Coverage, Timelines, and Determinants of Incomplete Immunization in Bangladesh
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Study Design and Data Collection
2.3. EPI History and Schedule
2.4. Immunization Coverage and Timeliness
2.5. Explanatory Variables
2.6. Analytical Methods
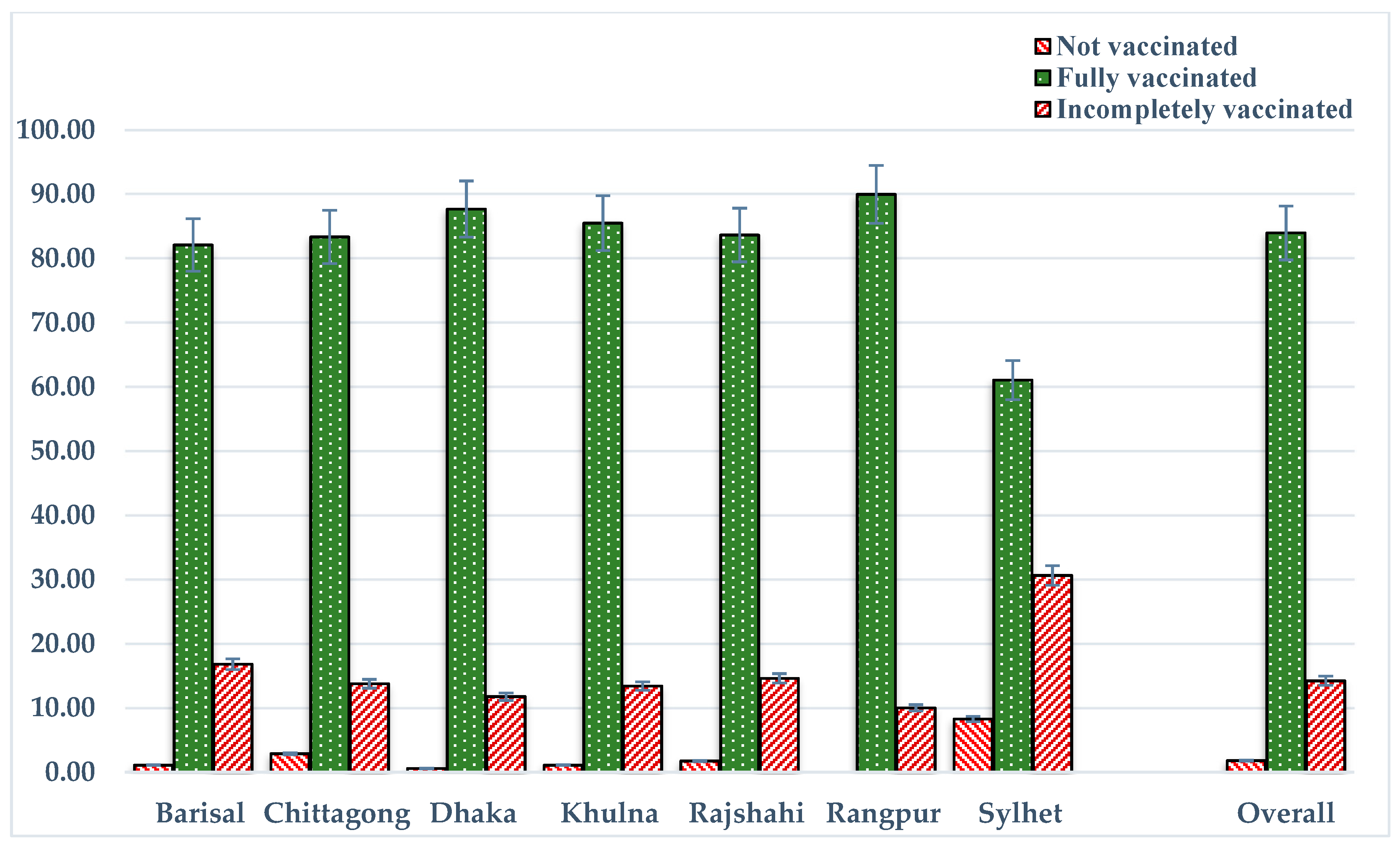
3. Results
3.1. Background Characteristics
3.2. Failure of Timely Vaccinations and Associated Factors
3.3. Factors of Incomplete Vaccinations
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Keja, K.; Chan, C.; Hayden, G.; Henderson, R. Expanded programme on immunization. World Health Stat. Q. 1988, 41, 59–63. [Google Scholar] [PubMed]
- Goldie, S.J.; O’Shea, M.; Diaz, M.; Kim, S.Y. Benefits, cost requirements and cost-effectiveness of the HPV16,18 vaccine for cervical cancer prevention in developing countries: Policy implications. Reprod. Health Matters 2008, 16, 86–96. [Google Scholar] [CrossRef]
- Andre, F.E.; Booy, R.; Bock, H.L.; Clemens, J.; Datta, S.K.; John, T.J.; Lee, B.W.; Lolekha, S.; Peltola, H.; Ruff, T.A.; et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull. World Health Organ. 2008, 86, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.; Kaddar, M. Role of the private sector in the provision of immunization services in low- and middle-income countries. Health Policy Plan. 2011, 26, 4–12. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Immunization Surveillance, Assessment and Monitoring; World Health Organization: Washington, DC, USA, 2014. [Google Scholar]
- Black, R.E.; Cousens, S.; Johnson, H.L.; Lawn, J.E.; Rudan, I.; Bassani, D.G.; Jha, P.; Campbell, H.; Walker, C.F.; Cibulskis, R.; et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet 2010, 375, 1969–1987. [Google Scholar] [CrossRef]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy—Causes, consequences, and a call to action. Vaccine 2015, 33, D66–D71. [Google Scholar] [CrossRef] [PubMed]
- Fadnes, L.T.; Jackson, D.; Engebretsen, I.M.; Zembe, W.; Sanders, D.; Sommerfelt, H.; Tylleskär, T. The PROMISE-EBF Study Group. Vaccination coverage and timeliness in three South African areas: A prospective study. BMC Public Health 2011, 11, 404. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaidi, S.M.A.; Khowaja, S.; Dharma, V.K.; Khan, A.J.; Chandir, S. Coverage, timeliness, and determinants of immunization completion in Pakistan: Evidence from the Demographic and Health Survey (2006-07). Hum. Vaccines Immunother. 2014, 10, 1712–1720. [Google Scholar] [CrossRef] [PubMed]
- Heininger, U.; Zuberbühler, M. Immunization rates and timely administration in pre-school and school-aged children. Eur. J. Pediatr. 2006, 165, 124–129. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Population Research and Training. Bangladesh Demographic and Health Survey 2014; NIPORT: Dhaka, Bangladesh; Mitra and Associates: Dhaka, Bangladesh; ICF International: Rockville, MD, USA, 2016.
