Dirofilaria repens in the Spermatic Cord of a 5-Year-Old Boy: A Rare Pediatric Case in Italy
Abstract
1. Introduction
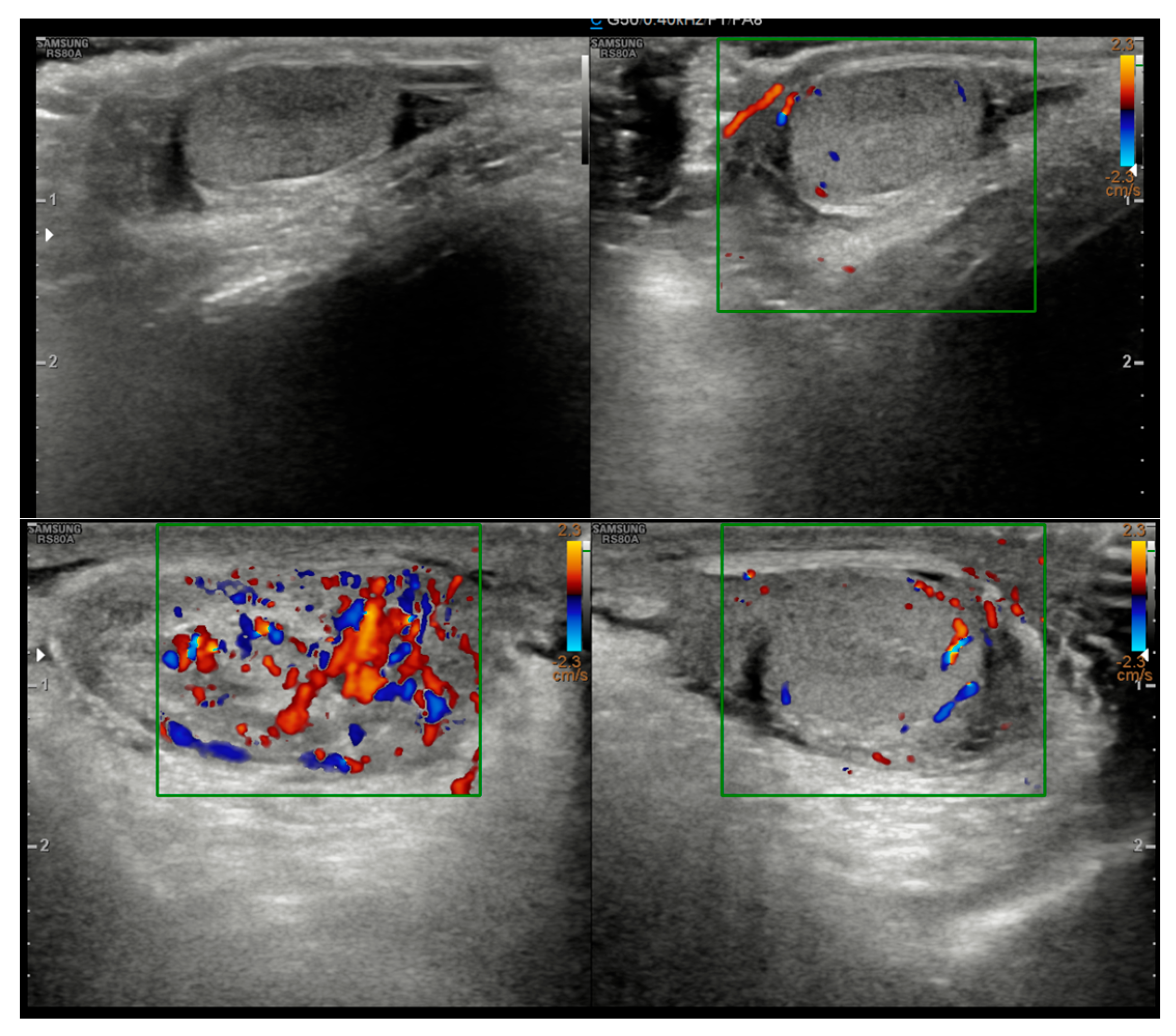
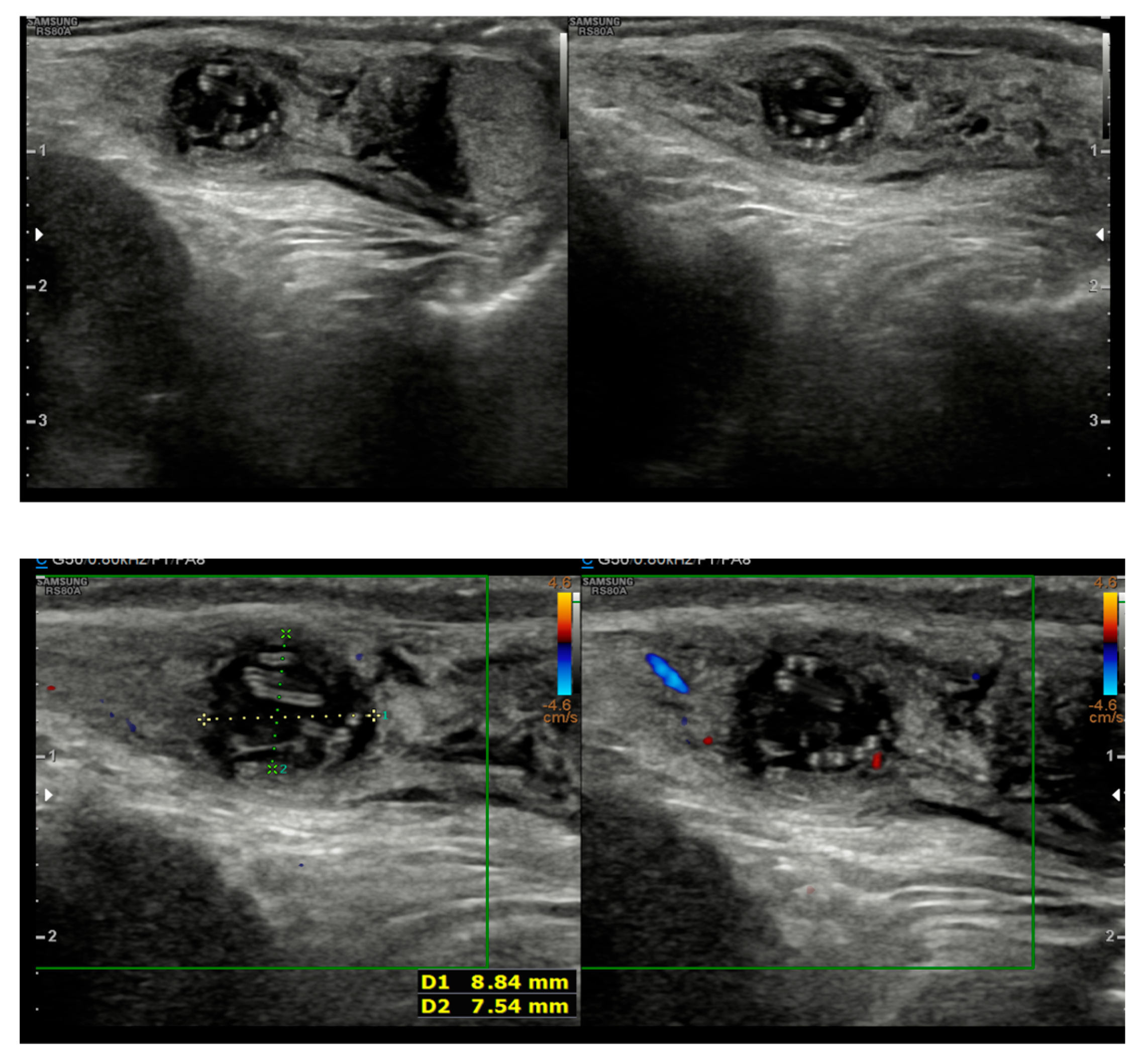
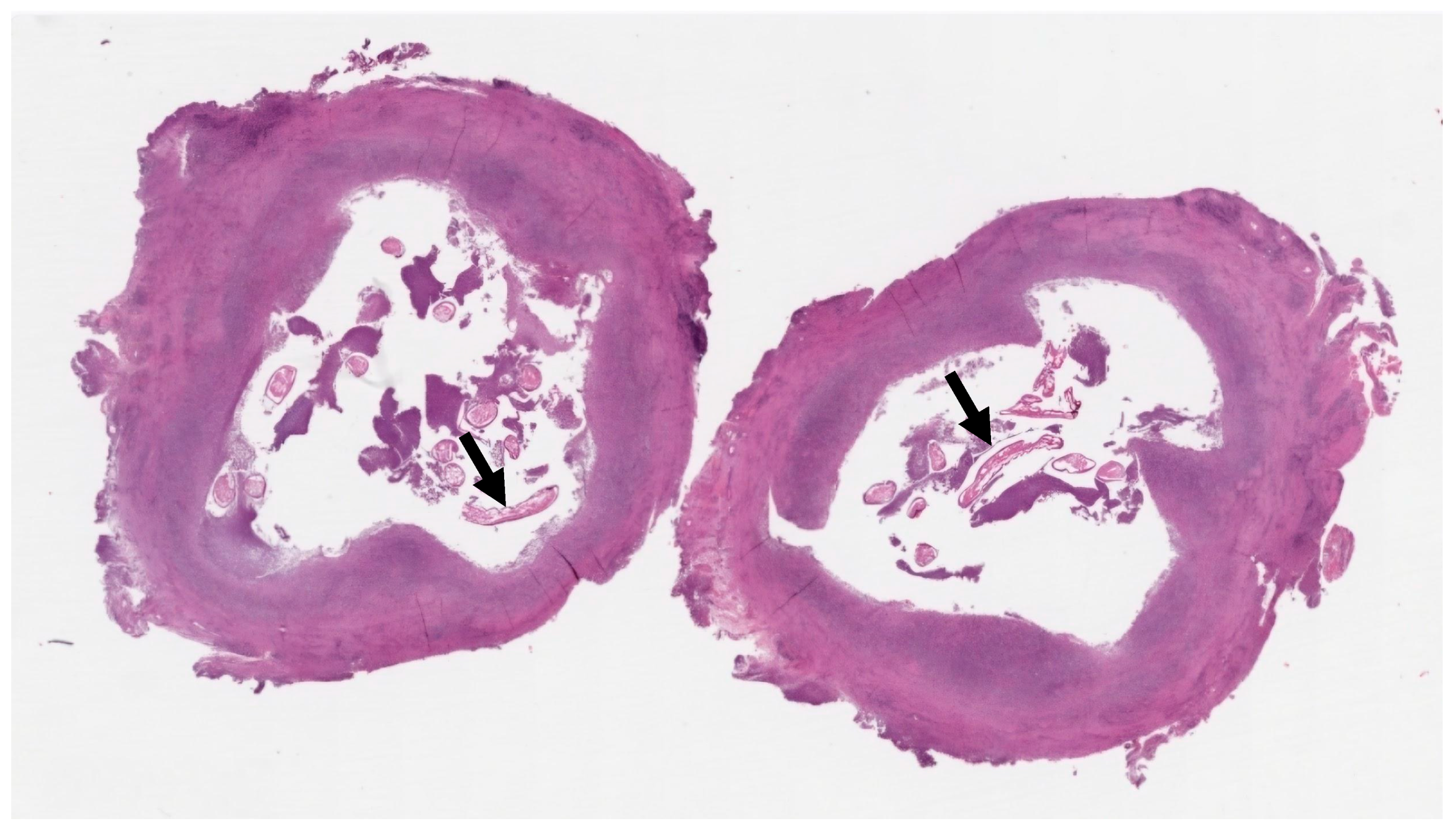
2. Case Presentation
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Capelli, G.; Genchi, C.; Baneth, G.; Bourdeau, P.; Brianti, E.; Cardoso, L.; Danesi, P.; Fuehrer, H.-P.; Giannelli, A.; Ionică, A.M.; et al. Recent advances on Dirofilaria repens in dogs and humans in Europe. Parasites Vectors 2018, 11, 663. [Google Scholar] [CrossRef] [PubMed]
- Simón, F.; López-Belmonte, J.; Marcos-Atxutegi, C.; Morchón, R.; Martín-Pacho, J. What is happening outside North America regarding human dirofilariasis? Veter. Parasitol. 2005, 133, 181–189. [Google Scholar] [CrossRef]
- Ugolini, S.; Lima, M.; Maffi, M.; Pierangeli, F.; Vastano, M.; Gargano, T.; Varani, S.; Gustinelli, A.; Caffara, M.; Fioravanti, M.L. Dirofilaria repens Testicular Infection in Child, Italy. Emerg. Infect. Dis. 2022, 28, 2569–2572. [Google Scholar] [CrossRef]
- Pampiglione, S.; Rivasi, F. Human Dirofilariasis Due to Dirofilaria (Nochtiella) Repens: An Update of World Literature from 1995 to 2000. 2000; 42, pp. 231–254. Available online: https://pubmed.ncbi.nlm.nih.gov/11686084/ (accessed on 20 June 2025).
