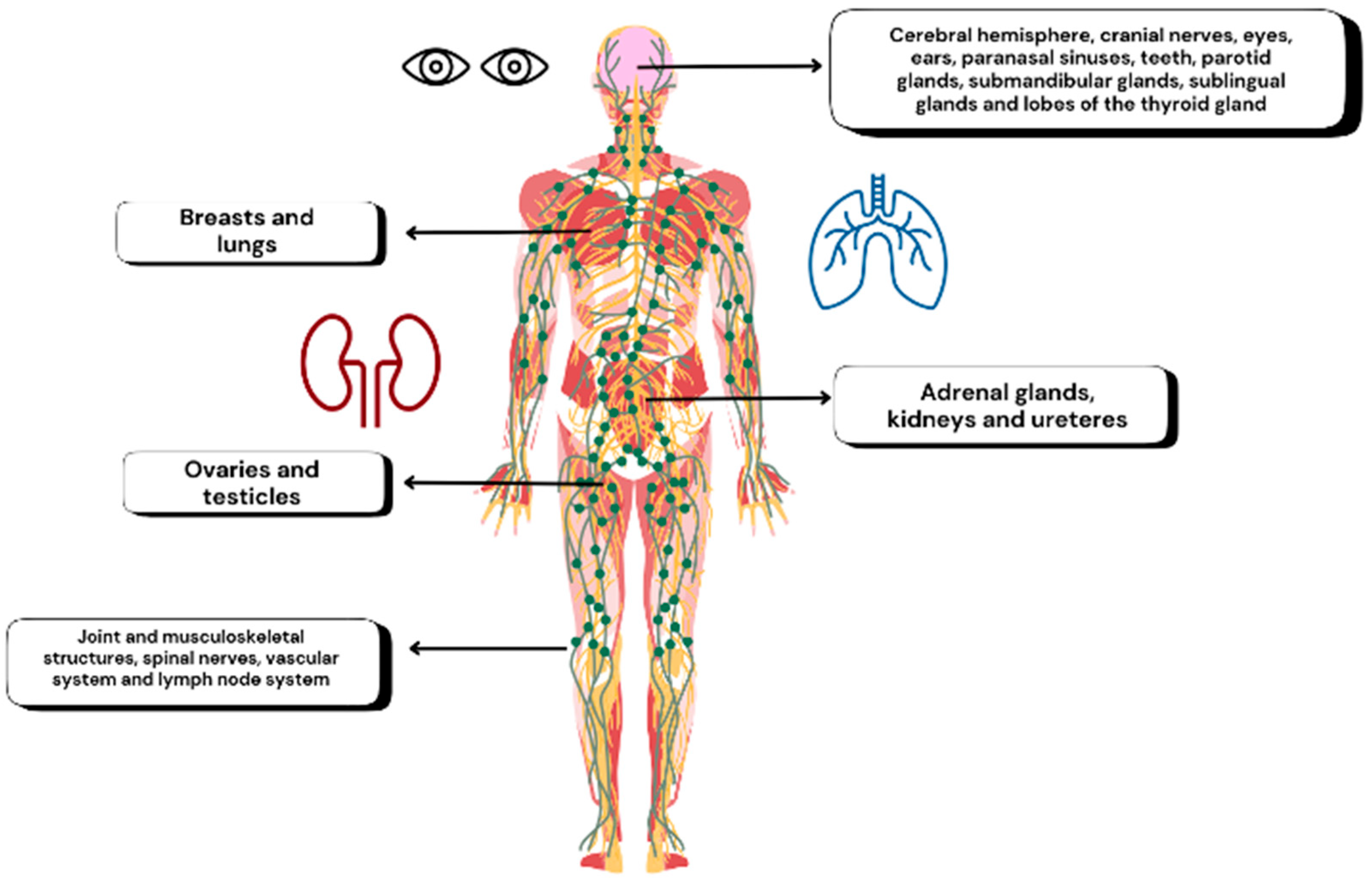
Lessons from Ophthalmology in Preventing Wrong-Site Errors in Paired-Organ Surgery
Abstract
1. Introduction
2. Methods
3. Main Surgical Errors in Ophthalmology
3.1. Historical Background and Overall Prevalence
3.2. Types of Errors
3.3. Key Contributing Factors
4. Interventions to Reduce Wrong-Site Errors
4.1. Standardized Safety Protocols
4.2. Continuous Training and Team Communication
4.3. Technology Support and Future Innovations
4.4. Shared Responsibility and the Culture of Safety
5. Case Study on Intravitreal Injections
5.1. Growing Volume and Underreported Errors
5.2. Common Pitfalls and Strategies
6. Medicolegal Implications
7. Future Directions and Challenges
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AIRS | Advanced Incident Reporting System |
| AR | Augmented reality |
| JCAHO | Joint Commission on Accreditation of Healthcare Organizations |
| NHS | National Health Service |
| NPSA | National Patient Safety Agency |
| NRLS | National Reporting and Learning System |
| WPSEs | Wrong-side/wrong-site, wrong-procedure, and wrong-patient adverse events |
| IOL | Intraocular lens |
| YOLOv3 | You Only Look Once version 3 (a deep learning model) |
| VGG-16 | Visual Geometry Group-16 (a convolutional neural network model) |
| SEIPS | Systems Engineering Initiative for Patient Safety |
| COPIC | Colorado Physicians Insurance Company database |
| VEGF | Vascular endothelial growth factor |
| AMD | Age-related macular degeneration |
| WHO | World Health Organization |
References
- Clarke, J.R.; Johnston, J.; Blanco, M.; Martindell, D.P. Wrong-Site Surgery: Can We Prevent It? Adv. Surg. 2008, 42, 13–31. [Google Scholar] [CrossRef] [PubMed]