- World Health Organization. Vaccination Coverage Cluster Surveys: Reference Manual; World Health Organization: Washington, DC, USA, 2015. [Google Scholar]
- Vasudevan, L.; Labrique, A.B.; Mehra, S.; Wu, L.; Levine, O.; Feikin, D.; Klemm, R.; Christian, P.; Keith, K.P., Jr. Maternal determinants of timely vaccination coverage among infants in rural Bangladesh. Vaccine 2014, 32, 5514–5519. [Google Scholar] [CrossRef] [PubMed]
- Hoest, C.; Seidman, J.C.; Lee, G.; Platts-Mills, J.A.; Ali, A.; Olortegui, M.P.; Bessong, P.; Chandyo, R.; Babji, S.; Mohan, V.R.; et al. Vaccine coverage and adherence to EPI schedules in eight resource poor settings in the MAL-ED cohort study. Vaccine 2017, 35, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Rammohan, A.; Awofeso, N. District-level variations in childhood immunizations in India: The role of socio-economic factors and health infrastructure. Soc. Sci. Med. 2015, 145, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Bugvi, A.S.; Rahat, R.; Zakar, R.; Zakar, M.Z.; Fischer, F.; Nasrullah, M.; Manawar, R. Factors associated with non-utilization of child immunization in Pakistan: Evidence from the Demographic and Health Survey 2006-07. BMC Public Health 2014, 14, 232. [Google Scholar] [CrossRef] [PubMed]
- An, D.T.M.; Lee, J.K.; Van Minh H, V.; Trang, N.T.H.; Huong, N.T.T.; Nam, Y.S.; Dung, D.V. Timely immunization completion among children in Vietnam from 2000 to 2011: A multilevel analysis of individual and contextual factors. Glob. Health Action 2016, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dietz, V.; Stevension, J.; Zell, E.R.; Cochi, S.; Hadler, S.; Eddins, D. Potential impact on vaccination coverage levels by administering vaccines simultaneously and reducing dropout rates. Arch. Pediatr. Adolesc. Med. 1994, 148, 943–949. [Google Scholar] [CrossRef] [PubMed]
- Breiman, R.F.; Streatfield, P.K.; Phelan, M.; Shifa, N.; Rashid, M.; Yunus, M. Effect of infant immunisation on childhood mortality in rural Bangladesh: Analysis of health and demographic surveillance data. Lancet 2004, 364, 2204–2211. [Google Scholar] [CrossRef]
- Odutola, A.; Afolabi, M.O.; Ogundare, E.O.; Lowe-Jallow, Y.N.; Worwui, A.; Okebe, J.; Martin, O.O. Risk factors for delay in age-appropriate vaccinations among Gambian children. BMC Health Serv. Res. 2015, 15, 346. [Google Scholar] [CrossRef] [PubMed]
- Uddin, M.J.; Adhikary, G.; Ali, M.W.; Ahmed, S.; Shamsuzzaman, M.; Odell, C.; Hashiguchi, L.; Lim, S.S.; Alam, N. Evaluation of impact of measles rubella campaign on vaccination coverage and routine immunization services in Bangladesh. BMC Infect. Dis. 2016, 16, 411. [Google Scholar] [CrossRef] [PubMed]
