The Influence of Ionizing Radiation on the Morphological Structure of the Fluoride-Releasing Restorative Materials in Cancer Patients: An In Vitro Study
Abstract
1. Introduction
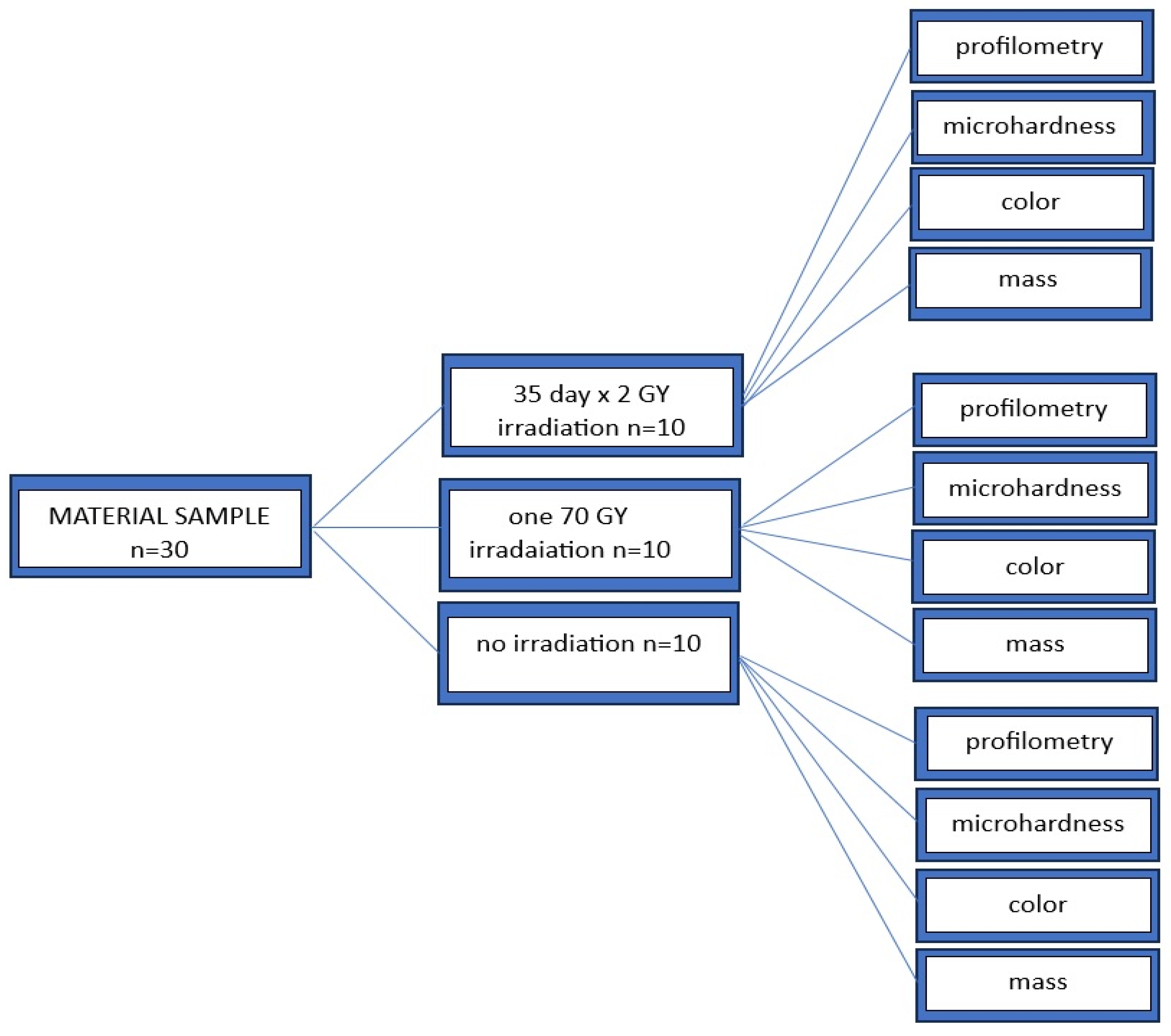
2. Materials and Methods
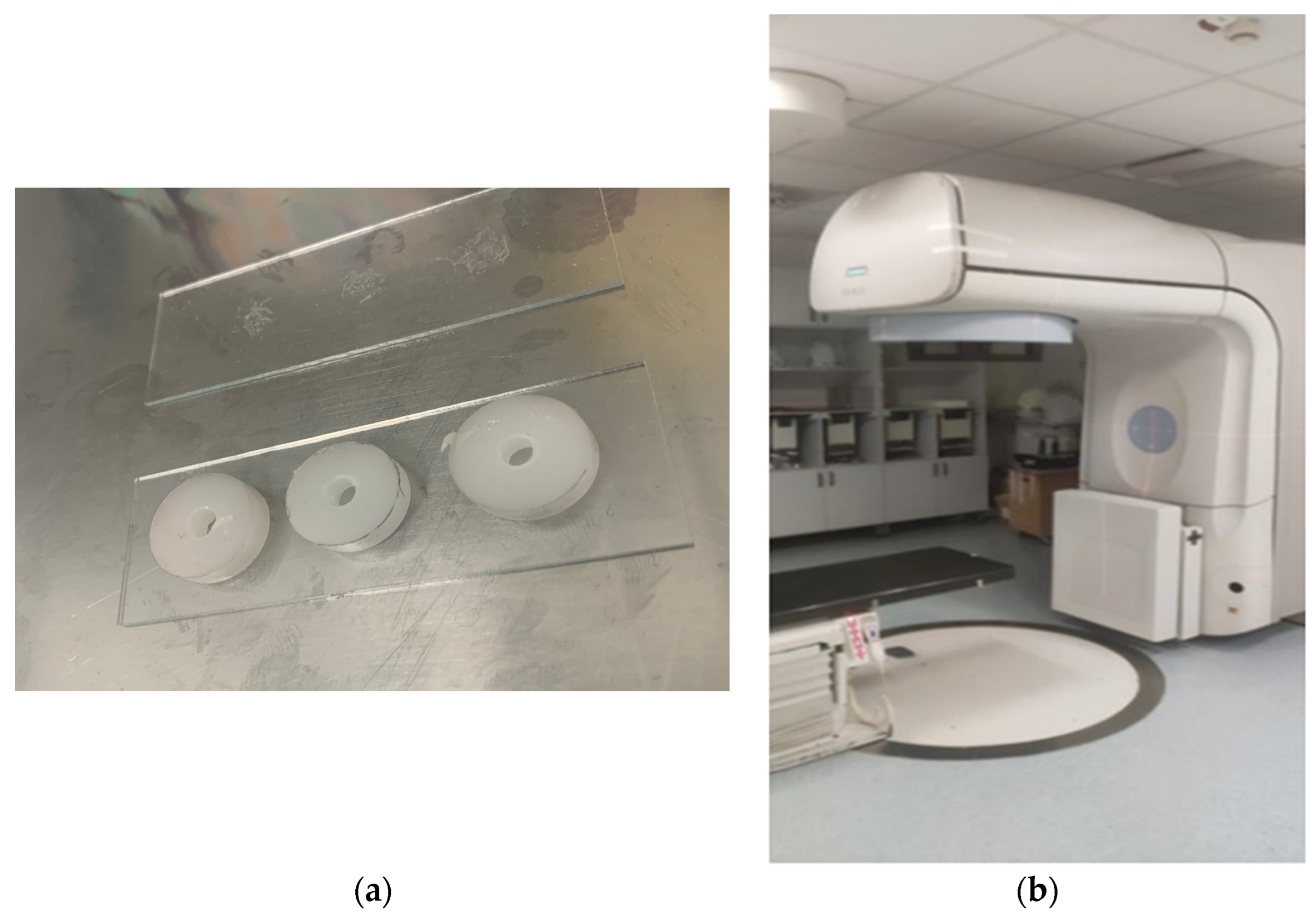