- Kumar, J.; Raina, R. ‘Never Events in Surgery’: Mere Error or an Avoidable Disaster. Indian J. Surg. 2017, 79, 238. [Google Scholar] [CrossRef] [PubMed]
- Haynes, A.B.; Weiser, T.G.; Berry, W.R.; Lipsitz, S.R.; Breizat, A.-H.S.; Dellinger, E.P.; Herbosa, T.; Joseph, S.; Kibatala, P.L.; Lapitan, M.C.M.; et al. A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population. N. Engl. J. Med. 2009, 360, 491–499. [Google Scholar] [CrossRef] [PubMed]
- de Vries, E.N.; Prins, H.A.; Crolla, R.M.P.H.; den Outer, A.J.; van Andel, G.; van Helden, S.H.; Schlack, W.S.; van Putten, M.A.; Gouma, D.J.; Dijkgraaf, M.G.W.; et al. Effect of a Comprehensive Surgical Safety System on Patient Outcomes. N. Engl. J. Med. 2010, 363, 1928–1937. [Google Scholar] [CrossRef]
- Neily, J.; Mills, P.D.; Young-Xu, Y.; Carney, B.T.; West, P.; Berger, D.H.; Mazzia, L.M.; Paull, D.E.; Bagian, J.P. Association between Implementation of a Medical Team Training Program and Surgical Mortality. JAMA 2010, 304, 1693–1700. [Google Scholar] [CrossRef]
- Stahel, P.F.; Sabel, A.L.; Victoroff, M.S.; Varnell, J.; Lembitz, A.; Boyle, D.J.; Clarke, T.J.; Smith, W.R.; Mehler, P.S. Wrong-Site and Wrong-Patient Procedures in the Universal Protocol Era: Analysis of a Prospective Database of Physician Self-Reported Occurrences. Arch. Surg. 2010, 145, 978–984. [Google Scholar] [CrossRef]
- Omar, I.; Singhal, R.; Wilson, M.; Parmar, C.; Khan, O.; Mahawar, K. Common General Surgical Never Events: Analysis of NHS England Never Event Data. Int. J. Qual. Health Care 2021, 33, mzab045. [Google Scholar] [CrossRef]
- Patient Safety. Available online: https://www.who.int/news-room/fact-sheets/detail/patient-safety (accessed on 16 May 2025).
