Bacterial Pathogens and Antibiotic Resistance in Bloodstream Infections in Tunisia: A 13-Year Trend Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Study Setting
- General setting
- Specific setting: AMR surveillance network
2.4. Bacterial Species Identification and Antimicrobial Susceptibility Testing
2.5. Recording and Reporting System
2.6. Data Collection and Variables
- -
- E. cloacae, K. pneumoniae: Amoxicillin-clavulanic acid (AMC), cefotaxime (CTX), gentamicin (GEN), amikacin (AMK), imipenem (IMP), ertapenem (ERT), and ciprofloxacin (CIP).
- -
- S. aureus: Cefoxitin (FOX), GEN, AMK, ofloxacin (OFL), vancomycin (VAN), and linezolid (LIN).
- -
- E. faecium: Ampicillin (AMP), gentamicin high-charged (GHC), VAN, LIN, and tigecycline (TIG).
- -
- P. aeruginosa and A. baumannii: Piperacillin–tazobactam (PTZ), ceftazidime (CAZ), GEN, IMP, CIP, and AMK.
2.7. Data Analysis
3. Results
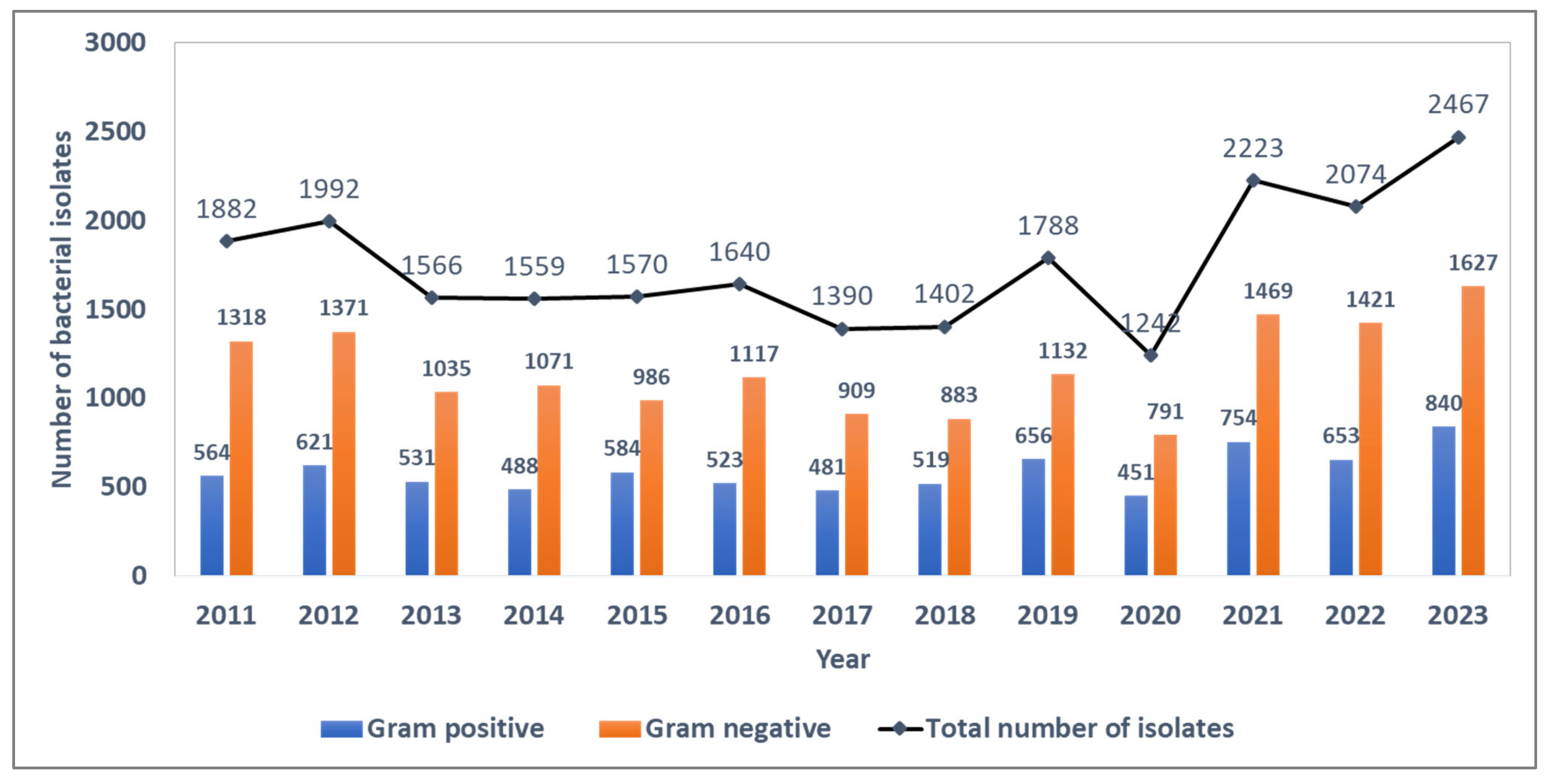
3.1. Trends in Bacterial Isolates
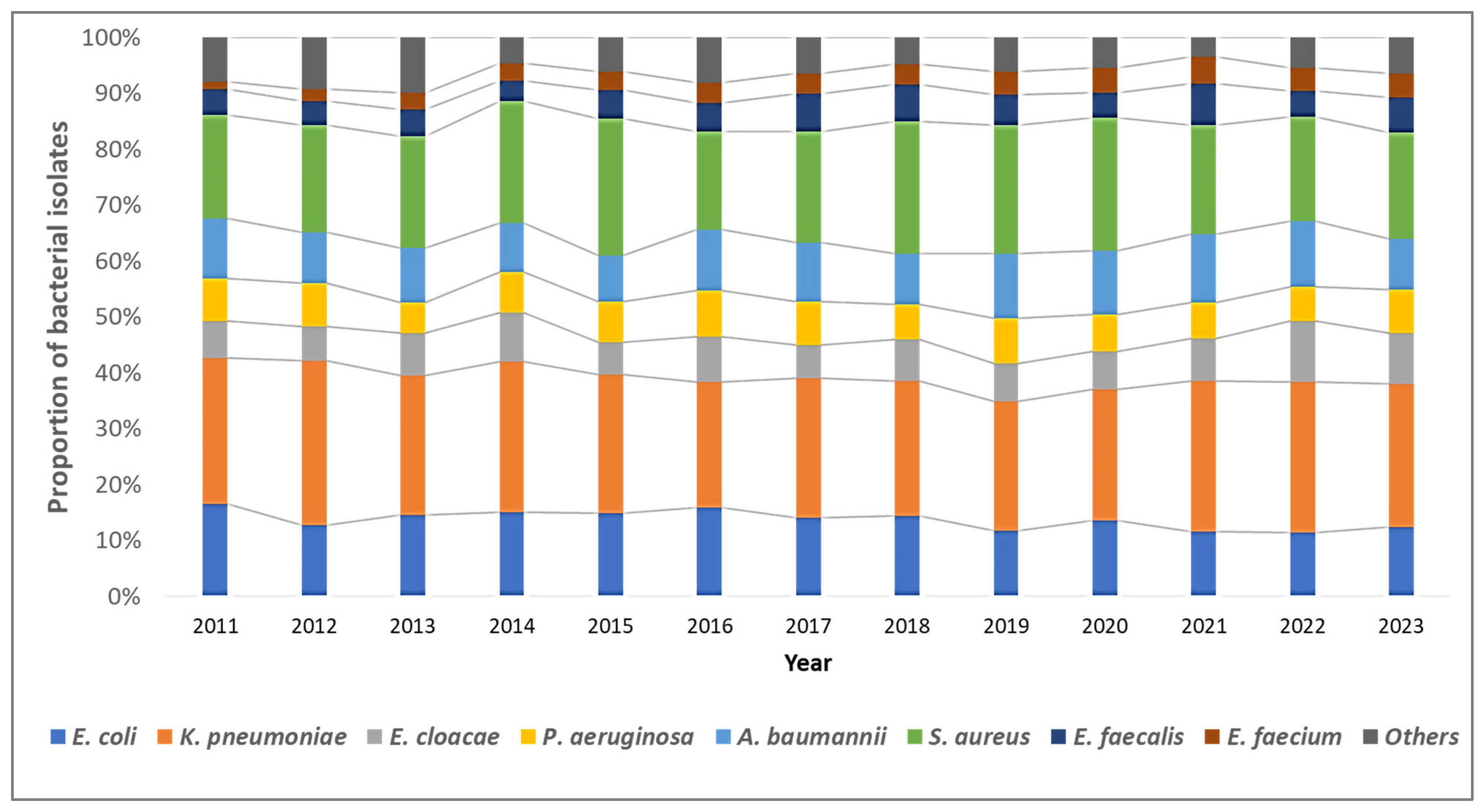
3.2. Trends in Distribution of Bacterial Pathogens
3.3. Patterns of Antibiotic Resistance and Their Trends
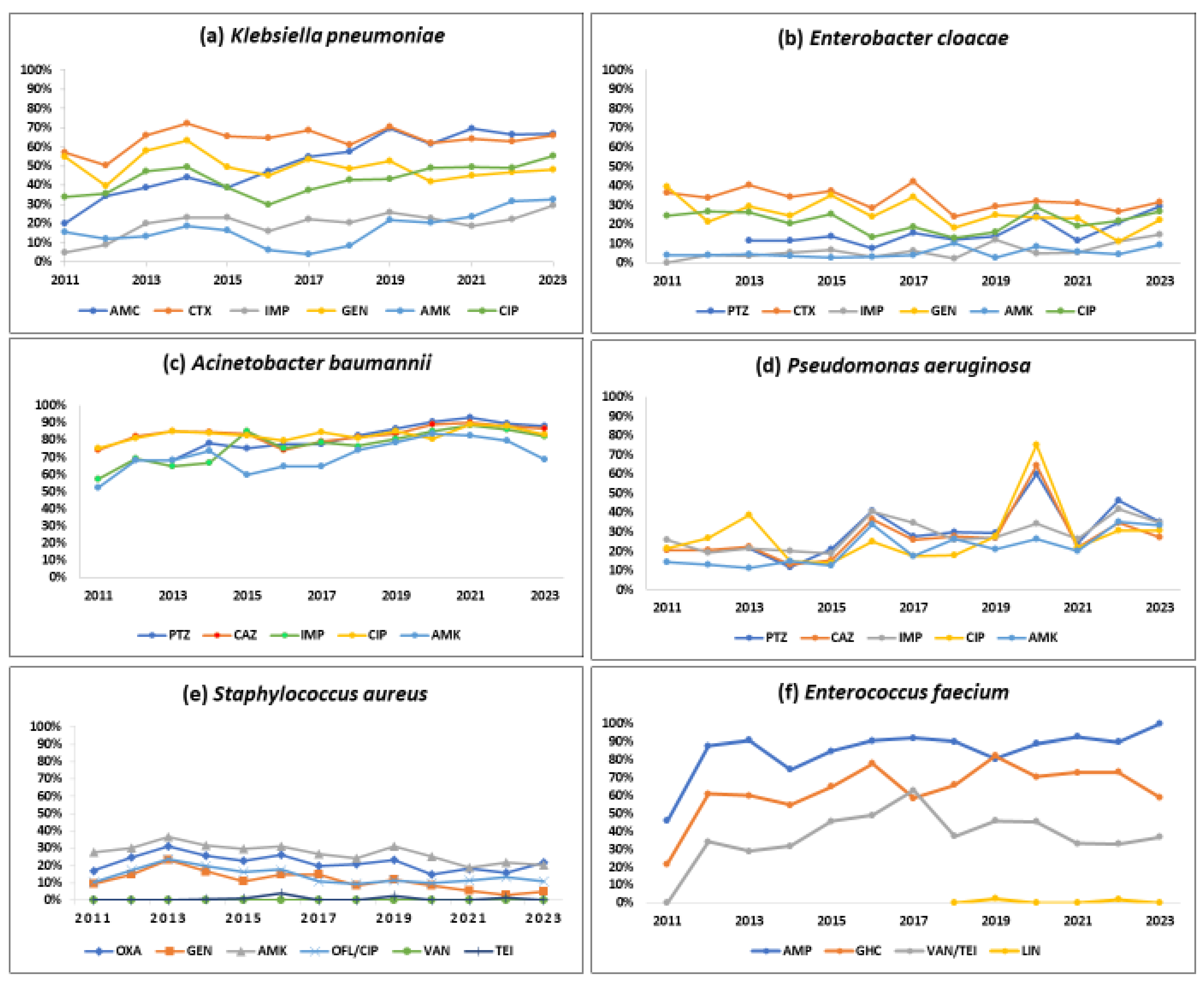
3.3.1. Klebsiella pneumoniae
3.3.2. Enterobacter cloacae
3.3.3. Acinetobacter baumannii
3.3.4. Pseudomonas aeruginosa
3.3.5. Stapylococcus aureus
3.3.6. Enterococcus faecium
3.3.7. Other Specific AMR Phenotypes
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AMR | Antimicrobial resistance |
| AMC | Amoxicillin-clavulanic acid |
| AMK | Amikacin |
| AMP | Ampicillin |
| BSI | Bloodstream infections |
