Low Praziquantel Treatment Coverage for Schistosoma mansoni in Mayuge District, Uganda, Due to the Absence of Treatment Opportunities, Rather Than Systematic Non-Compliance
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval and Study Setting
2.2. Survey Methodology
2.3. Outcomes and Explanatory Variables
2.4. Data Analysis
3. Results
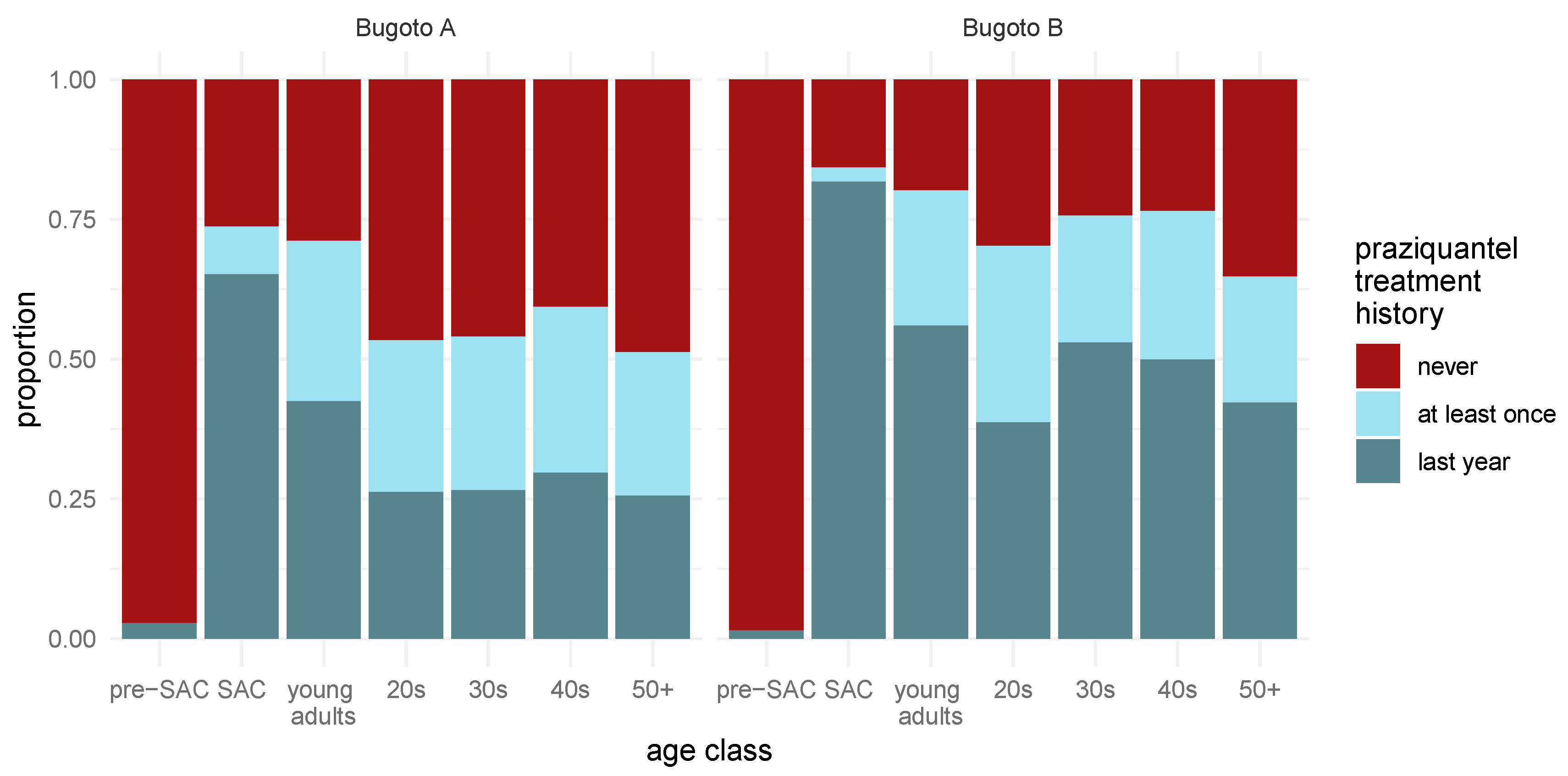
3.1. Self-Reported Praziquantel Uptake in Bugoto A and Bugoto B
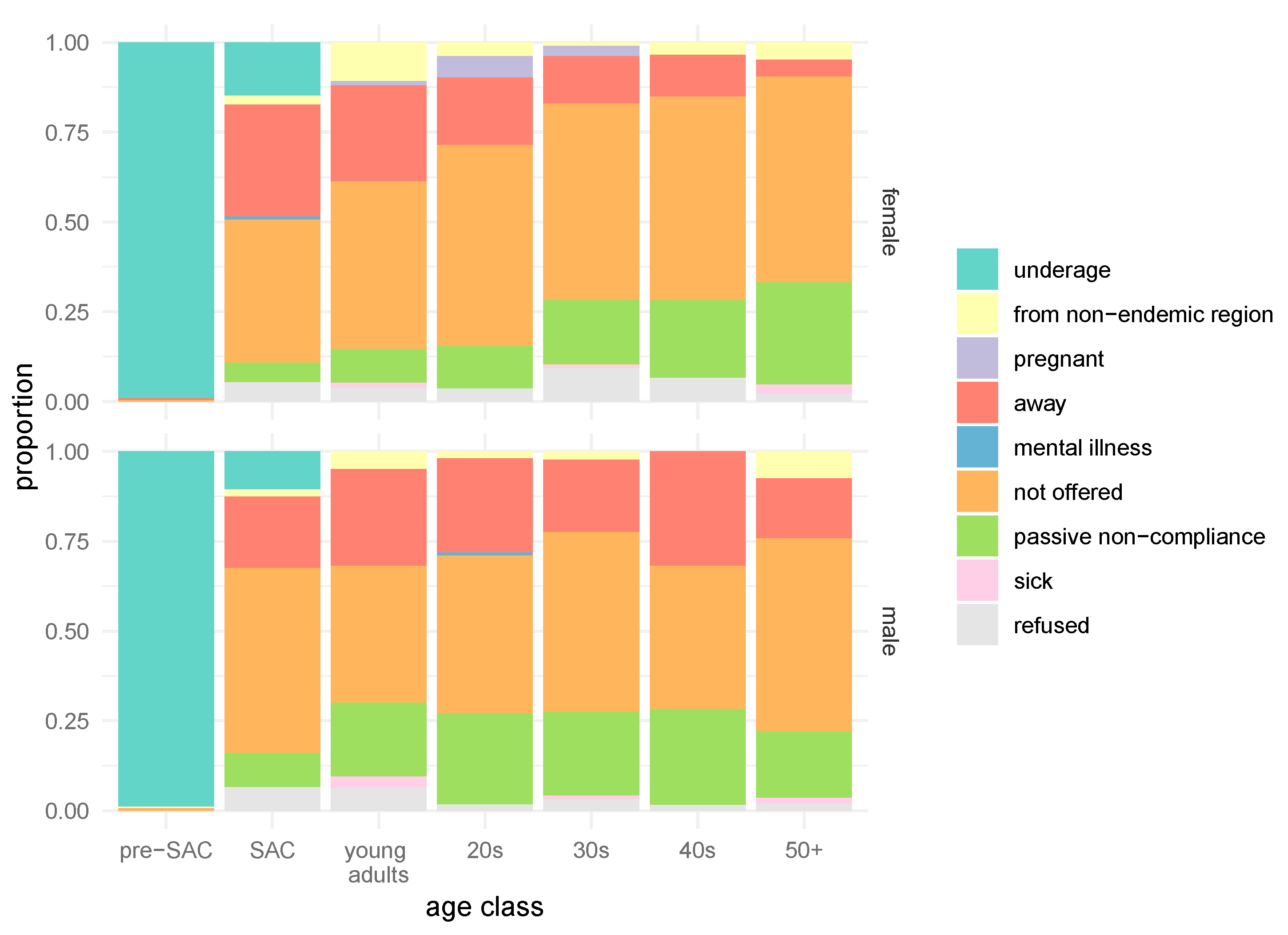
3.2. Self-Reported Reasons for Not Receiving Praziquantel during the Last MDA Round
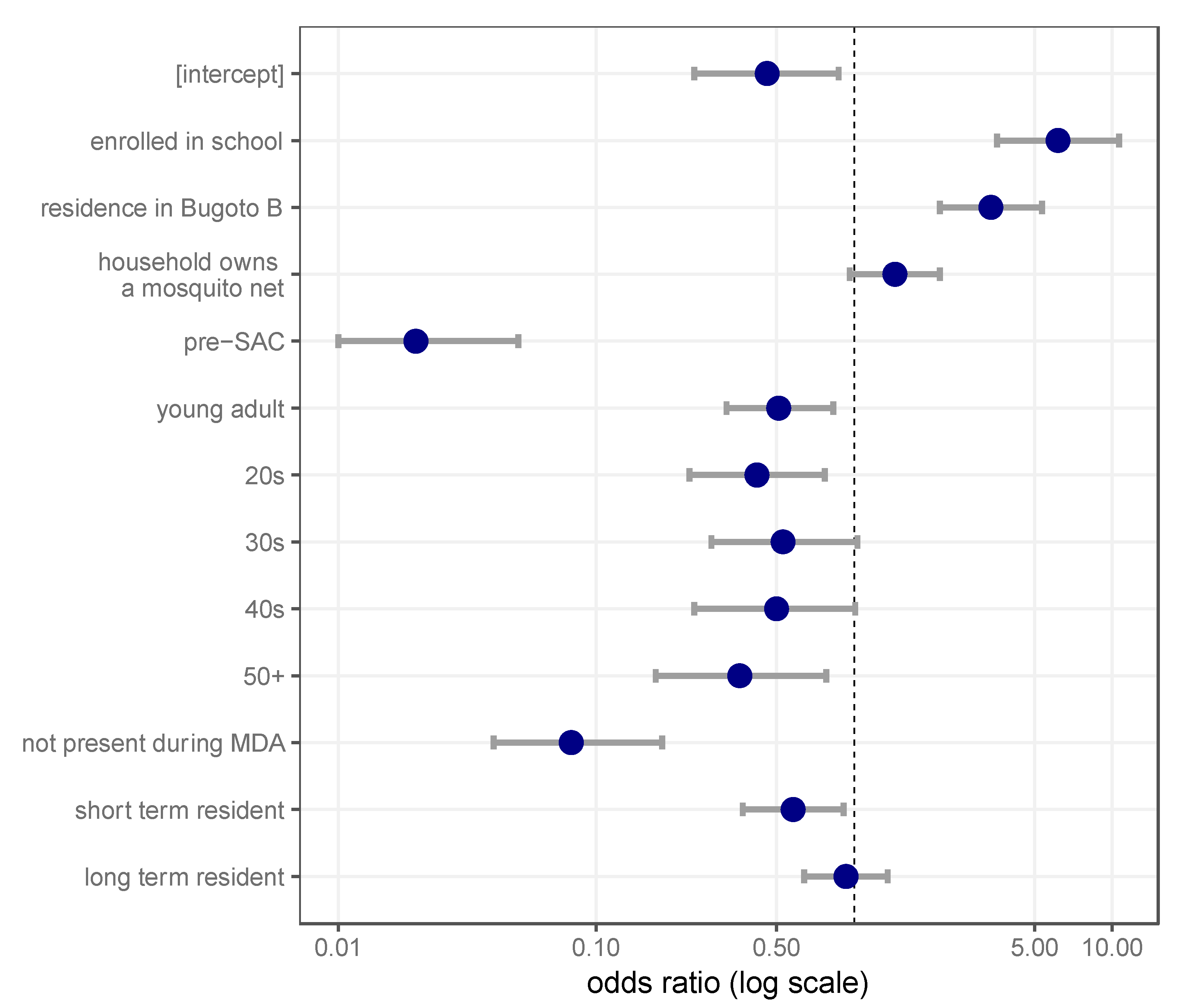
3.3. Socio-Economic and Individual Risk Factors Influence Praziquantel Uptake
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- WHO. Schistosomiasis: Progress Report 2001–2011, Strategic Plan 2012–2020; WHO: Geneva, Switzerland, 2013. [Google Scholar]
- Savioli, L.; Albonico, M.; Colley, D.G.; Correa-Oliveira, R.; Fenwick, A.; Green, W.; Kabatereine, N.; Kabore, A.; Katz, N.; Klohe, K.; et al. Building a global schistosomiasis alliance: An opportunity to join forces to fight inequality and rural poverty. Infect. Dis. Poverty 2017, 6, 65. [Google Scholar] [CrossRef] [PubMed]
- Hotez, P.J.; Molyneux, D.H.; Fenwick, A.; Kumaresan, J.; Sachs, S.E.; Sachs, J.D.; Savioli, L. Control of neglected tropical diseases. N. Engl. J. Med. 2007, 357, 1018–1027. [Google Scholar] [CrossRef] [PubMed]
