1. Introduction
Virtual reality focuses on simulating users’ physical presence within fully virtual environments generated by computational units, which users perceive as real through head-mounted devices due to their immersive and interactive nature as well as to the psychological and social aspects involved [
1,
2,
3]. Due to its nature, and the fact that the required hardware and software is becoming more widely available [
4], virtual reality is being applied in various domains, including education, training, entertainment, industry, manufacturing, healthcare, etc. Specifically, its use in the field of education has yielded several positive results, including more engaging and personalized learning, better learning outcomes, improved learners’ affective states, and unique learning environments that promote experiential learning [
5,
6]; hence, the research surrounding its adoption in educational contexts is increasing [
7,
8] as these benefits can influence several educational subjects, such as biology, chemistry, mathematics, physics, etc. Recent studies have indicated that by using virtual reality across educational levels and subjects, positive learning outcomes can be yielded [
9], more personalized learning experiences [
10] and more engaging and interactive learning environments can be created [
11], and students’ affective domain can be positively influenced [
12]. As a result, meaningful learning can be accomplished [
13].
Furthermore, given the capabilities of virtual reality to support learning [
14], emphasis is being placed on how it can affect students’ knowledge acquisition and practical skills development [
15]. When appropriately designed following a student-centered approach [
16], virtual reality learning experiences through immersive and secure learning environments where students can develop their skills, can be created [
17,
18]. These immersive environments offer personalized and adaptive experiences according to the needs and requirements of each individual [
19]. Studies have also disclosed the impact that virtual reality as a technology can have on the medical and healthcare domain [
20,
21,
22]. As a result, the interest surrounding its use in these domains is increasing. Recent studies explored using virtual reality in healthcare education [
23], medical education [
24,
25], nursing education [
26], as well as patient education [
27], revealing the transformative and positive influence that the adoption of virtual reality can have. Additionally, studies have demonstrated the effectiveness of utilizing virtual reality as a learning means to train healthcare and medical students and professionals [
28] as it can aid in them developing both technical and non-technical skills [
29].
Moreover, a scoping review by van der Kruk et al. [
30] highlighted the role of virtual reality as an effective patient education tool in healthcare, improving understanding and engagement. Meta-analyses and systematic reviews by Kyaw et al. [
31], Jiang et al. [
32], Kim et al. [
33], and Liu et al. [
34] revealed the effectiveness of utilizing virtual reality in medical and nursing education, showing improvements in clinical skills, procedural training, and knowledge retention compared with traditional methods. Choi et al. [
35] further emphasized the impact of virtual reality on nursing education, particularly on fostering critical thinking, knowledge acquisition, and decision-making in simulated environments. Additionally, Mergen et al. [
36] highlighted the increased adoption of virtual reality in medical curricula and made comments on the existing limitations that should be overcome. Finally, Abbas et al. [
37] defined and presented virtual reality in the context of healthcare while Liaw et al. [
38] highlighted the potential of multiuser virtual worlds to facilitate collaborative learning in healthcare education.
These studies highlight the potential of virtual reality to enhance learning outcomes in medical, nursing, and healthcare education. Nonetheless, given the rapid advancements in the domain of virtual reality, there is a lack of a comprehensive bibliometric and scientific mapping analysis that synthesizes the recent and global advances in applying virtual reality across these fields. The need to examine this field through a more holistic perspective becomes more evident when considering that existing studies focus on specific disciplines or outcomes. To address this gap in the literature, this study aims to provide an overview regarding the adoption and integration of virtual reality into healthcare, nursing, and medical education by examining the existing literature through a systematic bibliometric review. Hence, this study contributes to the existing field by providing a broader and data-driven overview of the most prominent research topics and areas and revealing areas for future research. The manuscript goes over the methodology adopted (
Section 2) and presents the analysis of the document collection created (
Section 3). The results are further discussed in