- Barata, R.B.; Ribeiro, M.C.S.D.A.; de Moraes, J.C.; Flannery, B. Socioeconomic inequalities and vaccination coverage: Results of an immunisation coverage survey in 27 Brazilian capitals, 2007–2008. J. Epidemiol. Commun. Health 2012, 66, 934–941. [Google Scholar] [CrossRef] [PubMed]
- Oyefara, J.L. Mothers’ Characteristics and immunization status of under-five children in Ojo Local Government Area, Lagos State, Nigeria. SAGE Open 2014, 4. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Uthman, O.A.; Ndumbe, P.M.; Hussey, G.D. Individual and contextual factors associated with low childhood immunisation coverage in sub-Saharan Africa: A multilevel analysis. PLoS ONE 2012, 7, e37905. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subhani, S.; Yaseen, R.; Khan, M.A.; Jeelani, G.; Fatima, R. Impact of mother’s education on child immunization: A comparative study of India and Pakistan. J. Financ. Econ. 2015, 3, 51–54. [Google Scholar] [CrossRef]
- Antai, D. Inequitable childhood immunization uptake in Nigeria: A multilevel analysis of individual and contextual determinants. BMC Infect. Dis. 2009, 9, 181. [Google Scholar] [CrossRef] [PubMed]
| Diseases | Vaccine | Recommended Age Period | Timely | Early | Late |
|---|---|---|---|---|---|
| Childhood tuberculosis (TB)/poliomyelitis | Bacille Calmette-Guerin (BCG) | At birth/0 day | 0–28 days | - | >28 days |
| Diphtheria/tetanus/pertussis/Hepatitis B/Hib pneumonia and meningitis | Pentavalent 1 | 42 days | 39–70 days | <39 days | >70 days |
| Pentavalent 2 | 70 days | 67–98 days | <67 days | >98 days | |
| Pentavalent 3 | 98 days | 95–126 days | <95 days | >126 days | |
| Poliomyelitis | Oral polio vaccine (OPV) 1 | 42 days | 39–70 days | <39 days | >70 days |
| OPV 2 | 70 days | 67–98 days | <67 days | >98 days | |
| OPV 3 | 98 days | 95–126 days | <95 days | >126 days | |
| Measles | Measles | 273 days | 270–301 days | <270 days | >301 days |
| Variables | n (%) |
|---|---|
| Sex of child | |
| Male | 862 (52.85) |
| Female | 769 (47.15) |
| Birth year | |
| 2012 | 460 (28.21) |
| 2013 | 1171 (71.79) |
| Birth season | |
| Summer | 537 (32.93) |
| Rainy | 563 (34.52) |
| Winter | 531 (32.55) |
| Birth order | |
| 1 | 657 (40.27) |
| 2–3 | 767 (47.07) |
| 4–5 | 151 (9.27) |
| >5 | 55 (3.39) |
| Place of birth | |
| Home | 973 (59.66) |
| Institution | 658 (40.34) |
| Birth size | |
| Normal | 1305 (80.04) |
| Small/poor | 325 (19.96) |
| Checkup of the infant from a professional | |
| Yes | 624 (38.27) |
| No | 1006 (61.73) |
| Mother’s number of living children | |
| 1–2 | 1227 (75.26) |
| >2 | 403 (24.74) |
| Mother’s age (in years) | |
| Less than 20 | 326 (20.00) |
| 20–34 | 1227 (75.23) |
| 35+ | 78 (4.77) |
| Mean age (mean ± S.D.) | 24.38 ± 5.53 |
| Mother’s education level | |
| No education | 206 (12.65) |
| Primary | 459 (28.14) |
| Secondary | 811 (49.72) |
| Higher | 155 (9.50) |
| Mother’s employment status | |
| Not employed | 1234 (75.71) |
| Employed | 396 (24.29) |
| Mother’s awareness of the community clinic | |
