The Effect of Acute Lumbopelvic Muscular Fatigue on Neuromechanical Contraction Characteristics and Nociception
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Procedures
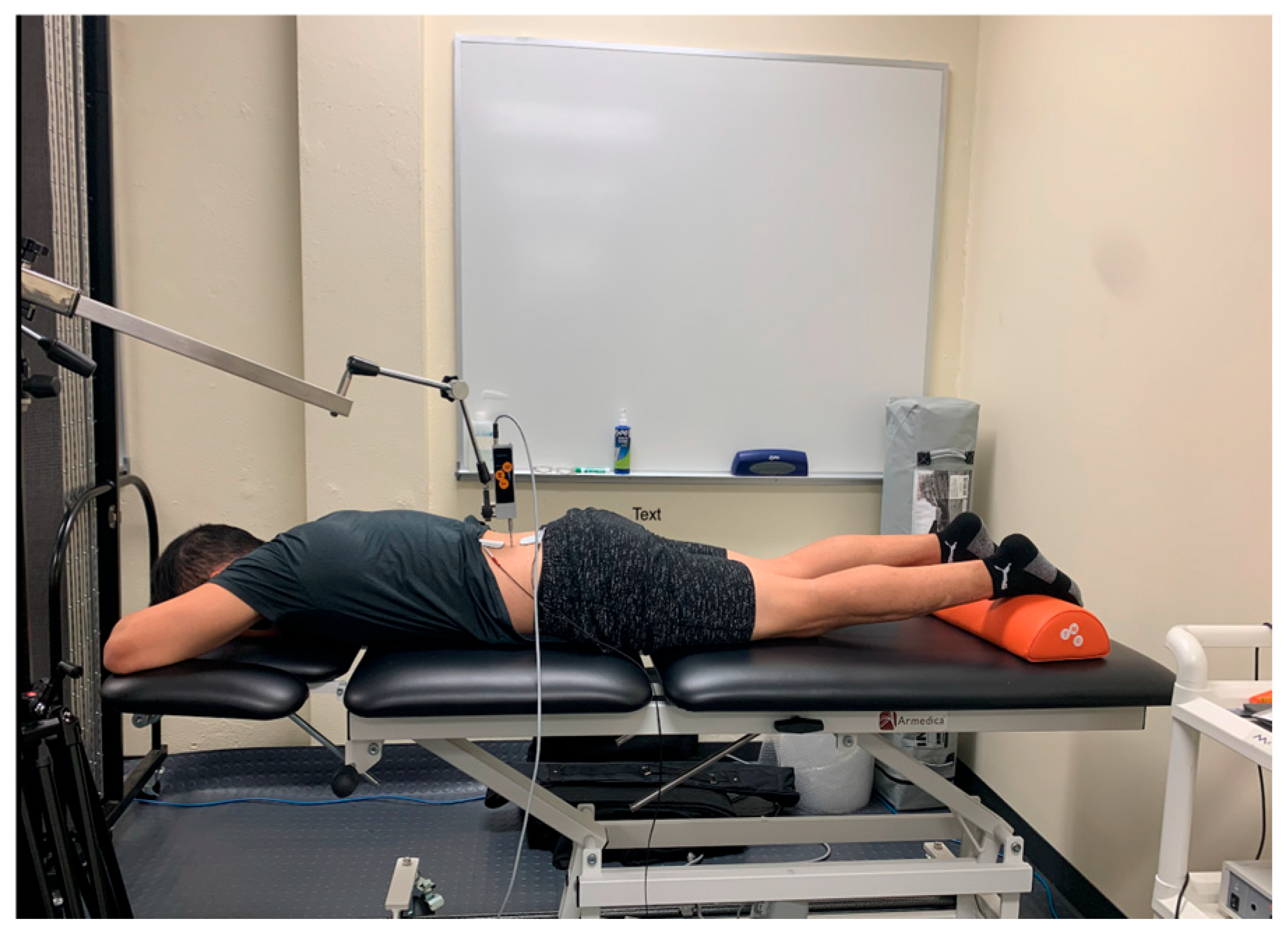
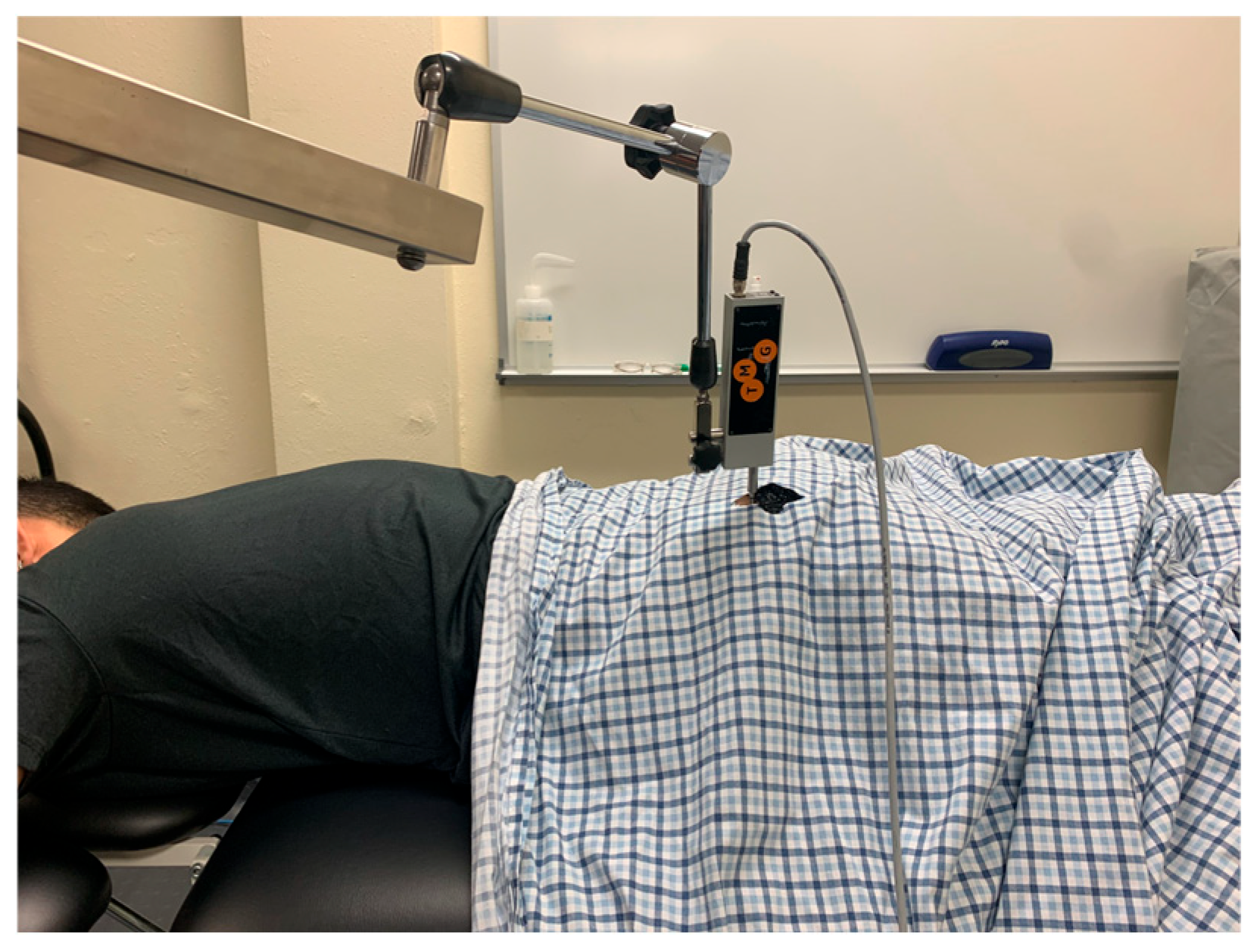
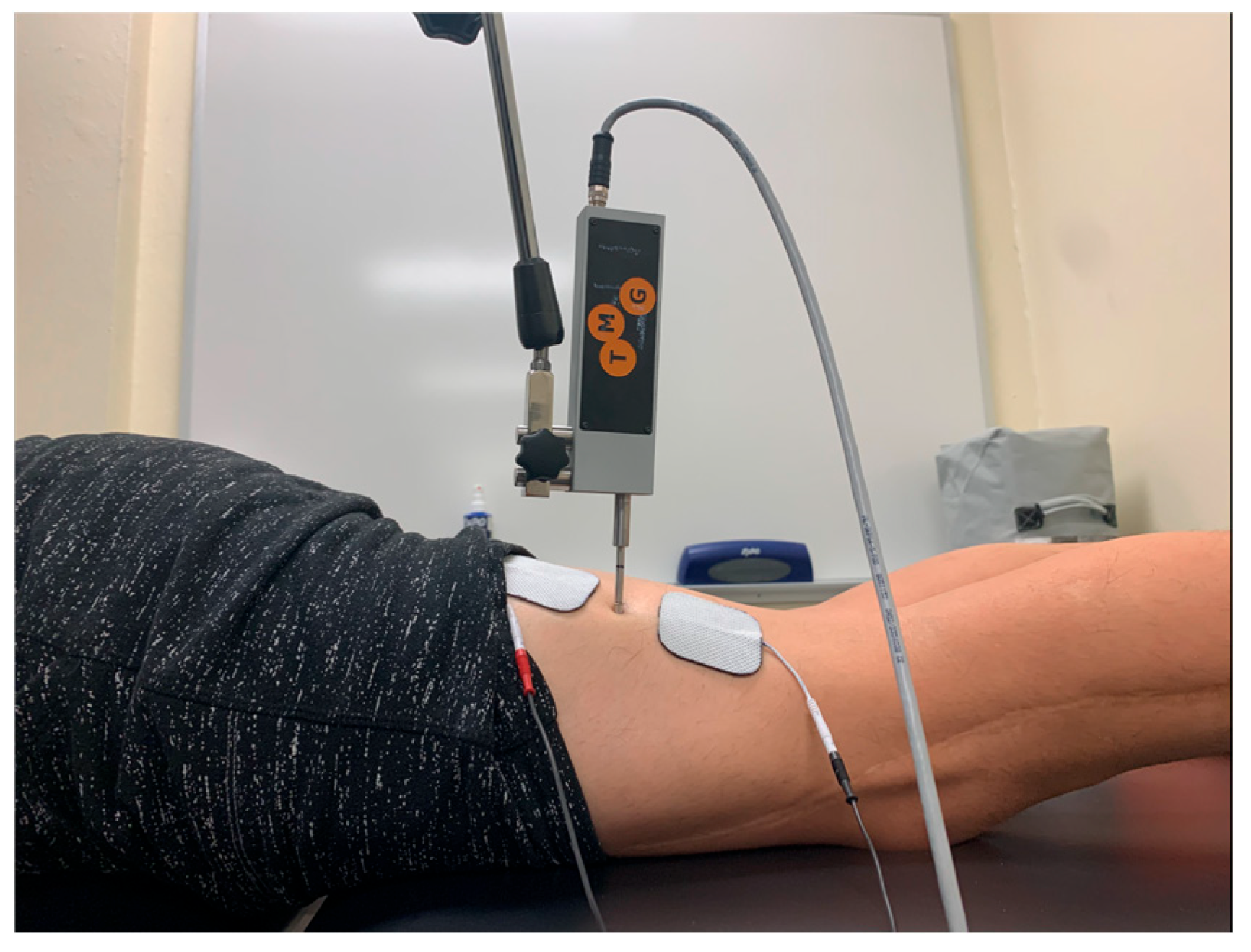
2.2.1. Tensiomyography Procedures
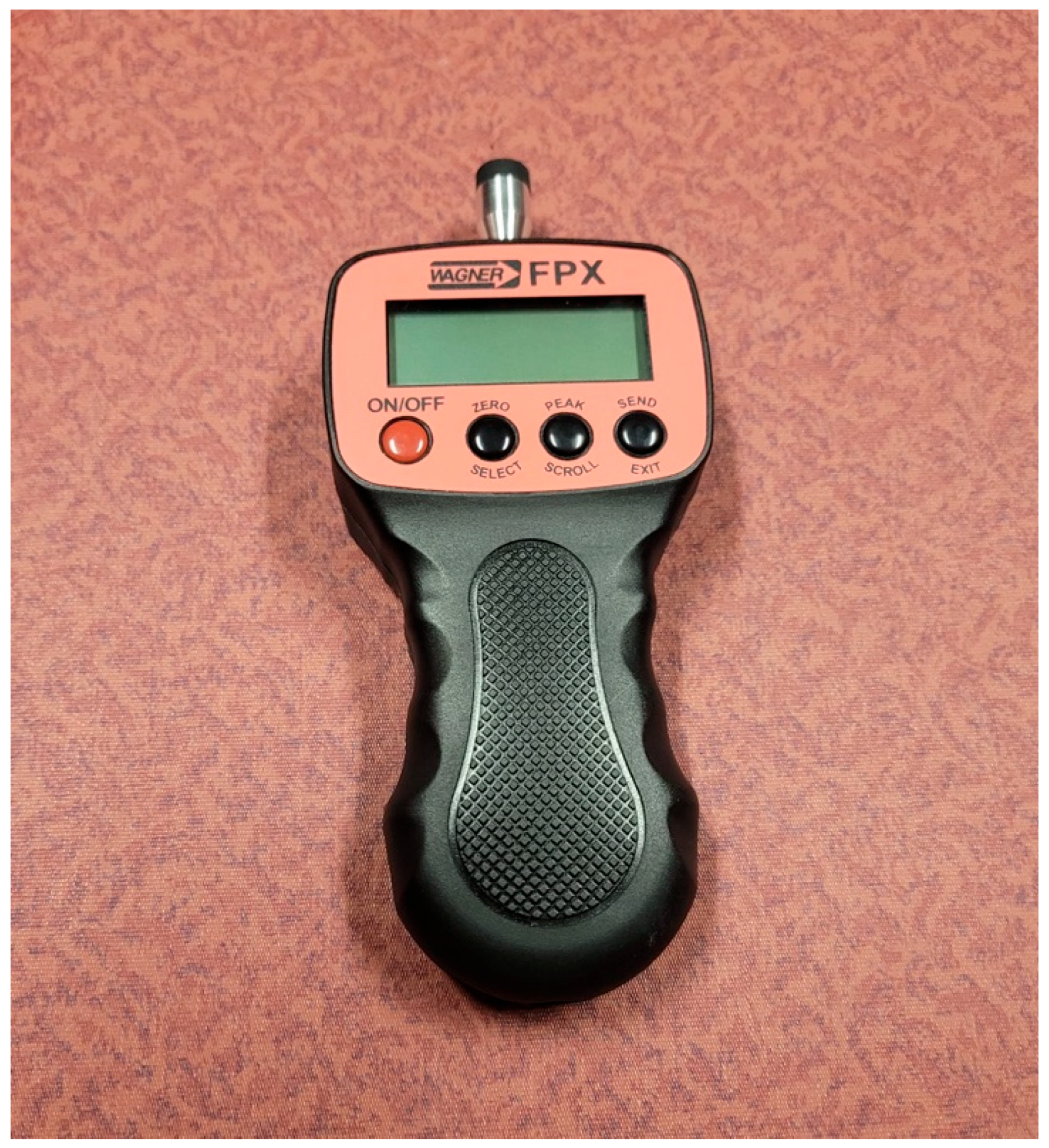
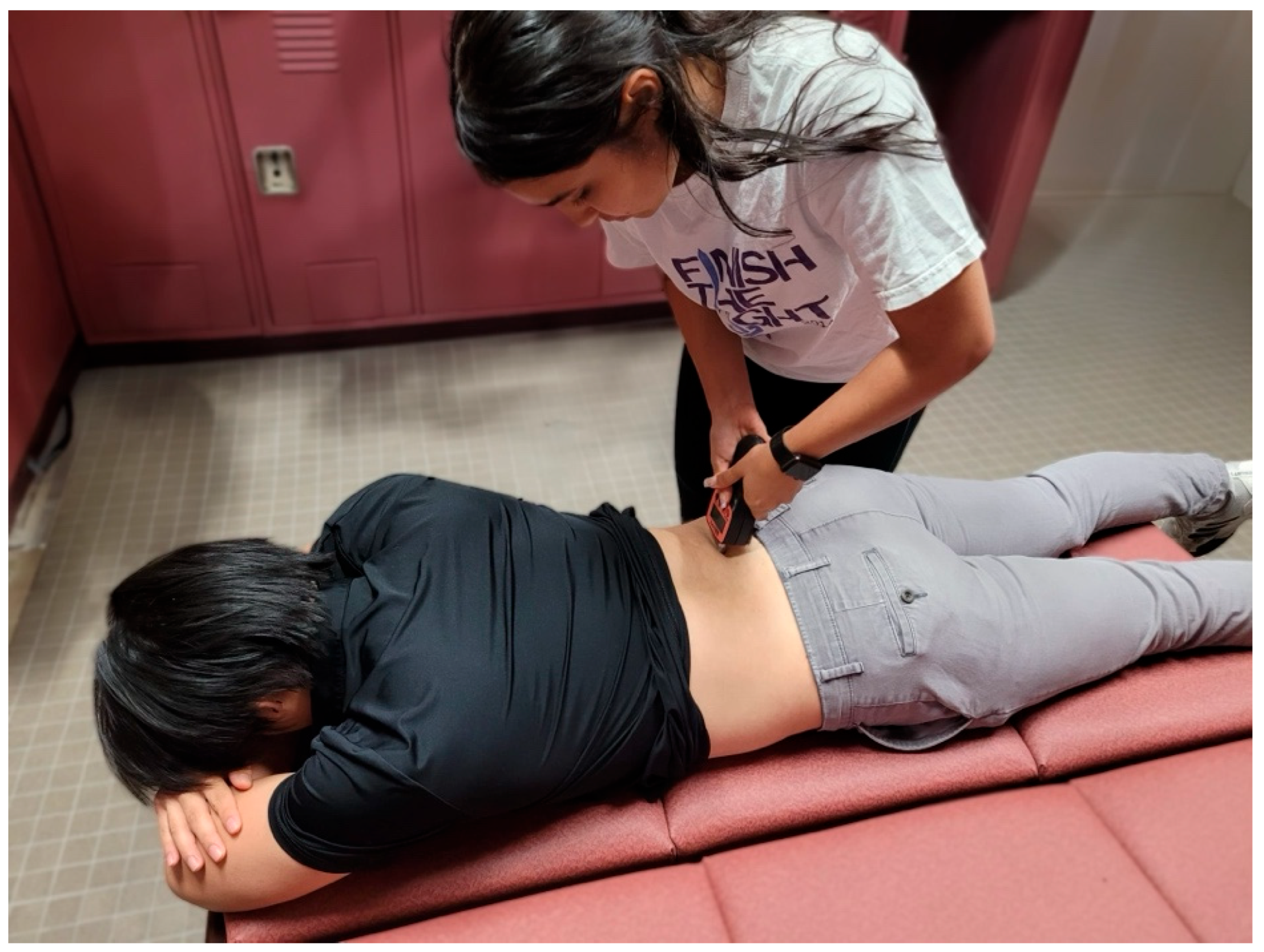
2.2.2. Pressure Algometry
2.3. Intervention
2.3.1. Warm-Up
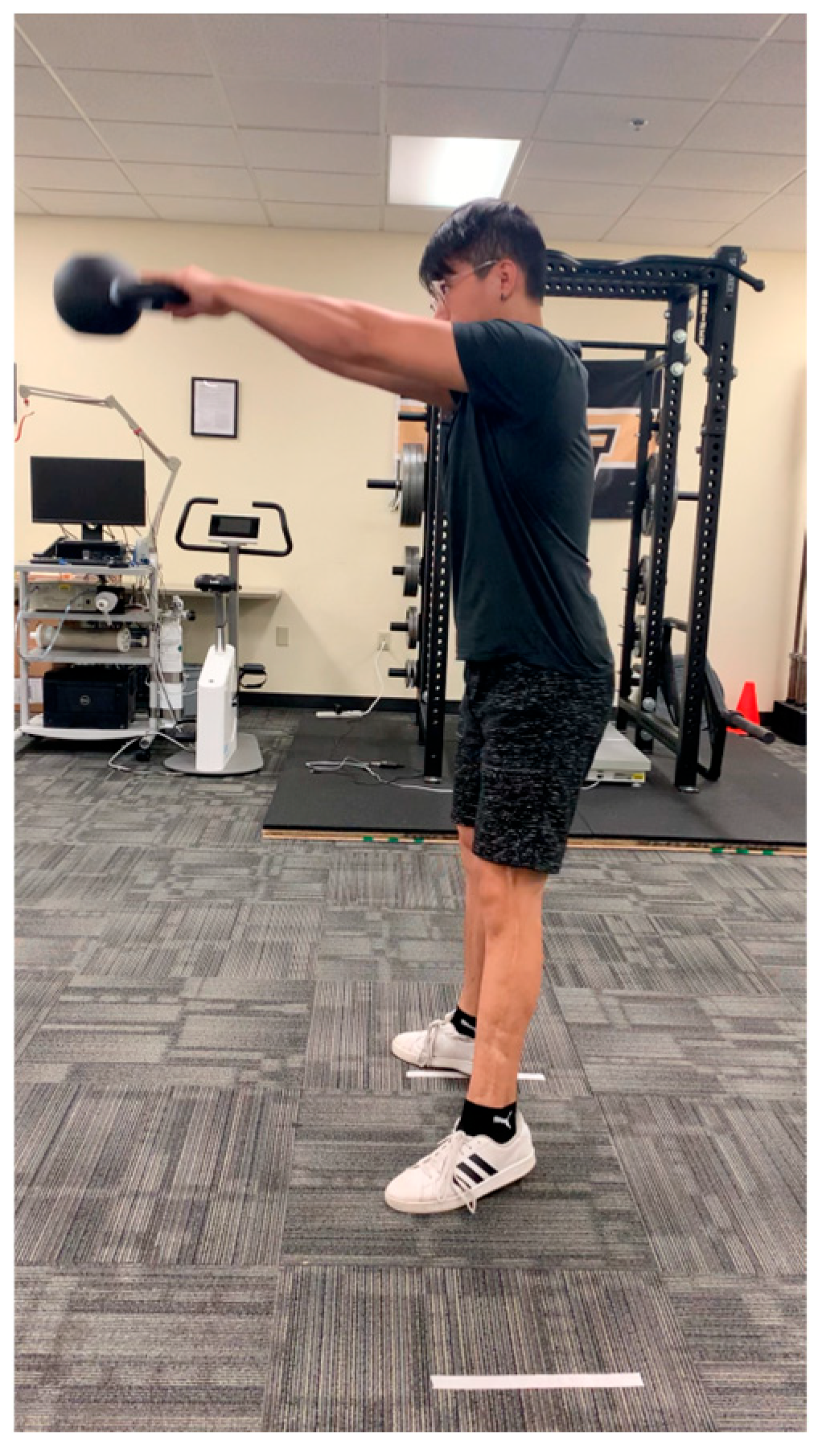
2.3.2. Kettlebell Swing Group
2.3.3. Isometric Hold
3. Results
3.1. Tensiomyography Results
3.2. Pressure Pain Threshold Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Piqueras-Sanchiz, F.; Cornejo-Daza, P.J.; Sánchez-Valdepeñas, J.; Bachero-Mena, B.; Sánchez-Moreno, M.; Martín-Rodríguez, S.; García-García, Ó.; Pareja-Blanco, F. Acute Mechanical, Neuromuscular, and Metabolic Responses to Different Set Configurations in Resistance Training. J. Strength Cond. Res. 2022, 36, 2983–2991. [Google Scholar] [CrossRef]
- Buoite Stella, A.; Cargnel, A.; Raffini, A.; Mazzari, L.; Martini, M.; Ajčević, M.; Accardo, A.; Deodato, M.; Murena, L. Shoulder Tensiomyography and Isometric Strength in Swimmers Before and After a Fatiguing Protocol. J. Athl. Train. 2024, 59, 738–744. [Google Scholar] [CrossRef]
- Westerblad, H.; Bruton, J.D.; Katz, A. Skeletal muscle: Energy metabolism, fiber types, fatigue and adaptability. Exp. Cell Res. 2010, 316, 3093–3099. [Google Scholar] [CrossRef]
- Pacheco-Barrios, K.; Carolyna Gianlorenço, A.; Machado, R.; Queiroga, M.; Zeng, H.; Shaikh, E.; Yang, Y.; Nogueira, B.; Castelo-Branco, L.; Fregni, F. Exercise-induced pain threshold modulation in healthy subjects: A systematic review and meta-analysis. Princ. Pract. Clin. Res. 2020, 6, 11–28. [Google Scholar] [CrossRef] [PubMed]