Section 4 and conclusive remarks, implications, and future research directions are presented in
Section 5.
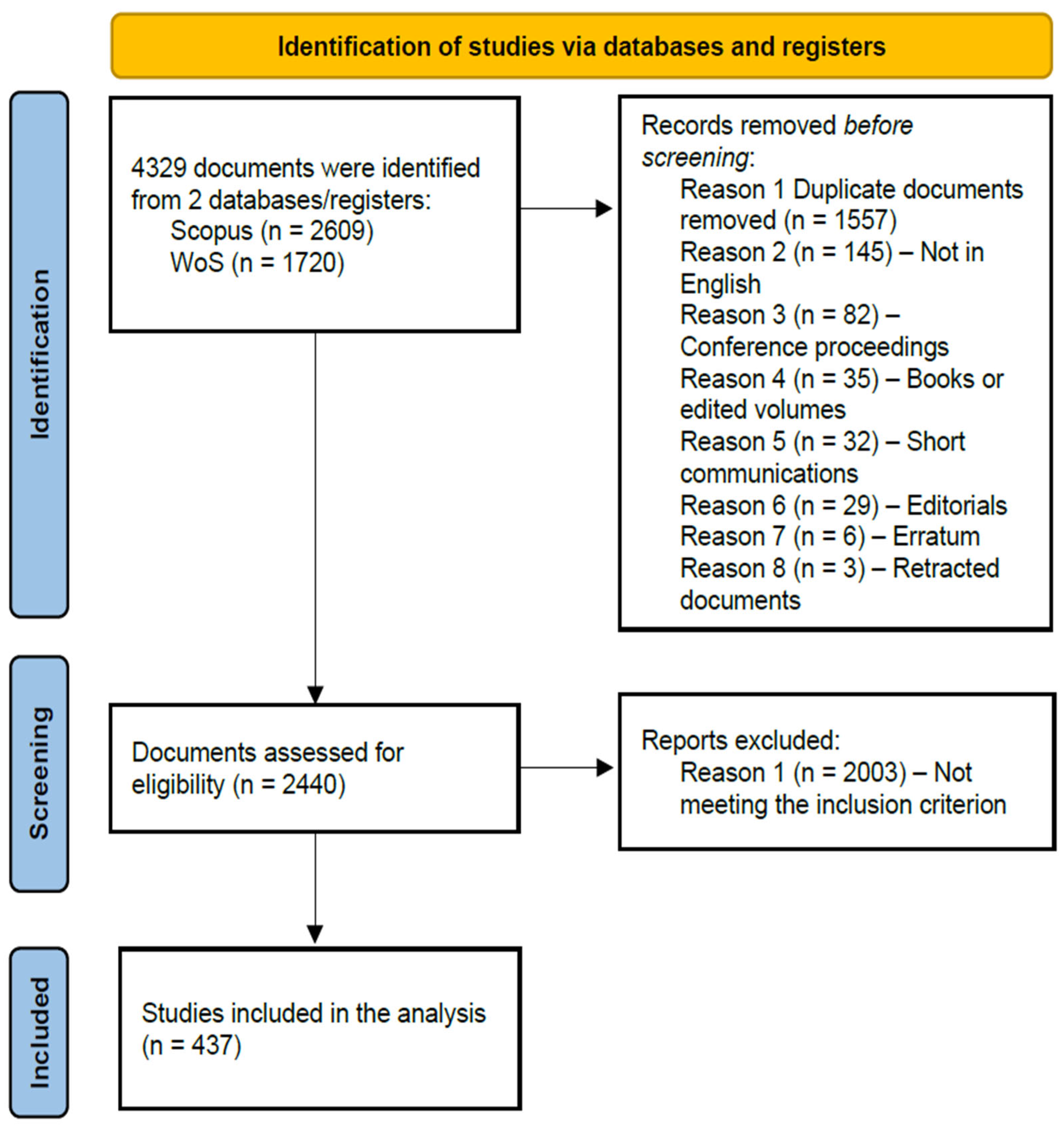
3. Analysis of Results
Using Bibliometrix, the document collection, comprising 437 documents, was examined to determine the main characteristics of the documents. The document collection information is described in
Table 1. The documents were published from 2010 to 2025 (May) in 243 different sources. When including the data from January to May 2025, the annual growth rate reported was 21.55%; however, when excluding this data and only including the related data from January 2010 to December 2024 the annual growth rate reported was 30.07%. This outcome is in line with the average age of the documents (2.87 years). Most documents were published as journal articles (63.4%), followed by conference and proceedings papers (17.6%) as well as review studies (15.6%). Fewer documents were published within edited volumes as book chapters (3.4%). In total, 1682 authors from 54 countries were identified, with the average number of co-authors per document being 4.58. Additionally, 20 single-authored documents that were written by 19 different authors were present in the document collection. Finally, the international co-authorship rate was 13.5%. The related outcomes are further discussed below.
When considering the annual growth rate and the average document age, the emergence of this field due to its potential and significance becomes evident. As depicted in
Figure 2, there is a continuous increase in the number of annually published documents, with most documents having been published in 2024 (
n = 119) and 2023 (
n = 74). These outcomes are in accordance with the advancements in the domain of virtual reality, including both hardware and software. It should also be noted that given the fact that the data was last updated in May 2025, there are already 56 relevant documents that have been published which, when taking the annual growth rate into account, is expected to meet and surpass the number of documents published in 2024. Thus, the increased interest in the field is being further highlighted. Moreover, based on the outcomes presented in
Table 2, it becomes evident that the documents published in 2017 have been the most impactful. Specifically, the mean total citations of the seven documents of 2017 was 117.57 and the mean total citations per year was 13.06. However, given that these documents were published 9 years ago, emphasis should also be put on more recent studies as well. For example, the studies published in 2019 have already amassed 64.93 mean total citations per document and a mean total citations per year of 9.28 citations. Given the emergence of this field and the increasing number of studies published, it is expected that these outcomes will change in the near future.
To better comprehend the characteristics of the sources in which these 437 documents were published in, the frequency of the source type was examined and Bradford’s law was also applied. The distribution of the source type was as follows: journal articles, 63.4%; conference and proceedings papers, 17.6%; review studies, 15.6%; and book chapters, 3.4%. Furthermore, using Bradford’s law, three clusters of documents were created (Clusters 1–3). Cluster 1 had the most impactful sources, that is those that published the most documents. Additionally, Cluster 1 had 19 sources (7.8%) and 146 published documents, Cluster 2 had 80 sources (32.9%) and 147 published documents, and Cluster 3 had 144 sources (59.3%) and 144 published documents. As presented in
Table 3, when considering the number of documents published by each source, the most impactful sources were “Nurse Education Today”, “BMC Medical Education”, “Clinical Simulation in Nursing”, “CIN: Computers, Informatics, Nursing”, “JMIR Medical Education”, “Nurse Education in Practice”, and “JMIR Serious Games”. Besides these outcomes, 7 sources each published five documents, 12 sources each published four documents, and 10 sources each published three documents. As these sources had the most published documents, the outcomes remain the same in terms of order when considering the h-index accumulated from the documents published, as is presented in
Table 4. Additionally, 4 sources had an h-index of 4 and 11 sources had an h-index of 3. Therefore, it can be stated that the sources of different types and publishers with diverse scope are selected to publish studies relevant to this field; thus, the multidisciplinary nature of this field of study is being highlighted.
Having examined the characteristics of the sources, the authors’ affiliations and countries were also explored. On average, the documents were written by 4.58 authors and out of the 437 studies, only 4.6% were single-authored. The number of documents written by the authors was further examined using Lotka’s law analysis, as can be seen in
Figure 3. The vast majority of authors contributed to a single study (
n = 1482, 88.1%), while eleven authors contributed to five studies and only two authors contributed to six studies.