2.1. Sample Preparation
2.2. Irradiation Procedure
2.3. Surface Microhardness Analysis
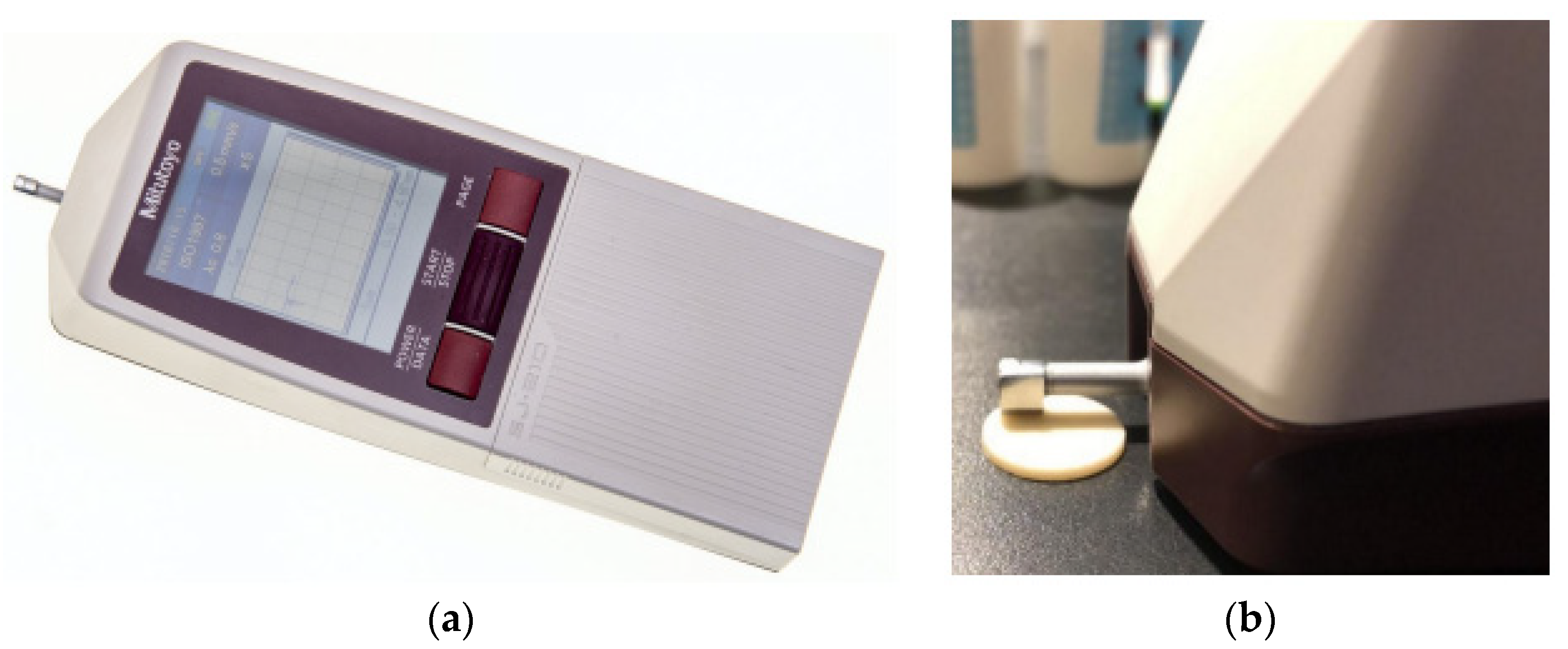
2.4. Prophylometry
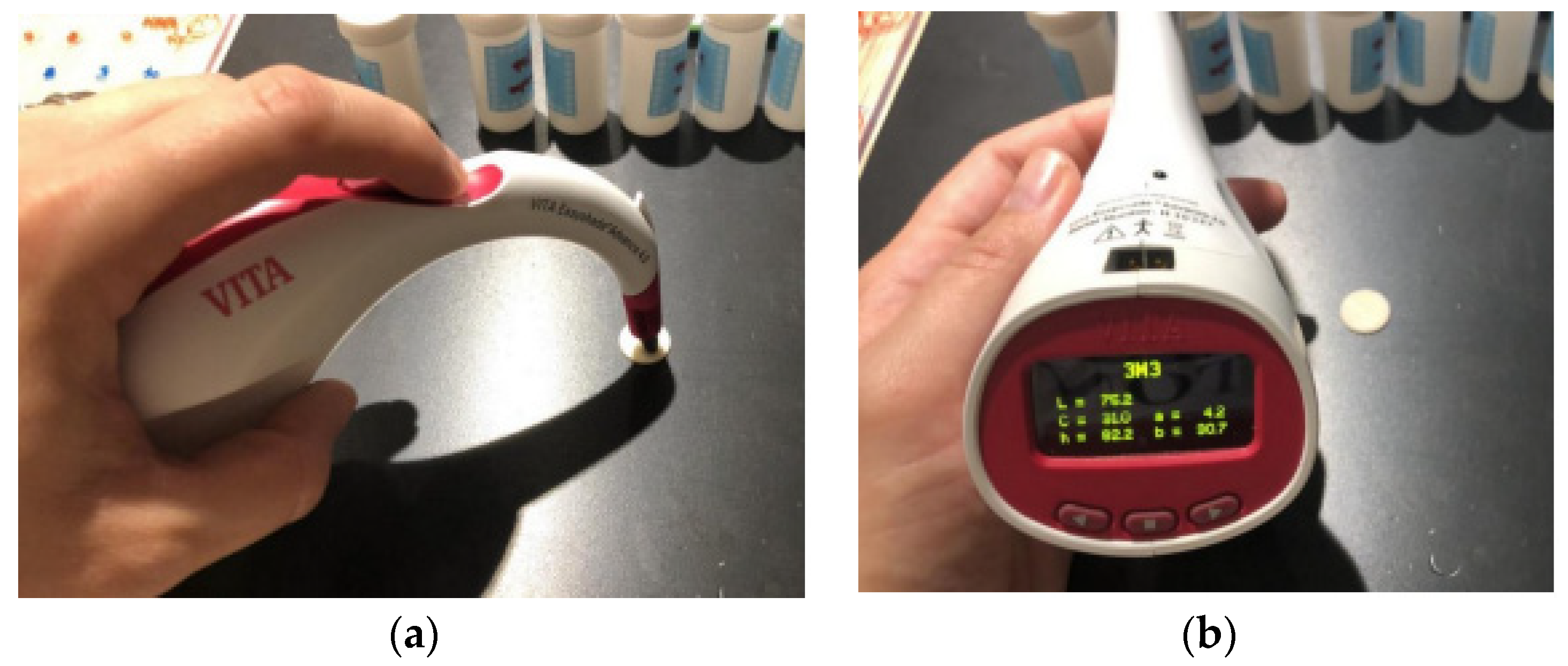
2.5. Measurement of Color Change
2.6. Mass Measurement
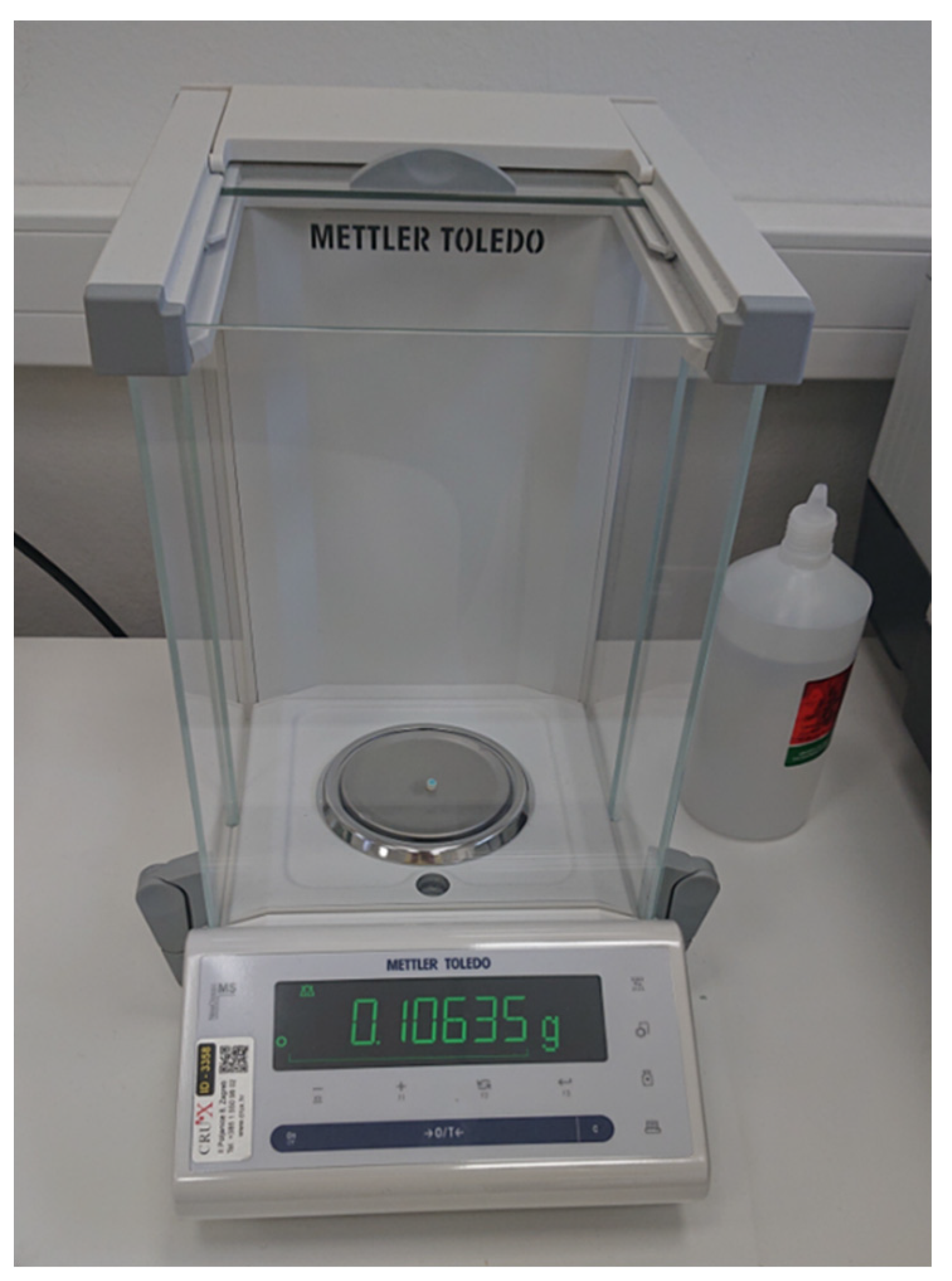
2.7. Statistical Analysis
3. Results
4. Discussion
- (1)
- After 35 days of radiation at 2 Gy per day, the CEN and PF materials demonstrated mass stability.
- (2)
- The surface roughness remained unchanged across all groups, while CEN, PF and EQ showed resistance to microhardness changes.
- (3)
- Significant color changes were observed in all groups, but brightness remained stable.
- (4)
- The CEN material showed the best overall stability and had an anti-caries effect, releasing ions under low pH conditions, which is beneficial for patients with xerostomia due to radiotherapy [25].
