Abstract
mHealth apps can promote behavior change to prevent heart disease. This study examined the efficacy of an 8-week theory-based mHealth intervention to promote heart disease preventive behaviors. The BaseMetrics app was designed using the Health Belief Model to improve users’ understanding of heart disease and its risk factors to promote behavior change. In this proof-of-concept intervention with no control group, twenty-two participants (14F/8M; age 51 ± 8 years) received access to the BaseMetrics app for 8 weeks. Biological, behavioral, and self-assessed heart disease risk and knowledge were measured pre- and post-intervention. At post-intervention, significant improvements were seen in self-reported fruit and vegetable intake (+1.1 servings/day) and skin carotenoids (+28 a.u.). Self-tracked activity decreased (−665 steps/day). No other outcomes were significantly different. Non-significant improvements with small-to-moderate effect sizes were observed in triglycerides, energy expenditure, knowledge, perceived risk, and perceived benefits of diet and exercise. Conversely, non-significant deteriorations with small-to-moderate effect sizes were observed for total cholesterol, LDL, and AST. This study yielded preliminary findings suggesting the benefits of the BaseMetrics mobile app for heart disease prevention. The results must be validated in a larger randomized controlled trial.
1. Introduction
The majority of cardiovascular events are preventable by controlling modifiable risk factors [1]. Unfortunately, the majority of adults continue to not engage in sufficient physical activity or consume a healthy diet. Even with the availability of effective evidence-based treatment options and guidelines for primordial and primary prevention of cardiovascular disease (CVD), patient outcomes are still poor due to non-adherence and poor self-management [2].
With the widespread adoption of smartphones across the world, they are increasingly used to deliver mobile interventions to support preventive health behaviors (mHealth). Several mHealth solutions have been developed to target various modifiable CVD risk factors or conditions [3]. Recent systematic reviews and meta-analyses have shown that mHealth interventions can significantly improve cardiovascular risk profiles, particularly by supporting lifestyle changes such as improvements in physical activity and diet [4,5]. However, most existing apps focus on secondary prevention among patients with an existing condition or single risk factors such as blood pressure or cholesterol [6]. Few mHealth solutions have been developed or evaluated for primordial prevention, where the goal is to prevent the emergence of risk factors in healthy but at-risk individuals. Furthermore, many existing apps lack theoretical underpinnings or offer limited support for user education and risk perception enhancement, which are critical in motivating early lifestyle changes [3]. Our novel mobile app called BaseMetrics addresses these gaps by targeting multiple CVD risk factors, grounding its design in behavioral theory, and focusing on increasing risk awareness and knowledge in a healthy population.
Theory-based intervention development has been cited as a critical issue for effective mHealth interventions [7]. Most digital CVD interventions reviewed by Steinmetz et al. [3] were not based on behavior change theory. Evidence suggests that theory-based mHealth interventions are more effective in promoting behavior change [8]. To help individuals with primordial prevention of CVD, there is a need to develop effective mHealth interventions grounded in behavior change theory and targeting primary prevention.
Among various behavioral theories, we selected the Health Belief Model (HBM) as the conceptual framework for this intervention because of its specific emphasis on perceived susceptibility and perceived severity—constructs that are directly relevant to increasing the awareness of CVD risk [9]. Compared to the theory of planned behavior (TPB), which focuses more on social norms and behavioral intentions [10], or the transtheoretical model (TTM), which emphasizes the stages of readiness to change [11], the HBM aligns more closely with the app’s goal of enhancing personal risk perception and motivating initial preventive action. HBM is particularly well suited for primordial prevention contexts where individuals may not yet perceive themselves at risk and where the intervention must first elevate the perceived threat before behavior change can occur [12].
The current study examines the efficacy of a novel mHealth intervention called BaseMetrics to aid primordial cardiovascular disease prevention by positively affecting the user’s CVD-related health risk perception and knowledge. The intervention combines several relevant behavior change techniques (BCTs) to target users’ CVD health beliefs and knowledge. Our hypothesis was that our novel mHealth intervention would lead to improvements in CVD prevention knowledge and risk perception, which may precipitate improvements in dietary and physical activity behaviors.
2. Materials and Methods
2.1. Overview of Design and Procedures
This trial was conducted to preliminarily evaluate the efficacy of the BaseMetrics app mHealth intervention. Informed consent was obtained from all subjects involved in this study. Participant characteristics, including age, sex, education, and ethnicity, were collected via online questionnaires. Metabolic, behavioral, anthropometric, and self-assessed risk measurements were collected pre- and post-intervention. For this proof-of-concept study, all participants received the mHealth intervention. Thus, there was no control group, which is a limitation of this study. The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board at Oklahoma State University (IRB-20-24-STW; approved: 10 February 2020).
