Pediatric Foreign Body Ingestion: Complications and Patient and Foreign Body Factors
Abstract
:1. Introduction
2. Risk of Complication: Patient Factors
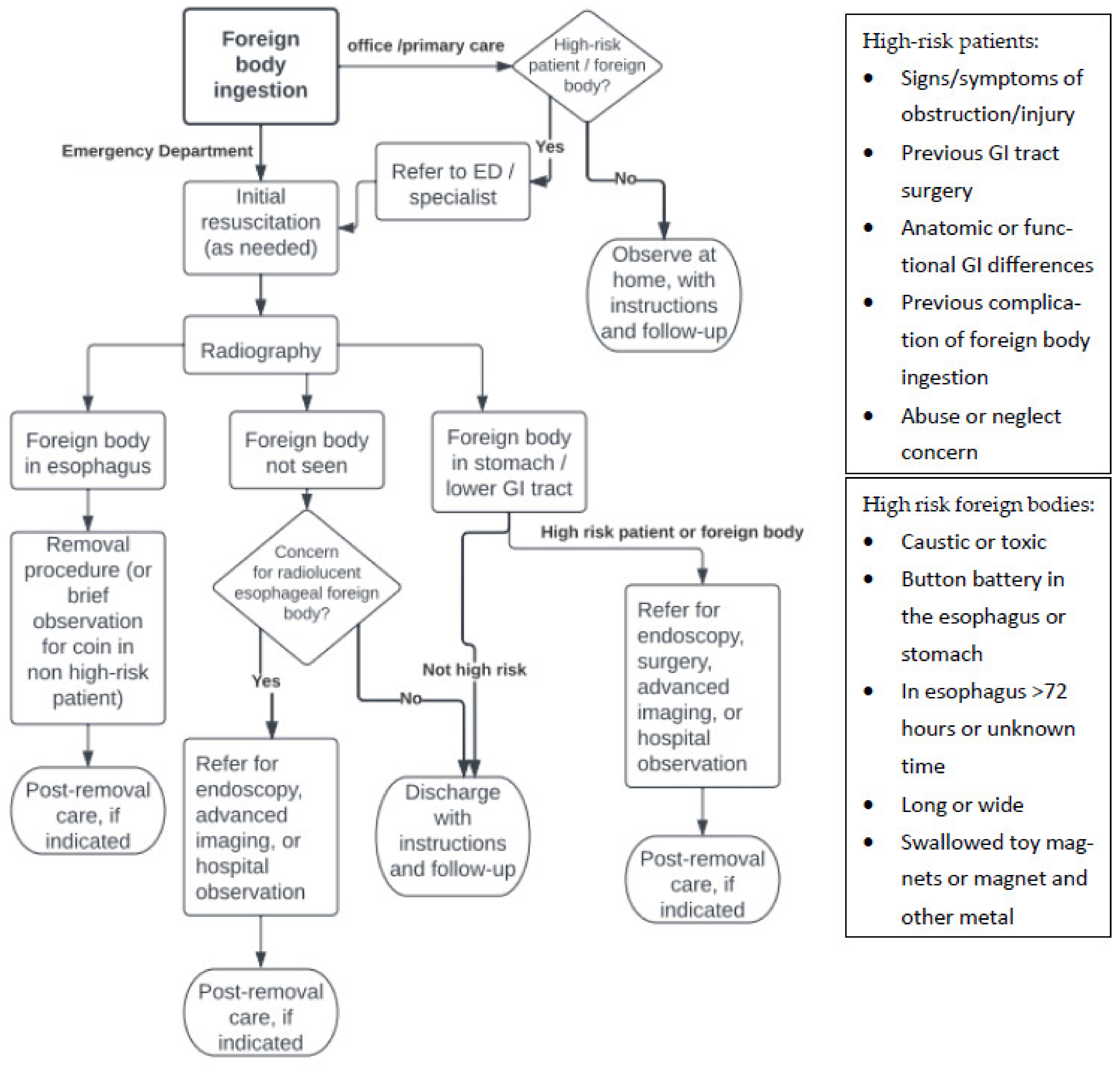
3. Risk of Complication: Foreign Body Factors
4. Patient Presentation
4.1. Emergency Management
4.2. History and Physical Examination
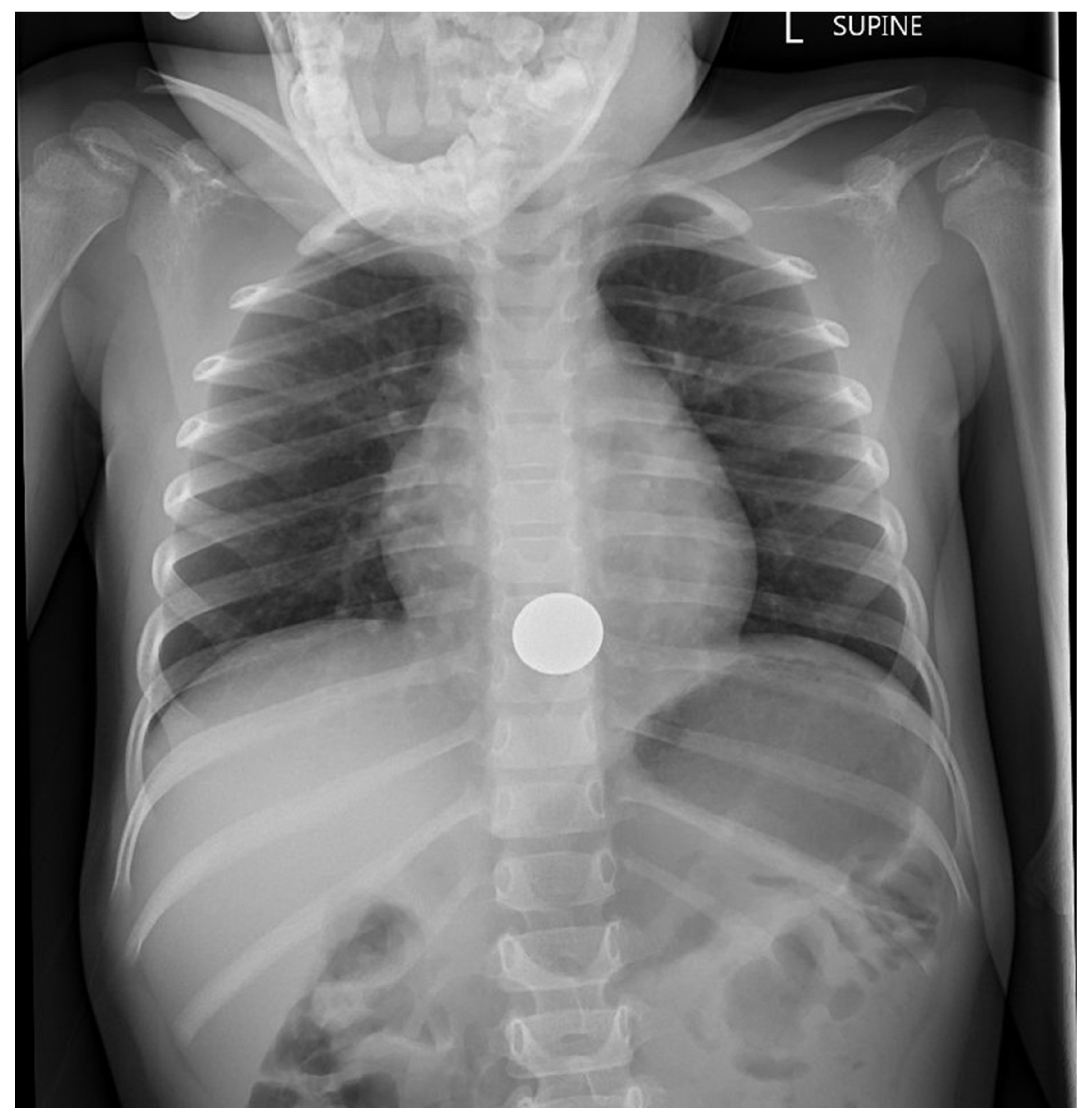
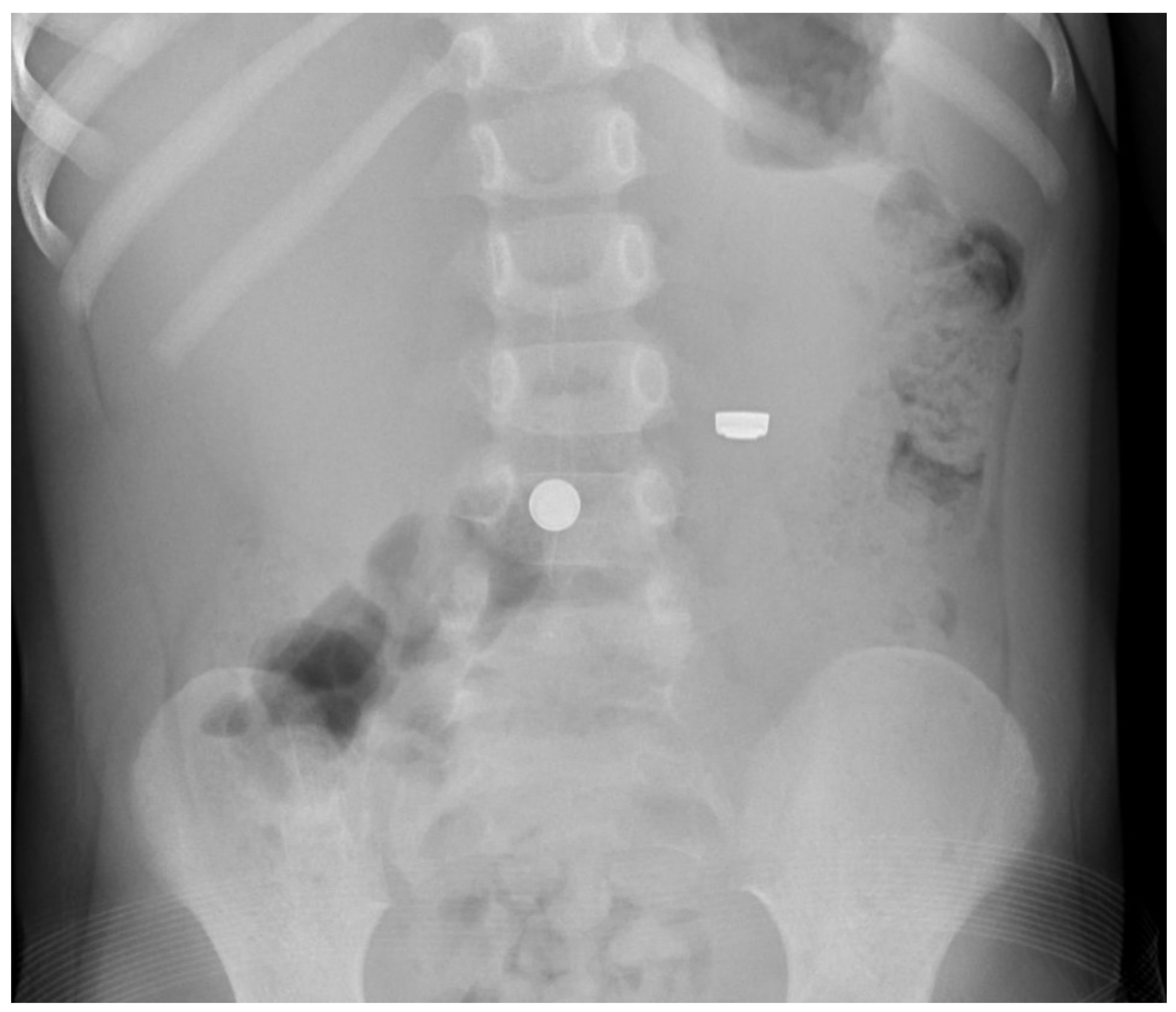
4.3. Imaging
4.4. Management
4.5. Postremoval Care
5. Prevention
6. Conclusions
Funding
Informed Consent Statement
Conflicts of Interest
References
- Conners, G.P.; Chamberlain, J.M.; Weiner, P.R. Pediatric coin ingestions: A home-based survey. Am. J. Emerg. Med. 1995, 13, 638–640. [Google Scholar] [CrossRef]
- Paul, R.I.; Christoffel, K.K.; Binns, H.J.; Jaffe, D.M. Foreign bodies in children: Risk of complication varies with site of initial health care contact. Pediatrics 1993, 91, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Louie, J.P.; Alpern, E.; Windreich, R.M. Witnessed and unwitnessed esophageal foreign bodies in children. Pediatr. Emerg. Care 2005, 21, 582–585. [Google Scholar] [CrossRef] [PubMed]
- Crysdale, W.S.; Sendi, K.S.; Yoo, J. Esophageal foreign bodies in children: 15-year review of 484 cases. Ann. Otol. Rhinol. Laryngol. 1991, 100, 320–324. [Google Scholar] [CrossRef] [PubMed]
- Stanley, P.; Law, B.S.; Young, L.W. Down’s syndrome, duodenal stenosis/annular pancreas, and a stack of coins. Am. J. Dis. Child. 1988, 142, 459–460. [Google Scholar]
- Shakir, A.K.; Ramji, F.; El Halabi, I. Penny for your thoughts; a coin in the stomach: Why did it get stuck? Hosp. Pediatr. 2017, 7, 294–296. [Google Scholar] [CrossRef] [Green Version]
- Stringer, M.D.; Kiely, E.M.; Drake, D.P. Gastric retention of swallowed coins after pyloromyotomy. Br. J. Clin. Pract. 1991, 45, 66–67. [Google Scholar]
