Snakebites in the Central American Region: More Government Attention Required
Abstract
1. Introduction
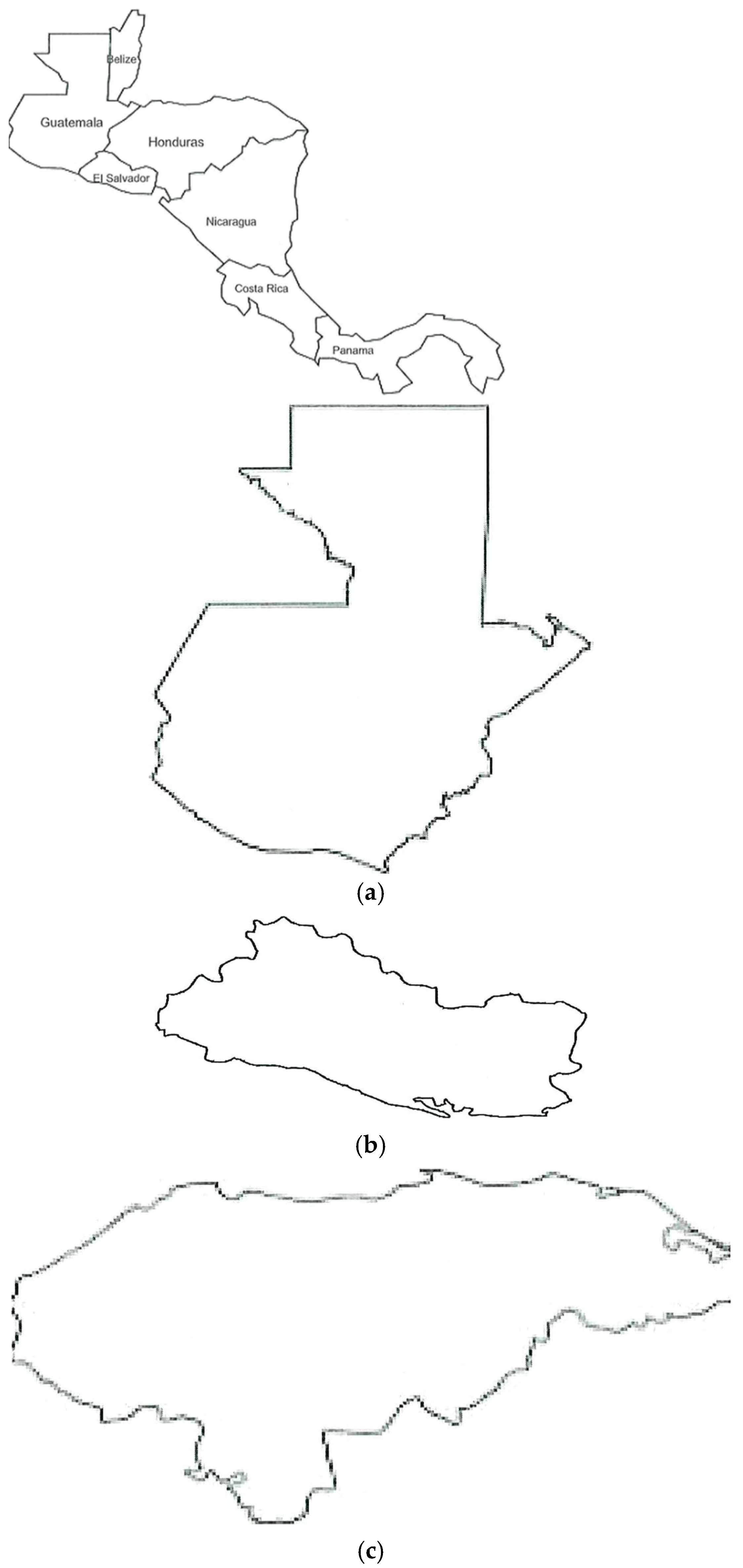
1.1. Snakebites in the Central American Region
1.2. Occupational Risk for Snakebites (Ophidian Accidents) in Central America
1.3. Species of the Family Viperidae
1.4. Species of the Family Elapidae
1.5. Treatment of Snakebites
2. Methods
3. Results
3.1. Belize
3.2. Guatemala
3.3. Honduras
3.4. El Salvador
3.5. Costa Rica
3.6. Panama
3.7. Nicaragua
4. Discussion
5. Conclusions
Future Directions
- http://gisgeography.com/central-america-blank-map/, accessed on 20 May 2025
- http://www.inaturalist.org, accessed on 20 May 2025
- https//icp.ucr.ac.cr/en/services and products/products-human-use, accessed on 20 May 2025
- https://birmex.gob.mx/, accessed on 20 May 2025
- https//www.miamidade.gov/fire/library/antivenom-species-covered.pdf, accessed on 20 May 2025
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Author | Country | Study Year | # Participants | Mean Age in Years | Reported Symptoms | Time from Snakebite to Healthcare Facility |
|---|---|---|---|---|---|---|
| Wellmann [28] | Guatemala | 2020 | Review (no sample) | Range 10–19 | Bleeding, clotting disorders, and shock | 5.6 h |
| Yee-Seuret [29] | Guatemala | 2012 | 87 | 19 | Local pain and edema | No information |
| Maltez [30] | Guatemala | 1994 | 7377 | 15 | Hematuria and clotting alteration | Not specified |
| Letona [31] | Guatemala | 2012 | Mean of 849 | 25.2 | Local pain, edema, and bleeding | 5.6 h |
| Guerra Otero [32] | Guatemala | 2016 | Surveillance in 5 years | 24 | Local pain and edema | 3–8 h |
| Matute-Martínez [33] | Honduras | 2016 | 59 | 28 | Lower limb lesions and some infections | 5.4 h |
| Laínez Mejía [34] | Honduras | 2017 | 84 | 15 | Local pain and edema | Not specified |
| Izaguirre Gonzalez [35] | Honduras | 2014 | 36 | 15 | Local inflammation, GI disorders, local lesions, and hematological disorders | Not specified |
| Ponce Orellana [36] | Honduras | 2016 | 33 | 17 | Pleural effusion, hemothorax, and wound in right toe | Not specified |
| Pinto L.J. [37] | Honduras | 2019 | 1 (Case study) | Range: 11–35 | Edema, pain, and ecchymosis headache | Not specified |
| Cerrato Contreras [38] | Honduras | 1989 | 63 | 10.6 | Local inflammation, vomiting, shock, and clotting problems | Not specified |
| Cerna Rodríguez [39] | Honduras | 2023 | 42 | No reported | 3 deaths reported by informants | No data |
| Aleman [40] | Honduras | 2011 | 56 informants | Range 18–35 | Local lesions | No data |
| Flores | Honduras | 2019 | 62 | School age | Vascular damage, neurological manifestations, and myotoxic effects | No data |
| Lopez Ponce | Honduras | 1987 | 20 | 11–29 | Local, hemotoxic, and neurological | 3 h to several days |
