Optimal Timing for Intraocular Pressure Measurement Following Phacoemulsification Cataract Surgery: A Systematic Review and a Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Risk of Bias Assessment
2.4. Data Extraction
2.5. Statistical Analysis
3. Results
3.1. Search Results
3.2. Study Characteristics
3.3. Risk of Bias Assessment Results
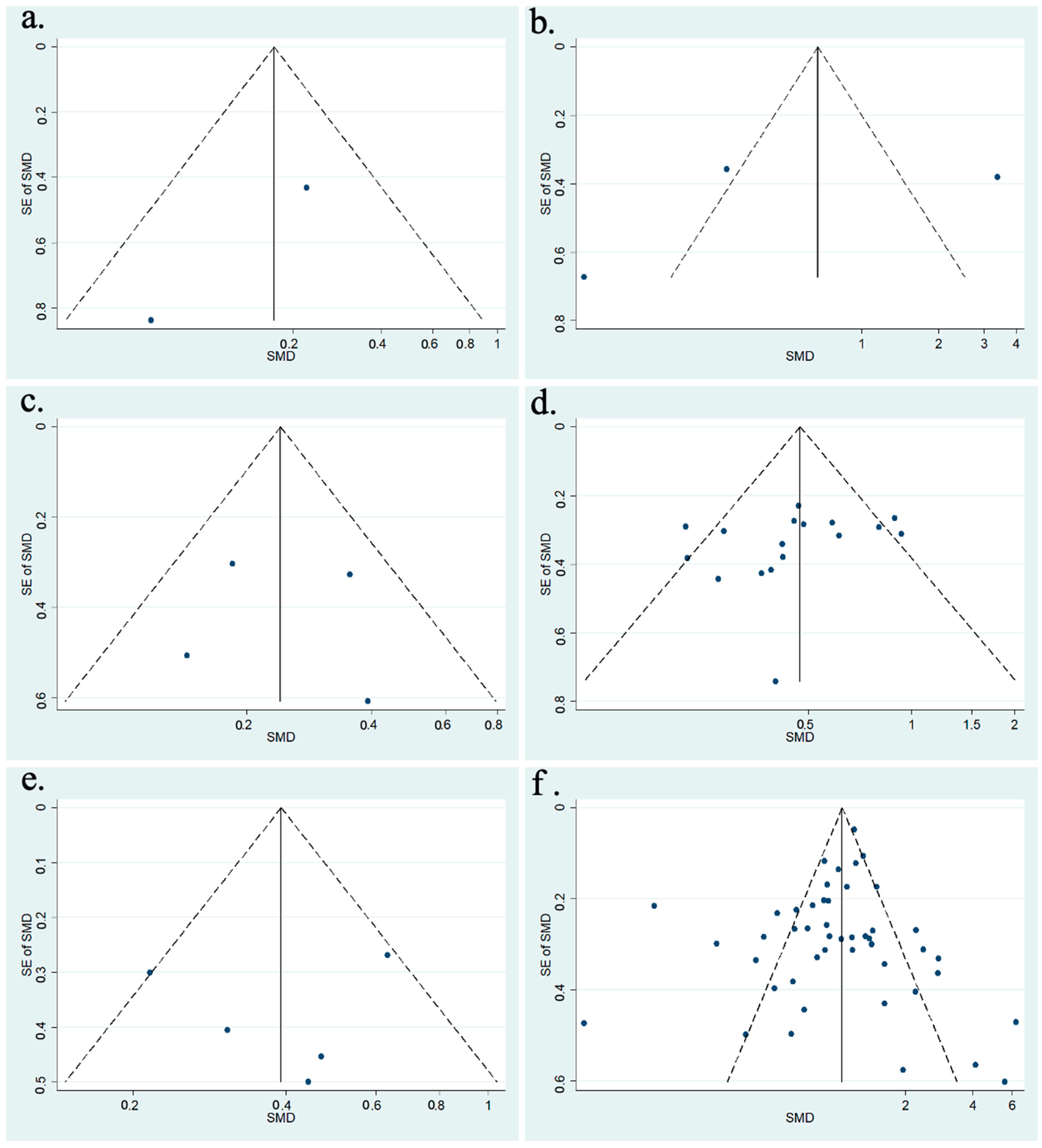
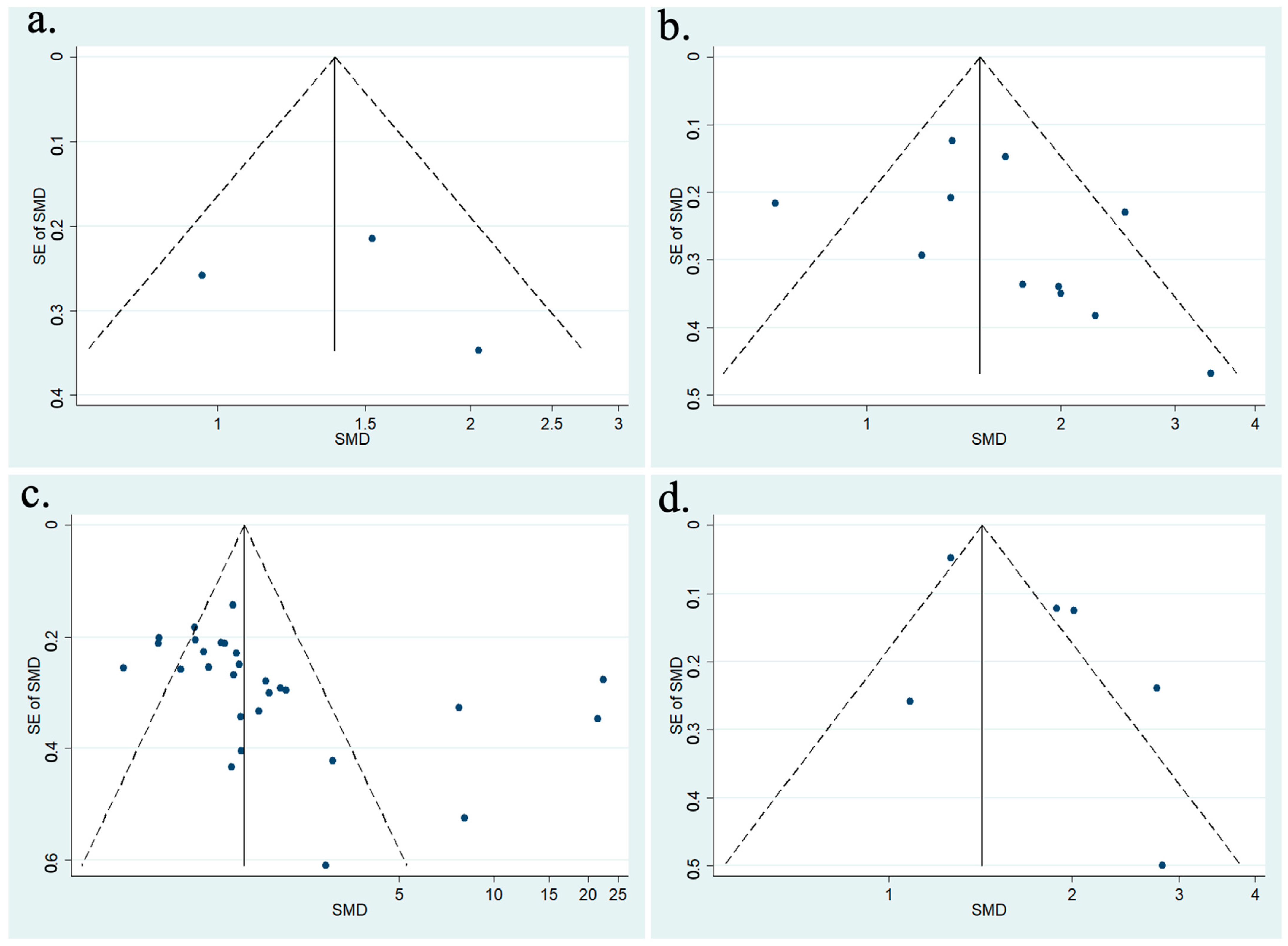
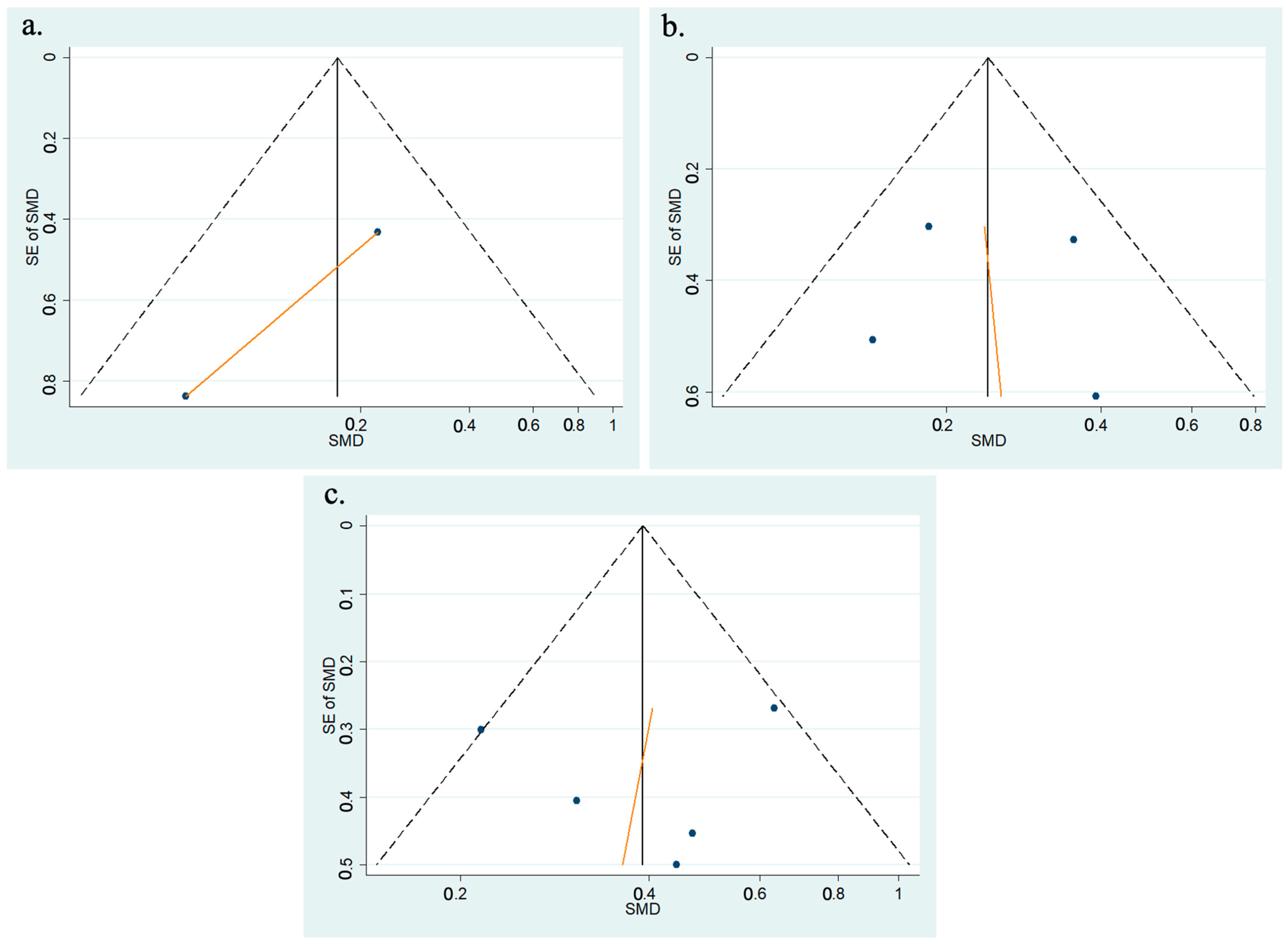
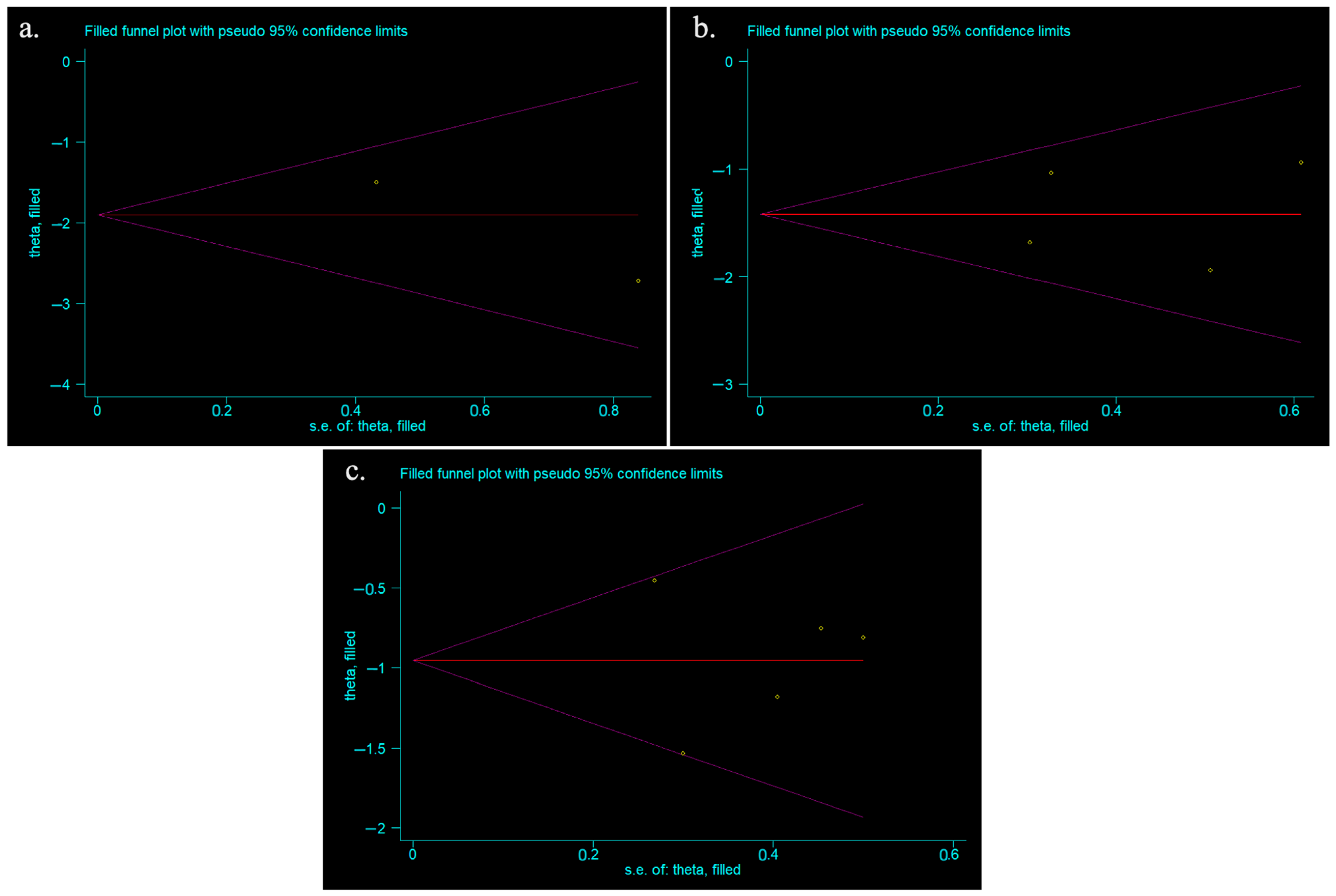
3.4. Publication Bias
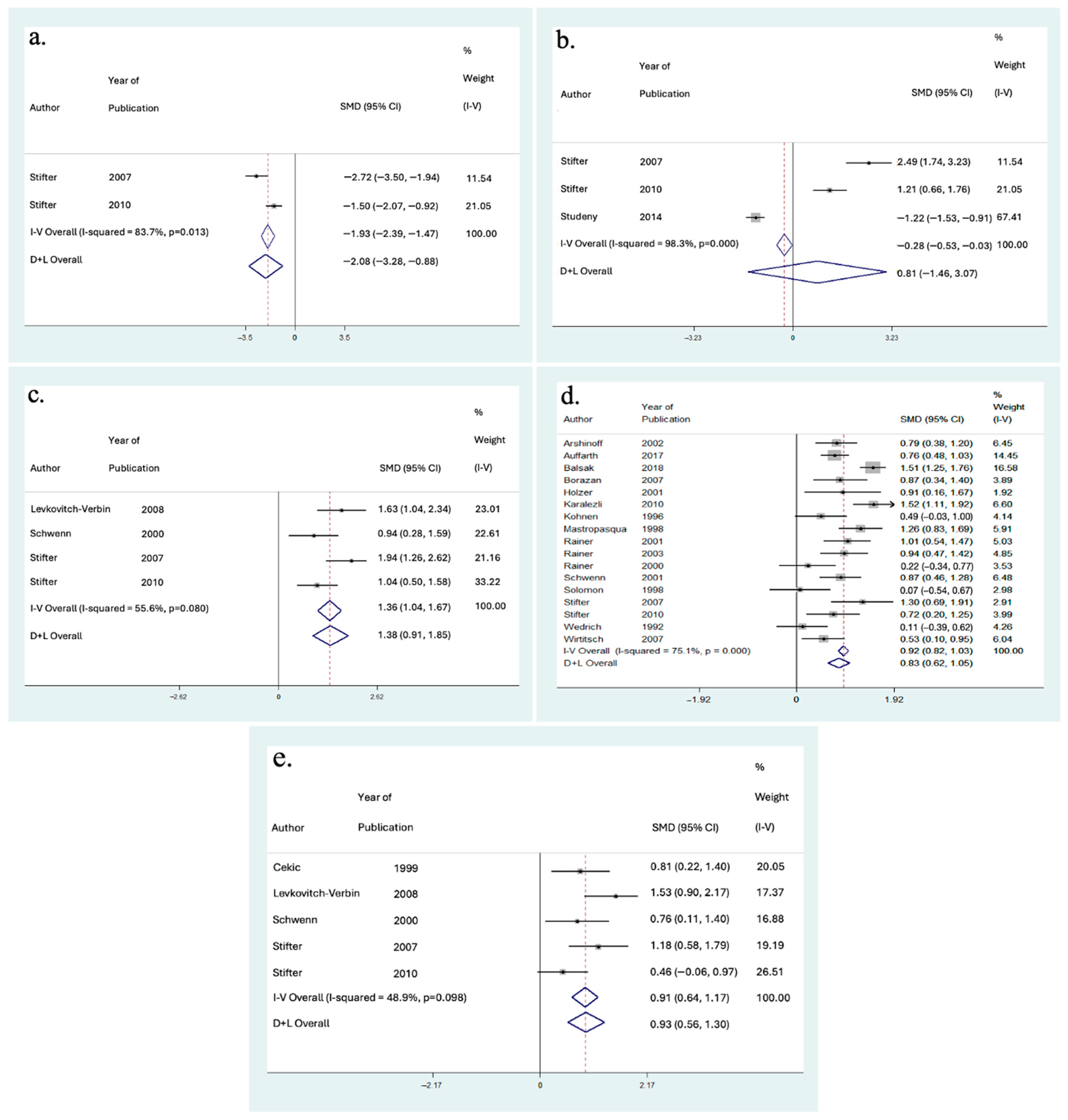
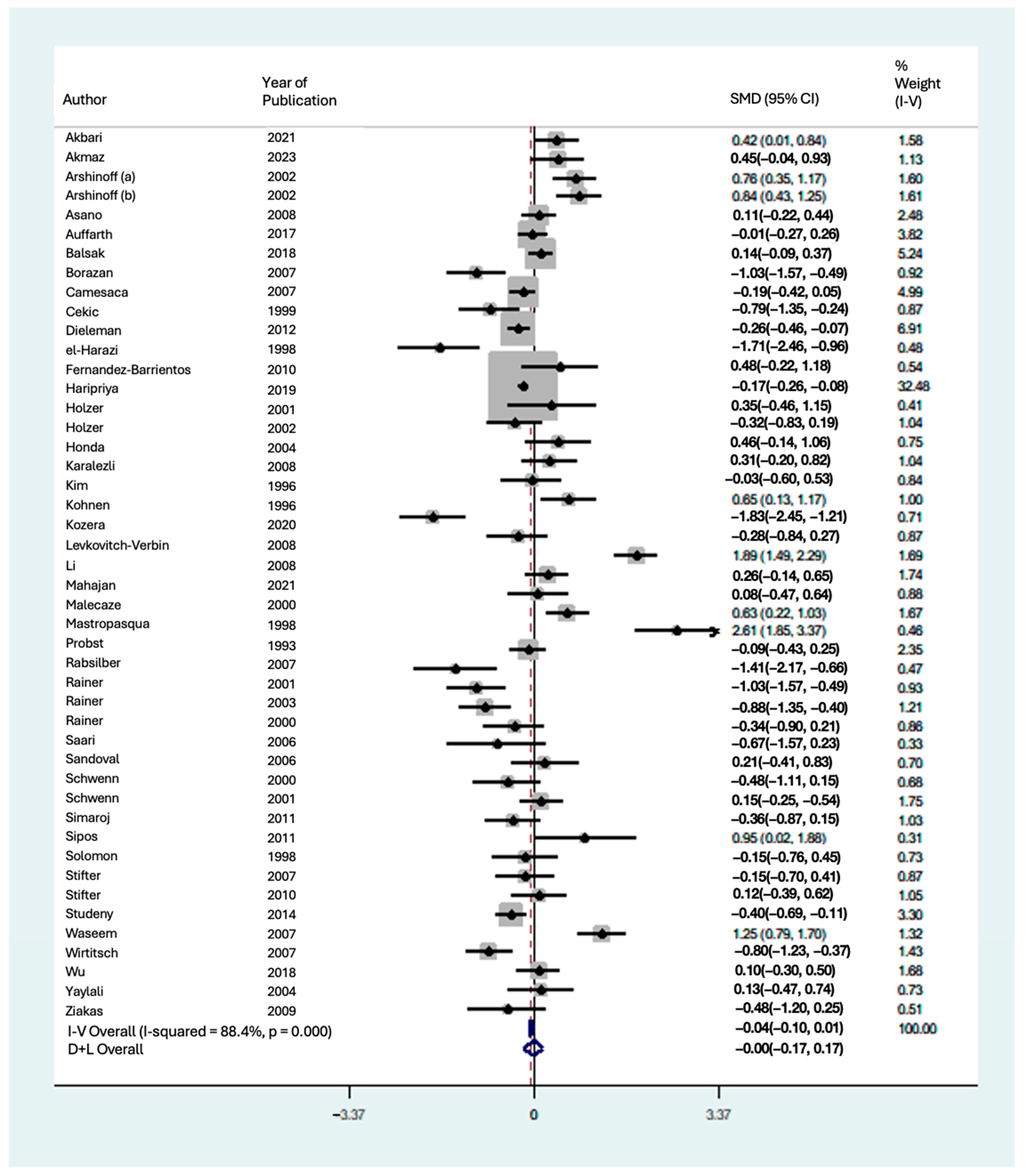
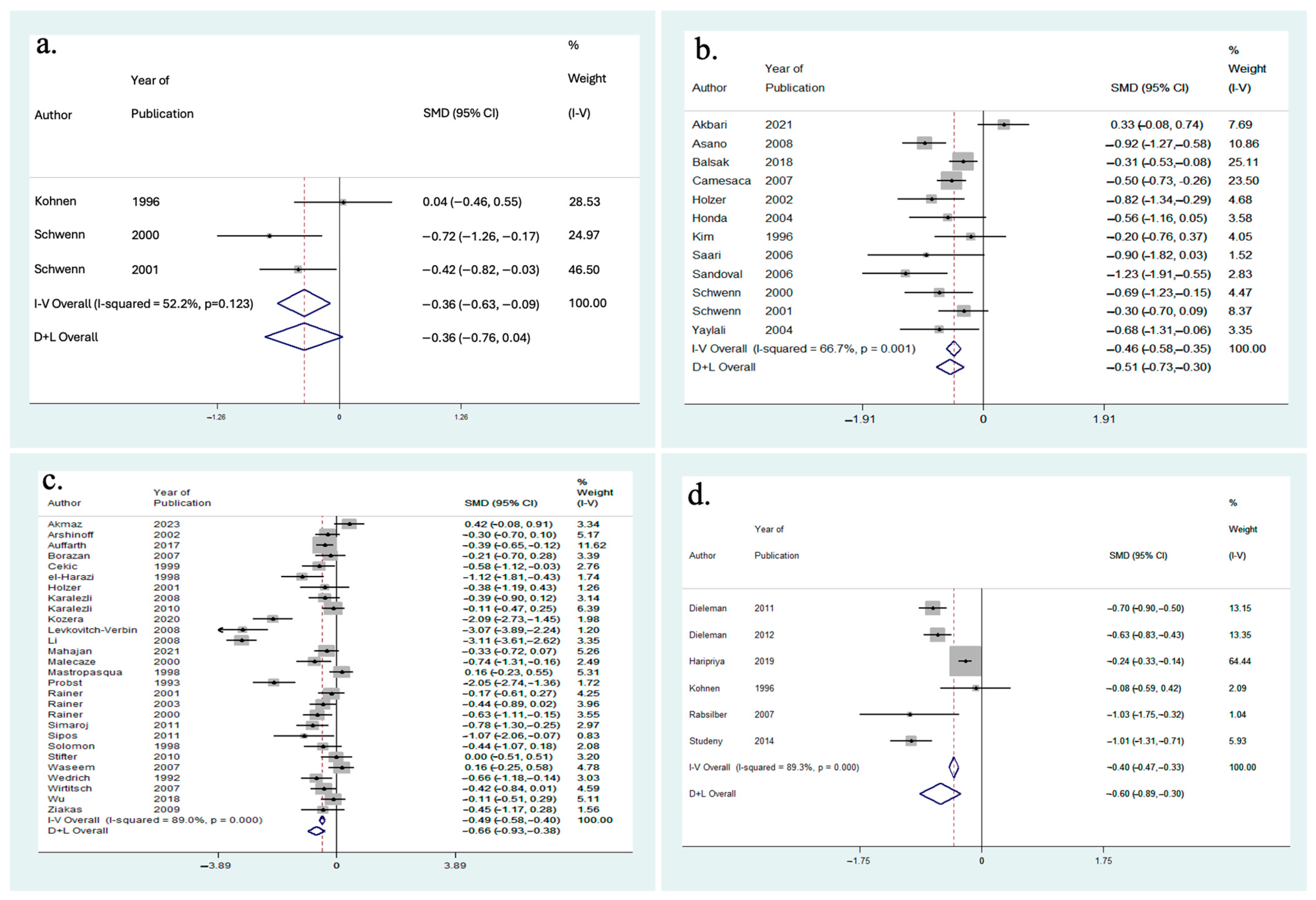
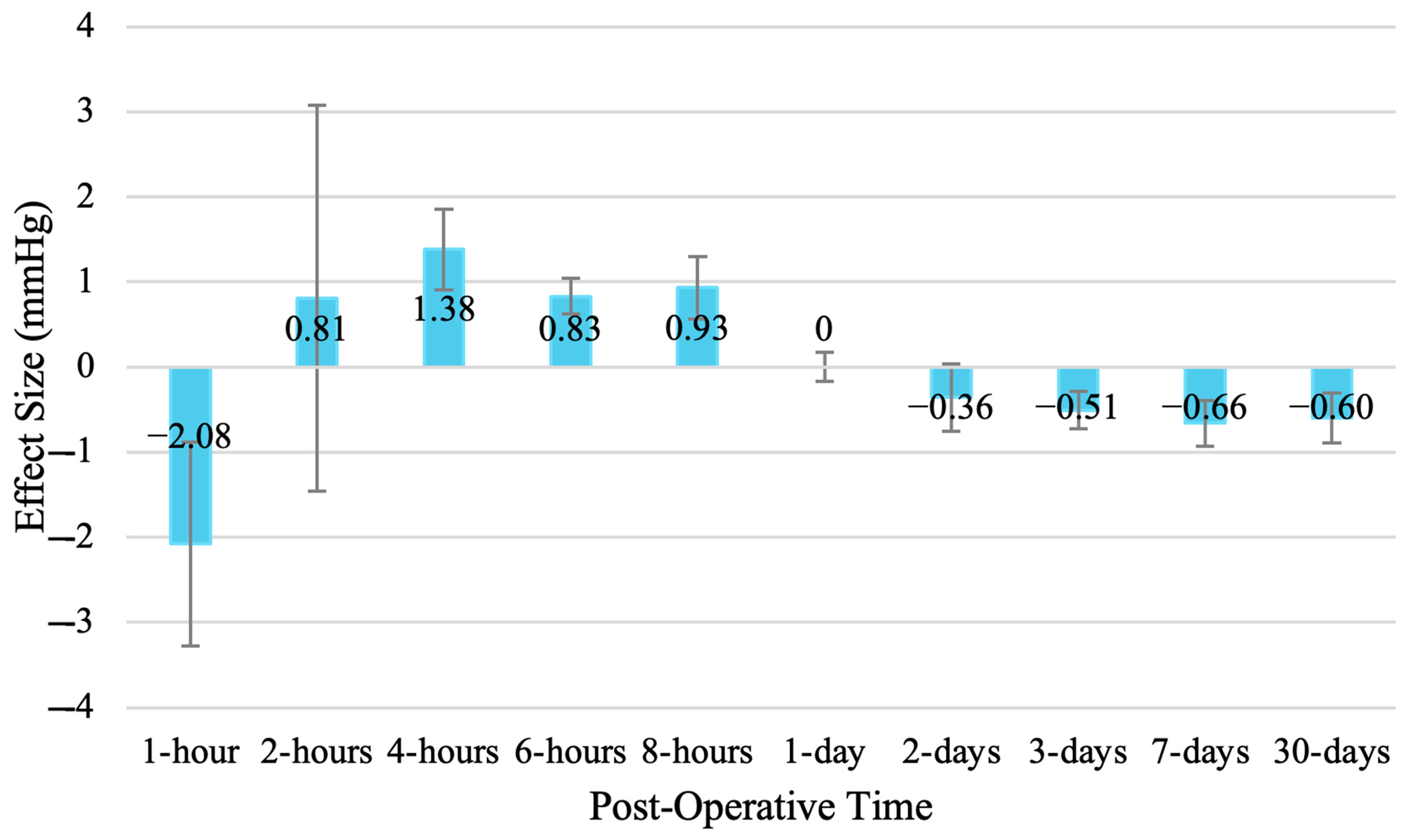
3.5. Effect on IOP
3.6. Surgical Parameters
3.7. Medications Administered