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Comprehensive Cancer Center Network. NCCN Guidelines for Head and Neck Cancers. J. Natl. Compr. Canc. Netw. 2018, 16, 479–490. [Google Scholar]
- Gernhardt, C.R.; Kielbassa, A.M.; Hahn, P.; Schaller, H.G. Tensile bond strengths of four different dentin adhesives on irradiated and non-irradiated human dentin in vitro. J. Oral Rehabil. 2001, 28, 814–820. [Google Scholar] [PubMed]
- Soares, C.J.; Castro, C.G.; Neiva, N.A.; Soares, P.V.; Santos-Filho, P.C.; Naves, L.Z. Effect of gamma irradiation on ultimate tensile strength of enamel and dentin. J. Dent. Res. 2010, 89, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Kielbassa, A.M.; Hinkelbein, W.; Hellwig, E.; Meyer-Luckel, H. Radiation-related damage to dentition. Lancet Oncol. 2006, 7, 326–335. [Google Scholar] [CrossRef] [PubMed]
- De Sanctis, V.; Bossi, P.; Sanguineti, G.; Trippa, F.; Ferrari, D.; Bacigalupo, A. Mucositis in head and neck cancer patients treated with radiotherapy and systemic therapies: Literature review and consensus statements. Crit. Rev. Oncol. Hematol. 2016, 100, 147–166. [Google Scholar] [CrossRef] [PubMed]
- Naves, L.Z.; Novais, V.R.; Armstrong, S.R.; Correr-Sobrinho, L.; Soares, C.J. Effect of gamma radiation on bonding to human enamel and dentin. Support. Care Cancer 2012, 20, 2873–2878. [Google Scholar] [CrossRef] [PubMed]
- Yesilyurt, C.; Bulucu, B.; Sezen, O.; Bulut, G.; Celik, D. Bond strengths of two conventional glass ionomer cements to irradiated and non-irradiated dentin. Dent. Mater. J. 2008, 27, 695–701. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Da Rosa Rodolpho, P.A.; Donassollo, T.A.; Cenci, M.S.; Loguercio, A.D.; Moraes, R.R.; Bronkhorst, E.M. 22-year clinical evaluation of the performance of two posterior composites with different filler characteristics. Dent. Mater. 2011, 27, 955–963. [Google Scholar] [CrossRef] [PubMed]
- Bernardo, M.; Luis, H.; Martin, M.D.; Leroux, B.G.; Rue, T.; Leitao, J. Survival and reasons for failure of amalgam versus composite posterior restorations placed in a randomized clinical trial. J. Am. Dent. Assoc. 2007, 138, 775–783. [Google Scholar] [CrossRef]
- Silva, A.R.; Alves, F.A.; Berger, S.B.; Giannini, M.; Goes, M.F.; Lopes, M.A. Radiation-related Caries and early failure in head and neck cancer patients. A polarized light microscopy and scanning electron microscopy study. Support. Care Cancer 2010, 18, 83–87. [Google Scholar] [CrossRef]
- Andrews, N.; Griffiths, C. Dental complications of head and neck radiotherapy: Part 2. Aust. Dent. J. 2001, 46, 174–182. [Google Scholar] [CrossRef] [PubMed]
- Hancock, P.J.; Epstein, J.B.; Sadler, G.R. Oral and dental management related to radiation therapy for head and neck cancer. J. Can. Dent. Assoc. 2003, 69, 585–590. [Google Scholar] [PubMed]
- Shaw, M.J.; Kumar, N.D.; Duggal, M.; Fiske, J.; Lewis, D.A.; Kinsella, T. Oral management of patients following oncology treatment: Literature review. Br. J. Oral Maxillofac. Surg. 2000, 38, 519–524. [Google Scholar] [CrossRef] [PubMed]
- Cruz, A.; Sinhoreti, M.; Ambrosano, G.; Rastelli, A.; Bagnato, V.; Bóscolo, F. Effect of therapeutic dose X rays on mechanical and chemical properties of esthetic dental materials. Mater. Res. 2008, 11, 313–318. [Google Scholar] [CrossRef]
- Beech, N.; Robinson, S.; Porcedds, S.; Batstone, M. Dental management of patients irradiated for head and neck cancer. Aust. Dent. J. 2014, 59, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Galetti, R.; Santos-Silva, A.R.; Antunes, A.N.; Alves Fde, A.; Lopes, M.A.; de Goes, M.F. Radiotherapy does not impair dentin adhesive properties in head and neck cancer patients. Clin. Oral Investig. 2014, 18, 1771–1778. [Google Scholar] [CrossRef] [PubMed]
- Chin, D.W.; Treister, N.; Friedland, B.; Cormack, R.A.; Tishler, R.B.; Makrigiorgos, G.M. Effect of dental restorations and prostheses on radiotherapy dose distribution: A Monte Carlo study. J. Appl. Clin. Med. Phys. 2009, 10, 80–89. [Google Scholar] [CrossRef] [PubMed]