2.2. Participants
Convenience sampling was used to recruit participants from a Midwestern university for this 8-week intervention. An email was sent to all university employees soliciting participation in the study. Healthy individuals aged 30 to 65 years who own and regularly use a smartphone (iOS Operating System) and wear a wrist-based physical activity measuring device were recruited for this study. Individuals using an Android smartphone were excluded because the mHealth application was not available for this operating system. For the first phase of development and testing, we developed the app only for iOS due to financial and personnel development constraints, with the rationale that preliminary data would be leveraged into expanded development and testing. Individuals with existing CVD, other chronic disease conditions, or those taking associated medications were excluded.
2.3. Base Metrics App
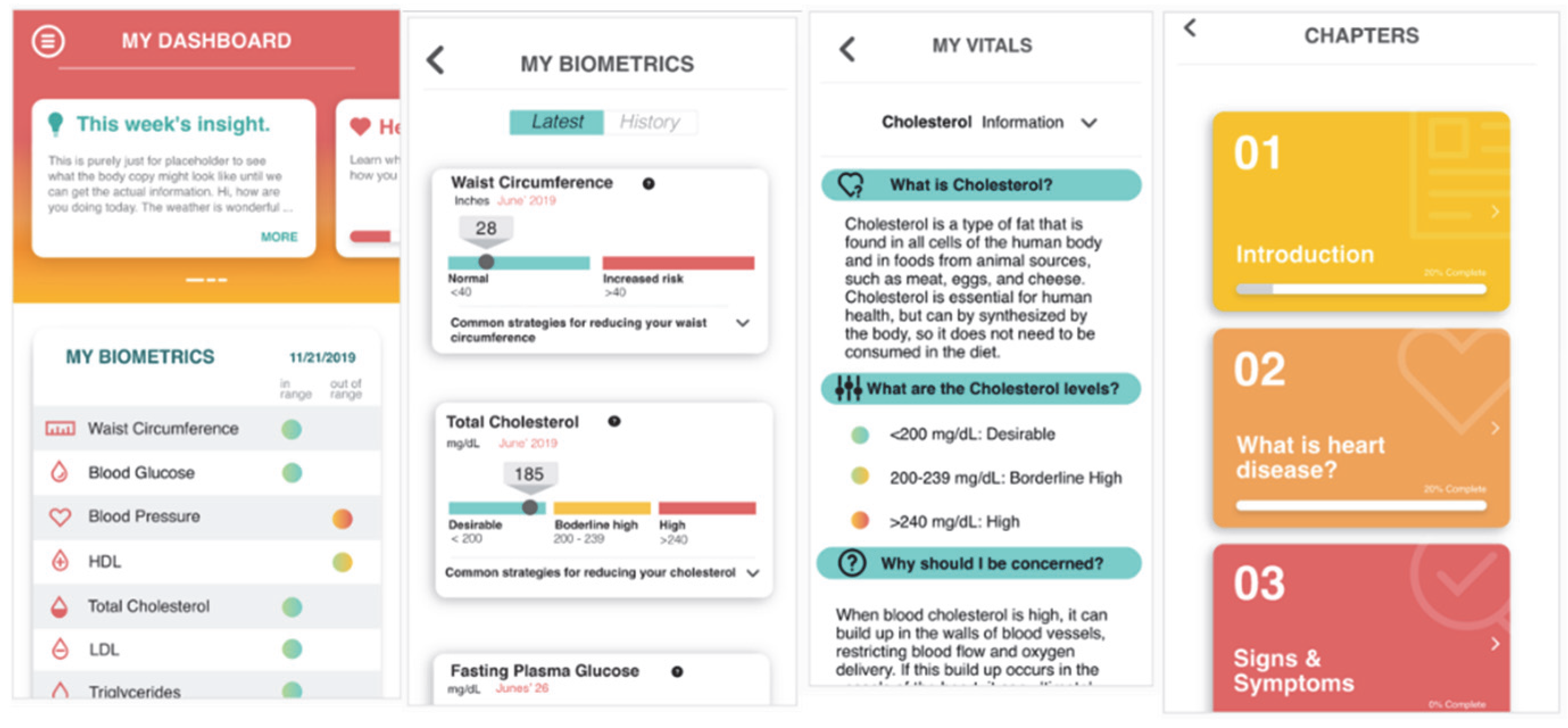
BaseMetrics (Figure 1) is a personal preventive cardiovascular health mobile application. The HBM guided the app’s design and development [9]. The HBM is a widely used framework in preventive health behavior research to explain health-related behavior and behavior change [13]. The HBM states that a person’s belief in a personal threat from an illness and perceived benefits of recommended health behavior predicts the likelihood of adopting a preventive health behavior [13]. The BaseMetrics app was developed to improve CVD knowledge, perceived susceptibility and severity of risk, perceived benefits of engaging in positive behaviors, and intent to engage in healthy behaviors to improve CVD risk factors. The app incorporates multiple BCTs, including the self-monitoring of behavior, information about health consequences, the salience of consequences, a comparison of outcomes, and instruction on how to perform a behavior [14]. The design of the BaseMetrics app was intended to provide actionable and evidence-based health information to help reduce the risk of cardiovascular disease. The app takes the user’s age, ethnicity, height, weight, and risk factor data as inputs. The app comprises four components: tracking and visualizing CVD risk factors, weekly health messages, heart health lessons, and goal setting. The weekly health messages and heart health lessons were standard for all participants. The app directed participants toward specific goals based on their entered risk factor values. The relationship between app features and incorporated BCTs is displayed in Table 1.