| CIP | Ciprofloxacin |
| CRE | Carbapenem-resistant Enterobacterales |
| CRAB | Carbapenem-resistant A. baumannii |
| CTX | Cefotaxime |
| CAZ | Ceftazidime |
| ERT | Ertapenem |
| DALYs | Disability-Adjusted Life Years |
| ESKAPE | E. cloacae, S. aureus, K. pneumoniae, A. baumannii, P. aeruginosa, E. faecium |
| FOX | Cefoxitin |
| GEN | Gentamicin |
| GHC | Gentamicin high-charged |
| GLASS | Global Antimicrobial Resistance and Use Surveillance System |
| ICU | Intensive care unit |
| IMP | Imipenem |
| LART | L’Antibiorésistance en Tunisie |
| LIN | Linezolid |
| LIS | Laboratory information system |
| MDR | Multidrug resistant |
| MENA | Middle East and North Africa |
| MRSA | Methicillin-resistant S. aureus |
| OFL | Ofloxacin |
| PTZ | Piperacillin–tazobactam |
| TIG | Tigecycline |
| 3GC | Third-generation cephalosporin |
| 3GCREB | Third-generation cephalosporin-resistant Enterobacterales |
| VAN | Vancomycin |
| VRE | Vancomycin-resistant Enterococci |
| WHO | World Health Organization |
References
- Stewardson, A.J.; Allignol, A.; Beyersmann, J.; Graves, N.; Schumacher, M.; Meyer, R.; Tacconelli, E.; De Angelis, G.; Farina, C.; Pezzoli, F.; et al. The health and economic burden of bloodstream infections caused by antimicrobial-susceptible and non-susceptible Enterobacteriaceae and Staphylococcus aureus in European hospitals, 2010 and 2011: A multicentre retrospective cohort study. Eurosurveillance 2016, 21, 30319. [Google Scholar] [CrossRef] [PubMed]