- Denney, W.; Ahmad, N.; Billard, B.; Nowicki, M. Children will eat the strangest things: A 10—year retrospective analysis of foreign body and caustic ingestions from a single academic center. Pediatr. Emerg. Care 2012, 28, 731–734. [Google Scholar] [CrossRef]
- Kaye, E.T.; Sax, C.F.; DiPietro, E.K.; Wong, A.H.C.; Leung, A.K.C. Systemic nickel hypersensitivity from a swallowed coin. Consult. Pediatr. 2012, 52, 275–277. [Google Scholar]
- Slim, R.; Geagea, A.; Yaghi, C.; Honein, K.; Sayegh, R.; Zoghbi, A. Unusual way of purging. Emerg. Med. J. 2006, 23, 486. [Google Scholar] [CrossRef]
- Paul, R.I.; Jaffe, D.M. Sharp object ingestions in children: Illustrative cases and literature review. Pediatr. Emerg. Care 1988, 4, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Pak, M.W.; Lee, W.C.; Fung, H.K.; van Hasselt, C.A. A prospective study of foreign-body ingestion in 311 cases. J. Paediatr. Child Health 2001, 58, 37–45. [Google Scholar]
- Hashmonai, M.; Kaufman, T.; Schramek, A. Silent perforations of the stomach and duodenum by needles. Arch. Surg. 1978, 113, 1406–1409. [Google Scholar] [CrossRef] [PubMed]
- Litovitz, T.; Whitaker, N.; Clark, L.; White, N.C.; Marsolek, M. Emerging battery-ingestion hazard: Clinical implications. Pediatrics 2010, 125, 1168–1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- National Capital Poison Center Button Battery Ingestion Triage and Treatment Guideline. Available online: https://www.poison.org/battery/guideline (accessed on 7 April 2020).
- Arfang, R.R.; Jatana, K.R.; Linn, R.L.; Rhoades, K.; Fry, J.; Jacobs, I.N. pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury. Laryngoscope 2019, 129, 49–57. [Google Scholar] [CrossRef]
- Hussain, S.Z.; Bousvaros, A.; Gilger, M.; Mamula, P.; Gupta, S.; Kramer, R.; Noel, R.A. Management of ingested magnets in children. J. Pediatr. Gastroenterol. Nutr. 2012, 55, 239–242. [Google Scholar] [CrossRef]
- Strickland, M.; Diamond, I.R.; Rosenfield, D. Case discussions and radiographic illustration of magnet-related injuries in children. J. Emerg. Med. 2020, 58, 902–909. [Google Scholar] [CrossRef]