Figure 1.
Example screenshots from the BaseMetrics app (v.1). Far left: dashboard screen with biometric risk factor data visualization; Middle left: detailed biometric risk factor data visualization; Middle right: example of detailed risk factor description; Far right: example chapters from the heart health lessons.

Table 1.
Mapping BaseMetrics app features to behavior change theories (BCTs).
2.4. Biological Measurements
Body mass and composition were measured using a bioelectrical impedance scale (Seca mBCA 514). Height was measured with a portable stadiometer (Seca 213 stadiometer). Blood pressure was measured with a commercial automated cuff (Omron 5 series BP742N). Blood pressure was measured until two consecutive measurements that differed by ≤5 mmHg were recorded and averaged. Fasting venous blood samples were collected from a forearm vein into vacutainers containing lithium heparin. A Piccolo Xpress clinical chemistry analyzer with Lipid Panel Plus reagent cassettes was used for the measurement of metabolic markers in whole blood (100 µL per sample). Metabolic outcomes included glucose, total cholesterol, HDL cholesterol, triglycerides, ALT, and AST. Calculated outcomes included VLDL, LDL and non-HDL cholesterol. The Piccolo Xpress analyzer conducts an internal quality control analysis during each test to verify that there are no confounding effects due to hemolysis, excessive lipemia, or contaminated samples.
2.5. Behavioral Measurements
User-generated physical activity was collected as well as both self-reported and objectively measured dietary data. Specifically, all participants were required to wear a wrist-based physical activity measurement device for seven days pre- and post-intervention. At their appointment, participants reported the mobile app-measured steps per day and daily energy expenditure for seven days. Daily results for each outcome were averaged, yielding a single data value for each participant pre- and post-intervention. Regarding their diet, participants were asked to report how many estimated servings of fruits and vegetables they consumed per day over the past week, similar to what has been performed and validated previously [15,16]. A VEGGIE METER® was used for the optical measurement of skin carotenoids as a biomarker of fruit and vegetable (FV) intake via pressure-mediated reflective spectroscopy [17]. The device emits broad-spectrum white light through a fiber optic probe placed on the fingertip and measures the intensity of light reflected back from subdermal tissues. Carotenoids in the skin absorb specific wavelengths of light, resulting in a characteristic spectral fingerprint. The device uses proprietary algorithms to quantify this signal and generate a unitless carotenoid score. Measurements are taken in triplicate and averaged to reduce variability. The device has been used and validated as a proxy for fruit and vegetable intake [18,19].
2.6. Self-Assessed Risk Measurements
A validated questionnaire was utilized to evaluate participants’ self-assessed CVD risk awareness [20]. The questionnaire addressed four domains: CVD knowledge, the perceived risk of CVD, the perceived benefit of engaging in healthy behaviors, and healthy behavior intentions. Knowledge of CVD risk and prevention was assessed using 18 items, with a higher score indicating greater knowledge about cardiovascular health. The perceived risk and vulnerability of CVD was measured with 20 items in which individuals were asked to rate the extent to which they feel vulnerable to experiencing a myocardial infarction or stroke. A higher score in this domain indicates a higher perception of risk. The perceived benefit of engaging in healthy behaviors was assessed with 6 items, in which a higher score reflects higher perceived benefit. Intention to change behavior or cues to action were measured with 18 items, and a higher score indicated a higher perceived readiness for making healthy lifestyle changes. The questionnaire utilized has been validated for assessing the measured constructs [20].
2.7. Statistical Analyses
GraphPad Prism 10 was used for data analyses. Data were checked for normality using a Shapiro–Wilk normality test. Normally and non-normally distributed data were analyzed with parametric and non-parametric tests, respectively. A paired t test or Wilcoxon matched-pairs signed rank test was used to compare pre- and post-intervention results. Adjustments for multiple comparisons were not made. An alpha level of 0.05 was used to determine significant differences. Cohen’s d effect size was also calculated for each comparison. A value of 0.2 or greater was considered a small effect, while a value of 0.5 or greater was considered a moderate effect, and a value of 0.8 or greater was considered a large effect. Participants were only included if data were available at both time points for a given variable. Single time points without a matched pair were excluded from analysis.