- Sulekova, L.F.; Gabrielli, S.; De Angelis, M.; Milardi, G.L.; Magnani, C.; Di Marco, B.; Taliani, G.; Cancrini, G. Dirofilaria repens microfilariae from a human node fine-needle aspirate: A case report. BMC Infect. Dis. 2016, 16, 248. [Google Scholar] [CrossRef]
- Kallampallil, J.; Wood, S.J.; O’DEmpsey, T.; Craigie, R.J. Nematode infection mimicking paratesticular malignancy. BMJ Case Rep. 2013, 2013. [Google Scholar] [CrossRef]
- Rose, R.; Kleitsch, K.-U.; Born, D.; Heye, P. Dirofilaria repens in a Pediatric Patient—First Case Report from Switzerland. Eur. J. Pediatr. Surg. Rep. 2023, 11, e29–e31. [Google Scholar] [CrossRef]
- Latrofa, M.S.; Weigl, S.; Dantas-Torres, F.; Annoscia, G.; Traversa, D.; Brianti, E.; Otranto, D. A multiplex PCR for the simultaneous detection of species of filarioids infesting dogs. Acta Trop. 2012, 122, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Passavia, S.; Marino, F.; Bonanno, F.; Giangreco, V.; Reale, S. Human dirofilariosis diagnosis by specific DNA marker identification. Med. Pap. 2018, 4, 3–6. [Google Scholar]
- Ro, J.Y.; Tsakalakis, P.J.; White, V.A.; Luna, M.A.; Chang-Tung, E.G.; Green, L.; Cribbett, L.; Ayala, A.G. Pulmonary dirofilariasis: The great imitator of primary or metastatic lung tumor. A clinicopathologic analysis of seven cases and a review of the literature. Hum. Pathol. 1989, 20, 69–76. [Google Scholar] [CrossRef]
- Pampiglione, S.; Rivasi, F.; Angeli, G.; Boldorini, R.; Incensati, R.M.; Pastormerlo, M.; Pavesi, M.; Ramponi, A. Dirofilariasis due to Dirofilaria repens in Italy, an emergent zoonosis: Report of 60 new cases. Histopathology 2001, 38, 344–354. [Google Scholar] [CrossRef]
- Žulpaitė, R.; Patašius, A.; Drachneris, J. Dirofilariasis in Male Genitalia: A Case Report and Literature Review. Iran. J. Parasitol. 2024, 19, 358–365. [Google Scholar] [CrossRef] [PubMed]
- Saydam, F.N.; Erdem, H.; Ankarali, H.; Ramadan, M.E.E.-A.; El-Sayed, N.M.; Civljak, R.; Pshenichnaya, N.; Moroti, R.V.; Mahmuodabad, F.M.; Maduka, A.V.; et al. Vector-borne and zoonotic infections and their relationships with regional and socioeconomic statuses: An ID-IRI survey in 24 countries of Europe, Africa and Asia. Travel Med. Infect. Dis. 2021, 44, 102174. [Google Scholar] [CrossRef] [PubMed]
- Mendoza-Roldan, J.A.; Gabrielli, S.; Cascio, A.; Manoj, R.R.; Bezerra-Santos, M.A.; Benelli, G.; Brianti, E.; Latrofa, M.S.; Otranto, D. Zoonotic Dirofilaria immitis and Dirofilaria repens infection in humans and an integrative approach to the diagnosis. Acta Trop. 2021, 223, 106083. [Google Scholar] [CrossRef]
- Balendran, T.; Yatawara, L.; Wickramasinghe, S. Human Dirofilariasis Caused by Dirofilaria repens in Sri Lanka from 1962 to 2020. Acta Parasitol. 2022, 67, 628–639. [Google Scholar] [CrossRef] [PubMed]
- Pupić-Bakrač, A.; Pupić-Bakrač, J.; Beck, A.; Jurković, D.; Polkinghorne, A.; Beck, R. Dirofilaria repens microfilaremia in humans: Case description and literature review. One Health 2021, 13, 100306. [Google Scholar] [CrossRef]