- Keilman, B.M.; Hanney, W.J.; Kolber, M.J.; Pabian, P.S.; Salamh, P.A.; Rothschild, C.E.; Liu, X. The Short-Term Effect of Kettlebell Swings on Lumbopelvic Pressure Pain Thresholds: A Randomized Controlled Trial. J. Strength Cond. Res. 2017, 31, 3001–3009. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, A.; Maruyama, T.; Naito, H.; Sinclair, P.J. Acute effects of high-intensity dumbbell exercise after isokinetic eccentric damage: Interaction between altered pain perception and fatigue on static and dynamic muscle performance. J. Strength Cond. Res. 2010, 24, 2042–2049. [Google Scholar] [CrossRef] [PubMed]
- Morris, M.G.; Dawes, H.; Howells, K.; Scott, O.M.; Cramp, M.; Izadi, H. Alterations in peripheral muscle contractile characteristics following high and low intensity bouts of exercise. Eur. J. Appl. Physiol. 2012, 112, 337–343. [Google Scholar] [CrossRef]
- Muñoz-López, A.; De Hoyo, M.; Nuñez, F.J.; Sañudo, B. Using Tensiomyography to Assess Changes in Knee Muscle Contraction Properties After Concentric and Eccentric Fatiguing Muscle Actions. J. Strength Cond. Res. 2022, 36, 935–940. [Google Scholar] [CrossRef]
- Jaiswal, P.R.; Ramteke, S.U.; Shedge, S. Enhancing Athletic Performance: A Comprehensive Review on Kettlebell Training. Cureus 2024, 16, e53497. [Google Scholar] [CrossRef]
- Vaegter, H.B.; Hoeger Bement, M.; Madsen, A.B.; Fridriksson, J.; Dasa, M.; Graven-Nielsen, T. Exercise increases pressure pain tolerance but not pressure and heat pain thresholds in healthy young men. Eur. J. Pain 2017, 21, 73–81. [Google Scholar] [CrossRef]
- Wewege, M.A.; Jones, M.D. Exercise-Induced Hypoalgesia in Healthy Individuals and People With Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. J. Pain 2021, 22, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Tabata, I. Tabata training: One of the most energetically effective high-intensity intermittent training methods. J. Physiol. Sci. 2019, 69, 559–572. [Google Scholar] [CrossRef] [PubMed]