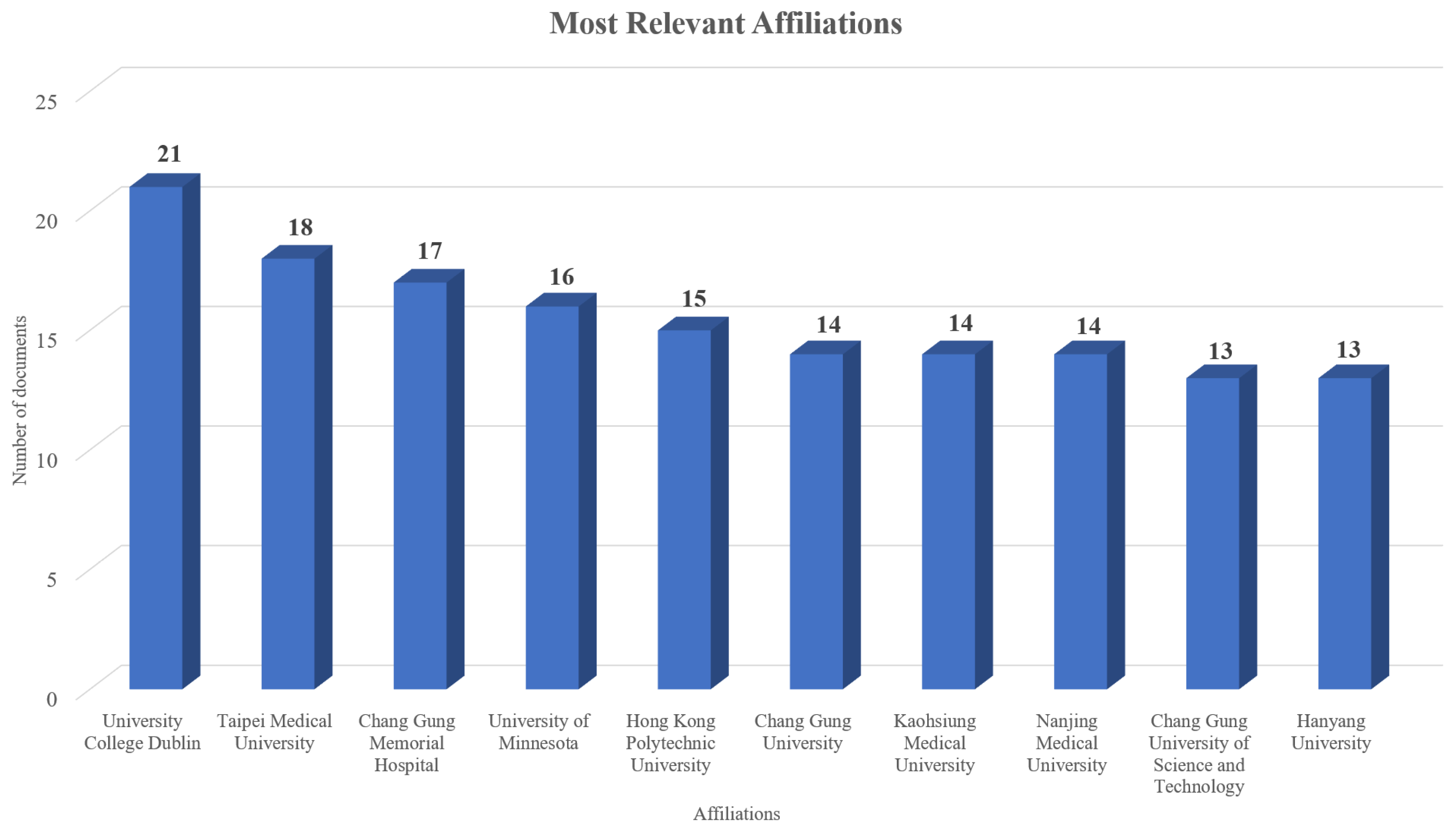
Furthermore, emphasis was placed on the authors’ affiliation to identify the ones that mostly focus on advancing this field of study. As can be seen in
Figure 4, the affiliations with the most relevant documents published were “University College Dublin”, “Taipei Medical University”, “Chang Gung Memorial Hospital”, “University of Minnesota”, “Hong Kong Polytechnic University”, “Chang Gung University”, “Kaohsiung Medical University”, “Nanjing Medical University”, “Chang Gung University of Science and Technology”, and “Hanyang University”. Based on the related outcomes, it is evident that most of the affiliations that have published the most documents are based in Asia.
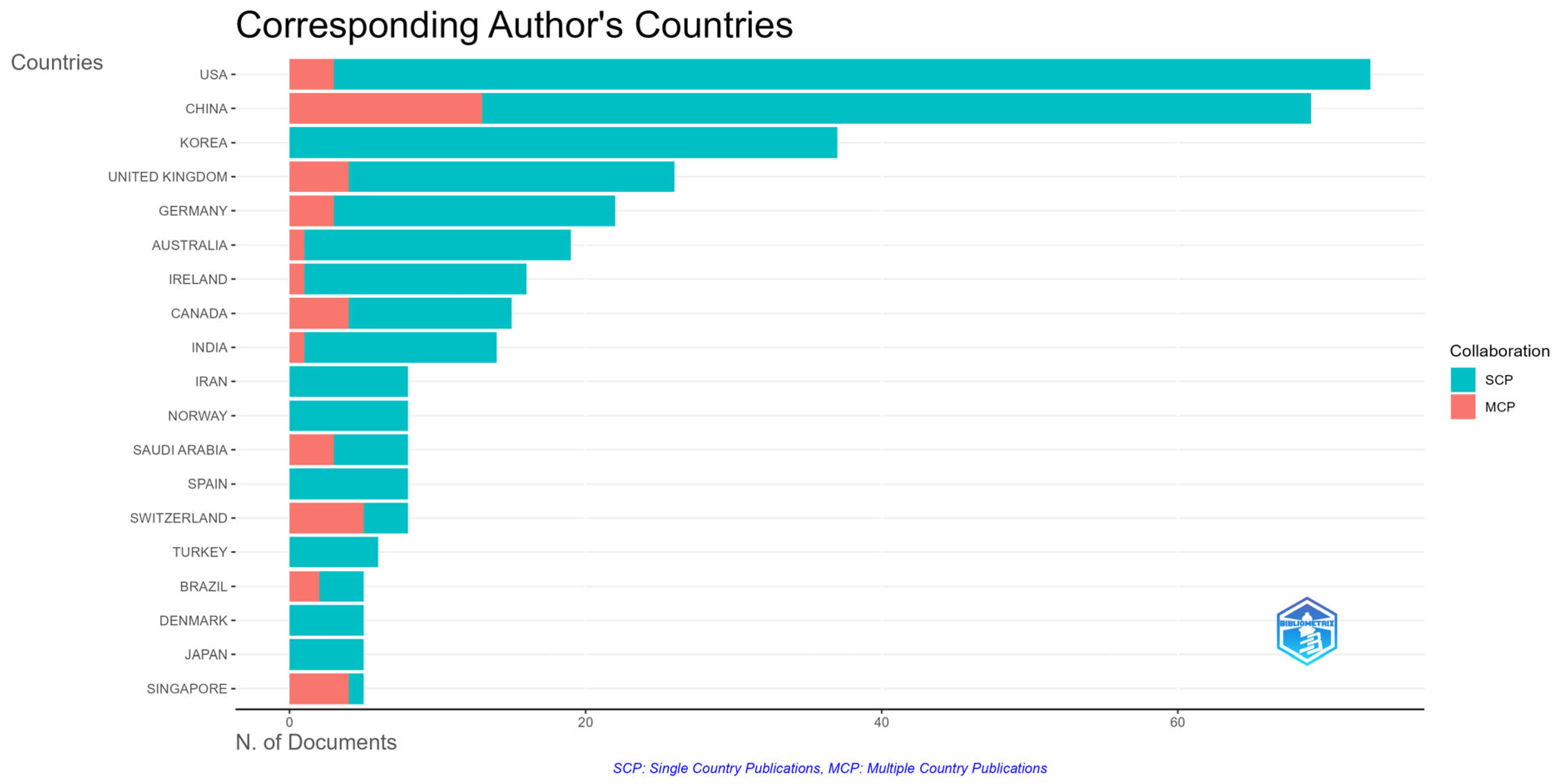
Additionally, the countries that published the most on this topic were examined. It should be noted that to categorize the countries the grouping carried out by Bibliometrix was used and the corresponding author’s country or the country of the first author, in case no corresponding author was indicated, was used. Hence, taking these limitations into consideration, 54 different countries were identified. The countries that have published at least 12 documents are presented in
Table 5, while the countries that have published at least 5 documents are depicted in