A priori sample size estimation was not conducted for this proof-of-concept study, which we acknowledge as a limitation. We conducted a post hoc power analysis to display the statistical power present for each outcome variable. These data are displayed in Supplementary Table S1.
3. Results
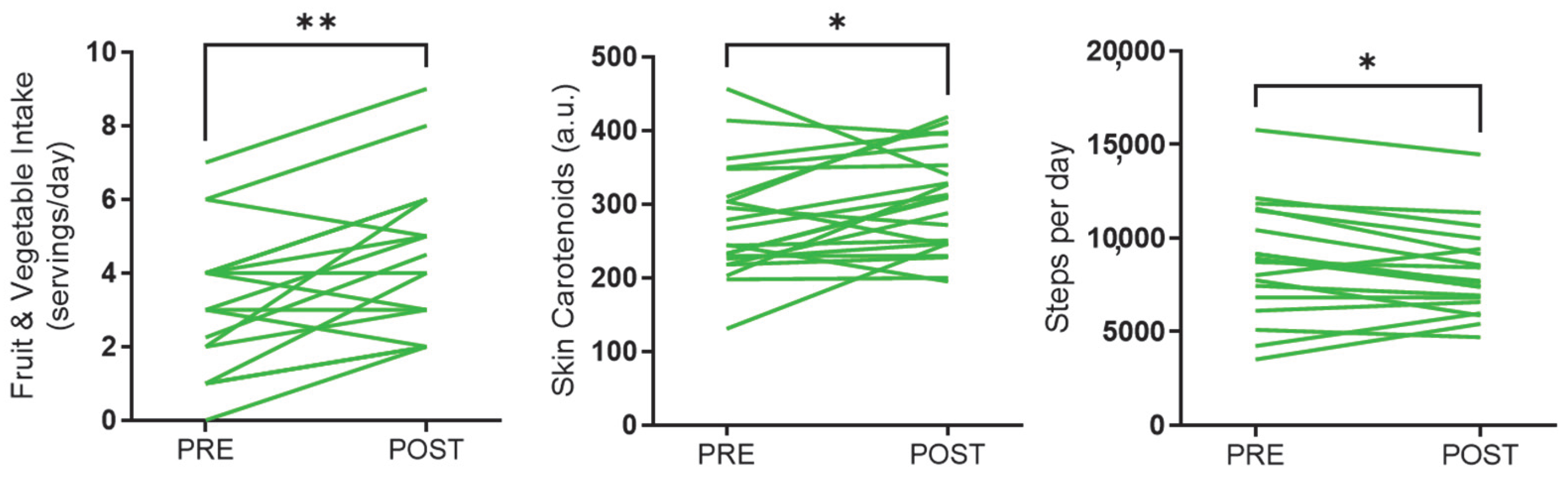
Twenty-two participants, including 14 females and 8 males, completed the study. Participant age at intervention onset was 51.4 ± 7.6 years. Pre- and post-intervention outcomes are displayed in Table 2. There were no significant differences observed in anthropometric outcomes, such as body mass, BMI, fat mass, or muscle mass. Similarly, there were no significant differences in blood pressure or metabolic risk factor outcomes. However, although non-significant, we did observe a small effect post-intervention for triglycerides (−10.9 mg/dL), total cholesterol (+9.7 mg/dL), LDL cholesterol (+11.4 mg/dL), and AST (+2.0 U/L). Steps per day significantly decreased from pre- to post-intervention (−665 steps/day) (Figure 2). On the other hand, FV intake (+1.1 servings/day) and skin carotenoids (+28.3 a.u.) significantly increased after the intervention. Although non-significant, there was a moderate effect size for energy expenditure post-intervention (+442 kcal/day). There were no significant differences in cardiovascular disease knowledge, perceived risk for myocardial infarction or stroke, perceived benefits and intentions to change, or healthy behavior intentions from pre- to post-intervention. However, there was a small but non-significant trend for cardiovascular disease knowledge (+0.33 a.u.), perceived risk (−0.67 a.u.), and perceived benefits (+0.02 a.u.).

Table 2.
Biological, behavioral, and self-assessed risk outcomes pre- and post-intervention.
Figure 2.
Individual-level changes in fruit and vegetable intake, skin carotenoids, and steps per day. Fruit and vegetable intake and skin carotenoids significantly increased, and steps per day significantly decreased from pre- to post-intervention (* p < 0.05; ** p < 0.01). Each line represents a single participant.
With respect to app usage, 68% of the users completed all the lessons in the education modules, 22% of users completed at least two lessons, and the remainder completed at least one lesson. Of the 22 participants, 12 (~55%) set at least one health goal via the mobile app. Among those who set goals, the average number of goals set per user was 2.08. The most common goals were to reduce glucose, followed by HDL, LDL, blood pressure, and waist circumference. Regarding personal risk factor entry, 40.9% of participants entered their vitals more than once, and those users averaged 8.3 vital entries during the study period. The number of times the app was opened and used during the study averaged 13.2 per week.