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Author | Year | Study Design | Study Location | Total Number of Participants, N | Total Number of Eyes, N | Age, Mean (SD); Range; N (%), etc. | Male Eyes, N (%) | Disease Population of Interest |
|---|---|---|---|---|---|---|---|---|
| Akbari et al. [15] | 2021 | Randomized Clinical Trial | Iran | 88 | 88 | 71.6 (7.8) | 41 (46.6) | Cataract with PEX |
| Akmaz et al. [16] | 2023 | Randomized Clinical Trial | Turkey | 65 | 65 | 66.6 (8.8) | 34 (52.3) | Cataract only |
| Arshinoff et al. [17] | 2002 | Randomized Clinical Trial | Canada | 99 | 198 | 71.7 (8.6) | 96 (48.5) | Cataract only |
| Asano et al. [18] | 2008 | Randomized Clinical Trial | Japan | 142 | 142 | 66.2 (5.5) | 63 (44.4) | Cataract only |
| Auffarth et al. [19] | 2017 | Randomized Clinical Trial | Multicenter (Europe) | 220 | 220 | 72.2 (7.6) | 84 (38.2) | Cataract only |
| Balsak et al. [20] | 2018 | Randomized Clinical Trial | Turkey | 257 | 277 | 65.9 (13.9) | 142 (51.2) | Cataract only |
| Borazan et al. [21] | 2007 | Randomized Clinical Trial | Turkey | 185 | 185 | 67.1 (8.3) | 107 (57.8) | Cataract only |
| Camesaca et al. [22] | 2007 | Randomized Clinical Trial | Italy | 143 | 286 | 73.7 (8.9) | 53 (18.5) | Cataract only |
| Cekic et al. [23] | 1999 | Randomized Clinical Trial | Turkey | 51 | 51 | 55.7 (-) | 30 (58.8) | Cataract only |
| Cekic et al. [24] | 1999 | Randomized Clinical Trial | Turkey | 58 | 58 | 57.3 (31–78) | 35 (60.3) | Cataract only |
| Chang et al. [25] | 2017 | Randomized Clinical Trial | Sweden | 43 | 43 | 69.5 (8.3) | - | Cataract only |