| Fernandez | Central America | 2023 | Review several studies | 15 | Not specified | No data |
| Ministry of Health [42] | El Salvador | 2013 | 1130 cases in 5 years | 28 | Not specified | No data |
| Chirino Molina [43] | El Salvador | 2025 | 1472 | 10–30 | Not specified | No data |
| Gutiérrez J.M. [24] | El Salvador | 2014 | 1130 and 4 deaths | No information | Pathology study | No information |
| Fernandez P | Costa Rica | 2008 | 48 deaths | 29 years | Coagulation disorders, pain, edema, and local necrosis | 1–3 h |
| Sasa M. [45] | Costa Rica | 2020 | 475 | No relevant | Mentions bothropic manifestation in patients | No information |
| Montoya-Vargas [46] | Costa Rica | 2022 | 936 pharmacists in charge of antivenoms | Not included | Shock and hemorrhages | Not specified |
| Jutzy D.A. [47] | Panama | 1953 | 23 cases and 7 deaths | Not relevant | Bothropic manifestations (clotting, hemorrhagic, myotoxic, and edematogenic) | Not relevant |
| Vélez S.M. [48] | Panama | 2017 | Study of 76 Bothrops venom samples | Not Included | Local symptoms around the bite site and hemorrhages | 34 deaths reported |
| D A Warrell [49] | Panama | 2010 | Review of venoms in different regions | Not relevant | Effects: hemorrhagic, edema-forming, myotoxic, proteolytic, and defibrinating | In Costa Rica, this ranges from less than 1 h to >3 h |
| Otero-Patiño [50] | Panama | 2009 | Review of snake venoms in Central America | Not included | Not specified | |
| Pecchio [51] | Panama | 2018 | 390 | 28 | Pain, edema, paresthesia, and hemorrhages | |
| Uribe-Arjona | Panama | 2021 | 78 specimens of Bothrops asper | Not included | Cytotoxic, hemorrhagic, and neurotoxic effects | |
| Campbell [53] | Nicaragua | 2004 | Study of local venomous snakes compared to other areas in Americas | |||
| Hansson [54] | Nicaragua | 2010 | 56 | |||
| Moreno Avellano [55] | Nicaragua | 2000 | 72 | |||
| Gutiérrez J. M. [24] | Costa Rica and Central America | 2014 | 5300 bites for Central America |
References
- Harrison, R.A.; Casewell, N.R.; Ainsworth, S.A.; Lalloo, D.G. The time is now: A call for action to translate recent momentum on tackling tropical snakebite into sustained benefit for victims. Trans. R. Soc. Trop. Med. Hyg. 2019, 113, 835–838. [Google Scholar] [CrossRef]
- Chippaux, J.P. Incidence and mortality due to snakebite in the Americas. PLoS Negl. Trop. Dis. 2017, 11, e0005662. [Google Scholar] [CrossRef]
- Gutiérrez, J.M.; Calvete, J.J.; Habib, A.G.; Harrison, R.A.; Williams, D.J.; Warrell, D.A. Snakebite envenoming. Nat. Rev. Dis. Primers 2017, 3, 17063. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Snakebite Envenoming. 2023. Available online: https://www.who.int/news-room/fact-sheets/detail/snakebite-envenoming (accessed on 7 July 2025).