Figure 5. The United States and China have published the most documents. South Korea, the United Kingdom, and Germany have contributed over 20 documents each while Australia, Ireland, Canada, and India have contributed at least 14 documents each. Similarly, the highest intra-country (SCP) collaborations were observed in the United States and China while China also had the highest inter-country (MCP) collaborations, followed by Switzerland (MCP = 5). Finally,
Table 6 presents the countries with the highest number of total citations received and their average citations per document. Once again, the documents published by China (TC = 1391) and the United States (TC = 1185) had the most citations. Despite the difference in the number of documents published and the citations received, it can be inferred that there is a global interest surrounding the integration of virtual reality in healthcare, nursing, and medical education.
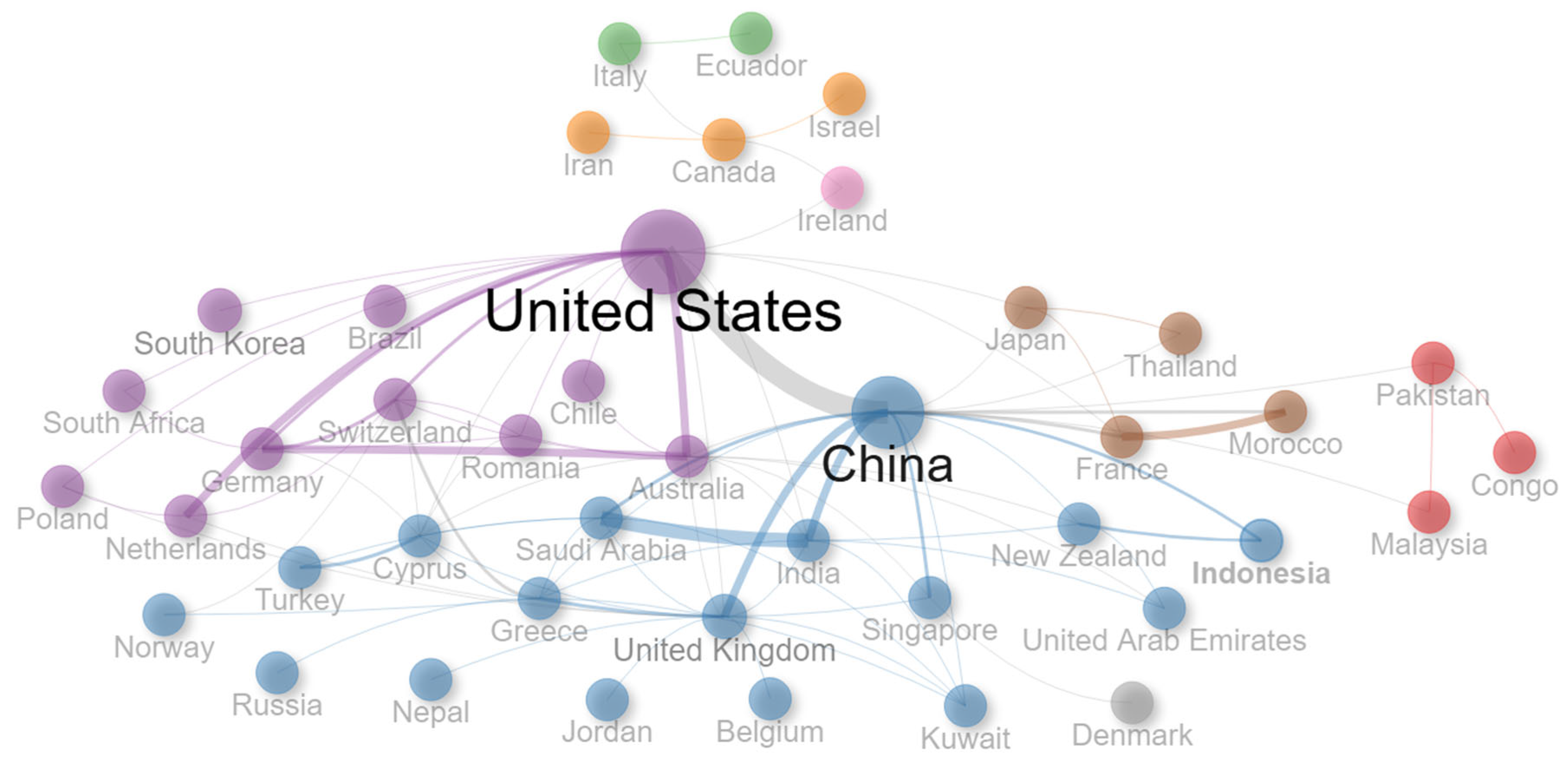
Despite the fact that a large number of countries from diverse continents contributed to this field of study, the international co-authorship rate being 13.5% shows that going forward there is a growing need to establish more international collaborations, as can also be seen in
Figure 6 and
Figure 7.