- Reitemeier, B.; Reitemeier, G.; Schmidt, A.; Schaal, W.; Blochberger, P.; Lehmann, D. Evaluation of a device for attenuation of electron release from dental restorations in a therapeutic radiation field. J. Prosthet. Dent. 2002, 87, 323–327. [Google Scholar] [CrossRef] [PubMed]
- De Moor, R.J.; Stassen, I.G.; van’t Veldt, Y.; Torbeyns, D.; Hommez, G.M. Two-year clinical performance of glass ionomer and resin composite restorations in xerostomic head- and neck irradiated cancer patients. Clin. Oral Investig. 2002, 15, 31–38. [Google Scholar] [CrossRef]
- McComb, D.; Erickson, R.L.; Maxymiw, W.G.; Wood, R.E. A clinical comparison of glass ionomer, resin-modifified glass ionomer and resin composite restorations in the treatment of cervical caries in xerostomic head and neck radiation patients. Oper. Dent. 2002, 27, 430–437. [Google Scholar]
- Ferracane, J.L. Resin composite—State of the art. Dent. Mater. 2011, 27, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Germano, F.; Melone, P.; Testi, D.; Arcuri, L.; Marmiroli, L.; Petrone, A. Oral complications of head and neck radiotherapy: Prevalence and management. Minerva Stomatol. 2015, 64, 189–202. [Google Scholar] [PubMed]
- Naz, F. Comparative evaluation of mechanical and physical properties of a new bulk-fill alkasite with conventional restorative materials. Saudi Dent. J. 2020, 33, 666–673. [Google Scholar] [CrossRef] [PubMed]
- Miletic, I. Modern solutions for direct posterior restorations. GC Get. Connected. 2015, 4, 32–36. [Google Scholar]
- MeSH Browser [Database on the Internet]. Cention N. Available online: https://meshb.nlm.nih.gov/ (accessed on 30 August 2020).
- Kolemen, U. Analysis of ISE in microhardness measurements of bulk MgB2 superconductors using different models. J. Alloys Compd. 2006, 429, 435. [Google Scholar] [CrossRef]
- Sidhu, S.K.; Sheriff, M.; Watson, T.F. In vivo changes in roughness of resin-modified glass ionomer materials. Dent. Mater. 1997, 13, 208–213. [Google Scholar] [CrossRef] [PubMed]
- Yip, H.K.; Lam, W.T.C.; Smales, R.J. Fluoride release, weight loss and erosive of modern aesthetic restoratives. Br. Dent. J. 1999, 187, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Yip, H.K.; Lam, W.T.C.; Smales, R.J. Surface roughness and weight loss of esthetic restorative materials related to fluoride release and uptake. J. Clin. Pediatr. Dent. 1999, 23, 321–326. [Google Scholar] [PubMed]
- Rios, D.; Honório, H.M.; Araújo, P.A.; Machado, M.A.A. Wear and superficial roughness of glass ionomer cements used as sealants, after simulated toothbrushing. Braz. Oral Res. 2002, 16, 343–348. [Google Scholar] [CrossRef]
- Warren, D.P.; Colescott, T.D.; Henson, H.A.; Powers, J.M. Effects of four prophylaxis pastes on surface roughness of a composite, a hybrid ionomer and a compomer restorative material. J. Esthet. Rest. Dent. 2002, 14, 245–251. [Google Scholar] [CrossRef]
- Lohbauer, U. Dental Glass Ionomer Cements as Permanent Filling Materials?—Properties, Limitations, Future Trends. Materials 2009, 3, 76–96. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Investigations on Mechanical Behaviour of Dental Composites. Clin. Oral Investig. 2009, 13, 427–438, Erratum in Clin. Oral Investig. 2009, 13, 485–487. [Google Scholar] [CrossRef] [PubMed]
- Czasch, P.; Ilie, N. In Vitro Comparison of Mechanical Properties and Degree of Cure of Bulk Fill Composites. Clin. Oral Investig. 2013, 17, 227–235. [Google Scholar] [CrossRef]
- Reis, A.F.; Giannini, M.; Lovadino, J.R.; Dias, C.T.S. The effect of six polishing systems on the surface roughness of two packable resin-based composites. Am. J. Dent. 2002, 15, 193–197. [Google Scholar] [PubMed]
- Billingham, N.C. Degradation and stabilization of polymers. In Materials Science and Technology; Wiley-VCH: Hoboken, NJ, USA, 2013; pp. 469–507. [Google Scholar]
- Jefferies, S.R. Abrasive Finishing and Polishing in Restorative Dentistry: A State-of-the-Art Review. Dent. Clin. N. Am. 2007, 51, 379–397. [Google Scholar] [CrossRef]
