta-analysis. Bull. World Health Organ. 2018, 96, 471–483. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Tovar, M.A.; Huff, D.; Boccia, D.; Montoya, R.; Ramos, E.; Datta, S.; Saunders, M.J.; Lewis, J.J.; Gilman, R.H.; et al. A randomized controlled study of socioeconomic support to enhance tuberculosis prevention and treatment, Peru. Bull. World Health Organ. 2017, 95, 270–280. [Google Scholar] [CrossRef] [PubMed]
- Wingfield, T.; Tovar, M.A.; Huff, D.; Boccia, D.; Montoya, R.; Ramos, E.; Datta, S.; Saunders, M.J.; Lewis, J.J.; Gilman, R.H.; et al. Socioeconomic support to improve initiation of tuberculosis preventive therapy and increase tuberculosis treatment success in Peru: A household-randomised, controlled evaluation. Lancet 2017, 389, S16. [Google Scholar] [CrossRef]
- Van Hoorn, R.; Jaramillo, E.; Collins, D.; Gebhard, A.; van den Hof, S. The Effects of Psycho-Emotional and Socio-Economic Support for Tuberculosis Patients on Treatment Adherence and Treatment Outcomes—A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0154095. [Google Scholar] [CrossRef] [PubMed]
- Nery, J.S.; Rodrigues, L.C.; Rasella, D.; Aquino, R.; Barreira, D.; Torrens, A.W.; Boccia, D.; Penna, G.O.; Penna, M.L.F.; Barreto, M.L.; et al. Effect of Brazil’s conditional cash transfer programme on tuberculosis incidence. Int. J. Tuberc. Lung Dis. 2017, 21, 790–796. [Google Scholar] [CrossRef] [PubMed]
- Torrens, A.W.; Rasella, D.; Boccia, D.; Maciel, E.L.N.; Nery, J.S.; Olson, Z.D.; Barreira, D.C.N.; Sanchez, M.N. Effectiveness of a conditional cash transfer programme on TB cure rate: A retrospective cohort study in Brazil. Trans. R. Soc. Trop. Med. Hyg. 2016, 110, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Klein, K.; Bernachea, M.P.; Irribarren, S.; Gibbons, L.; Chirico, C.; Rubinstein, F. Evaluation of a social protection policy on tuberculosis treatment outcomes: A prospective cohort study. PLoS Med. 2019, 9, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Health Organisation Guidelines for Treatment of Drug-Susceptible Tuberculosis and Patient Care (2017 Update); World Health Organization: Geneva, Switzerland, 2017.
- National Tuberculosis Program Nepal Annual Report 2074/75 (2018); National Tuberculosis Center: Bhaktapur, Nepal, 2018.
- World Health Organisation Global Tuberculosis Report 2018; World Health Organization: Geneva, Switzerland, 2018.
- De Cuevas, R.M.A.; Lawson, L.; Al-Sonboli, N.; Al-Aghbari, N.; Arbide, I.; Sherchand, J.B.; Nnamdi, E.E.; Aseffa, A.; Yassin, M.A.; Abdurrahman, S.T.; et al. Patients direct costs to undergo TB diagnosis. Infect. Dis. Poverty 2016, 5, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Bam, T.S.; Gunneberg, C.; Chamroonsawasdi, K.; Bam, D.S.; Aalberg, O.; Kasland, O.; Shiyalap, K.; Srisorrachatr, S. Factors affecting patient adherence to DOT in urban Kathmandu, Nepal. Int. J. Tuberc. Lung Dis. 2006, 10, 270–276. [Google Scholar] [PubMed]
- Ten Asbroek, A.H.; Bijlsma, M.W.; Malla, P.; Shrestha, B.; Delnoji, D.M. The road to tuberculosis treatment in rural Nepal: A qualitative assessment of 26 journeys. BMC Health Serv. Res. 2008, 10, 1–10. [Google Scholar]
- Baral, S.C.; Aryal, Y.; Bhattarai, R.; King, R.; Newell, J.N. The importance of providing counselling and financial support to patients receiving treatment for multi-drug resistant TB: Mixed method qualitative and pilot intervention studies. BMC Public Health 2014, 14, 46. [Google Scholar] [CrossRef] [PubMed]
- Dixit, K.; Rai, B.; Gurung, S.C.; Dhital, R.; Sah, M.K.; Aryal, T.P.; Pandit, R.N.; Majhi, G.; Caws, M.; Wingfield, T. Barriers and facilitators to accessing and engaging in tuberculosis care: A qualitative study from Nepal. In Proceedings of the 50th Union World Conference on Lung Health, Hyderabad, India, 30 October–2 November 2019. [Google Scholar]
- Dixit, K.; Gurung, S.; Dhital, R.; Caws, M.; Wingfield, T. Patient and stakeholder perspectives on barriers and facilitators to tuberculosis care in Nepal. In Proceedings of the 11th European Congress on Tropical Medicine and International Health, Liverpool, UK, 16–20 September 2019. [Google Scholar]
- Gurung, S.; Dixit, K.; Rai, B.; Caws, M.; Paudel, P.R.; Dhital, D.; Acharya, S.; Budhathoki, G.; Malla, D.; Levy, J.W.; et al. The role of active case finding in reducing patient incurred catastrophic costs for tuberculosis in Nepal. Infect. Dis. Poverty 2019, 8, 99. [Google Scholar] [CrossRef] [PubMed]
- Tuberculosis Patient Cost Survey: A Handbook; World Health Organization: Geneva, Switzerland, 2017.