- WHO Publishes List of Bacteria for Which New Antibiotics Are Urgently Needed. Available online: https://www.who.int/news/item/27-02-2017-who-publishes-list-of-bacteria-for-which-new-antibiotics-are-urgently-needed (accessed on 26 November 2023).
- Marchello, C.S.; Dale, A.P.; Pisharody, S.; Rubach, M.P.; Crump, J.A. A Systematic Review and Meta-analysis of the Prevalence of Community-Onset Bloodstream Infections among Hospitalized Patients in Africa and Asia. Antimicrob. Agents Chemother. 2019, 64, e01974-19. [Google Scholar] [CrossRef] [PubMed]
- Diekema, D.J.; Hsueh, P.-R.; Mendes, R.E.; Pfaller, M.A.; Rolston, K.V.; Sader, H.S.; Jones, R.N. The Microbiology of Bloodstream Infection: 20-Year Trends from the SENTRY Antimicrobial Surveillance Program. Antimicrob. Agents Chemother. 2019, 63, e00355-19. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Ikuta, K.S.; Sharara, F.; Swetschinski, L.; Aguilar, G.R.; Gray, A.; Han, C.; Bisignano, C.; Rao, P.; Wool, E.; et al. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Naghavi, M.; Vollset, S.E.; Ikuta, K.S.; Swetschinski, L.R.; Gray, A.P.; E Wool, E.; Aguilar, G.R.; Mestrovic, T.; Smith, G.; Han, C.; et al. Global burden of bacterial antimicrobial resistance 1990–2021: A systematic analysis with forecasts to 2050. Lancet 2024, 404, 1199–1226. [Google Scholar] [CrossRef]
- Talaat, M.; Zayed, B.; Tolba, S.; Abdou, E.; Gomaa, M.; Itani, D.; Hutin, Y.; Hajjeh, R. Increasing Antimicrobial Resistance in World Health Organization Eastern Mediterranean Region, 2017–2019. Emerg. Infect. Dis. 2022, 28, 717–724. [Google Scholar] [CrossRef]