- Soliman, H.A.N.; Elkholany, N.R.; Hamama, H.H.; El-Sharkawy, F.M.; Mahmoud, S.H.; Comisi, J.C. Effect of Different Polishing Systems on the Surface Roughness and Gloss of Novel Nanohybrid Resin Composites. Eur. J. Dent. 2021, 15, 259–265. [Google Scholar] [CrossRef]
- Kong, F.P.; Ten Haken, A.; Hayman, J. Personalized High Dose Radiation (>70 Gy) Is Significantly Associated with Better Local Regional Control and Overall Survival in Non-small Cell Lung Cancer Treated with Concurrent Chemoradiation. Int. J. Radiat. Oncol. Biol. Phys. 2011, 81, S594. [Google Scholar] [CrossRef]
- Bala, O.; Arisu, H.D.; Yikilgan, I.; Arslan, S.; Gullu, A. Evaluation of surface roughness and hardness of different glass ionomer cements. Eur. J. Dent. 2012, 6, 79–86. [Google Scholar] [CrossRef]
- Meena, B.; Hasija, M.; Wadhwani, K.K.; Wadhwa, D. Spectrometric analysis of intentionally stained hybrid and nanohybrid composites—An In vitro study. J. Int. Clin. Dent. Res. Organ. 2019, 11, 76–82. [Google Scholar] [CrossRef]
- Sarafianou, A.; Iosifidou, S.; Papadopoulos, T.; Eliades, G. Color Stability and Degree of Cure of Direct Composite Restoratives After Accelerated Aging. Oper. Dent. 2007, 32, 406–411. [Google Scholar] [CrossRef]
- Villalta, P.; Lu, H.; Okte, Z.; Garcia-Godoy, F.; Powers, J.M. Effects of Staining and Bleaching on Color Change of Dental Composite Resins. J. Prosthet. Dent. 2006, 95, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Lončar Brzak, B.; Mravak Stipetić, M. Ljestvice za procjenu oralnog mukozitisa. Medix 2014, 20, 213–216. [Google Scholar]
- Dirix, P.; Nuyts, S. Evidence—Based organ—Sparing radiotherapy in head and neck cancer. Lancet Oncol. 2010, 11, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Lima, R.B.; De Vasconcelos, L.C.; Pontual, M.L.; Meireles, S.S.; Andrade, A.K.M.; Duarte, R.M. Effect of ionizing radiation on the properties of restorative materials. Indian J. Dent. Res. 2019, 30, 408–413. [Google Scholar] [CrossRef]
- Turjanski, S.; Par, M.; Bergman, L.; Soce, M.; Grego, T.; Klaric Sever, E. Influence of ionizing radiation on fluoride-releasing dental restorative materials. Polymers 2023, 15, 632. [Google Scholar] [CrossRef]
- Atalay, C.; Yazici, R. Effect of radiotherapy on the surface roughness and microhardness of contemporary bioactive restorative materials. Support. Care Cancer 2024, 32, 295. [Google Scholar] [CrossRef]

| Material | Type | Manufacturer | Composition | Lot |
|---|---|---|---|---|
| GC Equia Forte HT | Bulk-fill glass hybrid | GC Corp., Tokyo, Japan | Powder: fuoroaluminosilicate glass, polyacrylic. Liquid: polybasic carboxylic acid, water. | 230310B |
| Cention N | non-adhesive bulk-fill resinous material | Ivoclar AG; Schaan, Liechtenstein | Powder: barium aluminum silicate glass, ytterbium trifuoride, isofller, calcium barium, aluminum fuorosilicate glass, calcium fuoro, silicate glass. Liquid: urethane dimethacrylate, tricyclodecandimethanol dimethacrylate, tetramethylxylylene diurethane dimethacrylate, polyethylene glycol 400 dimethacrylate, ivocerin, Hydroxyperoxide. | ZL08SP |
| Tetric EvoCeram | Sculptable composite | Ivoclar AG; Schaan, Liechtenstein | The monomer matrix is composed of dimethacrylates (20–21 wt.%). The fillers contain barium glass, ytterbium trifluoride, mixed oxide and copolymers (79–81 wt.%). Additives, initiators, stabilizers and pigments are additional ingredients (<1.0 wt.%). The total content of inorganic fillers is 76–77% weight or 53–54% volume. The particle sizes of the inorganic fillers range between 40 nm and 3 μm. | Z01V79 |
| Tetric PowerFill | Sculptable composite | Ivoclar AG; Schaan, Liechtenstein | The monomer matrix is composed of dimethacrylates (20–21 wt.%). The fillers contain barium glass, ytterbium trifluoride, mixed oxide and copolymers (79–80 wt.%). Additives, initiators, stabilizers and pigments are additional ingredients (<1.0 wt.%). The total content of inorganic fillers is 76–77 wt.% or 53–54 vol%. The particle size of inorganic fillers is between 40 nm and 3 μm. | Z009GW |