- Rudgard, W.E.; Evans, C.A.; Sweeney, S.; Wingfield, T.; Lönnroth, K.; Barreira, D.; Boccia, D. Comparison of two cash transfer strategies to prevent catastrophic costs for poor tuberculosis-affected households in low- and middle-income countries: An economic modelling study. PLoS Med. 2017, 14, 1–28. [Google Scholar] [CrossRef] [PubMed]
- Finnie, R.K.C.; Khoza, L.B.; van den Borne, B.; Mabunda, T.; Abotchie, P.; Mullen, P.D. Factors associated with patient and health care system delay in diagnosis and treatment for TB in sub-Saharan African countries with high burdens of TB and HIV. Trop. Med. Int. Health 2011, 16, 394–411. [Google Scholar] [CrossRef] [PubMed]
- Sommerland, N.; Wouters, E.; Mitchell, E.M.; Ngicho, M.; Redwood, L.; Masquillier, C.; van Hoorn, R.; van der Hof, S.; Van Rie, A. Evidence-based interventions to reduce tuberculosis stigma: A systematic review. Int. J. Tuberc. Lung Dis. 2017, 21, S81–S86. [Google Scholar] [CrossRef] [PubMed]
- Macq, J.; Solis, A.; Martinez, G. Assessing the stigma of tuberculosis. Psychol. Health Med. 2006, 11, 346–352. [Google Scholar] [CrossRef] [PubMed]
- De Almeida Crispim, J.; da Silva, L.M.C.; Yamamura, M.; Popolin, M.P.; Ramos, A.C.V.; Arroyo, L.H.; de Queiroz, A.A.R.; de Souza Belchior, A.; dos Santos, D.T.; Pieri, F.M.; et al. Validity and reliability of the tuberculosis-related stigma scale version for Brazilian Portuguese. BMC Infect. Dis. 2017, 17, 1–8. [Google Scholar] [CrossRef]
- Chinouya, M.J.; Adeyanju, O. A disease called stigma: The experience of stigma among African men with TB diagnosis in London. Public Health 2017, 145, 45–50. [Google Scholar] [CrossRef] [PubMed]
- NHRC. Assessment of Social Health Insurance Scheme in Selected Districts of Nepal; Nepal Health Research Council: Kathmandu, Nepal, 2018.
- Kidd, S.; Calder, R.; Wylde, E. Assessing Targeting Options for Nepal’s Social Grants: What does the Evidence Tell Us? Development Pathways (UK) and DFID (Nepal); Department for International Development: London, UK, 2015.
- Kidd, S.; Calder, R. Conditional Cash Transfer Programmes: Their Relevance for Nepal; Department for International Development: London, UK, 2011.
- Willitts-King, B.; Bryant, J. Scaling up Humanitarian Cash Transfers in Nepal; Working paper 503; Overseas Development Institute: London, UK; Available online: https://www.odi.org/sites/odi.org.uk/files/resource-documents/11288.Pdf (accessed on 20 October 2019).