- Panagioti, M.; Khan, K.; Keers, R.N.; Abuzour, A.; Phipps, D.; Kontopantelis, E.; Bower, P.; Campbell, S.; Haneef, R.; Avery, A.J.; et al. Prevalence, Severity, and Nature of Preventable Patient Harm across Medical Care Settings: Systematic Review and Meta-Analysis. BMJ 2019, 366, L4185. [Google Scholar] [CrossRef]
- Martin, G.C.; Tanoubi, I.; Barjol, A.; Cruz Panesso, I.; Jannin, P.; Hardy, I.; Mouriaux, F. Beyond the Microscope: Embracing Soft Skills in Ophthalmology for Enhanced Patient Care and Clinician Well-Being. Eye 2024, 38, 2485–2487. [Google Scholar] [CrossRef]
- Medress, Z.A.; Jin, M.C.; Feng, A.; Varshneya, K.; Veeravagu, A. Medical Malpractice in Spine Surgery: A Review. Neurosurg. Focus. 2020, 49, e16. [Google Scholar] [CrossRef]
- Banschbach, S.K. Revisiting the Universal Protocol. AORN J. 2009, 89, 257–259. [Google Scholar] [CrossRef] [PubMed]
- Maloley, L.; Morgan, L.A.; High, R.; Suh, D.W. Wrong-Site Surgery in Pediatric Ophthalmology. J. Pediatr. Ophthalmol. Strabismus 2018, 55, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Elston, D.M. Cognitive Bias and Medical Errors. J. Am. Acad. Dermatol. 2019, 81, 1249. [Google Scholar] [CrossRef] [PubMed]
- Dixon-Woods, M. Why Is Patient Safety so Hard? A Selective Review of Ethnographic Studies. J. Health Serv. Res. Policy 2010, 15 (Suppl. S1), 11–16. [Google Scholar] [CrossRef]
- Lippera, M.; Bijon, J.; Eandi, C.; Virgili, G. Patient Safety in Ophthalmology. In Textbook of Patient Safety and Clinical Risk Management; Springer: Berlin/Heidelberg, Germany, 2020; pp. 339–361. [Google Scholar] [CrossRef]
- Munavalli, J.R.; Rao, S.V.; Srinivasan, A.; Srinivas, A.; van Merode, F. The Optimization in Workflow Management. J. Health Manag. 2016, 18, 21–30. [Google Scholar] [CrossRef]
- Honavar, S.G. To Err Is Human, but Errors Can Be Prevented. Indian. J. Ophthalmol. 2019, 67, 1517–1518. [Google Scholar] [CrossRef]
- Parikh, R.; Palmer, V.; Kumar, A.; Simon, J.W. Surgical Confusions in Ophthalmology: Description, Analysis, and Prevention of Errors from 2006 through 2017. Ophthalmology 2020, 127, 296–302. [Google Scholar] [CrossRef]
- Abdulkareem, I.H. The Surgical Waiting Time Initiative: A Review of the Nigerian Situation. Niger. Med. J. 2014, 55, 443–451. [Google Scholar] [CrossRef]
- Hull, L.; Arora, S.; Amaya, A.C.; Wheelock, A.; Gaitán-Duarte, H.; Vincent, C.; Sevdalis, N. Building Global Capacity for Patient Safety: A Training Program for Surgical Safety Research in Developing and Transitional Countries. Int. J. Surg. 2012, 10, 493–499. [Google Scholar] [CrossRef]
- Wilson, R.M.; Michel, P.; Olsen, S.; Gibberd, R.W.; Vincent, C.; El-Assady, R.; Rasslan, O.; Qsous, S.; Macharia, W.M.; Sahel, A.; et al. Patient Safety in Developing Countries: Retrospective Estimation of Scale and Nature of Harm to Patients in Hospital. BMJ 2012, 344, e832. [Google Scholar] [CrossRef]
- Traquair, H.M. Removal of the Wrong Eye. Br. J. Ophthalmol. 1947, 31, 8–12. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.W. Preventing Surgical Confusions in Ophthalmology (an American Ophthalmological Society Thesis). Trans. Am. Ophthalmol. Soc. 2007, 105, 513–529. [Google Scholar] [PubMed]
- Shen, E.; Porco, T.; Rutar, T. Errors in Strabismus Surgery. JAMA Ophthalmol. 2013, 131, 75–79. [Google Scholar] [CrossRef] [PubMed]