4. Discussion
The purpose of this study was to examine the efficacy of an eight-week theory-based mHealth behavior change intervention for aiding in the primary prevention of CVD risk factors. This study is limited by a small sample size and intervention duration, as well as a lack of randomization or a control group. Although many outcomes did not change during the intervention period, our study does provide preliminary evidence for potential benefits associated with access to the BaseMetrics app to warrant future rigorous testing.
Our study observed an increase in self-reported FV intake from pre- to post-intervention. This finding was supported by an increase in skin carotenoids measured via pressure-mediated reflective spectroscopy. Taken together, these findings suggest that access to and utilization of the BaseMetrics app may have stimulated increased FV intake. A systematic review including 23 studies reported a small positive effect of mHealth interventions on healthy eating behaviors [21]. Specifically in patients with CVD, another systematic review that included 13 studies observed that mHealth interventions improved clinically guided diet adherence [22]. Most studies included in these reviews utilized interventions longer than 8 weeks. Thus, our results agree with previous studies, suggesting that mHealth interventions may be an effective approach to promote healthy eating, despite the relatively short intervention duration utilized in the present study. Also, many past studies have studied clinical populations, whereas BaseMetrics is designed to improve health outcomes in people without a diagnosed disease. In addition, the present study is the first to our knowledge to simultaneously observe an increase in skin carotenoids. It should be noted that in this pilot study, we utilized a quick and simple assessment of fruit and vegetable intake by having participants directly self-report this outcome. Future testing of the app should include more rigorous dietary assessments, such as random 24 h recalls, in order to verify this finding.
We also observed a significant decrease in self-reported steps per day from pre- to post-intervention. Since the BaseMetrics app encourages protective behaviors like physical activity, this was an unexpected finding. This result may be partially due to seasonal changes. Most participants began the intervention in late summer or early fall and concluded the intervention in late fall or early winter. During this time, in the geographic location of the study, the temperature gradually decreases, and sunlight duration shortens. Therefore, it is possible that a decrease in physical activity during the study period reflects the influence of seasonal change rather than the influence of the BaseMetrics app. Regardless, our results disagree with past mHealth interventions that observe an improvement or no change in physical activity. A large meta-analysis that included 28 studies observed a small-to-moderate effect of using a physical activity-promoting mobile app on physical activity measures, including an estimated increase of 1850 steps per day [23]. The more individualized the features of the app, the more likely the app was to have a positive effect on physical activity. It should be noted that the mean duration of interventions was 13 weeks, ranging from 8 to 40 weeks. Another systematic review of 13 mHealth studies reported that 5 studies observed a significant increase in physical activity with the intervention, and the remaining studies observed no change [24]. The average intervention duration was 6.4 months. Thus, there is evidence of a positive impact of mHealth app interventions for promoting physical activity. It is possible that our negative results are due to a combination of seasonality and short intervention duration. Similar to diet data, a future randomized trial testing the BaseMetrics app should utilize a more robust measure of physical activity, such as accelerometry, as well as testing participants at various times throughout the year in order to remove the potential confounding effects of seasonality.
It should be noted that most of the biometric outcomes we measured did not change during the intervention period. This includes outcomes, such as body mass and composition, blood pressure, glucose, several lipid outcomes, and liver enzymes. Thus, our significant findings related to self-reported fruit and vegetable consumption, skin carotenoids, and self-reported physical activity should be weighed against these null results. Our generally null biometric results counter past findings that have generally shown a modest improvement in body mass/composition [25,26] and blood pressure [27] with mHealth interventions. It is possible that our intervention duration was too short to detect significant changes in these outcomes. Similar to our findings, many past mHealth interventions have not observed improvements in blood lipids [28].
Behavior change interventions offered via mHealth have the potential to impact large groups of the population by promoting risk-reduction behavior. Several mHealth interventions have been developed for cardiac rehabilitation and individual risk factor management, such as increased physical activity or improved diet [29,30,31]. To our knowledge, no previous mHealth interventions have specifically focused on primordial prevention of multiple behaviors and risk factors for CVD, including the targeting enhancement of CVD knowledge. Further, the BaseMetrics app is unique in that it incorporates multiple BCTs. The BaseMetrics app attempts to promote CVD prevention by combining several BCTs with compelling visual design. An effective mHealth intervention successfully addressing primordial prevention of CVD could significantly impact future research and practice. For healthy people, mHealth interventions like BaseMetrics could re-enforce or encourage positive health behaviors and outcomes. With regard to patients with an existing disease, mHealth interventions in health care provide a cost-effective opportunity to scale evidence-based intervention to a large population. Specifically, many primary care providers are severely time-limited for engaging in meaningful conversations with patients about understanding CVD risk factors and their management [32]. An mHealth intervention like BaseMetrics could be a very useful tool for educating and engaging with primary care patients about CVD prevention. However, it should be noted that findings related to the BaseMetrics app are very preliminary and need to be validated in larger randomized trials before the app can be clinically implemented.