| Intervention Element | Existing Interventions | Refinements of Existing Interventions | Suitable Potential Interventions | Mode of Delivery |
|---|---|---|---|---|
| Psychosocial | Routine NTP-led counseling for TB-affected people, which focuses solely on TB treatment adherence There is no routine counselling available to address the psychosocial impact of TB (e.g., stigma) | Existing counselling about adherence to TB medications could be supplemented by complementary psychosocial counselling | Educational and social awareness campaigns Provision of complementary counseling focused on stigma, low mood and depression, and isolation and marginalization Integrated psychosocial counseling for people with TB and comorbidities (e.g., diabetes, depression) | Psychosocial counseling to patients/households by trained health workers in healthcare facilities or in people’s homes Peer counseling and mutual support (“TB survivors group”) Research into psychosocial status of TB-affected people throughout treatment, especially vulnerable groups |
| Economic | Rs 3000/month as nutritional/transport allowance for ambulatory DR cases Rs 1000/month for hostel-based DR cases Community-based DOT: Rs 1500 for volunteers, Rs 500 for health worker | For people with DS-TB Rs 1500/month nutritional allowance for every DS case Rs 500/month transport allowance (conditional) for DOT and follow up Rs 1000 for side effect management (conditional) For people with DR-TB Rs 3000/month for transportation Rs 2000/month for nutrition Rs 5000 for side effect management (conditional) | Income generation activities or back-to-work schemes Cash transfer schemes Incentivized TB screening program (e.g., economic, nutritional, or other incentive for attending TB screening facilities, being screened for TB if appropriate, and/or having a positive TB smear or culture) Nutritional package program for TB-affected person and their household | Conditional cash transfer through bank accounts or mobile phones Household visits to reduce travel costs and support TB treatment and prevention activities Partnering with local organizations to provide support and DOT Community sensitization and mobilization Microcredit and vocational training |
| Vulnerable Groups | Targeting Support | Benefits | Drawbacks |
|---|---|---|---|
| Two main options for provision of socioeconomic support were discussed:
|
|
|
| Psychosocial Package | Votes | Economic Package | Votes |
|---|---|---|---|
| A. CB-DOT provider / CHV assesses stigma level at household visit (or in hostel) and invite whole household to local mutual peer support TB group | 21% (8/38) | A. Economic intervention:
| 12% (4/34) |
| B. CB-DOT provider / CHV assesses stigma level at household visit and do stigma counselling session with household during visit | 79% (30/38) | B. Economic intervention:
| 88% (30/34) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rai, B.; Dixit, K.; Prasad Aryal, T.; Mishra, G.; Teixeira de Siqueira-Filha, N.; Paudel, P.R.; Levy, J.W.; van Rest, J.; Gurung, S.C.; Dhital, R.; et al. Developing Feasible, Locally Appropriate Socioeconomic Support for TB-Affected Households in Nepal. Trop. Med. Infect. Dis. 2020, 5, 98. https://doi.org/10.3390/tropicalmed5020098
Rai B, Dixit K, Prasad Aryal T, Mishra G, Teixeira de Siqueira-Filha N, Paudel PR, Levy JW, van Rest J, Gurung SC, Dhital R, et al. Developing Feasible, Locally Appropriate Socioeconomic Support for TB-Affected Households in Nepal. Tropical Medicine and Infectious Disease. 2020; 5(2):98. https://doi.org/10.3390/tropicalmed5020098
Chicago/Turabian StyleRai, Bhola, Kritika Dixit, Tara Prasad Aryal, Gokul Mishra, Noemia Teixeira de Siqueira-Filha, Puskar Raj Paudel, Jens W. Levy, Job van Rest, Suman Chandra Gurung, Raghu Dhital, and et al. 2020. "Developing Feasible, Locally Appropriate Socioeconomic Support for TB-Affected Households in Nepal" Tropical Medicine and Infectious Disease 5, no. 2: 98. https://doi.org/10.3390/tropicalmed5020098
APA StyleRai, B., Dixit, K., Prasad Aryal, T., Mishra, G., Teixeira de Siqueira-Filha, N., Paudel, P. R., Levy, J. W., van Rest, J., Gurung, S. C., Dhital, R., Lönnroth, K., Squire, S. B., Caws, M., & Wingfield, T. (2020). Developing Feasible, Locally Appropriate Socioeconomic Support for TB-Affected Households in Nepal. Tropical Medicine and Infectious Disease, 5(2), 98. https://doi.org/10.3390/tropicalmed5020098