- Seiden, S.C.; Barach, P. Wrong-Side/Wrong-Site, Wrong-Procedure, and Wrong-Patient Adverse Events: Are They Preventable? Arch. Surg. 2006, 141, 931–939. [Google Scholar] [CrossRef]
- Loh, H.P.; de Korne, D.F.; Chee, S.P.; Mathur, R. Reducing Wrong Intraocular Lens Implants in Cataract Surgery. Int. J. Health Care Qual. Assur. 2017, 30, 492–505. [Google Scholar] [CrossRef]
- Devine, J.; Chutkan, N.; Norvell, D.C.; Dettori, J.R. Avoiding Wrong Site Surgery: A Systematic Review. Spine 2010, 35, S28–S36. [Google Scholar] [CrossRef]
- Kelly, S.P.; Barua, A. A Review of Safety Incidents in England and Wales for Vascular Endothelial Growth Factor Inhibitor Medications. Eye 2011, 25, 710–716. [Google Scholar] [CrossRef]
- Cavallini, G.M.; Campi, L.; De Maria, M.; Forlini, M. Clinical Risk Management in Eye Outpatient Surgery: A New Surgical Safety Checklist for Cataract Surgery and Intravitreal Anti-VEGF Injection. Graefes Arch. Clin. Exp. Ophthalmol. 2013, 251, 889–894. [Google Scholar] [CrossRef]
- White, M.M.; Gupta, M.; Utman, S.A.K.; Dhillon, B. Importance of Side Marking in Ophthalmic Surgery. Surgeon 2009, 7, 82–85. [Google Scholar] [CrossRef]
- Woolf, S.H.; Kuzel, A.J.; Dovey, S.M.; Phillips, R.L. A String of Mistakes: The Importance of Cascade Analysis in Describing, Counting, and Preventing Medical Errors. Ann. Fam. Med. 2004, 2, 317–326. [Google Scholar] [CrossRef]
- Saufl, N.M. Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. J. Perianesth Nurs. 2004, 19, 348–351. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Li, Y.I.; Pieters, T.A.; Towner, J.; Li, K.Z.; Al-Dhahir, M.A.; Childers, F.; Li, Y.M. Sepsis and Septic Shock after Craniotomy: Predicting a Significant Patient Safety and Quality Outcome Measure. PLoS ONE 2020, 15, e0235273. [Google Scholar] [CrossRef] [PubMed]
- Simon, J.W.; Ngo, Y.; Khan, S.; Strogatz, D. Surgical Confusions in Ophthalmology. Arch. Ophthalmol. 2007, 125, 1515–1522. [Google Scholar] [CrossRef] [PubMed]
- Reason, J. Safety in the Operating Theatre—Part 2: Human Error and Organisational Failure. Qual. Saf. Health Care 2005, 14, 56–60. [Google Scholar] [CrossRef]
- Treadwell, J.R.; Lucas, S.; Tsou, A.Y. Surgical Checklists: A Systematic Review of Impacts and Implementation. BMJ Qual. Saf. 2014, 23, 299–318. [Google Scholar] [CrossRef]
- Garnerin, P.; Arès, M.; Huchet, A.; Clergue, F. Verifying Patient Identity and Site of Surgery: Improving Compliance with Protocol by Audit and Feedback. Qual. Saf. Health Care 2008, 17, 454–458. [Google Scholar] [CrossRef]
- Alexander, P.; Poulson, A. V National Patient Safety Agency Protocol for Preoperative Site Marking. Br. J. Ophthalmol. 2007, 91, 124. [Google Scholar]
- Giles, S.J.; Rhodes, P.; Clements, G.; Cook, G.A.; Hayton, R.; Maxwell, M.J.; Sheldon, T.A.; Wright, J. Experience of Wrong Site Surgery and Surgical Marking Practices among Clinicians in the UK. Qual. Saf. Health Care 2006, 15, 363–368. [Google Scholar] [CrossRef]
- Lingard, L.; Regehr, G.; Orser, B.; Reznick, R.; Baker, G.R.; Doran, D.; Espin, S.; Bohnen, J.; Whyte, S. Evaluation of a Preoperative Checklist and Team Briefing among Surgeons, Nurses, and Anesthesiologists to Reduce Failures in Communication. Arch. Surg. 2008, 143, 12–17. [Google Scholar] [CrossRef]
- NHS England. National Patient Safety Incident Reports. Available online: https://www.england.nhs.uk/patient-safety/national-patient-safety-incident-reports/ (accessed on 27 February 2025).
