Physiological State Monitoring in Advanced Soldiers: Precision Health Strategies for Modern Military Operations
Abstract
1. Introduction
2. Materials and Methods
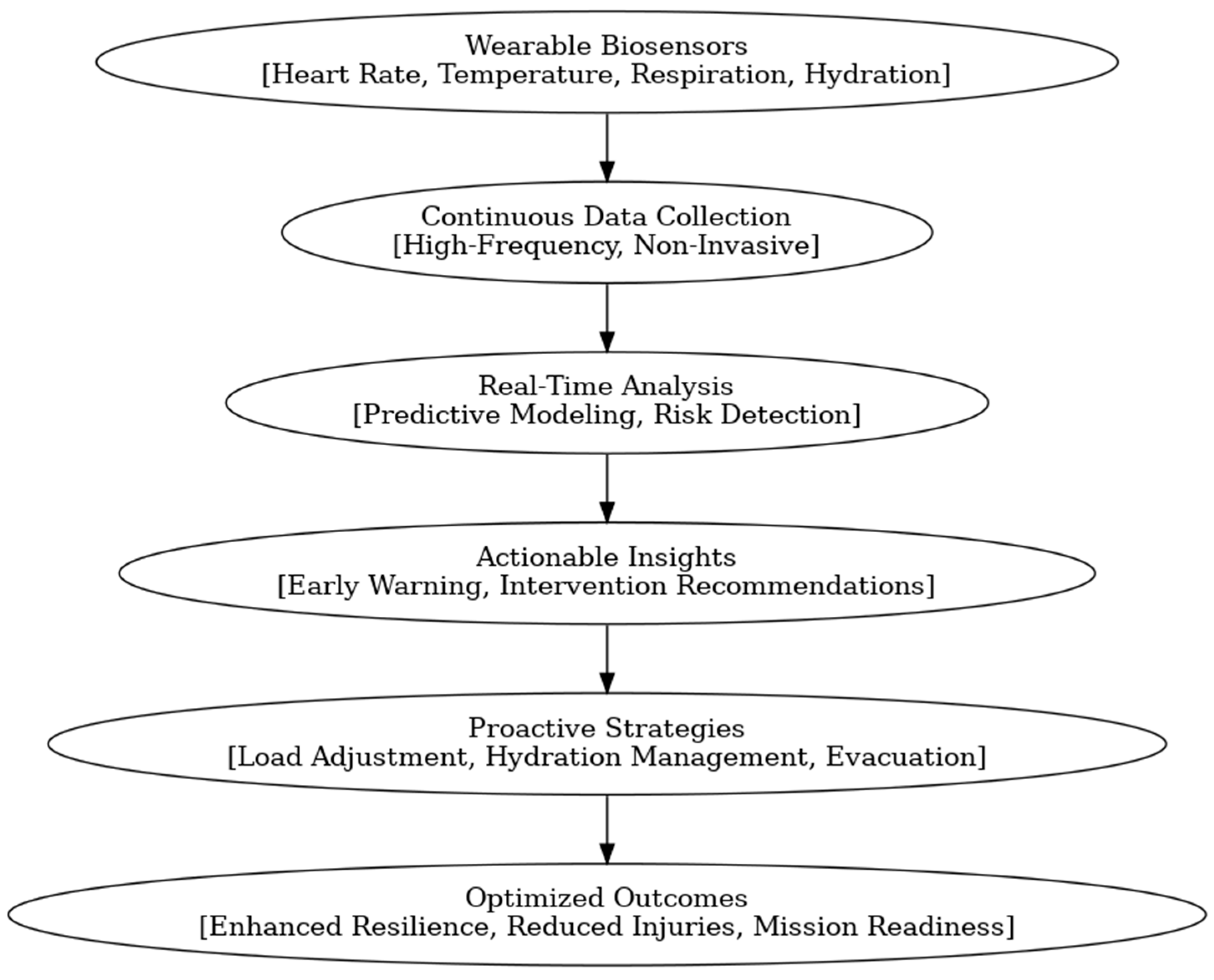
3. Physiological State Monitoring
4. Precision Health Applications
5. Advanced Technological Systems for High-Stakes Environments
6. Enhanced Responsiveness and Safety
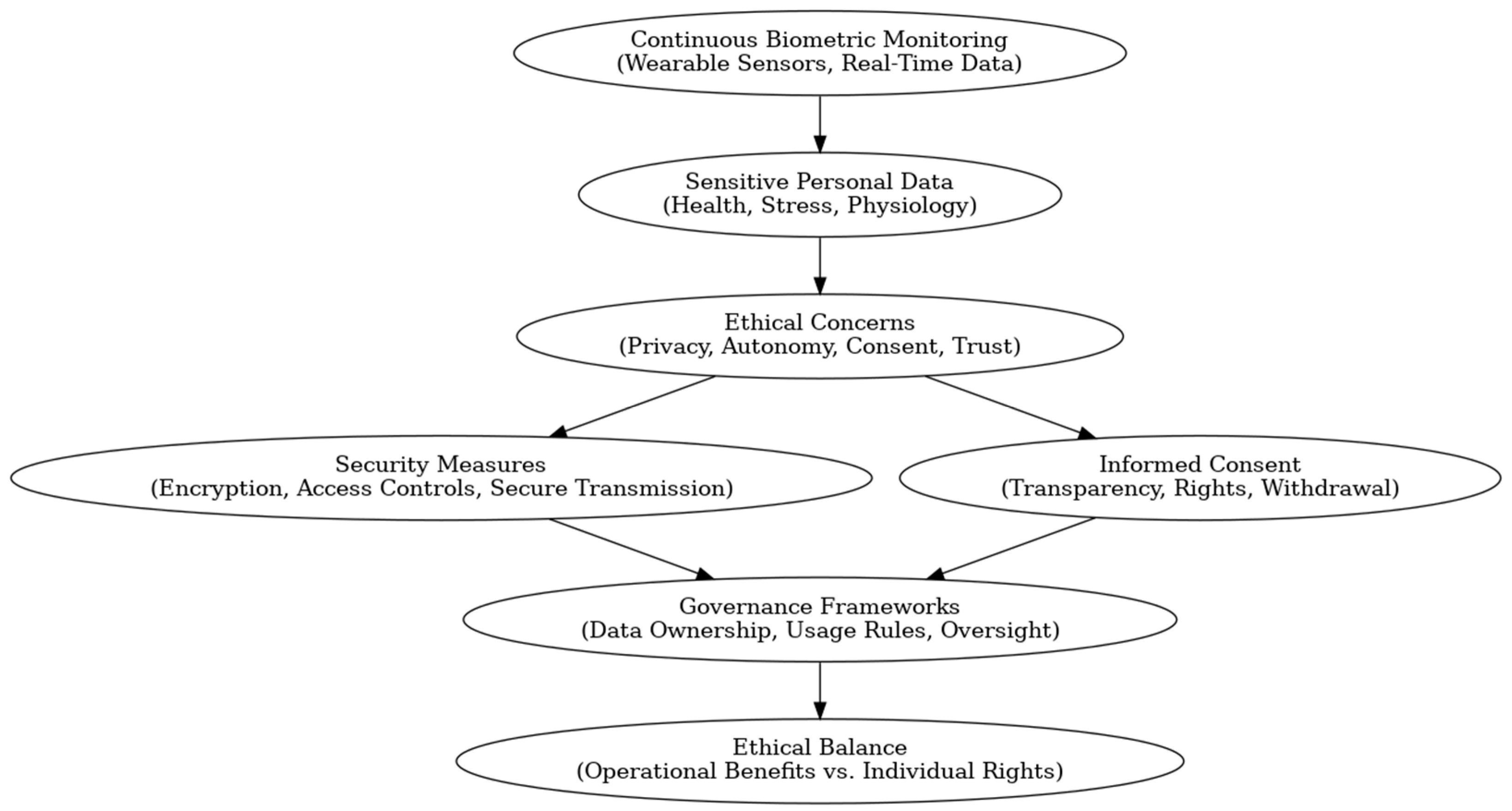
7. Ethical and Security Concerns
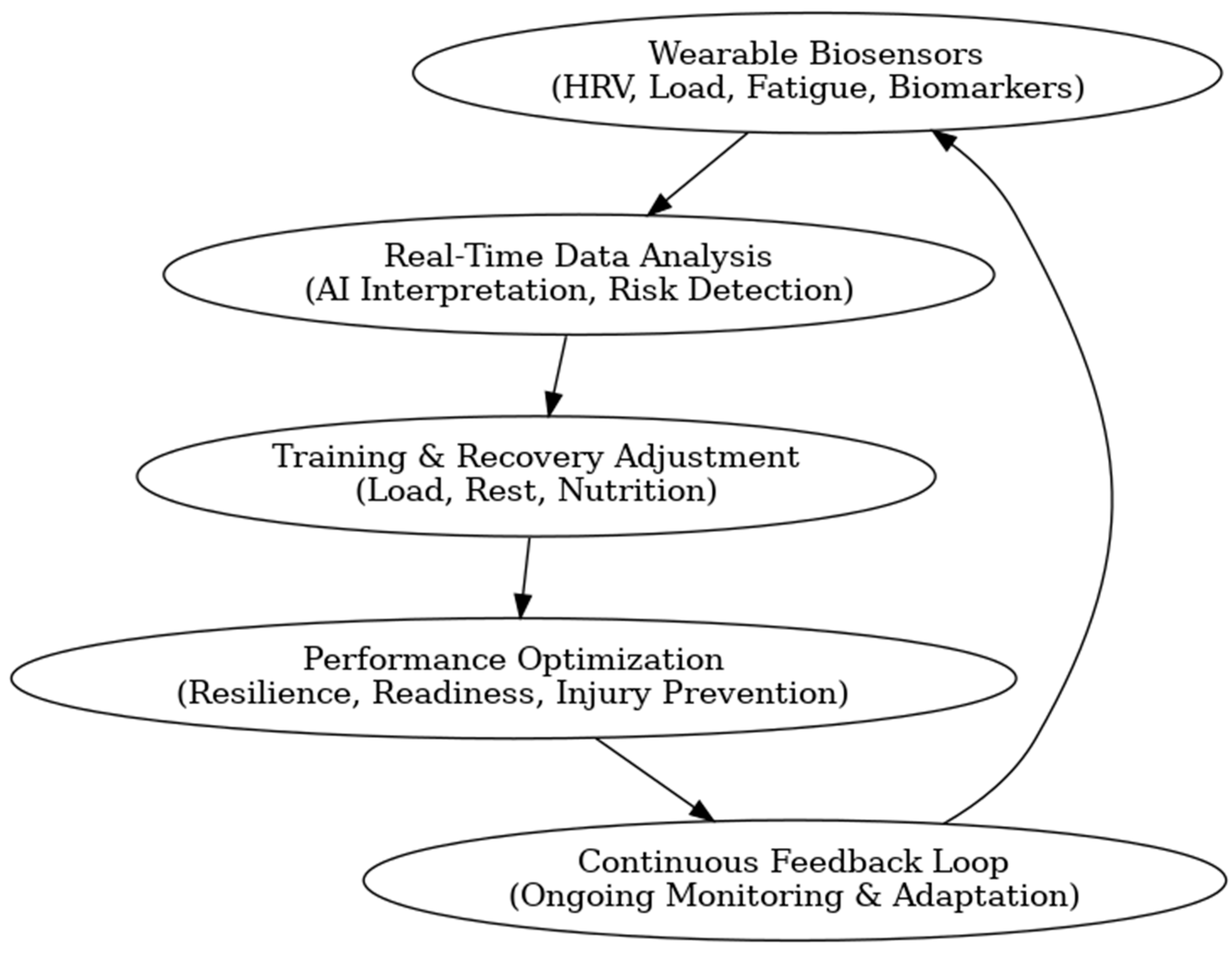
8. Performance Optimization
9. Discussion
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sawka, M.N.; Cheuvront, S.N.; Kenefick, R.W. Hypohydration and human performance: Impact of environment and fluid intake. Sports Med. 2015, 45 (Suppl. 1), S51–S60. [Google Scholar] [CrossRef]
- Gibson, O.R.; James, C.A.; Mee, J.A.; Willmott, A.G.; Turner, G.; Hayes, M.; Maxwell, N.S. Heat alleviation strategies for athletic performance: A review and practitioner guidelines. Temperature 2019, 7, 3–36. [Google Scholar] [CrossRef] [PubMed]
- González-Alonso, J.; Teller, C.; Andersen, S.L.; Jensen, F.B.; Hyldig, T.; Nielsen, B. Influence of body temperature on the development of fatigue during prolonged exercise in the heat. J. Appl. Physiol. 1999, 86, 1032–1039. [Google Scholar] [CrossRef]
- Lieberman, H.R. Cognitive methods for assessing mental energy. Nutr. Neurosci. 2007, 10, 229–242. [Google Scholar] [CrossRef] [PubMed]
- Bourdon, P.C.; Cardinale, M.; Murray, A.; Gastin, P.; Kellmann, M.; Varley, M.C.; Gabbett, T.J.; Coutts, A.J.; Burgess, D.J.; Gregson, W.; et al. Monitoring athlete training loads: Consensus statement. Int. J. Sports Physiol. Perform. 2017, 12 (Suppl. 2), S161–S170. [Google Scholar] [CrossRef] [PubMed]
- Corrigan, S.L.; Bulmer, S.; Roberts, S.S.H.; Warmington, S.; Drain, J.; Main, L.C. Monitoring Responses to Basic Military Training with Heart Rate Variability. Med. Sci. Sports Exerc. 2022, 54, 1506–1514. [Google Scholar] [CrossRef]
- Berg Rice, V.J.; Connolly, V.L.; Pritchard, A.; Bergeron, A.; Mays, M.Z. Effectiveness of a screening tool to detect injuries during Army Health Care Specialist training. Work 2007, 29, 177–188. [Google Scholar] [CrossRef]
- Grant, C.C.; Mongwe, L.; van Rensburg, D.C.J.; Fletcher, L.; Wood, P.S.; Terblanche, E.; du Toit, P.J. The Difference Between Exercise-Induced Autonomic and Fitness Changes Measured After 12 and 20 Weeks of Medium-to-High Intensity Military Training. J. Strength Cond. Res. 2016, 30, 2453–2459. [Google Scholar] [CrossRef]