- Lake, J.P.; Lauder, M.A. Kettlebell swing training improves maximal and explosive strength. J. Strength Cond. Res. 2012, 26, 2228–2233. [Google Scholar] [CrossRef] [PubMed]
- Čular, D.; Babić, M.; Zubac, D.; Kezić, A.; Macan, I.; Peyré-Tartaruga, L.A.; Ceccarini, F.; Padulo, J. Tensiomyography: From muscle assessment to talent identification tool. Front. Physiol. 2023, 14, 1163078. [Google Scholar] [CrossRef]
- Edinborough, L.; Fisher, J.P.; Steele, J. A Comparison of the Effect of Kettlebell Swings and Isolated Lumbar Extension Training on Acute Torque Production of the Lumbar Extensors. J. Strength Cond. Res. 2016, 30, 1189–1195. [Google Scholar] [CrossRef]
- McGill, S.M.; Marshall, L.W. Kettlebell swing, snatch, and bottoms-up carry: Back and hip muscle activation, motion, and low back loads. J. Strength Cond. Res. 2012, 26, 16–27. [Google Scholar] [CrossRef]
- Van Gelder, L.H.; Hoogenboom, B.J.; Alonzo, B.; Briggs, D.; Hatzel, B. EMG Analysis and Sagittal Plane Kinematics of the Two-Handed and Single-Handed Kettlebell Swing: A Descriptive Study. Int. J. Sports Phys. Ther. 2015, 10, 811–826. [Google Scholar]
- Martín-Rodríguez, S.; Loturco, I.; Hunter, A.M.; Rodríguez-Ruiz, D.; Munguia-Izquierdo, D. Reliability and Measurement Error of Tensiomyography to Assess Mechanical Muscle Function: A Systematic Review. J. Strength Cond. Res. 2017, 31, 3524–3536. [Google Scholar] [CrossRef]
- Lohr, C.; Braumann, K.M.; Reer, R.; Schroeder, J.; Schmidt, T. Reliability of tensiomyography and myotonometry in detecting mechanical and contractile characteristics of the lumbar erector spinae in healthy volunteers. Eur. J. Appl. Physiol. 2018, 118, 1349–1359. [Google Scholar] [CrossRef]
- Burger, H.; Valencic, V.; Marincek, C.; Kogovsek, N. Properties of musculus gluteus maximus in above-knee amputees. Clin. Biomech. 1996, 11, 35–38. [Google Scholar] [CrossRef]