- Hotez, P.J.; Alvarado, M.; Basanez, M.G.; Bolliger, I.; Bourne, R.; Boussinesq, M.; Brooker, S.J.; Brown, A.S.; Buckle, G.; Budke, C.M.; et al. The Global Burden of Disease Study 2010: Interpretation and implications for the neglected tropical diseases. PLoS Negl. Trop. Dis. 2014, 8, e2865. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 Maternal Mortality Collaborators. Global, regional, and national levels of maternal mortality, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1775–1812. [Google Scholar] [CrossRef]
- GBD 2016 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1260–1344. [Google Scholar] [CrossRef]
- Lo, N.C.; Addiss, D.G.; Hotez, P.J.; King, C.H.; Stothard, J.R.; Evans, D.S.; Colley, D.G.; Lin, W.; Coulibaly, J.T.; Bustinduy, A.L.; et al. A call to strengthen the global strategy against schistosomiasis and soil-transmitted helminthiasis: The time is now. Lancet Infect. Dis. 2017, 17, e64–e69. [Google Scholar] [CrossRef]
- Colley, D.G.; Andros, T.S.; Campbell, C.H., Jr. Schistosomiasis is more prevalent than previously thought: What does it mean for public health goals, policies, strategies, guidelines and intervention programs? Infect. Dis. Poverty 2017, 6, 63. [Google Scholar] [CrossRef] [PubMed]