4. Discussion
Due to the educational benefits that virtual reality can yield, it is increasingly being used in different learning settings [
45,
46,
47]. The outcomes of recent studies have highlighted its potential to positively influence health sciences education in the context of nursing education [
26], patient education [
27,
30], healthcare education [
23], and medical education [
24,
25]. Virtual reality can create immersive, personalized, and safe learning environments in which learners can acquire hands-on experience and practice clinical skills, decision-making, and patient interactions within controlled settings without risking patient safety [
9,
10]. Hence, it can support both students and professionals and enable them to increase their knowledge and skills [
28,
29]. Students who learn through virtual reality showcase increased learning outcomes, including academic achievements, clinical skills, procedural training, decision-making, critical thinking, as well as knowledge acquisition and retention [
35]. Hence, it is being more widely adopted in health sciences curricula [
36]. These outcomes suggest that virtual reality plays a vital role in the enrichment and transformation of healthcare, nursing, and medical education.
Since there is an increasing interest in this multidisciplinary field and many relevant studies are being published, this study examined and mapped the current literature. This approach provides a clearer comprehension and representation of the current research landscape and offers insights into the main topics and research directions. Therefore, in addition to analyzing the characteristics of the document collection, attention was also given to identifying the primary topics explored and examined the documents that received the most citations (over 100 citations). The related documents are described in
Table 7 and provide valuable insight into the role, integration, and use of virtual reality.
Moro et al. [
48] explored the effectiveness of both virtual reality and augmented reality in health sciences. Their results revealed that between virtual and augmented reality, no major differences were observed in terms of students’ scores. However, some students who learnt through virtual reality reported adverse effects, such as blurred vision, dizziness, and headaches. Nonetheless, both technologies emerged as being valuable for teaching medical and healthcare related subjects while also promoting students’ engagement and immersion. Chen et al. [
26] focused on examining the effectiveness of virtual reality in nursing education through a meta-analysis of 12 related studies. Their results revealed that students who learnt through virtual reality showcased improved knowledge. However, no major differences were observed in regard to students’ confidence, skills, performance time, and satisfaction. The study highlights the need for future studies to focus on larger sample sizes. Through a systematic literature review of 27 related studies, Barteit et al. [
49] explored the use of head-mounted devices for augmented, mixed, and virtual reality within medical education. Their findings revealed that virtual reality and augmented reality were mostly used to train students in the fields of surgery and anatomy. Students found learning through these technologies engaging and motivating and expressed higher levels of enjoyment and enthusiasm. Head-mounted display interventions arose as effective in both cases. Hence, it was concluded that learning using head-mounted displays within augmented reality and virtual reality environments can be effective for medical education.
Baniasadi et al. [
50] focused on the challenges and practical considerations associated with the adoption and integration of virtual reality in medical education. Based on their results, both general and specific challenges were identified. The general challenges involved “reduced face-to-face communications, education, cost challenges, and users’ attitudes”, while the specific challenges involved “designing, safety considerations, virtual reality side effects, evaluation, and validation of virtual reality applications”. It is highlighted that these challenges can have different effects when learning through virtual reality and that it is important to develop new standards and protocols. Joda et al. [
51] carried out a systematic literature review of 16 studies focusing on the role and use of augmented and virtual reality in dental medicine. Their outcomes revealed that both technologies were mostly used for motor skills training, treatment, concept learning, and clinical testing. However, the nature of the studies and data examined did not allow for a meta-analysis of the outcomes to be conducted. Nonetheless, the study highlighted the positive impact that these technologies can have in the field of medical education and commented upon the need for more case studies to be conducted and for suitable technological standards to be developed.
Through a systematic mapping review of 22 studies, Plotzky et al. [
52] explored the integration of virtual reality simulations within nurse education. The data revealed that the definition of virtual reality simulations for educational purposes varied greatly. Additionally, these simulations were mostly used to improve students’ procedural skills, psychomotor skills, soft skills, as well as technical knowledge and proficiency. Despite using various simulation designs and adopting diverse approaches, positive educational outcomes were reported. The study commented that more studies should emphasize the implications of immersive virtual reality. In the context of medical anatomy education, Maresky et al. [
53] examined the use of virtual reality to support teaching and learning activities. Their experimental study revealed that students can better understand anatomy related concepts through the use of virtual reality. Hence, it was concluded that virtual reality is a viable educational means that can effectively support medical anatomy education since it provides anatomically correct and immersive visual–spatial environments. Dyer et al. [
54] focused on teaching empathy in the context of medical education through the use of virtual reality. Their results disclosed that when students learn through virtual reality, their knowledge and understanding of age-related health problems were increased and simultaneously their empathy for older adults also improved. Hence, virtual reality emerged as an effective teaching method to support students pursuing health and medical professions.