- Helén, J.; Kyröläinen, H.; Ojanen, T.; Pihlainen, K.; Santtila, M.; Heikkinen, R.; Vaara, J.P. High-Intensity Functional Training Induces Superior Training Adaptations Compared With Traditional Military Physical Training. J. Strength Cond. Res. 2023, 37, 2477–2483. [Google Scholar] [CrossRef]
- Patel, S.; Park, H.; Bonato, P.; Chan, L.; Rodgers, M. A review of wearable sensors and systems with application in rehabilitation. J. Neuroeng. Rehabil. 2012, 9, 21. [Google Scholar] [CrossRef]
- De Castro, M.; Biesecker, L.G.; Turner, C.; Brenner, R.; Witkop, C.; Mehlman, M.; Bradburne, C.; Green, R.C. Genomic medicine in the military. NPJ Genom. Med. 2016, 1, 15008. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Giudice, G.; Petsalaki, E. Proteomics and phosphoproteomics in precision medicine: Applications and challenges. Brief. Bioinform. 2019, 20, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Friedl, K.E. Military applications of soldier physiological monitoring. J. Sci. Med. Sport. 2018, 21, 1147–1153. [Google Scholar] [CrossRef] [PubMed]
- Buller, M.J.; Welles, A.P.; Friedl, K.E. Wearable physiological monitoring for human thermal-work strain optimization. J. Appl. Physiol. 2018, 124, 432–441. [Google Scholar] [CrossRef]
- de Vries, H.J.; van der Wal, S.J.; Delahaij, R.; Venrooij, W.; Kamphuis, W. Real-time monitoring of military health and readiness: A perspective on future research. Front. Digit. Health 2025, 7, 1542140. [Google Scholar] [CrossRef]
- O’Leary, T.J.; Wardle, S.L.; Rawcliffe, A.J.; Chapman, S.; Mole, J.; Greeves, J.P. Understanding the musculoskeletal injury risk of women in combat: The effect of infantry training and sex on musculoskeletal injury incidence during British Army basic training. BMJ Mil. Health 2023, 169, 57–61. [Google Scholar] [CrossRef]
- Aroganam, G.; Manivannan, N.; Harrison, D. Review on wearable technology sensors used in consumer sport applications. Sensors 2019, 19, 1983. [Google Scholar] [CrossRef]
- Liu, Y.; Zhu, S.H.; Wang, G.H.; Ye, F.; Li, P.Z. Validity and reliability of multiparameter physiological measurements recorded by the Equivital LifeMonitor during activities of various intensities. J. Occup. Environ. Hyg. 2013, 10, 78–85. [Google Scholar] [CrossRef]
- Buller, M.J.; Tharion, W.J.; Cheuvront, S.N.; Montain, S.J.; Kenefick, R.W.; Castellani, J.; A Latzka, W.; Roberts, W.S.; Richter, M.; Jenkins, O.C.; et al. Estimation of human core temperature from sequential heart rate observations. Physiol. Meas. 2013, 34, 781–798. [Google Scholar] [CrossRef]
- Drain, J.; Billing, D.; Neesham-Smith, D.; Aisbett, B. Predicting physiological capacity of human load carriage—A review. Appl. Ergon. 2016, 52, 85–94. [Google Scholar] [CrossRef]