- Rubo, M.; Czuppon, P. How should we speak about years of life lost (YLL) values? Eur. J. Epidemiol. 2023, 38, 345–347. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bhaumik, S.; Zwi, A.B.; Norton, R.; Jagnoor, J. How and why snakebite became a global health priority: A policy analysis. BMJ Glob. Health 2023, 8, e011923. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- GBD 2019 Snakebite Envenomation Collaborators. Global mortality of snakebite envenoming between 1990 and 2019. Nat. Commun. 2022, 13, 6160. [Google Scholar] [CrossRef]
- Harrison, R.A.; Hargreaves, A.; Wagstaff, S.C.; Faragher, B.; Lalloo, D.G. Snake envenoming: A disease of poverty. PLoS Negl. Trop. Dis. 2009, 3, e569. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Russell, F.E.; Walter, F.G.; Bey, T.A.; Fernandez, M.C. Snakes and snakebite in Central America. Toxicon 1997, 35, 1469–1522. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, J.M. Understanding and confronting snakebite envenoming: The harvest of cooperation. Toxicon 2016, 109, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Neri-Castro, E.; Bénard-Valle, M.; Paniagua, D.; Boyer, L.V.; Possani, L.D.; López-Casillas, F.; Olvera, A.; Romero, C.; Zamudio, F.; Alagón, A. Neotropical Rattlesnake (Crotalus simus) Venom Pharmacokinetics in Lymph and Blood Using an Ovine Model. Toxins 2020, 12, 455. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jowers, M.J.; Smart, U.; Sánchez-Ramírez, S.; Murphy, J.C.; Gómez, A.; Bosque, R.J.; Sarker, G.C.; Noonan, B.P.; Faria, J.F.; Harris, D.J.; et al. Unveiling underestimated species diversity within the Central American Coralsnake, a medically important complex of venomous taxa. Sci. Rep. 2023, 13, 11674. [Google Scholar] [CrossRef]
- Guerra-Centeno, D. Ética sobre el envenenamiento por serpiente en el agro paisaje de Guatemala. Cienc. Tecnol. Salud 2015, 2, 65–73. [Google Scholar] [CrossRef]
- Fernández, C.E.A.; Youssef, P. Snakebites in the Americas: A Neglected Problem in Public Health. Curr. Trop. Med. Rep. 2024, 11, 19–27. [Google Scholar] [CrossRef]
- Alape-Girón, A.; Sanz, L.; Escolano, J.; Flores-Díaz, M.; Madrigal, M.; Sasa, M.; Calvete, J.J. Snake Venomics of the Lancehead Pitviper Bothrops asper: Geographic, Individual, and Ontogenetic Variations. J. Proteome Res. 2008, 7, 3556–3571. [Google Scholar] [CrossRef]
- Calvete, J.J.; Sanz, L.; Cid, P.; de la Torre, P.; Flores-Díaz, M.; Dos Santos, M.C.; Borges, A.; Bremo, A.; Angulo, Y.; Lomonte, B.; et al. Snake Venomics of the Central American Rattlesnake Crotalus simus and the South American Crotalus durissus Complex Points to Neurotoxicity as an Adaptive Paedomorphic Trend along Crotalus Dispersal in South America. J. Proteome Res. 2010, 9, 528–544. [Google Scholar] [CrossRef]