- Thomsen, J.; Abdulrazzaq, N.M.; Alrand, H.; Everett, D.B.; Senok, A.; Menezes, G.A.; Ayoub Moubareck, C. Epidemiology and antimicrobial resistance trends of Acinetobacter species in the United Arab Emirates: A retrospective analysis of 12 years of national AMR surveillance data. Front. Public Health 2024, 11, 1245131. [Google Scholar] [CrossRef]
- Zha, L.; Li, S.; Guo, J.; Hu, Y.; Pan, L.; Wang, H.; Zhou, Y.; Xu, Q.; Lu, Z.; Kong, X.; et al. Global and regional burden of bloodstream infections caused by carbapenem-resistant Gram-negative bacteria in 2019: A systematic analysis from the MICROBE database. Int. J. Infect. Dis. 2025, 153, 107769. [Google Scholar] [CrossRef]
- Browne, A.J.; Chipeta, M.G.; Haines-Woodhouse, G.; A Kumaran, E.P.; Hamadani, B.H.K.; Zaraa, S.; Henry, N.J.; Deshpande, A.; Reiner, R.C.; Day, N.P.J.; et al. Global antibiotic consumption and usage in humans, 2000–2018: A spatial modelling study. Lancet Planet Health 2021, 5, e893–e904. [Google Scholar] [CrossRef]
- World Health Organization. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report 2022. Available online: https://www.who.int/publications/book-orders (accessed on 26 November 2023).
- Comité de l’Antibiograme de la Société Française de Microbiologie. Available online: https://www.sfm-microbiologie.org/categorie-produit/livres/ (accessed on 26 November 2023).
- Saïdani, M.; Boutiba, I.; Ghozzi, R.; Kammoun, A.; Redjeb, S.B. Communication brève Profil bactériologique des bactériémies à germes multirésistants à l’hôpital Charles-Nicolle de Tunis Bacteriologic profile of bacteremia due to multi-drug resistant bacteria at Charles-Nicolle hospital of Tunis. Médecine Mal. Infect. 2006, 36, 163–166. [Google Scholar] [CrossRef]