- Pogorelic, Z.; Boric, M.; Markic, J.; Jukic, M.; Grandic, L. A case of a 2-year-old child with entero-enteric fistula following ingestion of 25 magnets. Acta Med. 2016, 59, 140–142. [Google Scholar] [CrossRef] [Green Version]
- Shastri, N.; Leys, C.; Fowler, M.; Conners, G.P. Pediatric button battery and small magnet co-ingestion: Two cases with different outcomes. Pediatr. Emerg. Care 2011, 27, 642–644. [Google Scholar] [CrossRef]
- Conners, G.P.; Chamberlain, J.M.; Ochsenschlager, D.W. Symptoms and spontaneous passage of esophageal coins. Arch. Pediatr. Adolesc. Med. 1995, 149, 36–39. [Google Scholar] [CrossRef]
- Brayer, A.F.; Sciera, M.; Conners, G.P. Pediatric coin ingestion: An unusual presentation. Int. J. Pediatr. Otorhinolaryngol. 2000, 55, 211–213. [Google Scholar] [CrossRef]
- Joseph, P.R. Management of coin ingestion. Arch. Pediatr. Adolesc. Med. 1990, 144, 449–450. [Google Scholar] [CrossRef] [PubMed]
- Johansen, A.; Conners, G.P.; Lee, J.; Robinson, A.L.; Chew, W.L.; Chan, S.S. Pediatric esophageal foreign body: Possible role for digital tomosynthesis. Pediatr. Emerg. Care 2021, 37, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Shatani, N.; Alshaibani, S.; Potts, J.; Phillips, B.; Bray, H. Chest radiograph alone is sufficient as the foreign body survey for children presenting with coin ingestion. Pediatr. Emerg. Care 2021, 37, e524–e527. [Google Scholar] [CrossRef]
- Valente, J.H.; Lemke, T.; Ridlen, M.; Ritter, D.; Clyne, B.; Reinert, S.E. Aluminum foreign bodies: Do they show up on X-ray? Emerg. Radiol. 2006, 12, 30–33. [Google Scholar] [CrossRef]
- Takahashi, J.; Shiga, T.; Funakoshi, H. Oesophageal coins invisible on chest radiography: A case report. Int. J. Emerg. Med. 2017, 10, 27. [Google Scholar] [CrossRef]
- Conners, G.P. Diagnostic uses of metal detectors: A review. Int. J. Clin. Pract. 2005, 59, 946–949. [Google Scholar] [CrossRef]