- Arroyo, C.; Solano, S.; Segura, A.; Herrera, M.; Estrada, R.; Villalta, M.; Vargas, M.; Gutiérrez, J.M.; Leon, G. Cross-reactivity and cross-immunomodulation between venoms of the snakes Bothrops asper, Crotalus simus and Lachesis stenophrys, and its effect in the production of polyspecific antivenom for Central America. Toxicon 2017, 138, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Hernández, R.; Cabalceta, C.; Saravia-Otten, P.; Chaves, A.; Gutiérrez, J.M.; Rucavado, A. Poor regenerative outcome after skeletal muscle necrosis induced by Bothrops asper venom: Alterations in microvasculature and nerves. PLoS ONE 2011, 6, e19834, Erratum in PLoS ONE 2011, 6, e19834. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gutiérrez, J.M.; Escalante, T.; Hernández, R.; Gastaldello, S.; Saravia-Otten, P.; Rucavado, A. Why is Skeletal Muscle Regeneration Impaired after Myonecrosis Induced by Viperid Snake Venoms? Toxins 2018, 10, 182. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gutiérrez, J.M. Snakebite envenomation in Central America. In Handbook of Venoms and Toxins of Reptiles; Mackessy, S.P., Ed.; CRC Press: Boca Raton, FL, USA, 2009; pp. 491–507. [Google Scholar]
- Gutiérrez, J.M. Current challenges for confronting the public health problem of snakebite envenoming in Central America. J. Venom. Anim. Toxins Incl. Trop. Dis. 2014, 20, 7. [Google Scholar] [CrossRef] [PubMed]
- Hessel, M.M.; McAninch, S.A. Coral Snake Toxicity. [Updated 13 March 2023]. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK519031/ (accessed on 20 May 2025).
- Ratanabanangkoon, K. Polyvalent Snake Antivenoms: Production Strategy and Their Therapeutic Benefits. Toxins 2023, 15, 517. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gutiérrez, J.M.; Arias-Rodríguez, J.; Alape-Girón, A. Envenenamiento Ofídico en Costa Rica: Logros y Tareas Pendientes. Acta Méd. Costarric. September 2020, Volume 62, pp. 102–108. Available online: http://www.scielo.sa.cr/scielo.php?script=sci_arttext&pid=S0001-60022020000300102&lng=en (accessed on 20 May 2025).
- Sant’Ana Malaque, C.M.; Gutiérrez, J.M. Snakebite Envenomation in Central and South America. In Critical Care Toxicology; Brent, J., Burkhart, K., Dargan, P., Hatten, B., Megarbane, B., Palmer, R., Eds.; Springer: Cham, Switzerland, 2015. [Google Scholar] [CrossRef]
- Giovannini, P.; Howes, M.R. Medicinal plants used to treat snakebite in Central America: Review and assessment of scientific evidence. J. Ethnopharmacol. 2017, 199, 240–256. [Google Scholar] [CrossRef]
- Available online: https://lovefm.com/boy-hospitalized-after-snake-bite-in-southern-belize/ (accessed on 20 May 2025).