- Đorđević, S.; Rozman, S.; Zupet, P.; Dopsaj, M.; Maffulli, N. Tensiomyography Allows to Discriminate between Injured and Non-Injured Biceps Femoris Muscle. Biology 2022, 11, 746. [Google Scholar] [CrossRef]
- Walton, D.M.; Macdermid, J.C.; Nielson, W.; Teasell, R.W.; Chiasson, M.; Brown, L. Reliability, standard error, and minimum detectable change of clinical pressure pain threshold testing in people with and without acute neck pain. J. Orthop. Sports Phys. Ther. 2011, 41, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Jay, K.; Frisch, D.; Hansen, K.; Zebis, M.K.; Andersen, C.H.; Mortensen, O.S.; Andersen, L.L. Kettlebell training for musculoskeletal and cardiovascular health: A randomized controlled trial. Scand. J. Work. Environ. Health 2011, 37, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Lyons, B.C.; Mayo, J.J.; Tucker, W.S.; Wax, B.; Hendrix, R.C. Electromyographical Comparison of Muscle Activation Patterns Across Three Commonly Performed Kettlebell Exercises. J. Strength Cond. Res. 2017, 31, 2363–2370. [Google Scholar] [CrossRef] [PubMed]
- Neto, W.K.; Soares, E.G.; Vieira, T.L.; Aguiar, R.; Chola, T.A.; Sampaio, V.L.; Gama, E.F. Gluteus Maximus Activation during Common Strength and Hypertrophy Exercises: A Systematic Review. J. Sports Sci. Med. 2020, 19, 195–203. [Google Scholar]
- Liu, J.; Teng, H.L.; Selkowitz, D.M.; Asavasopon, S.; Powers, C.M. Influence of hip and knee positions on gluteus maximus and hamstrings contributions to hip extension torque production. Physiother. Theory Pract. 2022, 38, 2650–2657. [Google Scholar] [CrossRef]
- Niwa, Y.; Shimo, K.; Ohga, S.; Tokiwa, Y.; Hattori, T.; Matsubara, T. Effects of Exercise-Induced Hypoalgesia at Different Aerobic Exercise Intensities in Healthy Young Adults. J. Pain Res. 2022, 15, 3615–3624. [Google Scholar] [CrossRef]