- Mellouli, A.; Chebbi, Y.; El Fatmi, R.; Raddaoui, A.; Lakhal, A.; Torjmane, L.; Abdeljelil, N.B.; Belloumi, D.; Ladeb, S.; Othmen, T.B. Multidrug resistant bacteremia in hematopoietic stem cell transplant recipients Bactériémies à bactéries multirésistantes chez les greffés de cellules souches-hématopoïétiques. Tunis Med. 2021, 99, 269–276. [Google Scholar] [PubMed]
- Bertagnolio, S.; Dobreva, Z.; Centner, C.M.; Olaru, I.D.; Donà, D.; Burzo, S.; Huttner, B.D.; Chaillon, A.; Gebreselassie, N.; Wi, T.; et al. WHO global research priorities for antimicrobial resistance in human health. Lancet Microbe 2024, 5, 100902. [Google Scholar] [CrossRef] [PubMed]
- Brayek, A.; Bouguerra, H. Carte Sanitaire Tunisie 2021. Available online: https://santetunisie.rns.tn/fr/carte-sanitaire/carte-sanitaire-2011 (accessed on 26 November 2023).
- EUCAST: European Committee of Antimicrobial Susceptbility Testing. Available online: https://www.eucast.org (accessed on 26 November 2023).
- Dziri, R.; El Kara, F.; Barguellil, F.; Ouzari, H.-I.; El Asli, M.S.; Klibi, N. Vancomycin-Resistant Enterococcus faecium in Tunisia: Emergence of Novel Clones. Microb. Drug Resist. 2019, 25, 469–474. [Google Scholar] [CrossRef]
- Antimicrobial Resistance in the EU/EEA (EARS-Net)-Annual Epidemiological Report for 2021. Available online: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2021 (accessed on 29 November 2023).