- Ashley, E.A. Towards precision medicine. Nat. Rev. Genet. 2016, 17, 507–522. [Google Scholar] [CrossRef]
- Schork, N.J. Personalized medicine: Time for one-person trials. Nature 2015, 520, 609–611. [Google Scholar] [CrossRef]
- Wang, R.C.; Wang, Z. Precision Medicine: Disease Subtyping and Tailored Treatment. Cancers 2023, 15, 3837. [Google Scholar] [CrossRef] [PubMed]
- Sutehall, S.; Pitsiladis, Y. Personalized Nutrition for the Enhancement of Elite Athletic Performance. Scand. J. Med. Sci. Sports. 2025, 35, e70044. [Google Scholar] [CrossRef] [PubMed]
- Nindl, B.C.; Beals, K.; Witchalls, J.; Friedl, K.E. Military human performance optimization and injury prevention: Strategies for the 21st century warfighter. J. Sci. Med. Sport. 2017, 20 (Suppl. 4), S1–S2. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Mustafa, M. Precision Emergency Medicine: A Systematic Review. Cureus 2024, 16, e75068. [Google Scholar] [CrossRef]
- Shi, H.; Zhao, H.; Liu, Y.; Gao, W.; Dou, S.C. Systematic Analysis of a Military Wearable Device Based on a Multi-Level Fusion Framework: Research Directions. Sensors 2019, 19, 2651. [Google Scholar] [CrossRef]
- Bustos, D.; Guedes, J.C.; Vaz, M.P.; Pombo, E.; Fernandes, R.J.; Costa, J.T.; Baptista, J.S. Non-Invasive Physiological Monitoring for Physical Exertion and Fatigue Assessment in Military Personnel: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 8815. [Google Scholar] [CrossRef]
- Doody, C.B.; Robertson, L.; Cox, K.M.; Bogue, J.; Egan, J.; Sarma, K.M. Pre-deployment programmes for building resilience in military and frontline emergency service personnel. Cochrane Database Syst Rev. 2021, 12, CD013242. [Google Scholar] [CrossRef]
- Russell, B.K.; McGeown, J.; Beard, B.L. Developing AI enabled sensors and decision support for military operators in the field. J. Sci. Med. Sport. 2023, 26 (Suppl. 1), S40–S45. [Google Scholar] [CrossRef]
- Ordóñez, F.J.; Roggen, D. Deep convolutional and LSTM recurrent neural networks for multimodal wearable activity recognition. Sensors 2016, 16, 115. [Google Scholar] [CrossRef]
- Shi, W.; Cao, J.; Zhang, Q.; Li, Y.; Xu, L. Edge computing: Vision and challenges. IEEE Internet Things J. 2016, 3, 637–646. [Google Scholar] [CrossRef]
- Porambage, P.; Okwuibe, J.; Liyanage, M.; Ylianttila, M.; Taleb, T. Survey on multi-access edge computing for Internet of Things realization. IEEE Commun. Surv. Tutor. 2018, 20, 2961–2991. [Google Scholar] [CrossRef]
- Zhou, L.; Kang, M.; Chen, W. Lightweight Security Transmission in Wireless Sensor Networks through Information Hiding and Data Flipping. Sensors 2022, 22, 823. [Google Scholar] [CrossRef]