- Hoeger Bement, M.K.; Dicapo, J.; Rasiarmos, R.; Hunter, S.K. Dose response of isometric contractions on pain perception in healthy adults. Med. Sci. Sports Exerc. 2008, 40, 1880–1889. [Google Scholar] [CrossRef]
- Probst, D.; Stout, A.; Hunt, D. Piriformis Syndrome: A Narrative Review of the Anatomy, Diagnosis, and Treatment. PM R. 2019, 11 (Suppl. 1), S54–S63. [Google Scholar] [CrossRef]
- Samani, M.; Ghaffarinejad, F.; Abolahrari-Shirazi, S.; Khodadadi, T.; Roshan, F. Prevalence and sensitivity of trigger points in lumbo-pelvic-hip muscles in patients with patellofemoral pain syndrome. J. Bodyw. Mov. Ther. 2020, 24, 126–130. [Google Scholar] [CrossRef]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; Blair, S.N.; Corrado, D.; Estes, N.A., 3rd; Fulton, J.E.; Gordon, N.F.; Haskell, W.L.; Link, M.S.; et al. Exercise and acute cardiovascular events placing the risks into perspective: A scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation 2007, 115, 2358–2368. [Google Scholar] [CrossRef] [PubMed]
- van Teeffelen, W.M.; de Beus, M.F.; Mosterd, A.; Bots, M.L.; Mosterd, W.L.; Pool, J.; Doevendans, P.A.; Grobbee, D.E. Risk factors for exercise-related acute cardiac events. A case-control study. Br. J. Sports Med. 2009, 43, 722–725. [Google Scholar] [CrossRef] [PubMed]
- Wiles, J.D.; Taylor, K.; Coleman, D.; Sharma, R.; O’Driscoll, J.M. The safety of isometric exercise: Rethinking the exercise prescription paradigm for those with stage 1 hypertension. Medicine 2018, 97, e0105. [Google Scholar] [CrossRef] [PubMed]





| Control Group | Kettlebell Swing Group | Isometric Hold | |
|---|---|---|---|
| Age | 23.5 ± 2.5 | 24.3 ± 3.3 | 23.6 ± 2.5 |
| Gender | |||
| Male | 10 | 7 | 10 |
| Female | 3 | 6 | 4 |
| Exercise Level | |||
| 1 * | 1 | 2 | 2 |
| 2 ** | 10 | 7 | 10 |
| 3 *** | 2 | 4 | 2 |