| Dieleman et al. [26] | 2011 | Randomized Clinical Trial | Netherlands | 400 | 400 | 70.8 (41–91) | 158 (39.5) | Cataract only |
| Dieleman et al. [27] | 2012 | Randomized Clinical Trial | Netherlands | 400 | 400 | 70.8 (41–93) | 158 (39.5) | Cataract only |
| el-Harazi et al. [28] | 1998 | Randomized Clinical Trial | United States | 58 | 58 | 69.8 (11.0) | 30 (51.7) | Cataract only |
| Fernandez-Barrientos et al. [29] | 2010 | Randomized Clinical Trial | Spain | 16 | 16 | 76.7 (5.8) | 9 (56.3) | Cataract with Glaucoma |
| Gungor et al. [30] | 2014 | Randomized Clinical Trial | Turkey | 60 | 60 | 70.4 (9.9) | 24 (40.0) | Cataract only |
| Haripriya et al. [31] | 2019 | Randomized Clinical Trial | India | 1406 | 1406 | 61.3 (7.4) | 717 (51.0) | Cataract only and, Cataract with PEX |
| Holzer et al. [32] | 2001 | Randomized Clinical Trial | United States | 81 | 81 | 71.2 (7.6) | - | Cataract only |
| Holzer et al. [33] | 2002 | Randomized Clinical Trial | Germany | 60 | 60 | 67.9 (p = 0.62) | 21 (35.0) | Cataract only |
| Honda et al. [34] | 2004 | Randomized Clinical Trial | Japan | 44 | 44 | 61.0 (9.5) | 23 (52.3) | Cataract only |
| Karalezli et al. [35] | 2008 | Randomized Clinical Trial | Turkey | 60 | 60 | 66.0 (7.1) | 27 (45) | Cataract only |
| Karalezli et al. [36] | 2010 | Randomized Clinical Trial | Turkey | 120 | 120 | 66.6 (8.7) | 68 (56.7) | Cataract only |
| Kim et al. [37] | 1996 | Randomized Clinical Trial | Korea | 24 | 24 | 63.0 (5.5) | 9 (37.5) | Cataract only |
| Kohnen et al. [38] | 1996 | Randomized Clinical Trial | Germany | 60 | 60 | 73.2 (9.1) | - | Cataract only |