Huang et al. [
55] explored students’ acceptance of using virtual reality within medical education. Their outcomes showcased that students positively assessed the use of virtual reality and highlighted its immersion and imagination features as key aspects. These elements can predict students’ perceived ease of use and usefulness and as such, are key contributors to identifying and examining students’ behavioral intention of using virtual reality for educational purposes. Through a systematic review and meta-analysis of 58 studies, Moro et al. [
56] examined medical and health sciences students’ test performance in medical related fields. Focusing on the use of virtual reality, students who learnt using virtual reality performed better when compared with those that learnt through traditional teaching methods. The results of the study highlighted virtual reality as a viable alternative or as a supportive method to the existing education in medical and health sciences courses. In their systematic review using machine learning techniques, Winkler-Schwartz et al. [
57] examined 12 studies regarding surgical experiences in virtual reality simulations. Specifically, they developed and presented the “Machine Learning to Assess Surgical Expertise (MLASE)” checklist to enhance the quality of producing and reviewing manuscripts that focus on assessing surgical expertise within virtual reality learning environments.
Dubovi et al. [
58] explored non-immersive virtual reality simulations and their influence on nursing students. The outcomes suggest that students can achieve significantly higher procedural and conceptual knowledge when learning within non-immersive virtual reality environments in comparison with lecture-based learning. These simulations offered students a sense of presence and control which can positively influence their practical skills training. With an emphasis on nursing education, Kilmon et al. [
59] examined the influence of immersive virtual reality simulations. Based on their outcomes, immersive virtual reality simulations can support the education of undergraduate nursing students but can also assist experienced nurses in learning advanced skills. These immersive simulations can supplement clinical instruction and constitute an effective educational strategy for nursing education. Hence, it is suggested that they will be more commonly used in nursing education in the near future. However, it is highlighted that there is a clear need for more interdisciplinary collaboration to develop effective immersive virtual reality simulations. Focusing on immersive technologies, including virtual reality, Tang et al. [
60] carried out a systematic literature review of 128 studies to examine their application in medical education and training. Their results revealed that virtual reality is primarily used in teaching anatomy-related or surgery-related subjects. Given the data explored and the future trends explained, virtual reality, and immersive technologies in general, arose as promising and effective tools to support medical education and practices.
The related studies further validate the positive influence that virtual reality can have on medical, healthcare, and nursing education. Additionally, they highlight the benefits of the immersive, interactive, and safe learning environments offered through virtual reality. However, despite the pedagogical value that virtual reality has, there are still challenges that need to be overcome before it is being more widely adopted. Despite the existing limitations, the aforementioned studies regard virtual reality as an educational tool that can significantly enhance the quality and effectiveness of students’ and professionals’ training in various domains of health sciences education, including nursing, healthcare, and medical education.