| No | 1174 (71.97) |
| Yes | 457 (28.03) |
| Mother’s access to electronic media | |
| Yes | 663 (40.66) |
| No | 968 (59.34) |
| Household fuel types | |
| Clean fuel | 238 (14.61) |
| Polluted fuel | 1392 (85.39) |
| Source of drinking water | |
| Improved | 1444 (88.53) |
| Non-improved | 187 (11.47) |
| Type of toilet | |
| Improved | 996 (61.11) |
| Non-improved | 634 (38.89) |
| Household size | |
| ≤5 members | 855 (52.42) |
| >5 members | 776 (47.58) |
| Average household size (mean ± S.D.) | 6.07 ± 2.81 |
| Wealth index | |
| Poorest | 373 (22.89) |
| Poorer | 292 (17.93) |
| Middle | 323 (19.80) |
| Richer | 336 (20.59) |
| Richest | 307 (18.80) |
| Residence | |
| Urban | 423 (25.96) |
| Rural | 1207 (74.04) |
| Divisions | |
| Barisal | 92 (5.63) |
| Chittagong | 349 (21.43) |
| Dhaka | 622 (38.17) |
| Khulna | 129 (7.89) |
| Rajshahi | 163 (10.01) |
| Rangpur | 146 (8.96) |
| Sylhet | 129 (7.91) |
| Vaccine Name | Time of Vaccination 1 | Had Vaccination Card (%) | Overall Coverage 2 (%) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Early, n (%) | Timely n (%) | Delayed, n (%) | |||||||||
| <2 Weeks | 2–3 Weeks | ≥4 Weeks | Total n (%) | <2 Months | 3–6 Months | ≥7 Months | Total n (%) | ||||
| BCG (n = 1201) | - | - | - | - | 293 (24.41) | 820 (90.40) | 80 (8.83) | 7 (0.78) | 908 (75.59) | 73.64 | 1597 (97.90) |
| Pentavalent 1 (n = 1201) | 11 (8.59) | 15 (11.79) | 100 (79.62) | 126 (10.47) | 754 (62.75) | 207 (64.34) | 108 (33.53) | 7 (2.14) | 322 (26.77) | 73.64 | 1582 (97.00) |
| Pentavalent 2 (n = 1180) | - | 2 (2.82) | 61 (97.18) | 63 (5.30) | 639 (54.18) | - | 457 (95.61) | 21 (4.39) | 478 (40.52) | 72.35 | 1556 (95.40) |
| Pentavalent 3 (n = 1141) | - | - | 31 (100.00) | 31 (2.74) | 527 (46.21) | - | 500 (85.87) | 82 (14.13) | 583 (51.05) | 69.96 | 1489 (91.30) |
| OPV 1 (n = 1201) | 12 (9.21) | 15 (11.88) | 99 (78.91) | 125 (10.40) | 754 (62.79) | 206 (64.35) | 107 (33.50) | 7 (2.15) | 322 (26.81) | 73.70 | 1589 (97.40) |
| OPV 2 (n = 1180) | - | 2 (2.87) | 60 (97.13) | 62 (5.22) | 639 (54.14) | - | 457 (95.68) | 21 (4.32) | 477 (40.64) | 72.35 | 1558 (95.50) |
| OPV 3 (n = 1141) | - | - | 32 (100.00) | 32 (2.81) | 525 (46.04) | - | 499 (85.82) | 83 (14.18) | 584 (51.16) | 69.96 | 1491 (91.40) |
| Measles (n = 1053) | 2 (1.42) | - | 122 (98.58) | 124 (11.78) | 551 (52.33) | - | - | 378 (100.00) | 378 (35.90) | 64.56 | 1404 (86.10) |
| Variables | Failure of Timely Vaccination | Incomplete Vaccination | ||
|---|---|---|---|---|
| BCG | Pentavalent Vaccine/OPV | Measles | ||
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Sex of children | ||||
| Male (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Female | 0.92 (0.69, 1.23) | 1.08 (0.84, 1.39) | 1.14 (0.88, 1.47) | 0.90 (0.66, 1.23) |
| Birth year | ||||
| 2012 | 1.06 (0.74, 1.50) | 1.04 (0.75, 1.43) | 1.1 (0.80, 1.53) | 1.15 (0.78, 1.69) |