- Wellmann, I.A.; Guerra-Centeno, D. Envenenamientos por mordedura de serpiente en Guatemala: Revisión de literatura. Cienc. Tecnol. Salud 2020, 7, 251–264. [Google Scholar] [CrossRef]
- Yee-Seuret, S.; Vargas-González, A.; Hernández-Torres, L. Mordeduras por Serpientes Venenosas en Guatemala. Revista Electrónica de Portales Medicos.com. 2012. Available online: https://www.revista-portalesmedicos.com/revista-medica/mordeduras-por-serpientes-venenosas-en-guatemala/ (accessed on 20 May 2025).
- Maltez, J.C. Accidente Ofídico: Estudio Retrospectivo, Clínico, Antropológico y Epidemiológico, Realizado en el Departamento de Guatemala, Región Sur, del 1 de enero de 1987 al 31 de Diciembre de 1992. Ph.D. Thesis, Universidad de San Carlos de Guatemala, Cdad. de Guatemala, Guatemala, 1994. [Google Scholar]
- Letona, C.A. Guía de Animales Ponzoñosos de Guatemala: Manejo del Paciente Intoxicado. Ph.D. Thesis, Universidad de San Carlos de Guatemala, Cdad. de Guatemala, Guatemala, 2012. [Google Scholar]
- Guerra-Centeno, D. Perfil epidemiológico del accidente ofídico en las tierras bajas de Guatemala. Cienc. Tecnol. Salud 2016, 3, 127–138. [Google Scholar] [CrossRef]
- Matute-Martínez, C.F.; Sánchez-Sierra, L.E.; Barahona-López, D.M.; LaínezMejía, J.L.; Matute-Martínez, F.J.; Perdomo-Vaquero, R. Caracterización de pacientes que sufrieron mordedura de serpiente, atendidos en Hospital Público de Juticalpa, Olancho. Rev. Fac. Cienc. Med. 2016, 13, 18–26. [Google Scholar]
- Laínez Mejía, J.L.; Barahona López, D.M.; Sánchez Sierra, L.E.; Matute Martínez, C.F.; Córdova Avila, C.N.; Perdomo Vaquero, R. Caracterización de pacientes con mordedura de serpiente atendidos en Hospital Tela, Atlantida—Characterization of patients with snake bite treated in Tela, Atlántida Hospital. Rev. Fac. Cienc. Méd. (Impr.) 2017, 14, 9–17. [Google Scholar]
- Izaguirre Gonzalez, A.I.; Matute-Martinez, C.F.; Barahona Lopez, D.M.; Sanchez-Sierra, L.E.; Perdomo-Vaquero, R. Clinical epidemiological characterization of snakebites at the Hospital Sta Teresa de Comayagua 2014–2015. Rev. Med. Hondur. 2017, 85, 21–26. [Google Scholar]
- Ponce Orellana, C.P. Caracterizacion Epidemiológica y Clinica de Pacientes con Envenenamiento por Mordedura de Serpiente en Pediatria de Enero 2015 a Junio 2016. Ph.D. Thesis, Universidad Nacional de Honduras, Tegucigalpa, Honduras, 2016. [Google Scholar]
- Pinto, L.J.; Lee Fernández, L.; Gutiérrez, J.M.; Simón, D.S.; Ceballos, Z.; Aguilar, L.F.; Sierra, M. Case Report: Hemothorax in Envenomation by the Viperid Snake Bothrops asper. Am. J. Trop. Med. Hyg. 2019, 100, 714–716. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cerrato Contreras, R.S. Mordeduras de Serpiente in Hospital Leonardo Martinez Valenzuela 1981–1985. Ph.D. Thesis, Universidad Nacional Autónoma de Honduras, Tegucigalpa, Honduras, 1989. [Google Scholar]
- Cerna Rodríguez, D.A. Características Epidemiológicas y Complicaciones Asociadas a Mordeduras de Serpiente en el Hospital Materno Infantil, Tegucigalpa. MDC. Honduras, en el Periodo Comprendido de Agosto 2018 a Septiembre 2019. Ph.D. Thesis, Universidad Nacional Autónoma de Nicaragua, Managua, Nicaragua, 2023. [Google Scholar]
- Aleman, B.; de Clerck, E.; Fenegan, B.; Casanoves, B.; Garcia, J. Caracterización de Reptiles y percepción local hacia las serpientes en la subcuenca del rio Copan, Honduras. Agroforesteria Am. 2011, 48, 103–117. [Google Scholar]
- Gutiérrez, J.M.; Castillo, L.; de Naves, K.M.D.; Masís, J.; Alape-Girón, A. Epidemiology of snakebites in El Salvador (2014–2019). Toxicon 2020, 186, 26–28. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Salud de El Salvador. Lineamientos Técnicos para la Prevención y Atención de Personas Mordidas por Serpiente; Ministerio de Salud: San Salvador, El Salvador, 2013; p. 40.