- Lafferty, M.; Lyttle, M.K.; Mullen, N.; on behalf of PERUKI. Ingestion of metallic foreign bodies: A paediatric emergency research in the United Kingdom and Ireland survey of current practice and hand-held metal detector use. J. Paediatr. Child Health 2021, 57, 867–871. [Google Scholar] [CrossRef]
- Mori, T.; Nomura, O.; Hagiwara, Y. Another application of point-of-care ultrasound: Detection of esophageal foreign bodies in pediatric patients. Pediatr. Emerg. Care 2019, 35, 154–156. [Google Scholar] [CrossRef]
- Dowd, M.D. Esophageal coins. Arch. Pediatr. Adolesc. Med. 1994, 148, 423–424. [Google Scholar] [CrossRef]
- Conners, G.P.; Hadley, J.A. Esophageal coin with an unusual radiographic appearance. Pediatr. Emerg. Care 2005, 21, 667–669. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Milkovich, S.; Stool, D.; Reilly, J.; Rider, G. Pediatric coin ingestion and aspiration. Int. J. Pediatr. Otorhinolaryngol. 2005, 70, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Swischuk, L.E. Swallowed a coin. Well-maybe not. Pediatr. Emerg. Care 2007, 23, 47–48. [Google Scholar] [CrossRef] [PubMed]
- Jackson, J.T.; Conners, G.P. Radiographic identification of an esophageal United States one cent coin. Vis. J. Emerg. Med. 2017, 9, 31–32. [Google Scholar] [CrossRef]
- Voelker, J.; Voelker, C.; Voelker, J.; Engert, J.; Schendzielorz, P.; Hagen, R.; Rak, K. Button batteries and typical swallowed foreign bodies can be differentiated in high-resolution x-rays. Int. J. Pediatr. Otorhinolaryngol. 2021, 142, 110604. [Google Scholar] [CrossRef]
- Silverberg, M.; Tillotson, R. Esophageal foreign body mistaken for impacted button battery. Pediatr. Emerg. Care 2006, 22, 262–265. [Google Scholar] [CrossRef]
- Cutajar, J.; Astl, J.; Borg, C. Radiologically aligned triple coin impaction in the upper oesophagus: The value of second-look oesophagoscopy. Int. J. Pediatr. Otorhinolaryngol. Extra 2011, 6, 192–194. [Google Scholar] [CrossRef]