- Lester, R.; Musicha, P.; van Ginneken, N.; Dramowski, A.; Hamer, D.H.; Garner, P.; A Feasey, N. Prevalence and outcome of bloodstream infections due to third-generation cephalosporin-resistant Enterobacteriaceae in sub-Saharan Africa: A systematic review. J. Antimicrob. Chemother. 2019, 75, 492–507. [Google Scholar] [CrossRef]
- Ma, C.; McClean, S. Mapping global prevalence of Acinetobacter baumannii and recent vaccine development to tackle it. Vaccines 2021, 9, 570. [Google Scholar] [CrossRef]
- Abukhalil, A.; Barakat, S.; Mansour, A.; Al-Shami, N.; Naseef, H. ESKAPE Pathogens: Antimicrobial Resistance Patterns, Risk Factors, and Outcomes a Retrospective Cross-Sectional Study of Hospitalized Patients in Palestine. Infect. Drug Resist. 2024, 17, 3813–3823. [Google Scholar] [CrossRef]
- Itani, R.; Khojah, H.M.J.; Karout, S.; Rahme, D.; Hammoud, L.; Awad, R.; Abu-Farha, R.; Mukattash, T.L.; Raychouni, H.; El-Lakany, A. Acinetobacter baumannii: Assessing susceptibility patterns, management practices, and mortality predictors in a tertiary teaching hospital in Lebanon. Antimicrob. Resist. Infect. Control 2023, 12, 136. [Google Scholar] [CrossRef]
- Bandy, A.; Almaeen, A.H. Pathogenic spectrum of blood stream infections and resistance pattern in Gram negative bacteria from Aljouf region of Saudi Arabia. PLoS ONE 2020, 15, e0233704. [Google Scholar] [CrossRef]
- Surveillance of Antimicrobial Resistance in Europe, 2023 Data: Executive Summary. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/antimicrobial-resistance-ECDC-WHO-executive-summary-2023-data.pdf (accessed on 29 November 2024).
- Rolain, J.-M.; Abat, C.; Brouqui, P.; Raoult, D. Worldwide decrease in methicillin-resistant Staphylococcus aureus: Do we understand something? Clin. Microbiol. Infect. 2015, 21, 515–517. [Google Scholar] [CrossRef]
- Thomsen, J.; Abdulrazzak, N.M.; AlRand, H.; Menezes, G.A.; Moubareck, C.A.; Everett, D.B.; Senok, A.; Podbielski, A. Epidemiology of vancomycin-resistant enterococci in the United Arab Emirates: A retrospective analysis of 12 years of national AMR surveillance data. Front. Public Health 2023, 11, 1275778. [Google Scholar] [CrossRef]
- Moemen, D.; Tawfeek, D.; Badawy, W. Healthcare-associated vancomycin resistant Enterococcus faecium infections in the Mansoura University Hospitals intensive care units. Egypt. Braz. J. Microbiol. 2015, 46, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Surveillance Atlas of Infectious Diseases. Available online: https://www.ecdc.europa.eu/en/surveillance-atlas-infectious-diseases (accessed on 29 November 2023).