- Kiuchi, G.; Tanabe, M.; Nagata, K.; Ishitobi, N.; Tabuchi, H.; Oshika, T. Deep Learning-Based System for Preoperative Safety Management in Cataract Surgery. J. Clin. Med. 2022, 11, 5397. [Google Scholar] [CrossRef]
- Aydındoğan, G.; Kavaklı, K.; Şahin, A.; Artal, P.; Ürey, H. Applications of Augmented Reality in Ophthalmology [Invited]. Biomed. Opt. Express 2021, 12, 511–538. [Google Scholar] [CrossRef] [PubMed]
- Mak, S.T. Sentinel Events in Ophthalmology: Experience from Hong Kong. J. Ophthalmol. 2015, 2015, 454096. [Google Scholar] [CrossRef] [PubMed]
- White, M.M.; Gupta, M.; Dhillon, B. Patient Safety and Ophthalmic Surgery Marking: Which Side Are You On? Br. J. Ophthalmol. 2007, 91, 123–124. [Google Scholar] [PubMed]
- Poore, S.O.; Sillah, N.M.; Mahajan, A.Y.; Gutowski, K.A. Patient Safety in the Operating Room: I. Preoperative. Plast. Reconstr. Surg. 2012, 130, 1038–1047. [Google Scholar] [CrossRef]
- Hempel, S.; Maggard-Gibbons, M.; Nguyen, D.K.; Dawes, A.J.; Miake-Lye, I.; Beroes, J.M.; Booth, M.J.; Miles, J.N.V.; Shanman, R.; Shekelle, P.G. Wrong-Site Surgery, Retained Surgical Items, and Surgical Fires: A Systematic Review of Surgical Never Events. JAMA Surg. 2015, 150, 796–805. [Google Scholar] [CrossRef]
- Steeples, L.R.; Hingorani, M.; Flanagan, D.; Kelly, S.P. Wrong Intraocular Lens Events-What Lessons Have We Learned? A Review of Incidents Reported to the National Reporting and Learning System: 2010–2014 versus 2003–2010. Eye 2016, 30, 1049–1055. [Google Scholar] [CrossRef]
- Paull, D.E.; Mazzia, L.M.; Wood, S.D.; Theis, M.S.; Robinson, L.D.; Carney, B.; Neily, J.; Mills, P.D.; Bagian, J.P. Briefing Guide Study: Preoperative Briefing and Postoperative Debriefing Checklists in the Veterans Health Administration Medical Team Training Program. Am. J. Surg. 2010, 200, 620–623. [Google Scholar] [CrossRef]
- Elwy, A.R.; Bokhour, B.G.; Maguire, E.M.; Wagner, T.H.; Asch, S.M.; Gifford, A.L.; Gallagher, T.H.; Durfee, J.M.; Martinello, R.A.; Schiffner, S.; et al. Improving Healthcare Systems’ Disclosures of Large-Scale Adverse Events: A Department of Veterans Affairs Leadership, Policymaker, Research and Stakeholder Partnership. J. Gen. Intern. Med. 2014, 29 (Suppl. S4), 895–903. [Google Scholar] [CrossRef]
- Gagliardi, A.R.; Straus, S.E.; Shojania, K.G.; Urbach, D.R. Multiple Interacting Factors Influence Adherence, and Outcomes Associated with Surgical Safety Checklists: A Qualitative Study. PLoS ONE 2014, 9, e108585. [Google Scholar] [CrossRef]
- Yoo, T.K.; Oh, E.; Kim, H.K.; Ryu, I.H.; Lee, I.S.; Kim, J.S.; Kim, J.K. Deep Learning-Based Smart Speaker to Confirm Surgical Sites for Cataract Surgeries: A Pilot Study. PLoS ONE 2020, 15, e0231322. [Google Scholar] [CrossRef]
- Tabuchi, H.; Ishitobi, N.; Deguchi, H.; Nakaniida, Y.; Tanaka, H.; Akada, M.; Tanabe, M. Large-Scale Observational Study of AI-Based Patient and Surgical Material Verification System in Ophthalmology: Real-World Evaluation in 37 529 Cases. BMJ Qual. Saf. 2024. [Google Scholar] [CrossRef] [PubMed]
- Grzybowski, A.; Schwartz, S.G.; Kishor, K.S.; Villegas, M.; Leffler, C.; Olawade, D.B.; Weerasinghe, K.; Don, M.; Mathugamage, D.E.; Odetayo, A.; et al. Enhancing Ophthalmic Diagnosis and Treatment with Artificial Intelligence. Medicina 2025, 61, 433. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.; Huang, X.; Sheng, Y.; Tang, N.; Lian, H.; Zhang, W.; Zhao, L.; Zhu, H.; Chang, P.; Guo, Y. Intelligent Verification Tool for Surgical Information of Ophthalmic Patients—A Study Based on Artificial Intelligence Technology. J. Patient Saf. 2024, 21, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Carlà, M.M.; Gambini, G.; Giannuzzi, F.; Boselli, F.; De Luca, L.; Rizzo, S. Testing the Reliability of ChatGPT Assistance for Surgical Choices in Challenging Glaucoma Cases. J. Pers. Med. 2025, 15, 97. [Google Scholar] [CrossRef]
- Robinson, A.; Aggarwal, S. When Precision Meets Penmanship: ChatGPT and Surgery Documentation. Cureus 2023, 15, e40546. [Google Scholar] [CrossRef]