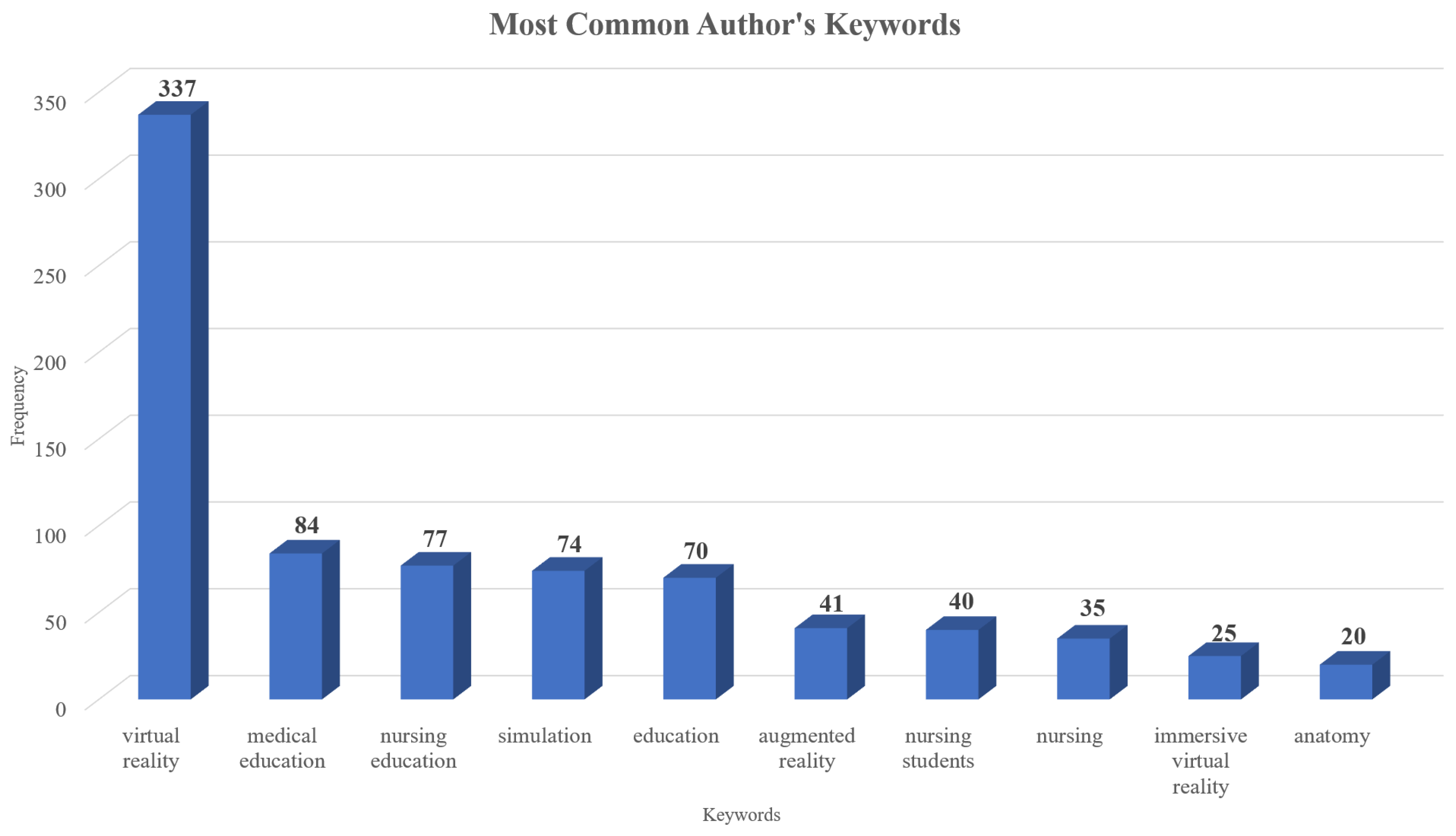
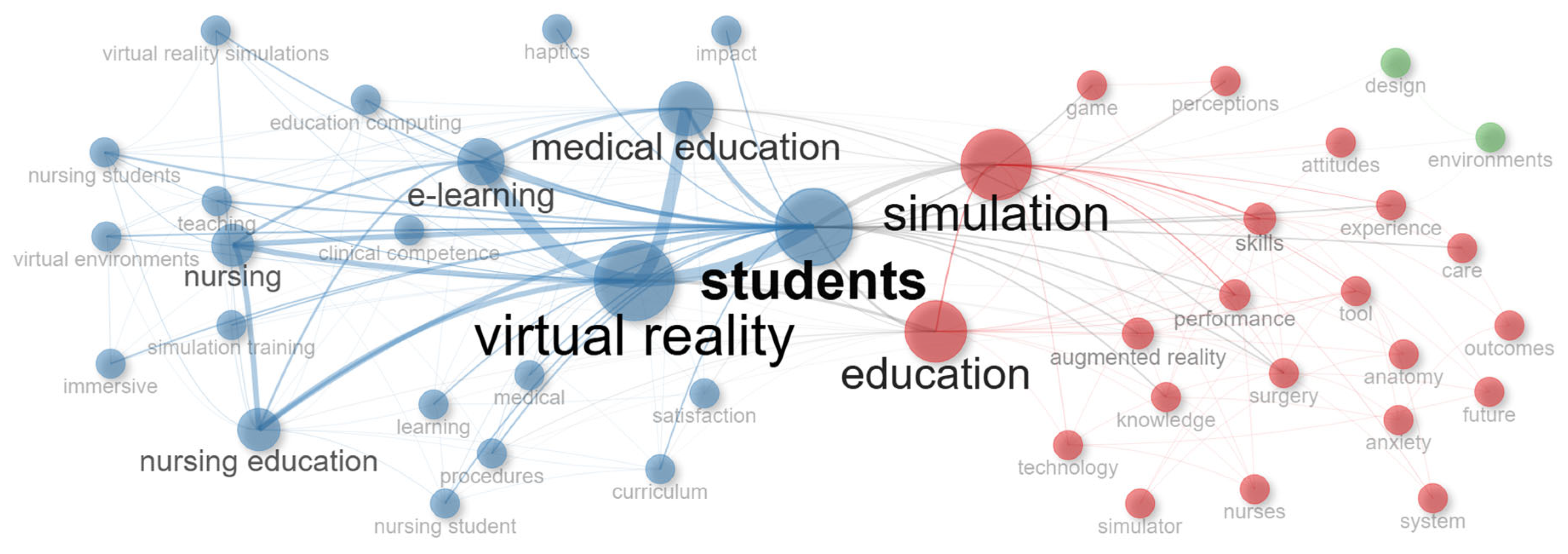
Furthermore, the keywords of the documents were also examined to identify key topics within the collection. Both keywords plus and author’s keywords were used, as can be seen in
Figure 8 and
Figure 9, which present the most frequently used keywords. Specifically, the most frequent keywords plus were “virtual reality”, “simulation”, “education”, “students”, “medical education”, “e-learning”, “performance”, “skills”, “nursing”, and “nursing education”, while the most frequent author’s keywords were “virtual reality”, “medical education”, “nursing education”, “simulation”, “education”, “augmented reality”, “nursing students”, “nursing”, “immersive virtual reality”, and “anatomy”. Based on these outcomes and the results of the related studies presented, the close relationship between virtual reality with medical and nursing education is highlighted. Additionally, the emphasis on simulations and immersive experiences and the focus on nursing students, surgery, and anatomy education can be observed. Finally, in the co-occurrence network of keywords presented in
Figure 10, the relationships among the keywords can be seen. Specifically, three main clusters arose with the first cluster (blue) focusing more on students, virtual reality, medical education, nursing education, and e-learning, the second cluster (red) focusing more on education and simulations, and the third cluster (green) focusing on the design of virtual reality learning environments. Having a separated cluster dedicated to the design aspects further highlights the significance of developing virtual reality experiences following user-centered design principles.
Emphasis was also placed on identifying topics through the analysis of the keywords of both categories. As can be seen in
Table 8, eight main topics arose. These topics were related to: (i) Virtual reality and immersive technologies in health sciences education; (ii) Simulation-based learning in healthcare; (iii) Medical and nursing education; (iv) Learning outcomes; (v) Psychological and cognitive aspects of learning; (vi) Clinical skills and competency development; (vii) Patient-centered and empathy training; and (viii) Emerging technologies and innovative approaches.
Based on these topics, it can be inferred that virtual reality can enrich and transform health sciences education. Specifically, virtual reality provides immersive, safe, and interactive environments and simulations in which students can familiarize themselves with complex clinical scenarios and can cultivate their clinical skills and competency within controlled environments; thus, enabling students to practice procedures without affecting patient safety. In this context, emphasis is put on medical education and nursing education and how virtual reality can effectively support them. Research has also explored the impact of virtual reality on students’ learning outcomes, experiences, and attitudes, along with its effects on the psychological and cognitive dimensions of learning. Given the nature of this field, particular emphasis is being placed on improving patient-centered care and empathy training through virtual reality to enable future healthcare professionals to embody patient perspectives, increase their communication skills, and to acquire a deeper emotional understanding. Finally, virtual reality can be used in conjunction with other emerging technologies and support innovative approaches to increase education quality. Therefore, virtual reality can be regarded as an effective educational means that can enhance education and strengthen the healthcare ecosystem.