- WHO. Preventive Chemotherapy in Human Helminthiasis: Coordinated Use of Anthelminthic Drugs in Control Interventions: A Manual for Health Professionals and Programme Managers; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- WHO. Accelerating Work to Overcome the Global Impact of Neglected Tropical Diseases—A Roadmap for Implementation; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Turner, H.C.; Truscott, J.E.; Bettis, A.A.; Farrell, S.H.; Deol, A.K.; Whitton, J.M.; Fleming, F.M.; Anderson, R.M. Evaluating the variation in the projected benefit of community-wide mass treatment for schistosomiasis: Implications for future economic evaluations. Parasit. Vectors 2017, 10, 213. [Google Scholar] [CrossRef] [PubMed]
- Shuford, K.V.; Turner, H.C.; Anderson, R.M. Compliance with anthelmintic treatment in the neglected tropical diseases control programmes: A systematic review. Parasit. Vectors 2016, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- French, M.D.; Churcher, T.S.; Webster, J.P.; Fleming, F.M.; Fenwick, A.; Kabatereine, N.B.; Sacko, M.; Garba, A.; Toure, S.; Nyandindi, U.; et al. Estimation of changes in the force of infection for intestinal and urogenital schistosomiasis in countries with schistosomiasis control initiative-assisted programmes. Parasit. Vectors 2015, 8, 558. [Google Scholar] [CrossRef] [PubMed]