| 2013 (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Birth season | ||||
| Summer | 1.53 ** (1.04, 2.26) | 0.94 (0.67, 1.31) | 1.49 ** (1.05, 2.10) | 1.70 ** (1.09, 2.67) |
| Rainy | 1.27 (0.90, 1.79) | 1.06 (0.78, 1.45) | 1.13 (0.82, 1.55) | 2.14 *** (1.45, 3.17) |
| Winter (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Birth order | ||||
| 1 | 1.04 (0.71, 1.53) | 1.16 (0.83, 1.62) | 1.44 (0.97, 2.03) | 1.1 (0.72, 1.67) |
| 2–3 (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| 4–5 | 0.99 (0.53, 1.87) | 1.68 (0.97, 2.91) | 1.20 (0.68, 2.13) | 2.10 ** (1.09, 4.02) |
| >5 | 1.87 (0.70, 5.04) | 2.10 (0.90, 4.88) | 3.11 ** (1.29, 7.54) | 1.80 (0.71, 4.58) |
| Place of birth | ||||
| Home | 1.39 (0.93, 2.07) | 2.13 ** (1.50, 3.03) | 0.91 (0.64, 1.30) | 1.25 (0.78, 2.01) |
| Institution (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Birth size | ||||
| Normal (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Small/poor | 1.30 (0.89, 1.91) | 1.06 (0.77, 1.47) | 0.83 (0.59, 1.16) | 1.21 (0.84, 1.75) |
| Checkup of the infant from a professional | ||||
| Yes | 1.40 (0.94, 2.09) | 1.77 *** (1.25, 2.51) | 1.33 (0.94, 1.89) | 0.93 (0.59, 1.48) |
| No (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Number of living children | ||||
| 1–2 | 0.67 (0.41, 1.08) | 1.48 ** (1.02, 2.18) | 0.92 (0.60, 1.39) | 1.48 (0.88, 2.51) |
| >2 (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Mother’s age (in years) | ||||
| Less than 20 | 1.48 (0.65, 3.41) | 0.76 (0.36, 1.62) | 1.15 (0.54, 2.44) | 3.21 ** (1.02, 10.13) |
| 20–34 | 1.34 (0.67, 2.70) | 0.76 (0.40, 1.45) | 1.39 (0.74, 2.62) | 3.01 ** (1.05, 8.60) |
| 35+ (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Mother’s education level | ||||
| No education | 0.83 (0.41, 1.68) | 2.34 ** (1.26, 4.35) | 0.93 (0.49, 1.76) | 2.25 (0.92, 5.54) |
| Primary | 1.19 (0.65, 2.18) | 2.37 *** (1.40, 4.01) | 1.49 (0.87, 2.55) | 2.72 ** (1.20, 6.16) |
| Secondary | 1.16 (0.68, 1.98) | 2.15 *** (1.35, 3.42) | 1.20 (0.75, 1.93) | 1.58 (0.72, 3.46) |
| Higher (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Mother’s employment status | ||||
| Not employed | 1.38 ** (1.02, 1.93) | 0.92 (0.68, 1.24) | 1.46 ** (1.06, 2.00) | 0.65 ** (0.46, 0.92) |
| Employed (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Aware of the community clinic | ||||
| No | 0.78 (0.57, 1.08) | 1.40 ** (1.06, 1.86) | 0.92 (0.69, 1.22) | 1.36 (1.01, 1.96) |
| Yes (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Access to electronic media | ||||
| Yes | 1.14 (0.74, 1.73) | 1.26 (0.88, 1.80) | 1.41 (0.98, 2.03) | 1.09 (0.69, 1.74) |
| No (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Source of drinking water | ||||
| Improved (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-improved | 2.73 ** (1.03, 7.21) | 0.66 (0.36, 1.21) | 1.13 (0.58, 2.23) | 1.46 (0.90, 2.37) |