| Height (cm) | 174.6 ± 9.7 | 173.6 ± 12.8 | 174.7 ± 15.1 |
| Weight (kg) | 72.1 ± 14.5 | 73.1 ± 12.5 | 75.9 ± 13.9 |
| KB Control (n = 13) | KB Swing (n = 13) | KB Isometric (n = 14) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre (ms) | Post (ms) | Effect Size | p Value Within Group | Pre (ms) | Post (ms) | Effect Size | p Value Within Group | Pre (ms) | Post (ms) | Effect Size | p Value Within Group | p-Value Group x Time | |
| Tc | 18.53 ± 11.44 | 17.00 ± 6.82 | 0.25 | 0.38 | 18.88 ± 6.22 | 38.69 ± 60.93 | −0.31 | 0.27 | 16.41 ± 7.85 | 22.79 ± 26.03 | −0.31 | 0.25 | 0.35 |
| Tr | 200.94 ± 174.00 | 180.71 ± 169.16 | 0.09 | 0.73 | 157.68 ± 251.91 | 139.36 ± 131.85 | 0.06 | 0.826 | 91.87 ± 117.92 | 152.78 ± 211.53 | −0.42 | 0.13 | 0.55 |
| Td | 33.23 ± 47.13 | 32.55 ± 43.61 | 0.17 | 0.53 | 31.98 ± 37.50 | 34.01 ± 38.72 | −0.50 | 0.09 | 20.25 ± 5.37 | 27.92 ± 27.42 | −0.23 | 0.38 | 0.53 |
| Ts | 404.41 ± 284.22 | 468.74 ± 310.36 | −0.21 | 0.45 | 399.24 ± 361.36 | 422.12 ± 312.15 | −0.04 | 0.87 | 346.42 ± 371.62 | 280.19 ± 267.36 | 0.19 | 0.46 | 0.67 |
| KB Control (n = 13) | KB Swing (n = 13) | KB Isometric (n = 14) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre (ms) | Post (ms) | Effect Size | p Value Within Group | Pre (ms) | Post (ms) | Effect Size | p Value Within Group | Pre (ms) | Post (ms) | Effect Size | p Value Within Group | p Value Group x Time | |
| Tc | 29.85 ± 8.16 | 34.34 ± 15.17 | −0.30 | 0.30 | 39.60 ± 14.70 | 43.00 ± 13.61 | −0.37 | 0.20 | 37.78 ± 11.19 | 37.19 ± 10.57 | 0.09 | 0.72 | 0.43 |
| Tr | 99.52 ± 60.95 | 77.94 ± 37.99 | 0.33 | 0.25 | 71.01 ± 38.19 | 78.81 ± 71.04 | −0.09 | 0.73 | 83.54 ± 54.85 | 78.56 ± 40.28 | 0.14 | 0.59 | 0.48 |
| Td | 29.00 ± 8.10 | 27.51 ± 5.21 | 0.20 | 0.48 | 41.18 ± 29.45 | 32.30 ± 8.20 | 0.31 | 0.27 | 35.022 ± 20.16 | 30.82 ± 7.40 | 0.23 | 0.39 | 0.62 |