- Rollinson, D.; Knopp, S.; Levitz, S.; Stothard, J.R.; Tchuem Tchuente, L.A.; Garba, A.; Mohammed, K.A.; Schur, N.; Person, B.; Colley, D.G.; et al. Time to set the agenda for schistosomiasis elimination. Acta Trop. 2013, 128, 423–440. [Google Scholar] [CrossRef] [PubMed]
- Kabatereine, N.B.; Tukahebwa, E.; Kazibwe, F.; Namwangye, H.; Zaramba, S.; Brooker, S.; Stothard, J.R.; Kamenka, C.; Whawell, S.; Webster, J.P.; et al. Progress towards countrywide control of schistosomiasis and soil-transmitted helminthiasis in Uganda. Trans. R. Soc. Trop. Med. Hyg. 2006, 100, 208–215. [Google Scholar] [CrossRef] [PubMed]
- Standley, C.J.; Adriko, M.; Arinaitwe, M.; Atuhaire, A.; Kazibwe, F.; Fenwick, A.; Kabatereine, N.B.; Stothard, J.R. Epidemiology and control of intestinal schistosomiasis on the Sesse Islands, Uganda: Integrating malacology and parasitology to tailor local treatment recommendations. Parasit. Vectors 2010, 3, 64. [Google Scholar] [CrossRef] [PubMed]
- Standley, C.J.; Adriko, M.; Besigye, F.; Kabatereine, N.B.; Stothard, R.J. Confirmed local endemicity and putative high transmission of Schistosoma mansoni in the Sesse Islands, Lake Victoria, Uganda. Parasit. Vectors 2011, 4, 29. [Google Scholar] [CrossRef] [PubMed]
- Bockarie, M.J.; Kelly-Hope, L.A.; Rebollo, M.; Molyneux, D.H. Preventive chemotherapy as a strategy for elimination of neglected tropical parasitic diseases: Endgame challenges. Philos. Trans. R. Soc. Lond. B 2013, 368, 20120144. [Google Scholar] [CrossRef] [PubMed]
- WHO. Helminth Control in School-Age Children. A Guide for Managers for Control Programmes; WHO: Geneva, Switzerland, 2011. [Google Scholar]
- Truscott, J.; Gurarie, D.; Alsallaq, R.; Toor, J.; Yoon, N.; Farrell, S.; Turner, H.; Phillips, A.; Aurelio, H.; Ferro, J. A Comparison of two mathematical models of the impact of mass drug administration on the transmission and control of schistosomiasis. Epidemics 2017, 18, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Dyson, L.; Stolk, W.A.; Farrell, S.H.; Hollingsworth, T.D. Measuring and modelling the effects of systematic non-adherence to mass drug administration. Epidemics 2017, 18, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Farrell, S.H.; Truscott, J.E.; Anderson, R.M. The importance of patient compliance in repeated rounds of mass drug administration (MDA) for the elimination of intestinal helminth transmission. Parasit. Vectors 2017, 10, 291. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Republic of Uganda. Uganda Master Plan for National Neglected Tropical Diseases Programmes; Government of Uganda: Kampala, Uganda, 2014.
- Ministry of Health Republic of Uganda. Uganda Master Plan for National Neglected Tropical Diseases Programmes: 2017–2022; Government of Uganda: Kampala, Uganda, 2017.