| Type of toilet | ||||
| Improved (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-improved | 1.42 ** (1.01, 2.03) | 0.90 (0.66, 1.23) | 0.77 (0.56, 1.05) | 1.89 *** (1.32, 2.70) |
| Household size | ||||
| ≤5 members | 1.45 ** (1.06, 1.97) | 1.07 (0.81, 1.40) | 1.10 (0.83, 1.46) | 0.95 (0.67, 1.33) |
| >5 members (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Wealth index | ||||
| Poorest | 0.55 (0.27, 1.10) | 1.33 (0.72, 2.43) | 1.89 ** (1.02, 3.51) | 2.20 ** (1.05, 4.61) |
| Poorer | 0.54 (0.28, 1.04) | 1.16 (0.65, 2.06) | 2.17 ** (1.21, 3.89) | 1.26 (0.61, 2.60) |
| Middle | 0.92 (0.52, 1.64) | 1.13 (0.70, 1.84) | 1.64 ** (1.01, 2.66) | 1.10 (0.57, 2.14) |
| Richer | 1.02 (0.62, 1.67) | 0.8 (0.53, 1.21) | 1.47 (0.97, 2.23) | 1.01 (0.54, 1.84) |
| Richest (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Residence | ||||
| Urban (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Rural | 1.18 (0.82, 1.71) | 0.95 (0.69, 1.31) | 1.14 (0.82, 1.59) | 0.75 (0.49, 1.15) |
| Divisions | ||||
| Barisal | 1.61 (0.86, 3.01) | 1.73 (0.91, 3.29) | 0.65 (0.33, 1.26) | 1.7 (0.75, 3.85) |
| Chittagong | 3.01 *** (1.85, 4.91) | 1.29 (0.81, 2.05) | 1.24 (0.77, 2.01) | 1.5 (0.77, 2.90) |
| Dhaka | 3.78 *** (2.40, 5.95) | 0.98 (0.64, 1.52) | 1.84 ** (1.17, 2.91) | 1.18 (0.63, 2.23) |
| Khulna | 4.74 *** (2.44, 9.19) | 1.83 ** (1.02, 3.27) | 0.75 (0.41, 1.39) | 1.77 (0.81, 3.88) |
| Rajshahi | 4.96 *** (2.73, 9.02) | 1.52 (0.89, 2.60) | 1.37 (0.79, 2.38) | 1.62 (0.78, 3.37) |
| Rangpur (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Sylhet | 7.63 *** (3.55, 16.38) | 3.15 *** (1.6, 6.18) | 1.07 (0.56, 2.05) | 3.76 *** (1.84, 7.67) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sheikh, N.; Sultana, M.; Ali, N.; Akram, R.; Mahumud, R.A.; Asaduzzaman, M.; Sarker, A.R. Coverage, Timelines, and Determinants of Incomplete Immunization in Bangladesh. Trop. Med. Infect. Dis. 2018, 3, 72. https://doi.org/10.3390/tropicalmed3030072
Sheikh N, Sultana M, Ali N, Akram R, Mahumud RA, Asaduzzaman M, Sarker AR. Coverage, Timelines, and Determinants of Incomplete Immunization in Bangladesh. Tropical Medicine and Infectious Disease. 2018; 3(3):72. https://doi.org/10.3390/tropicalmed3030072
Chicago/Turabian StyleSheikh, Nurnabi, Marufa Sultana, Nausad Ali, Raisul Akram, Rashidul Alam Mahumud, Muhammad Asaduzzaman, and Abdur Razzaque Sarker. 2018. "Coverage, Timelines, and Determinants of Incomplete Immunization in Bangladesh" Tropical Medicine and Infectious Disease 3, no. 3: 72. https://doi.org/10.3390/tropicalmed3030072
APA StyleSheikh, N., Sultana, M., Ali, N., Akram, R., Mahumud, R. A., Asaduzzaman, M., & Sarker, A. R. (2018). Coverage, Timelines, and Determinants of Incomplete Immunization in Bangladesh. Tropical Medicine and Infectious Disease, 3(3), 72. https://doi.org/10.3390/tropicalmed3030072