In addition to primary care settings, mHealth interventions such as BaseMetrics may also have relevance for broader applications in community-based care and population health strategies. Recent work by Cordani et al. has highlighted the potential for digital health tools to bridge gaps in resource-constrained settings, facilitate patient engagement, and support chronic disease prevention through decentralized care delivery [33]. Their findings support the idea that mHealth platforms can enhance communication between patients and providers and serve as adjuncts to traditional health services, especially where time or access is limited. This aligns with the potential utility of BaseMetrics in complementing routine care and promoting behavioral risk reduction outside of clinic walls, particularly in underserved or at-risk populations. Future research should explore the implementation and integration of BaseMetrics within both clinical and community care contexts to better understand its feasibility, scalability, and impact on long-term cardiovascular outcomes.
Several considerations should be made when interpreting our data. This study was a pilot trial with a small sample size and without a control group, which is not as rigorous as a randomized controlled trial. The findings of this study must be validated in a larger randomized trial in order to ensure that the observed changes in this study were truly due to the BaseMetrics app. The BaseMetrics app was only available for iOS, and therefore, the study excluded Android users. Although our goal is to develop the app for both operating systems, the generalizability of these pilot findings is consequently limited. Further, it is possible that sociodemographic differences may exist between iOS and Android users, which would further limit our generalizability. It is possible that seasonal variation impacted our findings. Most participants had access to the BaseMetrics app from late summer/early fall to late fall/early winter. Our method for assessing fruits and vegetables was quick, simple, and via self-report, which no doubt introduced some degree of error into our diet intake data. Our participants were a convenience sample recruited through mass email at a midwestern US university, thus not likely highly generalizable to the general population. Due to the exploratory nature of this study, we did not adjust for multiple comparisons, which increases the risk of type 1 error.
This study evaluated a theory-based mHealth intervention for the primordial prevention of cardiovascular risk among employees. To the author’s knowledge, this is the first mHealth intervention to broadly address primordial CVD risk reduction, including behaviors and attitudes, among adults using a combination of BCTs and user-friendly visual design. The results of this study indicate positive, although very preliminary, outcomes for FV intake, but we also observed a decrease in self-reported physical activity. However, it should be noted that these findings are limited by a small sample size, a lack of a control group, and limited generalizability. These preliminary findings support the execution of a larger, randomized trial that tests the BaseMetrics app over a longer period of time.
Looking ahead, future development of the BaseMetrics app should prioritize enhancing usability and functionality to support long-term engagement and impact. Additional features such as social or peer support elements, personalized goal tracking, and gamification could further strengthen user motivation and adherence. Expanding platform availability to Android devices is critical. Exploring clinical integration, such as provider dashboards or EHR connectivity, may also increase reach and scalability. These future directions will be essential for transforming BaseMetrics from a promising prototype into a broadly applicable tool for cardiovascular disease prevention.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/sci7020071/s1, Table S1: Results of post hoc power analysis for each outcome variable.
Author Contributions