- Esparaz, J.R.; Carter, S.R.; Mathis, M.S.; Chen, M.K.; Russell, R.T. Esophageal foreign body management in children: Can it wait? J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 1286–1288. [Google Scholar] [CrossRef]
- Conners, G.P. A literature-based comparison of three methods of pediatric esophageal coin removal. Pediatr. Emerg. Care 1997, 13, 154–157. [Google Scholar] [CrossRef]
- Gonzalez, K.W.; Reddy, S.R.; Mundakkal, A.A.; St Peter, S.D. The financial impact of flipping the coin. J. Pediatr. Surg. 2017, 52, 153–155. [Google Scholar] [CrossRef]
- Heinzerling, N.P.; Christensen, M.A.; Swedler, R.; Cassidy, L.D.; Calkins, C.M.; Sato, T.T. Safe and effective management of esophageal coins in children with bougienage. Surgery 2015, 158, 1065–2015. [Google Scholar] [CrossRef] [PubMed]
- Kramer, R.E.; Lerner, D.G.; Lin, T.; Manfredi, M.; Shah, M.; Stephen, T.C.; Gibbons, T.E.; Pall, H.; Sahn, B.; McOmber, M.; et al. Management of ingested foreign bodies in children: A clinical report of the NASPGHAN endoscopy committee. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 562–574. [Google Scholar] [CrossRef] [PubMed]
- Lao, J.; Bostwick, H.E.; Berezin, S.; Halata, M.; Newman, L.J.; Medow, M.S. Esophageal food impaction in children. Pediatr. Emerg. Care 2003, 19, 402–407. [Google Scholar] [CrossRef]
- Peksa, G.D.; DeMott, J.M.; Slocum, G.W.; Burkins, J.; Gottlieb, M. Glucagon for relief of acute esophageal foreign bodies and food impactions: A systematic review and meta-analysis. Pharmacotherapy 2019, 39, 463–472. [Google Scholar] [CrossRef] [PubMed]
- Halverson, J.M.; Butterman, M.K.; Legier, J.F.; Mann, W.J.; Hoefer, R.A. Perforation of a Meckel’s diverticulum caused by ingestion of a coin. South. Med. J. 1994, 87, 823–824. [Google Scholar] [CrossRef]