- Buller, M.J.; Delves, S.K.; Fogarty, A.L.; Veenstra, B.J. On the real-time prevention and monitoring of exertional heat illness in military personnel. J. Sci. Med. Sport. 2021, 24, 975–981. [Google Scholar] [CrossRef]
- Hunt, A.P.; Billing, D.C.; Patterson, M.J.; Caldwell, J.N. Heat strain during military training activities: The dilemma of balancing force protection and operational capability. Temperature 2016, 3, 307–317. [Google Scholar] [CrossRef]
- Pearsons, A.; Hanson, C.L.; Neubeck, L.; Blackstock, C.; Clarke, E.; Reed, M.J. Usability and acceptability of ambulatory moni-toring in undiagnosed syncope: Insights from the ASPIRED-Q qualitative study. BMJ Open. 2025, 15, e095927. [Google Scholar] [CrossRef] [PubMed]
- Epstein, Y.; Druyan, A.; Heled, Y. Heat injury prevention: A military perspective. J. Strength. Cond. Res. 2012, 26 (Suppl. 2), S82–S86. [Google Scholar] [CrossRef] [PubMed]
- Westwood, C.S.; Fallowfield, J.L.; Delves, S.K.; Nunns, M.; Ogden, H.B.; Layden, J.D. Individual risk factors associated with exertional heat illness in military populations. J. Sci. Med. Sport 2021, 24, 386–392. [Google Scholar]
- Parsons, I.T.; Stacey, M.J.; Woods, D.R. Heat adaptation in military personnel: Mitigating risk, maximizing readiness. J. R. Army Med. Corps 2019, 165, 313–318. [Google Scholar]
- Yankelson, L.; Sadeh, B.; Gershovitz, L.; Werthein, J.; Heller, K.; Halpern, P.; Halkin, A.; Adler, A.; Steinvil, A.; Viskin, S. Life-threatening events during endurance sports: Is heat stroke more prevalent than arrhythmic death? J. Am. Coll. Cardiol. 2014, 64, 463–469. [Google Scholar] [CrossRef] [PubMed]
- Kenny, G.P.; Flouris, A.D.; Yagouti, A.; Notley, S.R. Towards establishing evidence-based guidelines on maximum workplace temperatures to reduce occupational heat injury risk: A6 systematic review. BMC Public Health 2019, 19, 453. [Google Scholar]
- Mittelstadt, B.D.; Floridi, L. The ethics of biomedical big data. Philos. Trans. A Math. Phys. Eng. Sci. 2016, 374, 20160112. [Google Scholar]
- Kalkman, S.; Mostert, M.; Gerlinger, C.; van Delden, J.J.; van Thiel, G.J. Responsible data sharing in international health research: A systematic review of principles and norms. BMC Med. Ethics. 2019, 20, 21. [Google Scholar] [CrossRef]
- Mehlman, M.J.; Li, T.Y. Ethical, legal, social, and policy issues in the use of genomic technology by the US military. J. Law. Biosci. 2014, 1, 244–280. [Google Scholar] [CrossRef]
- Almeida, D.; Shmarko, K.; Lomas, E. The ethics of facial recognition technologies, surveillance, and accountability in an age of artificial intelligence: A comparative analysis of US, EU, and UK regulatory frameworks. AI Ethics 2022, 2, 377–387. [Google Scholar] [CrossRef]