- Supriaga, V.G.; Starkova, T.V.; Korotkova, G.I. Klinicheskiĭ i parazitologicheskiĭ diagnoz dirofiliarioza cheloveka [Clinical and parasitological diagnosis of human dirofilariasis]. Med. Parazitol. 2002, 1, 53–55. [Google Scholar]
- D’Amuri, A.; Senatore, S.A.; Carlà, T.G.; Floccari, F.; Villani, E.; Leocata, P.; Crisman, G. Cutaneous dirofilariasis resulting in orchiectomy. J. Cutan. Pathol. 2011, 39, 304–305. [Google Scholar] [CrossRef]
- Ahmed, N.; Tonelli, L.; Labagnara, G.; Doglioni, C.; Pedica, F. Subcutaneous dirofilariosis in Italy: A diagnostic hypothesis to remind when the anamnesis is misleading. Pathologica 2022, 114, 174–177. [Google Scholar] [CrossRef]
- Favia, G.; Lanfrancotti, A.; Della Torre, A.; Cancrini, G.; Coluzzi, M. Advances in the identification of Dirofilaria repens and Dirofilaria immitis by a PCR-based approach. Parassitologia 1997, 39, 401–402. [Google Scholar]
- Manzocchi, S.; Venco, L.; Piseddu, E.; Pantchev, N.; Masserdotti, C.; Bonfanti, U.; Albanese, F.; Kramer, L.H.; Bertazzolo, W. Positive PCR alone should not be considered sufficient to establish Dirofilaria repens as the cause of subcutaneous nodular lesions in the absence of a clear cytologic picture. Veter. Clin. Pathol. 2017, 46, 389–390. [Google Scholar] [CrossRef]
- Pampiglione, S.; Rivasi, F.; Gustinelli, A. Histopathology would like to thank the following reviewers for their help in 2008. Histopathology 2008, 53, 746–747. [Google Scholar] [CrossRef]
- Poppert, S.; Hodapp, M.; Krueger, A.; Hegasy, G.; Niesen, W.-D.; Kern, W.V.; Tannich, E. Dirofilaria repens Infection and Concomitant Meningoencephalitis. Emerg. Infect. Dis. 2009, 15, 1844–1846. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Franzò, A.; Marino, A.; Celesia, B.M.; Bruno, R.; Catalano, P.; Cacciaguerra, S.; Reale, S.; Cacopardo, B.S.; Nunnari, G. Dirofilaria repens in the Spermatic Cord of a 5-Year-Old Boy: A Rare Pediatric Case in Italy. Trop. Med. Infect. Dis. 2025, 10, 184. https://doi.org/10.3390/tropicalmed10070184
Franzò A, Marino A, Celesia BM, Bruno R, Catalano P, Cacciaguerra S, Reale S, Cacopardo BS, Nunnari G. Dirofilaria repens in the Spermatic Cord of a 5-Year-Old Boy: A Rare Pediatric Case in Italy. Tropical Medicine and Infectious Disease. 2025; 10(7):184. https://doi.org/10.3390/tropicalmed10070184
Chicago/Turabian StyleFranzò, Alessandro, Andrea Marino, Benedetto Maurizio Celesia, Roberto Bruno, Pieralba Catalano, Sebastiano Cacciaguerra, Stefano Reale, Bruno Santi Cacopardo, and Giuseppe Nunnari. 2025. "Dirofilaria repens in the Spermatic Cord of a 5-Year-Old Boy: A Rare Pediatric Case in Italy" Tropical Medicine and Infectious Disease 10, no. 7: 184. https://doi.org/10.3390/tropicalmed10070184
APA StyleFranzò, A., Marino, A., Celesia, B. M., Bruno, R., Catalano, P., Cacciaguerra, S., Reale, S., Cacopardo, B. S., & Nunnari, G. (2025). Dirofilaria repens in the Spermatic Cord of a 5-Year-Old Boy: A Rare Pediatric Case in Italy. Tropical Medicine and Infectious Disease, 10(7), 184. https://doi.org/10.3390/tropicalmed10070184