| Mass | Control | 2 Gy/35 Days | Shock Dose (70 Gy) | ||
|---|---|---|---|---|---|
| Materials | Median (IQR) | Median (IQR) | p Value | Median (IQR) | p Value |
| CEN | 0.104 (0.095–0.114) | 0.103 (0.094–0.113) | 0.112 | 0.104 (0.096–0.115) | 0.415 |
| EQ | 0.110 (0.107–0.114) | 0.100 (0.094–0.106) | 0.001 | 0.105 (0.101–0.111) | 0.005 |
| PF | 0.122 (0.118–0.123) | 0.115 (0.110–0.121) | 0.005 | 0.122 (0.120–0.125) | 0.169 |
| EC | 0.121 (0.118–0.124) | 0.117 (0.113–0.122) | 0.005 | 0.117 (0.114–0.123) | 0.005 |
| Surface Microhardness | Pre-2 Gy/35 Days | Post-2 Gy/35 Days | p Value | Pre-Shock Dose (70 Gy) | Post-Shock Dose (70 Gy) | p Value |
|---|---|---|---|---|---|---|
| Materials | Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | ||
| CEN | 50.3 (47.4–54.9) | 50.1 (47.2–53.8) | 0.285 | 49.4 (45.2–52.0) | 49.4 (45.2–51.9) | 0.203 |
| EQ | 100.1 (77.6–109.7) | 99.9 (77.1–109.0) | 0.007 | 98.5 (95.1–102.9) | 98.6 (94.8–101.1) | 0.232 |
| PF | 74.4 (58.8–77.8) | 74.0 (59.6–77.4) | 0.721 | 80.6 (54.1–86.9) | 80.2 (50.2–86.7) | 0.006 |
| EC | 64.9 (62.5–68.6) | 65.2 (62.3–68.3) | 0.285 | 65.9 (60.3–69.8) | 66.4 (60.2–69.7) | 0.878 |
| T-Test for Dependant Samples Marked Differences Are Significant at p ˂ 0.0500 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean | Std.Dv. | N | Diff. | Std.Dv. | t | df | p | Confidence | Confidence |
| L before CEN | 68.640 | 3.712 | ||||||||
| L after CEN | 67.460 | 5.763 | 10 | 1.180 | 8.086 | 0.461 | 9 | 0.655 | −4.604 | 6.964 |
| L before EQ | 57.810 | 4.383 | ||||||||
| L after EQ | 57.260 | 5.040 | 10 | 0.550 | 6.628 | 0.262 | 9 | 0.798 | −4.191 | 5.291 |
| L before PF | 69.690 | 2.679 | ||||||||
| L after PF | 67.910 | 4.779 | 10 | 1.780 | 4.870 | 1.155 | 9 | 0.2775 | −4.604 | 6.964 |
| L before EC | 65.130 | 2.897 | ||||||||
| L after EC | 67.750 | 4.678 | 10 | −2.622 | 5.003 | −1.655 | 9 | 0.132 | −6.199 | 0.959 |
| T-Test for Dependant Samples Marked Differences Are Significant at p ˂ 0.0500 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean | Std.Dv. | N | Diff. | Std.Dv. | t | df | p | Confidence | Confidence |
| L before CEN | 68.640 | 3.712 | ||||||||
| L after CEN | 77.730 | 2.807 | 10 | −9.090 | 5.088 | −5.649 | 9 | 0.003 | −12.729 | −5.450 |
| L before EQ | 57.810 | 4.383 | ||||||||
| L after EQ | 63.140 | 2.270 | 10 | −5.330 | 5.053 | −3.336 | 9 | 0.008 | −8.944 | −1.715 |
| L before PF | 69.690 | 2.679 | ||||||||
| L after PF | 70.580 | 5.211 | 10 | −0.890 | 5.332 | −0.527 | 9 | 0.610 | −4.704 | 2.942 |
| L before EC | 65.130 | 2.897 | ||||||||
| L after EC | 74.140 | 3.678 | 10 | −9.100 | 4.788 | −5.950 | 9 | 0.000 | −12.435 | −5.584 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klarić, E.; Špiljak, B.; Šimunović, L.; Soče, M.; Grego, T.; Ivanišević, A. The Influence of Ionizing Radiation on the Morphological Structure of the Fluoride-Releasing Restorative Materials in Cancer Patients: An In Vitro Study. Sci 2024, 6, 47. https://doi.org/10.3390/sci6030047
Klarić E, Špiljak B, Šimunović L, Soče M, Grego T, Ivanišević A. The Influence of Ionizing Radiation on the Morphological Structure of the Fluoride-Releasing Restorative Materials in Cancer Patients: An In Vitro Study. Sci. 2024; 6(3):47. https://doi.org/10.3390/sci6030047
Chicago/Turabian StyleKlarić, Eva, Bruno Špiljak, Luka Šimunović, Majana Soče, Timor Grego, and Ana Ivanišević. 2024. "The Influence of Ionizing Radiation on the Morphological Structure of the Fluoride-Releasing Restorative Materials in Cancer Patients: An In Vitro Study" Sci 6, no. 3: 47. https://doi.org/10.3390/sci6030047
APA StyleKlarić, E., Špiljak, B., Šimunović, L., Soče, M., Grego, T., & Ivanišević, A. (2024). The Influence of Ionizing Radiation on the Morphological Structure of the Fluoride-Releasing Restorative Materials in Cancer Patients: An In Vitro Study. Sci, 6(3), 47. https://doi.org/10.3390/sci6030047