- Khalaf, R.T.; Ruan, W.; Orkin, S.; Wilsey, M.; Fishman, D.S.; Mallon, D.; Pan, Z.; Hazleton, K.Z.; Kramer, R.E.; Walker, T. Gastric injury secondary to button battery ingestions in children: A retrospective multicenter review. Gastrointest. Endosc. 2020, 92, 276–283. [Google Scholar] [CrossRef]
- Rios, G.; Rodriguez, L.; Lucero, Y.; Miquel, I.; Arancibia, M.E.; Alliende, F. Endoscopic findings associated with button battery ingestion in children: Do we need to change the protocol for managing gastric location? Pediatr. Emerg. Care 2020, 36, 523–526. [Google Scholar] [CrossRef]
- Middelberg, L.K.; Funk, A.R.; Hays, H.L.; McKenzie, L.B.; Rudolph, B.; Spiller, H.A. Magnet injuries in children: An analysis of the National Poison Data System from 2008 to 2019. J. Pediatr. 2021, 232, 251–256. [Google Scholar] [CrossRef]
- Turgut, K.; Poyraz, M.K.; Sekmen, E.; Aydin, I.; Algin, A.; Yavuz, E. Prevalence of attention deficit hyperactivity (ADHD) in children presenting with foreign body ingestion. Am. J. Emerg. Med. 2019, 37, 2121–2124. [Google Scholar] [CrossRef]
- Pizzol, A.; Rigazio, C.; Calvo, P.L.; Scottoni, F.; Pane, A.; Genneri, F.; Cisaro, F. Foreign-body ingestions in children during COVID-19 pandemic in a pediatric referral center. JPGN Rep. 2020, 1, e018. [Google Scholar] [CrossRef]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Conners, G.P. Pediatric Foreign Body Ingestion: Complications and Patient and Foreign Body Factors. Sci 2022, 4, 20. https://doi.org/10.3390/sci4020020
Conners GP. Pediatric Foreign Body Ingestion: Complications and Patient and Foreign Body Factors. Sci. 2022; 4(2):20. https://doi.org/10.3390/sci4020020
Chicago/Turabian StyleConners, Gregory P. 2022. "Pediatric Foreign Body Ingestion: Complications and Patient and Foreign Body Factors" Sci 4, no. 2: 20. https://doi.org/10.3390/sci4020020
APA StyleConners, G. P. (2022). Pediatric Foreign Body Ingestion: Complications and Patient and Foreign Body Factors. Sci, 4(2), 20. https://doi.org/10.3390/sci4020020