- Ferrara, E. Fairness and Bias in Artificial Intelligence: A Brief Survey of Sources, Impacts, and Mitigation Strategies. Sci. 2024, 6, 3. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Lin, C.-H.; Fan, C.-H.; Long, A.J.; Scholl, J.; Kao, Y.-P.; Iqbal, U.; Li, Y.-C.J. Machine Learning Approach to Identifying Wrong-Site Surgeries Using Centers for Medicare and Medicaid Services Dataset: Development and Validation Study. JMIR Form. Res. 2025, 9, e68436. [Google Scholar] [CrossRef]
- Nazari, H.; Modarres, M.; Parvaresh, M.M.; Ghasemi Falavarjani, K. Intravitreal Bevacizumab in Combination with Laser Therapy for the Treatment of Severe Retinopathy of Prematurity (ROP) Associated with Vitreous or Retinal Hemorrhage. Graefes Arch. Clin. Exp. Ophthalmol. 2010, 248, 1713–1718. [Google Scholar] [CrossRef]
- Visioli, G.; Alisi, L.; Mastrogiuseppe, E.; Albanese, G.M.; Romano, E.; Iannetti, L.; Armentano, M.; Giovannetti, F.; Gharbiya, M. OCT Biomarkers as Predictors of Visual Improvement in Diabetic Macular Edema Eyes Receiving Dexamethasone Implants. Int. J. Retin. Vitr. 2023, 9, 35. [Google Scholar] [CrossRef]
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.; et al. Global Causes of Blindness and Distance Vision Impairment 1990-2020: A Systematic Review and Meta-Analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef]
- Kelly, S.P.; Jalil, A. Wrong Intraocular Lens Implant; Learning from Reported Patient Safety Incidents. Eye 2011, 25, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Kato, K.; Matsumura, Y. Enhancing Safety in Ophthalmic Surgery: Database Analysis of Intraocular Lens Implantations in Japan for Classification of Human Errors. Human Factors Healthc. 2025, 7, 100103. [Google Scholar] [CrossRef]
- Gragoudas, E.S.; Adamis, A.P.; Cunningham, E.T.; Feinsod, M.; Guyer, D.R.; VEGF Inhibition Study in Ocular Neovascularization Clinical Trial Group. Pegaptanib for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2004, 351, 2805–2816. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, P.J.; Brown, D.M.; Heier, J.S.; Boyer, D.S.; Kaiser, P.K.; Chung, C.Y.; Kim, R.Y.; MARINA Study Group. Ranibizumab for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2006, 355, 1419–1431. [Google Scholar] [CrossRef]
- Brown, D.M.; Kaiser, P.K.; Michels, M.; Soubrane, G.; Heier, J.S.; Kim, R.Y.; Sy, J.P.; Schneider, S.; ANCHOR Study Group. Ranibizumab versus Verteporfin for Neovascular Age-Related Macular Degeneration. N. Engl. J. Med. 2006, 355, 1432–1444. [Google Scholar] [CrossRef]
- Scott, I.U.; Flynn, H.W. Reducing the Risk of Endophthalmitis Following Intravitreal Injections. Retina 2007, 27, 10–12. [Google Scholar] [CrossRef]
- Fintak, D.R.; Shah, G.K.; Blinder, K.J.; Regillo, C.D.; Pollack, J.; Heier, J.S.; Hollands, H.; Sharma, S. Incidence of Endophthalmitis Related to Intravitreal Injection of Bevacizumab and Ranibizumab. Retina 2008, 28, 1395–1399. [Google Scholar] [CrossRef]
- Mason, J.O.; White, M.F.; Feist, R.M.; Thomley, M.L.; Albert, M.A.; Persaud, T.O.; Yunker, J.J.; Vail, R.S. Incidence of Acute Onset Endophthalmitis Following Intravitreal Bevacizumab (Avastin) Injection. Retina 2008, 28, 564–567. [Google Scholar] [CrossRef]
- Pilli, S.; Kotsolis, A.; Spaide, R.F.; Slakter, J.; Freund, K.B.; Sorenson, J.; Klancnik, J.; Cooney, M. Endophthalmitis Associated with Intravitreal Anti-Vascular Endothelial Growth Factor Therapy Injections in an Office Setting. Am. J. Ophthalmol. 2008, 145, 879–882. [Google Scholar] [CrossRef]
- Chao, D.L.; Gregori, N.Z.; Khandji, J.; Goldhardt, R. Safety of Bilateral Intravitreal Injections Delivered in a Teaching Institution. Expert Opin. Drug Deliv. 2014, 11, 991–993. [Google Scholar] [CrossRef]
- Mazzuca, D.; Borselli, M.; Gratteri, S.; Zampogna, G.; Feola, A.; Della Corte, M.; Guarna, F.; Scorcia, V.; Giannaccare, G. Applications and Current Medico-Legal Challenges of Telemedicine in Ophthalmology. Int. J. Environ. Res. Public Health 2022, 19, 5614. [Google Scholar] [CrossRef] [PubMed]