- WHO. Schistosomiasis and Soil-Transmitted Helminthiases: Number of People Treated in 2016; WHO: Geneva, Switzerland, 2017. [Google Scholar]
- Chami, G.F.; Kontoleon, A.A.; Bulte, E.; Fenwick, A.; Kabatereine, N.B.; Tukahebwa, E.M.; Dunne, D.W. Community-directed mass drug administration is undermined by status seeking in friendship networks and inadequate trust in health advice networks. Soc. Sci. Med. 2017, 183, 37–47. [Google Scholar] [CrossRef] [PubMed]
- Chami, G.F.; Kontoleon, A.A.; Bulte, E.; Fenwick, A.; Kabatereine, N.B.; Tukahebwa, E.M.; Dunne, D.W. Profiling nonrecipients of mass drug administration for schistosomiasis and hookworm infections: A comprehensive analysis of praziquantel and albendazole coverage in community-directed treatment in Uganda. Clin. Infect. Dis. 2015, 62, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Tuhebwe, D.; Bagonza, J.; Kiracho, E.E.; Yeka, A.; Elliott, A.M.; Nuwaha, F. Uptake of mass drug administration programme for schistosomiasis control in Koome Islands, Central Uganda. PLoS ONE 2015, 10, e0123673. [Google Scholar] [CrossRef] [PubMed]
- Knopp, S.; Person, B.; Ame, S.M.; Ali, S.M.; Muhsin, J.; Juma, S.; Khamis, I.S.; Rabone, M.; Blair, L.; Fenwick, A.; et al. Praziquantel coverage in schools and communities targeted for the elimination of urogenital schistosomiasis in Zanzibar: A cross-sectional survey. Parasit. Vectors 2016, 9, 5. [Google Scholar] [CrossRef] [PubMed]
- Coulibaly, J.; Ouattara, M.; Barda, B.; Utzinger, J.; N’Goran, E.; Keiser, J. A rapid appraisal of factors influencing praziquantel treatment compliance in two communities endemic for schistosomiasis in Côte d’Ivoire. Trop. Med. Infect. Dis. 2018, 3, 69. [Google Scholar] [CrossRef] [PubMed]
- Krentel, A.; Fischer, P.U.; Weil, G.J. A review of factors that influence individual compliance with mass drug administration for elimination of lymphatic filariasis. PLoS Negl. Trop. Dis. 2013, 7, e2447. [Google Scholar] [CrossRef] [PubMed]
- Lamberton, P.H.; Kabatereine, N.B.; Oguttu, D.W.; Fenwick, A.; Webster, J.P. Sensitivity and specificity of multiple Kato-Katz thick smears and a circulating cathodic antigen test for Schistosoma mansoni diagnosis pre- and post-repeated-praziquantel treatment. PLoS Negl. Trop. Dis. 2014, 8, e3139. [Google Scholar] [CrossRef] [PubMed]
- Crellen, T.; Walker, M.; Lamberton, P.H.; Kabatereine, N.B.; Tukahebwa, E.M.; Cotton, J.A.; Webster, J.P. Reduced efficacy of praziquantel against Schistosoma mansoni is associated with multiple rounds of mass drug administration. Clin. Infect. Dis. 2016, 63, 1151–1159. [Google Scholar] [PubMed]
- Fleming, F.M.; Fenwick, A.; Tukahebwa, E.M.; Lubanga, R.G.; Namwangye, H.; Zaramba, S.; Kabatereine, N.B. Process evaluation of schistosomiasis control in Uganda, 2003 to 2006: Perceptions, attitudes and constraints of a national programme. Parasitology 2009, 136, 1759–1769. [Google Scholar] [CrossRef] [PubMed]
- Fenwick, A.; Webster, J.P.; Bosque-Oliva, E.; Blair, L.; Fleming, F.M.; Zhang, Y.; Garba, A.; Stothard, J.R.; Gabrielli, A.F.; Clements, A.C.; et al. The Schistosomiasis Control Initiative (SCI): Rationale, development and implementation from 2002–2008. Parasitology 2009, 136, 1719–1730. [Google Scholar] [CrossRef] [PubMed]
- Global Health Observatory Data Repository. Available online: http://www.who.int/gho/en/ (accessed on 11 April 2018).