| Ts | 207.5 ± 104.35 | 184.68 ± 89.39 | 0.21 | 0.44 | 190.69 ± 85.98 | 184.10 ± 91.09 | 0.09 | 0.74 | 201.95 ± 134.59 | 151.78 ± 55.63 | 0.49 | 0.08 | 0.48 |
| KB Control (n = 13) | KB Swing (n = 13) | KB Isometric (n = 14) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre (ms) | Post (ms) | Effect Size | p Value Within Group | Pre (ms) | Post (ms) | Effect Size | p Value Within Group | Pre (ms) | Post (ms) | Effect Size | p Value Within Group | p Value Group x Time Interaction | |
| Tc | 30.74 ± 17.23 | 28.06 ± 11.15 | 0.32 | 0.26 | 32.93 ± 19.67 | 35.08 ± 20.53 | −0.07 | 0.78 | 34.16 ± 25.08 | 26.19 ± 14.49 | 0.35 | 0.20 | 0.47 |
| Tr | 37.19 ± 35.24 | 59.83 ± 40.24 | −0.53 | 0.07 | 42.38 ± 40.84 | 36.86 ± 34.69 | 0.11 | 0.67 | 43.34 ± 37.24 | 26.50 ± 26.42 | 0.50 | 0.08 | 0.05 |
| Td | 29.55 ± 17.59 | 30.32 ± 15.22 | −0.07 | 0.80 | 27.96 ± 13.19 | 34.43 ± 25.97 | −0.36 | 0.21 | 42.99 ± 28.72 | 35.91 ± 32.37 | 0.20 | 0.45 | 0.33 |
| Ts | 167.02 ± 144.50 | 167.34 ± 78.74 | −0.01 | 0.99 | 179.43 ± 131.74 | 148.93 ± 94.25 | 0.34 | 0.23 | 165.42 ± 91.15 | 141.98 ± 97.23 | 0.21 | 0.43 | 0.77 |
| KB Control (n = 13) | KB Swing (n = 13) | KB Isometric (n = 14) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Effect Size | p-Value Within Group | Pre | Post | Effect Size | p-Value Within Group | Pre | Post | Effect Size | p-Value Within Group | p-Value Group x Time | |
| Erector Spinae | 4.59 ± 1.96 | 4.358 ± 2.00 | 0.32 | 0.27 | 3.8 ± 1.74 | 3.22 ± 1.51 | 0.38 | 0.19 | 4.19 ± 2.67 | 3.56 ± 2.36 | 0.34 | 0.21 | 0.75 |
| Gluteus Maximus | 5.77 ± 2.79 | 5.577 ± 2.65 | 0.12 | 0.66 | 5.21 ± 3.01 | 5.53 ± 3.19 | −0.17 | 0.53 | 6.07 ± 2.77 | 5.92 ± 2.34 | 0.07 | 0.78 | 0.72 |
| Biceps Femoris | 2.79 ± 2.66 | 2.934 ± 3.32 | −0.11 | 0.69 | 2.58 ± 2.17 | 2.20 ± 1.70 | 0.17 | 0.55 | 1.96 ± 1.52 | 1.89 ± 1.76 | 0.06 | 0.81 | 0.70 |