- Kshetri, N. Blockchain’s roles in meeting key supply chain management objectives. Int. J. Inf. Manag. 2018, 39, 80–89. [Google Scholar] [CrossRef]
- Alotaibi, B. A Survey on Industrial Internet of Things Security: Requirements, Attacks, AI-Based Solutions, and Edge Computing Opportunities. Sensors 2023, 23, 7470. [Google Scholar] [CrossRef]
- Volpato, L.; Del Río Carral, M.; Senn, N.; Santiago Delefosse, M. General Practitioners’ Perceptions of the Use of Wearable Electronic Health Monitoring Devices: Qualitative Analysis of Risks and Benefits. JMIR Mhealth Uhealth 2021, 9, e23896. [Google Scholar] [CrossRef]
- Gasser, U.; Ienca, M.; Scheibner, J.; Sleigh, J.; Vayena, E. Digital tools against COVID-19: Taxonomy, ethical challenges, and navigation aid. Lancet Digit. Health 2020, 2, e425–e434. [Google Scholar] [CrossRef]
- Nebeker, C.; Torous, J.; Bartlett Ellis, R.J. Building the case for actionable ethics in digital health research supported by artificial intelligence. BMC Med. 2019, 17, 137. [Google Scholar] [CrossRef] [PubMed]
- Halson, S.L. Monitoring training load to understand fatigue in athletes. Sports Med. 2014, 44 (Suppl. 2), S139–S147. [Google Scholar] [CrossRef] [PubMed]
- Soligard, T.; Schwellnus, M.; Alonso, J.-M.; Bahr, R.; Clarsen, B.; Dijkstra, H.P.; Gabbett, T.; Gleeson, M.; Hägglund, M.; Hutchinson, M.R.; et al. How much is too much? (Part 1) International Olympic Committee consensus statement on load in sport and risk of injury. Br. J. Sports Med. 2016, 50, 1030–1041. [Google Scholar] [CrossRef] [PubMed]
- Preatoni, E.; Bergamini, E.; Fantozzi, S.; Giraud, L.I.; Bustos, A.S.O.; Vannozzi, G.; Camomilla, V. The Use of Wearable Sensors for Preventing, Assessing, and Informing Recovery from Sport-Related Musculoskeletal Injuries: A Systematic Scoping Review. Sensors 2022, 22, 3225. [Google Scholar] [CrossRef]
- Li, R.T.; Kling, S.R.; Salata, M.J.; Cupp, S.A.; Sheehan, J.; Voos, J.E. Wearable Performance Devices in Sports Medicine. Sports Health 2016, 8, 74–78. [Google Scholar] [CrossRef]
- Wardle, S.L.; Greeves, J.P. Mitigating the risk of musculoskeletal injury: A systematic review of the most effective injury prevention strategies for military personnel. J. Sci. Med. Sport. 2017, 20 (Suppl. 4), S3–S10. [Google Scholar] [CrossRef]
- Halson, S.L.; Burke, L.M.; Pearce, J. Nutrition for travel: From jet lag to catering. Int. J. Sport. Nutr. Exerc. Metab. 2019, 29, 228–235. [Google Scholar] [CrossRef]