- French, M.D.; Churcher, T.S.; Gambhir, M.; Fenwick, A.; Webster, J.P.; Kabatereine, N.B.; Basáñez, M.G. Observed Reductions in Schistosoma mansoni transmission from large-scale administration of praziquantel in Uganda: A Mathematical modelling study. PLoS Negl. Trop. Dis. 2010, 4, e897. [Google Scholar] [CrossRef] [PubMed]
- Kabatereine, N.B.; Brooker, S.; Koukounari, A.; Kazibwe, F.; Tukahebwa, E.M.; Fleming, F.M.; Zhang, Y.; Webster, J.P.; Stothard, J.R.; Fenwick, A. Impact of a national helminth control programme on infection and morbidity in Ugandan schoolchildren. Bull. World Health Organ. 2007, 85, 91–99. [Google Scholar] [PubMed]
- The R Development Core Team. R: A Language and Environment for Statistical Computing; V 3.2; R Foundation for Statistical Computing: Vienna, Austria, 2015. [Google Scholar]
- Agresti, A.; Coull, B. Approximate is better than ‘exact’ for interval estimation of binomial proportions. Am. Stat. 1998, 52, 119–126. [Google Scholar]
- Akaike, H. Factor analysis and AIC. Psychometrika 1987, 52, 371–386. [Google Scholar] [CrossRef]
- Muhumuza, S.; Katahoire, A.; Nuwaha, F.; Olsen, A. Increasing teacher motivation and supervision is an important but not sufficient strategy for improving praziquantel uptake in Schistosoma mansoni control programs: Serial cross sectional surveys in Uganda. BMC Infect. Dis. 2013, 13, 590. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.; Allen, T. Does mass drug administration for the integrated treatment of neglected tropical diseases really work? Assessing evidence for the control of schistosomiasis and soil-transmitted helminths in Uganda. Health Res. Policy. Syst. 2011, 9, 3. [Google Scholar] [CrossRef] [PubMed]
- Muhumuza, S.; Olsen, A.; Katahoire, A.; Nuwaha, F. Uptake of preventive treatment for intestinal schistosomiasis among school children in Jinja district, Uganda: A cross-sectional study. PLoS ONE 2013, 8, e63438. [Google Scholar] [CrossRef] [PubMed]
- Fleming, F.M.; Matovu, F.; Hansen, K.S.; Webster, J.P. A mixed methods approach to evaluating community drug distributor performance in the control of neglected tropical diseases. Parasit. Vectors 2016, 9, 345. [Google Scholar] [CrossRef] [PubMed]
- Sangho, H.; Dabo, A.; Sidibe, A.; Dembele, R.; Diawara, A.; Diallo, A.; Konate, S. Coverage rate and satisfaction of populations after mass treatment with praziquantel and albendazole in Mali. Mali Med. 2009, 24, 21–24. [Google Scholar] [PubMed]
- Kabatereine, N.; Fleming, F.; Thuo, W.; Tinkitina, B.; Tukahebwa, E.M.; Fenwick, A. Community perceptions, attitude, practices and treatment seeking behaviour for schistosomiasis in L. Victoria Islands in Uganda. BMC Res. Notes 2014, 7, 900. [Google Scholar] [CrossRef] [PubMed]
- Parker, M.; Allen, T.; Hastings, J. Resisting control of neglected tropical diseases: Dilemmas in the mass treatment of schistosomiasis and soil-transmitted helminths in north-west Uganda. J. Biosoc. Sci. 2008, 40, 161–181. [Google Scholar] [CrossRef] [PubMed]
- Dabo, A.; Bary, B.; Kouriba, B.; Sankare, O.; Doumbo, O. Factors associated with coverage of praziquantel for schistosomiasis control in the community-direct intervention (CDI) approach in Mali (West Africa). Infect. Dis. Poverty 2013, 2, 11. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Republic of Uganda. Village Health Teams: Guide for Training the Trainers of Village Health Teams; Government of Uganda: Kampala, Uganda, 2010.