- Chirino Molina, W.Y.; Mendoza Rodríguez, E.W.; Gavidia Leiva, C.M. Epidemiology of venomous snake bites in El Salvador from 2011 to 2022. Alerta 2025, 8, 47–54. [Google Scholar] [CrossRef]
- Fernández, P.; Gutiérrez, J.M. Mortality due to snakebite envenomation in Costa Rica (1993–2006). Toxicon 2008, 52, 530–533. [Google Scholar] [CrossRef] [PubMed]
- Sasa, M.; Segura Cano, S.E. New insights into snakebite epidemiology in Costa Rica: A retrospective evaluation of medical records. Toxicon X 2020, 7, 100055. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Montoya-Vargas, W.; Gutiérrez, J.M.; Quesada-Morúa, M.S.; Morera-Huertas, J.; Rojas, C.; Leon-Salas, A. Preliminary assessment of antivenom availability and management in the public health system of Costa Rica: An analysis based on a survey to pharmacists in public health facilities. Toxicon X 2022, 16, 100139. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jutzy, D.A.; Biber, S.H.; Elton, N.W.; Lowry, E.C. A clinical and pathological analysis of snake bites on the Panama Canal Zone. Am. J. Trop. Med. Hyg. 1953, 2, 129–141. [Google Scholar] [CrossRef] [PubMed]
- Vélez, S.M.; Salazar, M.; Acosta de Patiño, H.; Gómez, L.; Rodriguez, A.; Correa, D.; Saldaña, J.; Navarro, D.; Lomonte, B.; Otero-Patiño, R.; et al. Geographical variability of the venoms of four populations of Bothrops asper from Panama: Toxicological analysis and neutralization by a polyvalent antivenom. Toxicon 2017, 132, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Warrell, D.A. Snake bite. Lancet 2010, 375, 77–88. [Google Scholar] [CrossRef]
- Otero-Patiño, R. Epidemiological, clinical and therapeutic aspects of Bothrops asper bites. Toxicon 2009, 54, 998–1011. [Google Scholar] [CrossRef]
- Pecchio, M.; Suárez, J.A.; Hesse, S.; Hersh, A.M.; Gundacker, N.D. Descriptive epidemiology of snakebites in the Veraguas province of Panama, 2007–2008. Trans. R. Soc. Trop. Med. Hyg. 2018, 112, 463–466, Erratum in Trans. R. Soc. Trop. Med. Hyg. 2019, 113, 845. [Google Scholar] [CrossRef] [PubMed]
- Uribe-Arjona, A.; Acosta-de-Patiño, H.; Martínez-Cortés, V.; Correa-Ceballos, D.; Rodríguez, A.; Gómez-Leija, L.; Vega, N.; Gutiérrez, J.-M.; Otero-Patiño, R. Toxicological, enzymatic, and immunochemical characterization of Bothrops asper (Serpentes: Viperidae) reference venom from Panama. Rev. Biol. Trop. 2021, 69, 127–138. [Google Scholar] [CrossRef]
- Campbell, J.A.; Lamar, W.W. The Venomous Reptiles of the Western Hemisphere; Comstock Publishing Associates: Ithaca, Greece; London, UK, 2004; pp. 870–1500. [Google Scholar]
- Hansson, E.; Cuadra, S.; Oudin, A.; de Jong, K.; Stroh, E.; Torén, K.; Albin, M. Mapping snakebite epidemiology in Nicaragua--pitfalls and possible solutions. PLoS Negl. Trop. Dis. 2010, 4, e896. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moreno Avellano, A.J. Manejo de las Mordeduras de Serpientes Venenosas en Pacientes Atendidos en el Servicio de Mediicina interna en el Hospital Escuela Oscar Danilo Rosales Arguello Durante el Periodo de Enero 1997–Noviembre 1999. Ph.D. Thesis, Universidad Nacional Autónoma de Nicaragua, Managua, Nicaragua, 2000. [Google Scholar]