- O’Toole, R.F.; Leong, K.W.; Cumming, V.; Van Hal, S.J. Vancomycin-resistant Enterococcus faecium and the emergence of new sequence types associated with hospital infection. Res. Microbiol. 2023, 174, 104046. [Google Scholar] [CrossRef] [PubMed]
- Ayobami, O.; Brinkwirth, S.; Eckmanns, T.; Markwart, R. Antibiotic resistance in hospital-acquired ESKAPE-E infections in low- and lower-middle-income countries: A systematic review and meta-analysis. Emerg. Microbes Infect. 2022, 11, 443–451. [Google Scholar] [CrossRef] [PubMed]
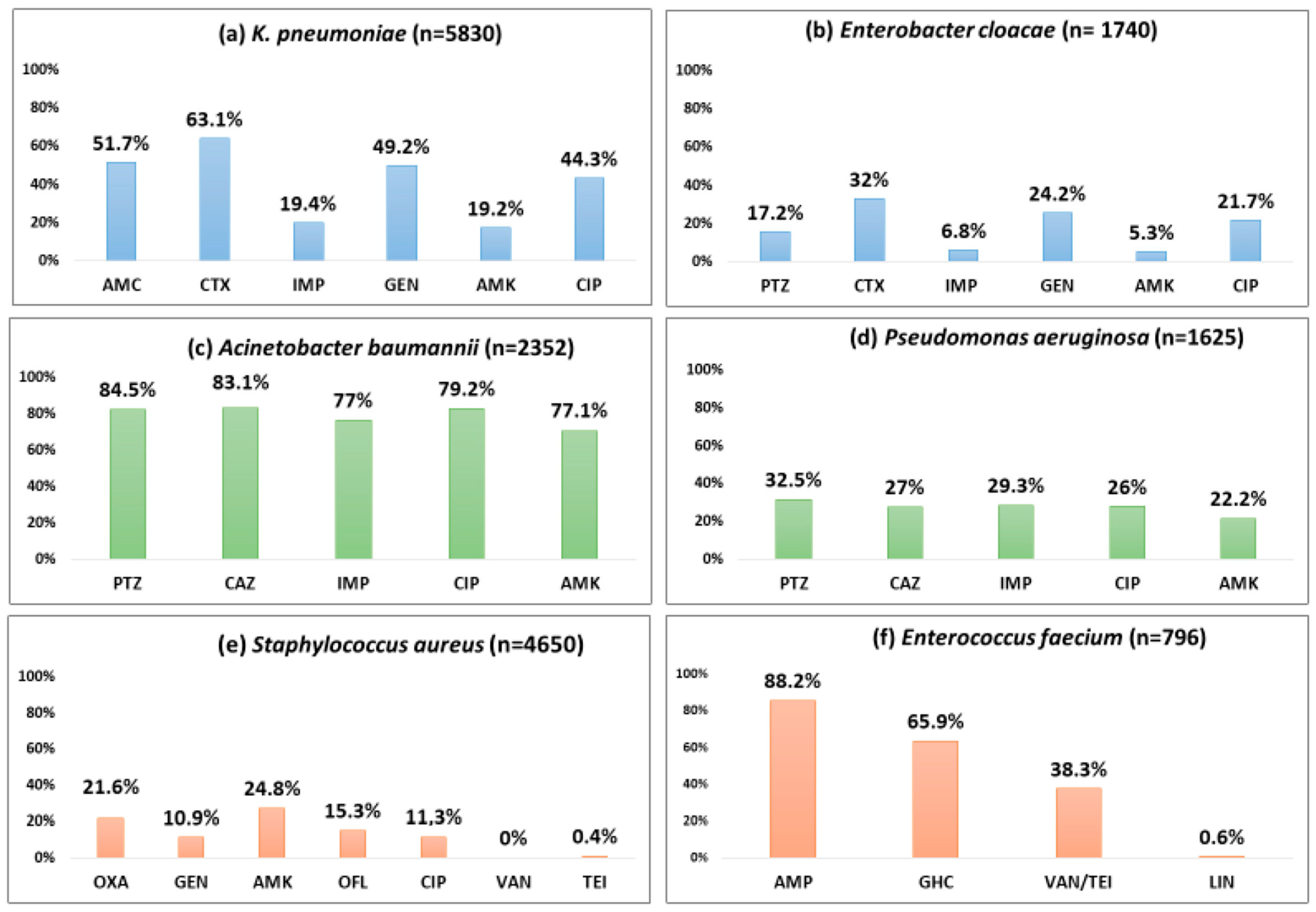
| (a) | |||||
| Antibiotics | K. pneumoniae (n = 5830) | E. cloacae (n = 1740) | A. baumannii (n = 2352) | P. aeruginosa (n = 1625) | |
| AMC | T | 5170 | NA | NA | NA |
| R | 2675 | NA | NA | NA | |
| % | 51.7 | NA | NA | NA | |
| PTZ | T | - | 1235 | 1521 | 1229 |
| R | - | 212 | 1286 | 399 | |
| % | - | 17.2 | 84.5 | 32.5 | |
| CTX | T | 5207 | 1638 | NA | NA |
| R | 3284 | 524 | NA | NA | |
| % | 63.1 | 32 | NA | NA | |
| CAZ | T | 5207 | - | 2023 | 1535 |
| R | 3191 | - | 1688 | 414 | |
| % | 61.3 | - | 83.4 | 27 | |
| IMP | T | 5089 | 1638 | 2145 | 1564 |
| R | 990 | 111 | 1651 | 458 | |
| % | 19.4 | 6.8 | 77 | 29.3 | |
| ERT | T | 5117 | 1625 | NA | NA |
| R | 1394 | 197 | NA | NA | |
| % | 27.2 | 36.7 | NA | NA | |
| GEN | T | 4777 | 1488 | 2350 | 1405 |
| R | 2353 | 360 | 1799 | 393 | |
| % | 49.2 | 24.2 | 76.5 | 28 | |
| AMK | T | 5427 | 1631 | 2080 | 1529 |
| R | 1041 | 86 | 1480 | 341 | |
| % | 19.2 | 5.3 | 71.1 | 22.2 | |
| CIP | T | 4966 | 1615 | 2010 | 1533 |
| R | 2199 | 350 | 1671 | 397 | |
| % | 44.3 | 21.7 | 79.2 | 26 | |
| (b) | |||||
| Antibiotics | S. aureus (n = 4650) | E. faecium (n = 796) | |||
| OXA | T | 4515 | NA | ||
| R | 975 | NA | |||
| % | 21.6 | NA | |||
| AMP | T | - | 761 | ||
| R | - | 671 | |||
| % | - | 88.2 | |||
| GEN | T | 4056 | 719 | ||
| R | 444 | 474 | |||
| % | 10.9 | 65.9 * | |||
| AMK | T | 3967 | - | ||