Conceptualization, J.H.R., A.B., and S.R.E.; methodology, J.H.R., A.B., J.B., and S.R.E.; investigation, J.H.R., A.B., B.H.K., S.W., I.U., A.R., and S.R.E.; resources, J.H.R. and S.R.E.; writing—original draft preparation, J.H.R. and S.R.E.; writing—review and editing, J.H.R., A.B., B.H.K., and S.R.E.; project administration, J.H.R. and S.R.E.; funding acquisition, J.H.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Oklahoma State University (protocol IRB-20-24; 2 October 2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors upon request.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Yusuf, S.; Joseph, P.; Rangarajan, S.; Islam, S.; Mente, A.; Hystad, P.; Brauer, M.; Kutty, V.R.; Gupta, R.; Wielgosz, A.; et al. Modifiable Risk Factors, Cardiovascular Disease and Mortality in 155,722 Individuals from 21 High-, Middle-, and Low-Income Countries. Lancet 2020, 395, 795–808. [Google Scholar] [CrossRef] [PubMed]
- Kotseva, K.; Wood, D.; De Bacquer, D.; De Backer, G.; Rydén, L.; Jennings, C.; Gyberg, V.; Amouyel, P.; Bruthans, J.; Castro Conde, A.; et al. EUROASPIRE IV: A European Society of Cardiology Survey on the Lifestyle, Risk Factor and Therapeutic Management of Coronary Patients from 24 European Countries. Eur. J. Prev. Cardiol. 2016, 23, 636–648. [Google Scholar] [CrossRef]
- Steinmetz, M.; Rammos, C.; Rassaf, T.; Lortz, J. Digital Interventions in the Treatment of Cardiovascular Risk Factors and Atherosclerotic Vascular Disease. Int. J. Cardiol. Heart Vasc. 2020, 26, 100470. [Google Scholar] [CrossRef]
- Widmer, R.J.; Collins, N.M.; Collins, C.S.; West, C.P.; Lerman, L.O.; Lerman, A. Digital Health Interventions for the Prevention of Cardiovascular Disease: A Systematic Review and Meta-Analysis. Mayo Clin. Proc. 2015, 90, 469–480. [Google Scholar] [CrossRef]
- Neubeck, L.; Lowres, N.; Benjamin, E.J.; Freedman, S.B.; Coorey, G.; Redfern, J. The Mobile Revolution—Using Smartphone Apps to Prevent Cardiovascular Disease. Nat. Rev. Cardiol. 2015, 12, 350–360. [Google Scholar] [CrossRef] [PubMed]
- Santo, K.; Richtering, S.S.; Chalmers, J.; Thiagalingam, A.; Chow, C.K.; Redfern, J. Mobile Phone Apps to Improve Medication Adherence: A Systematic Stepwise Process to Identify High-Quality Apps. JMIR mHealth uHealth 2016, 4, e132. [Google Scholar] [CrossRef] [PubMed]
- Cho, Y.-M.; Lee, S.; Islam, S.M.S.; Kim, S.-Y. Theories Applied to M-Health Interventions for Behavior Change in Low- and Middle-Income Countries: A Systematic Review. Telemed. e-Health 2018, 24, 727–741. [Google Scholar] [CrossRef]
- Vandelanotte, C.; Müller, A.M.; Short, C.E.; Hingle, M.; Nathan, N.; Williams, S.L.; Lopez, M.L.; Parekh, S.; Maher, C.A. Past, Present, and Future of eHealth and mHealth Research to Improve Physical Activity and Dietary Behaviors. J. Nutr. Educ. Behav. 2016, 48, 219–228.e1. [Google Scholar] [CrossRef]
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Godin, G.; Kok, G. The Theory of Planned Behavior: A Review of Its Applications to Health-Related Behaviors. Am. J. Health Promot. 1996, 11, 87–98. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Velicer, W.F. The Transtheoretical Model of Health Behavior Change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef] [PubMed]
- Janz, N.K.; Becker, M.H. The Health Belief Model: A Decade Later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Barbara, K.; Rimer, K.; Viswanath, C.; Orleans, T. Health Behavior and Health Education: Theory, Research, and Practice, 4th ed.; Jossey-Bass Inc Pub: San Francisco, CA, USA, 2008; p. 552. ISBN 978-0-7879-9614-7. [Google Scholar]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically Clustered Techniques: Building an International Consensus for the Reporting of Behavior Change Interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Vézina-Im, L.-A.; Godin, G.; Couillard, C.; Perron, J.; Lemieux, S.; Robitaille, J. Validity and Reliability of a Brief Self-Reported Questionnaire Assessing Fruit and Vegetable Consumption among Pregnant Women. BMC Public Health 2016, 16, 982. [Google Scholar] [CrossRef]
- Mainvil, L.A.; Horwath, C.C.; McKenzie, J.E.; Lawson, R. Validation of Brief Instruments to Measure Adult Fruit and Vegetable Consumption. Appetite 2011, 56, 111–117. [Google Scholar] [CrossRef]
- Ermakov, I.V.; Ermakova, M.; Sharifzadeh, M.; Gorusupudi, A.; Farnsworth, K.; Bernstein, P.S.; Stookey, J.; Evans, J.; Arana, T.; Tao-Lew, L.; et al. Optical Assessment of Skin Carotenoid Status as a Biomarker of Vegetable and Fruit Intake. Arch. Biochem. Biophys. 2018, 646, 46–54. [Google Scholar] [CrossRef]