- Shahbaz, R.; Salducci, M. Law and Order of Modern Ophthalmology: Teleophthalmology, Smartphones Legal and Ethics. Eur. J. Ophthalmol. 2020, 31, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Kahan, E.H.; Shin, J.D.; Jansen, M.E.; Parker, R.H.; Parikh, R. Malpractice Cases Arising From Telephone Based Telemedicine Triage in Ophthalmology. Semin. Ophthalmol. 2023, 38, 294–305. [Google Scholar] [CrossRef] [PubMed]
- Kirthi, V.; Neffendorf, J.E.; Navaratnam, A.V.; Machin, J.T.; Hingorani, M.; Briggs, T.W.R.; Davis, A.; MacEwen, C.; Jackson, T.L. Litigation in Ophthalmology against the National Health Service in England. Ophthalmology 2021, 128, 1487–1489. [Google Scholar] [CrossRef]
- Traina, F. Medical Malpractice: The Experience in Italy. Clin. Orthop. Relat. Res. 2009, 467, 434–442. [Google Scholar] [CrossRef]
- Ferorelli, D.; Spagnolo, L.; Misceo, F.; Silvestre, M.; Corradi, S.; Benevento, M.; Polo, L.; Marrone, M.; Crudele, L.; Zotti, F.; et al. Medico-Legal Suggestions for Young Doctors: The Application of Clinical Risk Management to Reduce the Risk of Litigation and Create an Environment of Trust. EuroMediterranean Biomed. J. 2021, 16, 52–57. [Google Scholar] [CrossRef]
- Smith, J.D.; Lemay, K.; Lee, S.; Nuth, J.; Ji, J.; Montague, K.; Garber, G.E. Medico-Legal Issues Related to Emergency Physicians’ Documentation in Canadian Emergency Departments. Can. J. Emerg. Med. 2023, 25, 768–775. [Google Scholar] [CrossRef]
- Unwin, E.; Woolf, K.; Wadlow, C.; Potts, H.W.W.; Dacre, J. Sex Differences in Medico-Legal Action against Doctors: A Systematic Review and Meta-Analysis. BMC Med. 2015, 13, 172. [Google Scholar] [CrossRef]
- Casey, G.; Lemay, K.; Ji, J.; Yang, Q.; MacIntyre, A.; Heroux, D.; Garber, G. Medico-Legal Cases Associated with Older Physicians’ Cognitive Ability to Practice Medicine. J. Healthc. Risk Manag. 2024, 43, 14–17. [Google Scholar] [CrossRef]
- McKinnon, K. Doctoring with Bureaucracy. In Birthing Work; Springer: Berlin/Heidelberg, Germany, 2020; pp. 69–85. [Google Scholar] [CrossRef]
- Charlton, B.G. The Cancer of Bureaucracy: How It Will Destroy Science, Medicine, Education; and Eventually Everything Else. Med. Hypotheses 2010, 74, 961–965. [Google Scholar] [CrossRef]
- Judson, D.H. Bureaucracy Hinders Prompt Care. BMJ Br. Med. J. 2003, 326, 714. [Google Scholar] [CrossRef] [PubMed]
- Petersson, L.; Larsson, I.; Nygren, J.M.; Nilsen, P.; Neher, M.; Reed, J.E.; Tyskbo, D.; Svedberg, P. Challenges to Implementing Artificial Intelligence in Healthcare: A Qualitative Interview Study with Healthcare Leaders in Sweden. BMC Health Serv. Res. 2022, 22, 850. [Google Scholar] [CrossRef] [PubMed]
- Peña, A.; Sepúlveda-Cano, L.M.; Gonzalez-Ruiz, J.D.; Marín-Rodríguez, N.J.; Botero-Botero, S. Deep Fuzzy Credibility Surfaces for Integrating External Databases in the Estimation of Operational Value at Risk. Sci 2024, 6, 74. [Google Scholar] [CrossRef]
- Park, J.; Chung, S.; An, H.; Park, S.; Lee, C.; Kim, S.Y.; Lee, J.D.; Kim, K.S. A Structural Model of Stress, Motivation, and Academic Performance in Medical Students. Psychiatry Investig. 2012, 9, 143. [Google Scholar] [CrossRef]

| Strategy | Content | Suggested by | Outcome | Reference |
|---|---|---|---|---|
| Standardized Security Protocols | Surgical checklist, Surgical Patient Safety System (SURPASS), WHO Surgical Safety Checklist | Joint Commission Universal Protocol | Improved compliance in identity verification (9.7% to 38.1%) and surgical site checks (32.2% to 52%) in Geneva hospitals. Reduction in postoperative complications from 27.3% to 16.7% in Dutch hospitals after implementing SURPASS. | [3,4,37,38] |
| Site Marking | Site marking protocols | Joint Commission on Accreditation of Healthcare Organizations and NPSA | Improved site-marking accuracy, reducing the incidence of wrong-site surgeries. | [39,40] |