- de Rijk, M.G.; van Eekelen, A.P.J.; Boesveldt, S.; Kaldenberg, E.; Holwerda, T.; Lansink, C.J.M.; Feskens, E.J.M.; de Vries, J.H.M. Macronutrient intake and alertness during night shifts—The time interval matters. Front. Nutr. 2023, 10, 1245420. [Google Scholar] [CrossRef]
- McClung, J.P.; Gaffney-Stomberg, E. Optimizing Performance, Health, and Well-being: Nutritional Factors. Mil Med. 2016, 181 (Suppl. 1), 86–91. [Google Scholar] [CrossRef]
- Nässi, A.; Ferrauti, A.; Meyer, T.; Pfeiffer, M.; Kellmann, M. Psychological tools used for monitoring training responses of athletes. Perform. Enhanc. Health 2017, 5, 125–133. [Google Scholar] [CrossRef]
- Scofield, D.E.; Kardouni, J.R. The tactical athlete: A product of 21st-century strength and conditioning. Strength. Cond. J. 2015, 37, 2–7. [Google Scholar] [CrossRef]
- He, M.; Cerna, J.; Alkurdi, A.; Dogan, A.; Zhao, J.; Clore, J.L.; Sowers, R.; Hsiao-Wecksler, E.T.; Hernandez, M.E. Physical, Social and Cognitive Stressor Identification using Electrocardiography-derived Features and Machine Learning from a Wearable Device. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. 2024, 2024, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Goods, P.S.R.; Maloney, P.; Miller, J.; Jennings, D.; Fahey-Gilmour, J.; Peeling, P.; Galna, B. Concurrent validity of the CORE wearable sensor with BodyCap temperature pill to assess core body temperature during an elite women’s field hockey heat training camp. Eur. J. Sport. Sci. 2023, 23, 1509–1517. [Google Scholar] [CrossRef]
- Moyen, N.E.; Bapat, R.C.; Tan, B.; Hunt, L.A.; Jay, O.; Mündel, T. Accuracy of Algorithm to Non-Invasively Predict Core Body Temperature Using the Kenzen Wearable Device. Int. J. Environ. Res. Public Health 2021, 18, 13126. [Google Scholar] [CrossRef]
- Budig, M.; Stoohs, R.; Keiner, M. Validity of Two Consumer Multisport Activity Tracker and One Accelerometer against Polysomnography for Measuring Sleep Parameters and Vital Data in a Laboratory Setting in Sleep Patients. Sensors 2022, 22, 9540. [Google Scholar] [CrossRef]
- Gahtan, B.; Funk, S.; Ketko, I.; Kodesh, E.; Kuflik, T.; Bronstein, A.M. WearableMil: An End-to-End Framework for Military Activity Recognition and Performance Monitoring. In Proceedings of the 2025 IEEE 13th International Conference on Healthcare Informatics (ICHI), Rende, Italy, 18–21 June 2025; pp. 618–623. [Google Scholar] [CrossRef]
- Nazari, G.; Bobos, P.; MacDermid, J.C.; Sinden, K.E.; Richardson, J.; Tang, A. Psychometric properties of the Zephyr bioharness device: A systematic review. BMC Sports Sci Med. Rehabil. 2018, 10, 6. [Google Scholar] [CrossRef]