- Di Noia, J.; Gellermann, W. Use of the Spectroscopy-Based Veggie Meter® to Objectively Assess Fruit and Vegetable Intake in Low-Income Adults. Nutrients 2021, 13, 2270. [Google Scholar] [CrossRef] [PubMed]
- May, K.; Jilcott Pitts, S.; Stage, V.C.; Kelley, C.J.; Burkholder, S.; Fang, X.; Zeng, A.; Lazorick, S. Use of the Veggie Meter® as a Tool to Objectively Approximate Fruit and Vegetable Intake among Youth for Evaluation of Preschool and School-Based Interventions. J. Hum. Nutr. Diet. 2020, 33, 869–875. [Google Scholar] [CrossRef]
- Woringer, M.; Nielsen, J.J.; Zibarras, L.; Evason, J.; Kassianos, A.P.; Harris, M.; Majeed, A.; Soljak, M. Development of a Questionnaire to Evaluate Patients’ Awareness of Cardiovascular Disease Risk in England’s National Health Service Health Check Preventive Cardiovascular Programme. BMJ Open 2017, 7, e014413. [Google Scholar] [CrossRef]
- McCarroll, R.; Eyles, H.; Ni Mhurchu, C. Effectiveness of Mobile Health (mHealth) Interventions for Promoting Healthy Eating in Adults: A Systematic Review. Prev. Med. 2017, 105, 156–168. [Google Scholar] [CrossRef]
- Thom, S.J.M.; Sivakumar, B.; Ayodele, T.; Tan, M.C.; Brown, J.M.; Arcand, J. Impact of mHealth Interventions on Supporting Dietary Adherence in Cardiovascular Disease: A Systematic Review. J. Nutr. Educ. Behav. 2023, 55, 419–436. [Google Scholar] [CrossRef] [PubMed]
- Laranjo, L.; Ding, D.; Heleno, B.; Kocaballi, B.; Quiroz, J.C.; Tong, H.L.; Chahwan, B.; Neves, A.L.; Gabarron, E.; Dao, K.P.; et al. Do Smartphone Applications and Activity Trackers Increase Physical Activity in Adults? Systematic Review, Meta-Analysis and Metaregression. Br. J. Sports Med. 2021, 55, 422–432. [Google Scholar] [CrossRef] [PubMed]
- Müller, A.M.; Alley, S.; Schoeppe, S.; Vandelanotte, C. The Effectiveness of E-& mHealth Interventions to Promote Physical Activity and Healthy Diets in Developing Countries: A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 109. [Google Scholar] [CrossRef]
- Bernabe-Ortiz, A.; Pauschardt, J.; Diez-Canseco, F.; Miranda, J.J. Sustainability of mHealth Effects on Cardiometabolic Risk Factors: Five-Year Results of a Randomized Clinical Trial. J. Med. Internet Res. 2020, 22, e14595. [Google Scholar] [CrossRef]
- Ranjani, H.; Avari, P.; Nitika, S.; Jagannathan, N.; Oliver, N.; Valabhji, J.; Mohan, V.; Chambers, J.C.; Anjana, R.M. Effectiveness of Mobile Health Applications for Cardiometabolic Risk Reduction in Urban and Rural India: A Pilot, Randomized Controlled Study. J. Diabetes Sci. Technol. 2025, 36, 34–55. [Google Scholar] [CrossRef]
- Abe, M.; Hirata, T.; Morito, N.; Kawashima, M.; Yoshida, S.; Takami, Y.; Fujimoto, T.; Kawasoe, S.; Shibukawa, T.; Segawa, H.; et al. Smartphone Application-Based Intervention to Lower Blood Pressure: A Systematic Review and Meta-Analysis. Hypertens. Res. 2025, 48, 492–505. [Google Scholar] [CrossRef]
- Villinger, K.; Wahl, D.R.; Boeing, H.; Schupp, H.T.; Renner, B. The Effectiveness of App-Based Mobile Interventions on Nutrition Behaviours and Nutrition-Related Health Outcomes: A Systematic Review and Meta-Analysis. Obes. Rev. 2019, 20, 1465–1484. [Google Scholar] [CrossRef] [PubMed]
- Bostrom, J.; Sweeney, G.; Whiteson, J.; Dodson, J.A. Mobile Health and Cardiac Rehabilitation in Older Adults. Clin. Cardiol. 2020, 43, 118–126. [Google Scholar] [CrossRef]
- Cajita, M.I.; Gleason, K.T.; Han, H.-R. A Systematic Review of mHealth-Based Heart Failure Interventions. J. Cardiovasc. Nurs. 2016, 31, E10. [Google Scholar] [CrossRef]
- Cruz-Cobo, C.; Bernal-Jiménez, M.Á.; Vázquez-García, R.; Santi-Cano, M.J. Effectiveness of mHealth Interventions in the Control of Lifestyle and Cardiovascular Risk Factors in Patients After a Coronary Event: Systematic Review and Meta-Analysis. JMIR mHealth uHealth 2022, 10, e39593. [Google Scholar] [CrossRef]
- Luquis, R.R.; Paz, H.L. Attitudes About and Practices of Health Promotion and Prevention Among Primary Care Providers. Health Promot. Pract. 2015, 16, 745–755. [Google Scholar] [CrossRef] [PubMed]
- Cordani, C.; Perillo, S.; Corbetta, D.; Sarasso, E.; Agosta, F.; Filippi, M.; Mazzali, A.G.; Pennestrì, F. Developing Physiotherapy in Primary Health Care: A First Snapshot from the Italian Metropolitan City of Milan. Healthcare 2024, 12, 1628. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).