- Katabarwa, M.; Habomugisha, P.; Eyamba, A.; Agunyo, S.; Mentou, C. Monitoring ivermectin distributors involved in integrated health care services through community-directed interventions—A comparison of Cameroon and Uganda experiences over a period of three years (2004–2006). Trop. Med. Int. Health 2010, 15, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Adeneye, A.K.; Akinwale, O.P.; Idowu, E.T.; Adewale, B.; Manafa, O.U.; Sulyman, M.A.; Omotola, B.D.; Akande, D.O.; Mafe, M.A.; Appelt, B. Sociocultural aspects of mass delivery of praziquantel in schistosomiasis control: The Abeokuta experience. Res. Soc. Adm. Pharm. 2006, 3, 183–198. [Google Scholar] [CrossRef] [PubMed]
- Chami, G.F.; Kontoleon, A.A.; Bulte, E.; Fenwick, A.; Kabatereine, N.B.; Tukahebwa, E.M.; Dunne, D.W. Diffusion of treatment in social networks and mass drug administration. Nat. Commun. 2017, 8, 1929. [Google Scholar] [CrossRef] [PubMed]
- Woolhouse, M.E.; Dye, C.; Etard, J.-F.; Smith, T.; Charlwood, J.; Garnett, G.; Hagan, P.; Hii, J.; Ndhlovu, P.; Quinnell, R. Heterogeneities in the transmission of infectious agents: Implications for the design of control programs. Proc. Natl. Acad. Sci. USA 1997, 94, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Lwambo, N.; Siza, J.; Brooker, S.; Bundy, D.; Guyatt, H. Patterns of concurrent hookworm infection and schistosomiasis in schoolchildren in Tanzania. Trans. R. Soc. Trop. Med. Hyg. 1999, 93, 497–502. [Google Scholar] [CrossRef]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adriko, M.; Faust, C.L.; Carruthers, L.V.; Moses, A.; Tukahebwa, E.M.; Lamberton, P.H.L. Low Praziquantel Treatment Coverage for Schistosoma mansoni in Mayuge District, Uganda, Due to the Absence of Treatment Opportunities, Rather Than Systematic Non-Compliance. Trop. Med. Infect. Dis. 2018, 3, 111. https://doi.org/10.3390/tropicalmed3040111
Adriko M, Faust CL, Carruthers LV, Moses A, Tukahebwa EM, Lamberton PHL. Low Praziquantel Treatment Coverage for Schistosoma mansoni in Mayuge District, Uganda, Due to the Absence of Treatment Opportunities, Rather Than Systematic Non-Compliance. Tropical Medicine and Infectious Disease. 2018; 3(4):111. https://doi.org/10.3390/tropicalmed3040111
Chicago/Turabian StyleAdriko, Moses, Christina L. Faust, Lauren V. Carruthers, Arinaitwe Moses, Edridah M. Tukahebwa, and Poppy H. L. Lamberton. 2018. "Low Praziquantel Treatment Coverage for Schistosoma mansoni in Mayuge District, Uganda, Due to the Absence of Treatment Opportunities, Rather Than Systematic Non-Compliance" Tropical Medicine and Infectious Disease 3, no. 4: 111. https://doi.org/10.3390/tropicalmed3040111
APA StyleAdriko, M., Faust, C. L., Carruthers, L. V., Moses, A., Tukahebwa, E. M., & Lamberton, P. H. L. (2018). Low Praziquantel Treatment Coverage for Schistosoma mansoni in Mayuge District, Uganda, Due to the Absence of Treatment Opportunities, Rather Than Systematic Non-Compliance. Tropical Medicine and Infectious Disease, 3(4), 111. https://doi.org/10.3390/tropicalmed3040111