- Chapman, C.L.; A Schafer, E.; Potter, A.W.; Lavoie, E.M.; Roberts, B.M.; Castellani, J.W.; E Friedl, K.; Looney, D.P. Day-to-day reliability of basal heart rate and short-term and ultra short-term heart rate variability assessment by the Equivital eq02+ LifeMonitor in US Army soldiers. BMJ Mil. Health 2024, 14, e002687. [Google Scholar] [CrossRef]
| Advantages | Disadvantages |
|---|---|
| Enables personalized medical treatments based on genomic and physiological data | Requires complex data integration and high infrastructure investment |
| Improves early detection of illness or injury risk through biomarker analysis | Raises ethical concerns regarding data privacy, consent, and ownership |
| Optimizes rehabilitation and return-to-duty timelines via real-time biometric feedback | May lead to over-reliance on technology in decision-making processes |
| Reduces adverse drug reactions through individualized pharmacogenomics | Logistical challenges in deploying and maintaining advanced systems in the field |
| Enhances operational readiness and resilience across diverse environments | Potential inequality in access or benefit depending on technological availability |
| Technology/Device | Parameters Monitored | Measurement Accuracy | Operational Range/Environment | Battery Life | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Equivital EQ02+ LifeMonitor | ECG, HR, RR, skin temperature, activity | HR: ±1 bpm, Temp: ±0.1 °C | −20 °C to +55 °C, up to 95% RH | 48–72 h | High accuracy; proven in field trials; rugged | Limited biochemical sensing; chest-strap form factor may cause discomfort |
| Zephyr BioHarness 3 | HR, RR, posture, activity, skin temperature | HR: ±1 bpm, Temp: ±0.2 °C | −10 °C to +50 °C | ~26 h | Lightweight; wireless connectivity | Short battery life; limited biochemical data |
| Hexoskin Smart Shirt | ECG, RR, activity, sleep metrics | HR: ±1 bpm | −5 °C to +40 °C | ~30 h | Comfortable garment integration | Not fully ruggedized for extreme environments |
| BodyCap e-Celsius® Performance | Core body temperature | ±0.2 °C | −20 °C to +50 °C | ~20 h continuous | Ingestible capsule; precise internal measurement | Single-use; no multi-parameter capability |
| Kenzen Patch | Hydration status, sweat electrolyte analysis | ±2% hydration | −10 °C to +45 °C | 24–48 h | Real-time biochemical feedback | Adhesive lifespan limits use; less robust in extreme sweat/heat |
| Garmin Tactix Delta Solar | HR, GPS, SpO2, environmental data | HR: ±3 bpm, SpO2: ±2% | −20 °C to +50 °C | Weeks (solar assist) | Long battery; integrated navigation | Consumer-grade accuracy; limited clinical validation |