- Funes, I.F.; Youssef, P.; Fernandez, E.A. Snakebites and their Impact on Disability. Med. Res. Arch. 2024, 1–1312. [Google Scholar] [CrossRef]
- Aglanu, L.M.; Amuasi, J.H.; Schut, B.A.; Steinhorst, J.; Beyuo, A.; Dari, C.D.; Agbogbatey, M.K.; Blankson, E.S.; Punguyire, D.; Lalloo, D.G.; et al. What the snake leaves in its wake: Functional limitations and disabilities among snakebite victims in Ghanaian communities. PLoS Negl. Trop. Dis. 2022, 16, e0010322. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sachett, A.; Strand, E.; Serrão-Pinto, T.; da Silva Neto, A.; Pinto Nascimento, T.; Rodrigues Jati, S.; Dos Santos Rocha, G.; Ambrósio Andrade, S.; Wen, F.H.; Berto Pucca, M.; et al. Capacity of community health centers to treat snakebite envenoming in indigenous territories of the Brazilian Amazon. Toxicon 2024, 241, 107681. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Country | Mortality 2019 Number of Individuals (Estimate) | Death Age Standardized Rate Per 100,000 in 2019 (DASR) | % of Change from 1990 to 2019 for DASR * | Years of Life Lost (YLLs) Age Standardized Rate Per 100,000 in 2019 | % Change 1990–2019 (YLL) ** |
|---|---|---|---|---|---|
| Guatemala | 10 (7.9–13) | 0.08 (0.06 to 0.10) | Increases [82%] | 2.97 (0.22 to 3.71) | Increase [47%] |
| El Salvador | 1.3 (<1–1.9) | 0.02 (0.1 to 0.03) | Increases [222%] | 0.88 (0.49 to 1.3) | Increase [150%] |
| Honduras | 5.3 (3.0–8.4) | 0.07 (0.04 to 0.12) | Decreases [53%] | 2.68 (1.59 to 4.33) | Increase [65%] |
| Nicaragua | 7.9 (4.9–10.0) | 0.15 (0.10 to 0.19) | Decreases [51%] | 5.95 (3.53 to 7.88) | Increase [57%] |
| Costa Rica | 3.9 (2.9–52) | 0.08 (0.06 to 0.10) | Decreases [20%] | 2.4 (1.75 to 3.24) | Decrease [23%] |
| Panama | 14 (11–19) | 0.35 (0.26 to 0.46) | Decreases [50%] | 14.96 (11.21 to 19.81) | Decrease [50%] |
| Belize | <1 (<1–1.1) | 0.27(0.22 to 0.33) | Increases [444%] | 10.38 (8.39 to 12.51) | Increase [372%] |
| Name of the Antivenom | Use for This Type of Venoms | Presentation | Commercialized in the Region | For use in This Type of Medical Facilities | Country of Production |
|---|---|---|---|---|---|
| Coral ICP | Most coral snakebites of Central America | Liquid | Yes | Hospitals | Costa Rica |
| Polival ICP | Most viperine bites venoms | Liquid | Yes | Hospitals | Costa Rica |
| Lyophilized Polivalent | Viperine bites | Lyophilized formulation | Yes | Hospitals | Costa Rica |
| Antivipmyn | Pit-viper bites (crotalids) | Liquid and lyophilized formulations | Yes | Hospitals | Mexico |
| Birmex | Viperine bites | Lyophilized formulation | Yes | Hospital | Mexico |
| Author | Country | Study Year(s) | # Cases | Mean Age (Years) | Common Symptoms | Time from Snakebite to Medical Facility | Main Snake Species Identified in the Study |