| Continuous Training of Staff | Briefing and debriefing sessions, Medical team training programs | Canadian academic tertiary care hospitals, VHA system | One-third of briefings led to process improvements, and structured training at VHA hospitals reduced surgical errors. | [5,41] |
| Technology Support and Future Innovations | Tracking systems, Sentinel Event Database, COPIC database, Web-Based WPSE Incident Reporting Tool | NPSA and NHS England through NRLS | NHS reported 2,345,817 incidents in 2021–2022, with wrong-site surgeries increasing by 26% in 2023. COPIC database recorded 107 wrong-site procedures between 2002–2008. | [6,26,42] |
| Machine Learning | YOLOv3 algorithm and VGG-16 for laterality confirmation | Research studies on AI-based surgical safety | First-attempt authentication rate of 82.5%, increasing to 98.2% with repeated attempts. | [43] |
| Virtual and Augmented Reality | AR head-mounted display, Eye trackers, Laser marking systems for enhanced visualization | Studies on AR/VR applications in surgical training | AR-based overlays assist in reducing surgical errors, while VR simulation improves surgical precision and training. | [44] |
| Knowledge of Safety and Shared Responsibility | Data collection through AIRS (Hong Kong Hospital Authority) and Veterans’ Health Administration databases | Patient safety reporting systems | A web-based reporting system led to a decline of 0.17 events per 100,000 surgeries annually. | [5,45] |
| Error Category | Description | Impact on Process | Consequences | Cumulative Effect | References |
|---|---|---|---|---|---|
| Distraction | Environmental interruptions (door open/close, noise, calls) | Reduced focus during preoperative checks | Missed time-out and de-briefing, site identification errors | Amplifies other mistakes (e.g., fatigue + poor communication) | [1,5,6,30] |
| Stress | Time pressure, legal responsibility, ophthalmology emergencies | Incorrect decisions | Wrong side surgery, wrong patient/IOL, wrong patient/wrong eye | Increases vulnerability to existing errors | [2,5,36] |
| Fatigue | Long shifts, heavy workload | Lower attention, document-reading errors | Incorrect site marking, dosing mistakes | Increases undetected errors by others | [5,32,36] |
| Poor Communication | No briefing, no instructions, unclear documents | Incomplete checks, confusion about site/procedure | Wrong eye procedure, incorrect medication | Amplifies other errors | [4,5,32] |
| Single Error | One mistake (e.g., missed marking) | Detectable if checks are in place | Less severe if isolated | Manageable with mutual supervision | [3,30,31,39] |
| Multiple Errors | Combination of issues(e.g., distraction + poor communication) | Breaks safety checks | Major issues (wrong eye, permanent harm, vision loss) | Exponentially increases risk and damage | [6,27,36] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romaniello, A.; Blasi, F.R.; Iannetti, L.; Armentano, M.; D’Andrea, M.; Visioli, G.; Alisi, L. Lessons from Ophthalmology in Preventing Wrong-Site Errors in Paired-Organ Surgery. Sci 2025, 7, 79. https://doi.org/10.3390/sci7020079
Romaniello A, Blasi FR, Iannetti L, Armentano M, D’Andrea M, Visioli G, Alisi L. Lessons from Ophthalmology in Preventing Wrong-Site Errors in Paired-Organ Surgery. Sci. 2025; 7(2):79. https://doi.org/10.3390/sci7020079
Chicago/Turabian StyleRomaniello, Annalisa, Francesca Romana Blasi, Ludovico Iannetti, Marta Armentano, Mattia D’Andrea, Giacomo Visioli, and Ludovico Alisi. 2025. "Lessons from Ophthalmology in Preventing Wrong-Site Errors in Paired-Organ Surgery" Sci 7, no. 2: 79. https://doi.org/10.3390/sci7020079
APA StyleRomaniello, A., Blasi, F. R., Iannetti, L., Armentano, M., D’Andrea, M., Visioli, G., & Alisi, L. (2025). Lessons from Ophthalmology in Preventing Wrong-Site Errors in Paired-Organ Surgery. Sci, 7(2), 79. https://doi.org/10.3390/sci7020079