| WearableMil Prototype | HRV, lactate, joint load, gait analysis | HR: ±1 bpm, Lactate: ±0.5 mmol/L | −20 °C to +50 °C | 36–48 h | Multi-parameter; AI injury prediction | Prototype stage; requires validation |
| Dimension | Civilian-Oriented Systems | Military-Oriented Systems |
|---|---|---|
| Primary Purpose | Fitness tracking, wellness monitoring, chronic disease management | Operational readiness, injury/illness prevention, mission performance optimization |
| Design Environment | Controlled, low-risk daily settings (home, gym, hospital) | Extreme environments (heat, cold, altitude, high humidity, combat stress) |
| Durability & Ruggedization | Consumer-grade; limited water/sweat resistance | Military-grade; resistant to shock, dust, extreme temperatures, and electromagnetic interference |
| Data Accuracy Requirements | Moderate (e.g., ±5 bpm HR, ±1 °C skin temp sufficient for wellness) | High precision (e.g., ±1 bpm HR, ±0.2 °C core temp, hydration ±2%) for mission-critical decisions |
| Battery Life | Optimized for daily use (12–72 h typical) | Extended endurance (≥48–72 h continuous use, sometimes weeks with solar assist) |
| Connectivity | Cloud-based, commercial networks (Bluetooth/Wi-Fi) | Secure, encrypted tactical communication systems; often works offline with edge computing |
| Ethical/Privacy Concerns | Focus on consumer consent, data-sharing policies | Involves chain-of-command oversight, limited autonomy, heightened risks of coercion or misuse |
| Examples | Apple Watch, Fitbit, Oura Ring, Hexoskin Smart Shirt | Equivital EQ02+, Zephyr BioHarness, WearableMil, BodyCap e-Celsius® |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sipos, D.; Vészi, K.; Bogár, B.; Pető, D.; Füredi, G.; Betlehem, J.; Pandur, A.A. Physiological State Monitoring in Advanced Soldiers: Precision Health Strategies for Modern Military Operations. Sci 2025, 7, 137. https://doi.org/10.3390/sci7040137
Sipos D, Vészi K, Bogár B, Pető D, Füredi G, Betlehem J, Pandur AA. Physiological State Monitoring in Advanced Soldiers: Precision Health Strategies for Modern Military Operations. Sci. 2025; 7(4):137. https://doi.org/10.3390/sci7040137
Chicago/Turabian StyleSipos, David, Kata Vészi, Bence Bogár, Dániel Pető, Gábor Füredi, József Betlehem, and Attila András Pandur. 2025. "Physiological State Monitoring in Advanced Soldiers: Precision Health Strategies for Modern Military Operations" Sci 7, no. 4: 137. https://doi.org/10.3390/sci7040137
APA StyleSipos, D., Vészi, K., Bogár, B., Pető, D., Füredi, G., Betlehem, J., & Pandur, A. A. (2025). Physiological State Monitoring in Advanced Soldiers: Precision Health Strategies for Modern Military Operations. Sci, 7(4), 137. https://doi.org/10.3390/sci7040137