| KB Control (n = 13) | KB Swing (n = 13) | KB Isometric (n = 14) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Effect Size | p-Value Within Group | Pre | Post | Effect Size | p-Value Within Group | Pre | Post | Effect Size | p-Value Within Group | p-Value Group x Time | |
| Erector Spinae | 58.86 ± 21.39 | 56.92 ± 22.70 | 0.164 | 0.564 | 78.04 ± 40.36 | 78.11 ± 41.71 | −0.007 | 0.982 | 64.37 ± 21.23 | 65.59 ± 24.13 | −0.107 | 0.696 | 0.764 |
| Quadratus Lumborum | 49.72 ± 20.49 | 49.03 ± 19.05 | 0.066 | 0.816 | 61.30 ± 23.54 | 63.62 ± 18.67 | −0.169 | 0.553 | 55.98 ± 22.81 | 57.94 ± 19.89 | −0.220 | 0.425 | 0.757 |
| Piriformis | 47.32 ± 13.67 | 56.03 ± 25.10 | -0.485 | 0.106 | 57.16 ± 18.44 | 64.52 ± 23.10 | −0.764 | 0.017 * | 50.80 ± 21.42 | 62.55 ± 32.94 | −0.747 | 0.015 * | 0.735 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanney, W.J.; Lee, C.; Cuevas-Hernandez, J.; Lin, J.; Kolber, M.J.; Anderson, A.W. The Effect of Acute Lumbopelvic Muscular Fatigue on Neuromechanical Contraction Characteristics and Nociception. Sci 2025, 7, 58. https://doi.org/10.3390/sci7020058
Hanney WJ, Lee C, Cuevas-Hernandez J, Lin J, Kolber MJ, Anderson AW. The Effect of Acute Lumbopelvic Muscular Fatigue on Neuromechanical Contraction Characteristics and Nociception. Sci. 2025; 7(2):58. https://doi.org/10.3390/sci7020058
Chicago/Turabian StyleHanney, William J., Christopher Lee, Julieanne Cuevas-Hernandez, Jing Lin, Morey J. Kolber, and Abigail W. Anderson. 2025. "The Effect of Acute Lumbopelvic Muscular Fatigue on Neuromechanical Contraction Characteristics and Nociception" Sci 7, no. 2: 58. https://doi.org/10.3390/sci7020058
APA StyleHanney, W. J., Lee, C., Cuevas-Hernandez, J., Lin, J., Kolber, M. J., & Anderson, A. W. (2025). The Effect of Acute Lumbopelvic Muscular Fatigue on Neuromechanical Contraction Characteristics and Nociception. Sci, 7(2), 58. https://doi.org/10.3390/sci7020058