Nonetheless, there are key challenges that influence its effective adoption which need to be further explored. Specifically, the variability in study designs, small sample sizes, and inconsistent outcome measures limit the generalizability of findings. Many current studies also lack long-term follow-up, making it difficult to assess sustained clinical impact. Limitations, such as motion sickness, blurred vision, and fatigue, affect a subset of learners, while the cognitive demands of navigating complex virtual environments may lead to distraction or overload. Accessibility remains another concern since some learners might be excluded from virtual reality experiences if they are not designed inclusively. Additionally, infrastructure issues like equipment costs, unreliable performance, and the need for ongoing technical support pose practical barriers, especially in resource-constrained settings.
Moreover, while virtual reality is being more widely adopted, there is a risk of overestimating its pedagogical value, especially in areas where authentic human interaction is critical. Current virtual reality technologies often fall short in replicating real-time interpersonal dynamics. This can lead to false confidence in communication skills and underdeveloped empathy or professionalism. The simplification of clinical scenarios to suit virtual platforms may also result in incomplete or misleading learning experiences. Furthermore, an increased reliance on virtual reality could inadvertently reduce opportunities for face-to-face learning, which remains essential for developing collaborative, relational, and patient-centered skills. Instructors may also feel unprepared or resistant to using unfamiliar technologies, highlighting the need for professional development and support. Finally, ethical considerations, including data privacy and security, consent, and cultural realism, are still underexplored.
For educators and institutions planning to adopt virtual reality, understanding these limitations is essential for successful and ethical integration. Virtual reality should not be seen as a replacement for face-to-face instruction but as a complementary tool. Hence, its use should be balanced with opportunities for real-world interpersonal skill development. Instructors may require dedicated training and curriculum support to meaningfully integrate virtual reality into their teaching strategies. Additionally, those developing virtual reality content should account for cultural sensitivity, data privacy, and learner diversity to ensure equity and realism. Institutions are advised to establish multidisciplinary teams of education stakeholders to oversee and guide the design and development of virtual reality learning experiences. Recognizing that the simplification of scenarios may lead to false confidence, educators should incorporate structured debriefs, reflection sessions, and assessments that bridge the gap between simulated and actual clinical practice. Addressing these challenges is essential to ensure that virtual reality will enrich the quality and equity of health professions education and that it will not hinder actual clinical practice.
5. Conclusions
While the amount of research regarding the integration of virtual reality in health sciences education increases, this study aimed to provide an overview of the existing literature. This study followed the PRISMA framework and examined 437 documents from Scopus and WoS that were published during 2010–2025. The studies were written by authors from 54 different countries and were published in 243 sources with most of the documents referring to journal articles. An annual growth rate of 30.07% was observed and most documents were published in 2024 and 2023. Additionally, the characteristics of the documents were examined, the most relevant sources were identified, and the number of published studies and their citations were analyzed. The affiliations and countries that contributed the most were identified. The United States and China published the most in this field and had the highest total citations, while studies from Australia had the highest average document citations. The collaboration network of countries was also examined. Finally, the documents with the most citations were analyzed and the main topics were identified. Finally, the topic analysis revealed the following eight topics: (i) Virtual reality and immersive technologies in health sciences education; (ii) Simulation-based learning in healthcare; (iii) Medical and nursing education; (iv) Learning outcomes; (v) Psychological and cognitive aspects of learning; (vi) Clinical skills and competency development; (vii) Patient-centered and empathy training; and (viii) Emerging technologies and innovative approaches.
Based on the analysis, virtual reality arose as an effective educational tool that can enrich and transform health sciences education, including healthcare education, nursing education, and medical education. Specifically, virtual reality can support both students and professionals through the immersive, realistic, and safe learning environments it offers where learners can practice their skills, patient interactions, and decision-making without risking patient safety. Increased learning outcomes in terms of performance, engagement, clinical skills development, knowledge acquisition, critical thinking, and decision-making were observed. Virtual reality also positively contributes to students’ developing their empathy and behavioral understanding. The ability of virtual reality to be utilized in conjunction with other emerging technologies and support different pedagogical approaches was noticed. As virtual reality becomes more accessible and cost effective in terms of both software and hardware, its integration into health sciences curricula is likely to become more widespread.
However, some key challenges and limitations were also identified. Specifically, the outcomes of some studies are limited in terms of generalizability due to the variation in study designs and in measures. The sample size in many cases was also relatively small. This limitation reveals the need for future experimental studies to emphasize examining the long-term effects within large-scale samples. Few studies also reported students showcasing adverse effects, such as blurred vision, dizziness, and headaches. Hence, there is a need for further research into the usability and design of virtual reality experiences. Another existing limitation is the lack of common evaluation methods and of unified design approaches and guidelines. Thus, more emphasis should be placed on developing suitable guidelines and identifying best practices and approaches in diverse settings. A lack of interdisciplinary and international collaborations was observed. Given the nature of the field, multidisciplinary perspectives are vital to ensure its effective development. Future studies should also focus on safety considerations, privacy and ethical concerns, reduced face-to-face interactions, and cost issues. Given the implementation limitations and issues associated with the effective introduction and utilization of virtual reality in education, emphasis should be placed on developing robust frameworks and policies, creating rigorous assessment methods and tools, and refining pedagogical and curriculum design approaches. There is also a need for training programs on how to use virtual reality technology for education stakeholders to be created and for developing suitable and accessible educational material for virtual reality environments. Finally, emphasis should be placed on examining the impact of immersive virtual reality and non-immersive virtual reality, and on combining virtual reality with other novel technologies to develop intelligent systems to aid the healthcare system.
All in all, virtual reality has emerged as an effective educational tool for increasing learning outcomes across healthcare, nursing, and medical education. However, for its pedagogical value to be fully realized and its integration to become more widespread, the existing challenges should be addressed. As evidence supporting its impact increases, virtual reality is more than likely to become an integral part of health professions education.