| R | 986 | - | |||
| % | 24.8 | - | |||
| OFL ** | T | 2875 | - | ||
| R | 441 | - | |||
| % | 15.3 | - | |||
| CIP | T | 1175 | - | ||
| R | 133 | - | |||
| % | 11.3 | - | |||
| VAN | T | 2011 | 768 | ||
| R | 0 | 294 | |||
| % | 0 | 38.3 | |||
| TEI | T | 2013 | 768 | ||
| R | 8 | 294 | |||
| % | 0.4 | 38.3 | |||
| LIN | T | 3770 | 353 | ||
| R | 0 | 2 | |||
| % | 0 | 0.6 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kanzari, L.; Ferjani, S.; Meftah, K.; Zribi, M.; Mezghani, S.; Ferjani, A.; Chebbi, Y.; Hamdoun, M.; Rhim, H.; Kadri, Y.; et al. Bacterial Pathogens and Antibiotic Resistance in Bloodstream Infections in Tunisia: A 13-Year Trend Analysis. Trop. Med. Infect. Dis. 2025, 10, 164. https://doi.org/10.3390/tropicalmed10060164
Kanzari L, Ferjani S, Meftah K, Zribi M, Mezghani S, Ferjani A, Chebbi Y, Hamdoun M, Rhim H, Kadri Y, et al. Bacterial Pathogens and Antibiotic Resistance in Bloodstream Infections in Tunisia: A 13-Year Trend Analysis. Tropical Medicine and Infectious Disease. 2025; 10(6):164. https://doi.org/10.3390/tropicalmed10060164
Chicago/Turabian StyleKanzari, Lamia, Sana Ferjani, Khaoula Meftah, Mariem Zribi, Sonda Mezghani, Asma Ferjani, Yosra Chebbi, Manel Hamdoun, Hajer Rhim, Yosr Kadri, and et al. 2025. "Bacterial Pathogens and Antibiotic Resistance in Bloodstream Infections in Tunisia: A 13-Year Trend Analysis" Tropical Medicine and Infectious Disease 10, no. 6: 164. https://doi.org/10.3390/tropicalmed10060164
APA StyleKanzari, L., Ferjani, S., Meftah, K., Zribi, M., Mezghani, S., Ferjani, A., Chebbi, Y., Hamdoun, M., Rhim, H., Kadri, Y., Frigui, S., Mhiri, E., Ghariani, A., Ben Ayed, N., Mahjoubi, F., Ben Lamine, Y., Kaoual, S., Mnif, B., Naija, H., ... Boutiba-Ben Boubaker, I. (2025). Bacterial Pathogens and Antibiotic Resistance in Bloodstream Infections in Tunisia: A 13-Year Trend Analysis. Tropical Medicine and Infectious Disease, 10(6), 164. https://doi.org/10.3390/tropicalmed10060164