|---|---|---|---|---|---|---|---|
| Letona (2012) [31] | Guatemala | 2002–2010 | 7377 | 15 | Local pain, edema, bleeding | Not specified | B asper, C. simus, A mexicanus, M. nigrocinctus |
| Guerra-Otero (2016) [32] | Guatemala | 2008–2013 | 305 | 25.2 | Local pain, hemorrhages | 5–6 h | B. asper, C. simus, A. bilineatus, Micrurus sp. |
| Yee-Seuret (2012) [29] | Guatemala | 2008–2011 | 87 | 19 | Local pain, edema | Not specified | B. asper, C simus |
| Izaguirre Gonzalez (2014) [35] | Honduras | 2014–2015 | 36 | 15 | Local inflammation, Gastrointestinal (GI) disorders | Not specified time | C. simus, Micrurus sp, Botriechis marchi, B. nasutus, B. asper |
| Laínez Mejía (2017) [34] | Honduras | 2013–2015 | 84 | 28 | Local pain and edema | 5.4 h | B. asper, C. simus |
| Ponce Orellana (2016) [36] | Honduras | 2015–2016 | 33 | 15 | Local symptoms, GI, and hematological disorders | Not specified | B. asper, Micrurus spp. |
| Gutiérrez J.M. (2020) [41] | El Salvador | 2014–2019 | 1130 | 15 | Not specified | Not specified | C. simus |
| Chirino Molina (2025) [43] | El Salvador | 2011–2022 | 1472 | 28 | Not specified | Not specified | C. simus, Porthidium ophriomegas, Cerrophidium wilsoni |
| Fernandez P. (2008) [44] | Costa Rica | 1993–2006 | 48 defunction cases | No Info | Not specified | No information | B. asper |
| Sasa (2020) [45] | Costa Rica | 2012–2013 | 475 | 29 | Coagulation disorders, pain, edema and local necrosis | 1–3 h | B. asper, Micrurus sp. |
| Jutzy (1953) [47] | Panama | 1953 | 23 | No Info | Shock and hemorrhages | Not specified Report 7 deaths | Bothropa atrox |
| Pecchio (2019) [51] | Panama | 2007–2018 | 390 | No info | Local symptoms and hemorrhages | No information | Bothrops asper |
| Hansson (2010) [54] | Nicaragua | 2005–2009 | 56 | No info | No information | 34 deaths were reported | B. asper, C. simus |
| Moreno Avellano (2000) [55] | Nicaragua | 1997–1999 | 72 | 28 | Pain, edema, paresthesia, hemorrhages | 8 h | Crotalus durissus |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernandez, E.A.; Fernandez Funez, I.S. Snakebites in the Central American Region: More Government Attention Required. Trop. Med. Infect. Dis. 2025, 10, 225. https://doi.org/10.3390/tropicalmed10080225
Fernandez EA, Fernandez Funez IS. Snakebites in the Central American Region: More Government Attention Required. Tropical Medicine and Infectious Disease. 2025; 10(8):225. https://doi.org/10.3390/tropicalmed10080225
Chicago/Turabian StyleFernandez, Eduardo Alberto, and Ivan Santiago Fernandez Funez. 2025. "Snakebites in the Central American Region: More Government Attention Required" Tropical Medicine and Infectious Disease 10, no. 8: 225. https://doi.org/10.3390/tropicalmed10080225
APA StyleFernandez, E. A., & Fernandez Funez, I. S. (2025). Snakebites in the Central American Region: More Government Attention Required. Tropical Medicine and Infectious Disease, 10(8), 225. https://doi.org/10.3390/tropicalmed10080225