| Kozera et al. [39] | 2020 | Randomized Clinical Trial | Poland | 36 | 36 | 71.8 (6.7) | 8 (22.2) | Cataract with Glaucoma |
| Levkovitch-Verbin et al. [40] | 2008 | Randomized Clinical Trial | Israel | 122 | 122 | 75.0 (3.8) | 53 (43.4) | Cataract only, Cataract with Glaucoma, and Cataract with PEX |
| Li et al. [41] | 2008 | Randomized Clinical Trial | China | 140 | 140 | 72.4 (9.5) | 63 (45.0) | Cataract only |
| Mahajan et al. [42] | 2021 | Randomized Clinical Trial | India | 150 | 150 | 64.4 (9.4) | 72 (48.0) | Cataract only |
| Malecaze et al. [43] | 2000 | Randomized Clinical Trial | France | 50 | 50 | 75.0 (70–79) | 21 (42.0) | Cataract only |
| Mastropasqua et al. [44] | 1998 | Randomized Clinical Trial | Italy | 100 | 100 | 68.2 (11.9) | 55 (55.0) | Cataract only |
| Paganelli et al. [45] | 2004 | Randomized Clinical Trial | Brazil | 100 | 100 | 65.2 (7.9) | 48 (48.0) | Cataract only |
| Paganelli et al. [46] | 2009 | Randomized Clinical Trial | Brazil | 135 | 135 | 69.2 (8.0) | 54 (40.0) | Cataract only |
| Probst et al. [47] | 1993 | Randomized Clinical Trial | Canada | 49 | 50 | 67.6 (12.4) | 28 (56.0) | Cataract only |
| Rabsilber et al. [48] | 2007 | Randomized Clinical Trial | Germany | 17 | 34 | 70.1 (9.7) | 12 (35.3) | Cataract only |
| Rainer et al. [49] | 2000 | Randomized Clinical Trial | Austria | 25 | 50 | 75.7 (10.5) | 20 (40.0) | Cataract only |
| Rainer et al. [50] | 2000 | Randomized Clinical Trial | Austria | 35 | 70 | 75.5 (9.1) | 28 (40.0) | Cataract only |
| Rainer et al. [51] | 2001 | Randomized Clinical Trial | Austria | 40 | 80 | 75.9 (9.3) | 26 (32.5) | Cataract only |
| Rainer et al. [52] | 2001 | Randomized Clinical Trial | Austria | 40 | 80 | 69.9 (12.1) | 30 (37.5) | Cataract only |
| Rainer et al. [53] | 2001 | Randomized Clinical Trial | Austria | 30 | 60 | 64.8 (15.2) | 12 (20) | Cataract only |
| Rainer et al. [54] | 2003 | Randomized Clinical Trial | Austria | 38 | 76 | 75.6 (10.9) | 10 (13.2) | Cataract only |
| Saari et al. [55] | 2006 | Randomized Clinical Trial | Finland | 20 | 20 | 72.0 (6.3) | 8 (40.0) | Cataract only |
| Sandoval et al. [56] | 2006 | Randomized Clinical Trial | United States | 40 | 40 | 71.5 (8.4) | 18 (45.0) | Cataract only |
| Schwenn et al. [57] | 2000 | Randomized Clinical Trial | Germany | 48 | 48 | - | - | Cataract only |
| Schwenn et al. [58] | 2001 | Randomized Clinical Trial | Germany | 100 | 100 | 71.2 (12.9) | 66 (66.0) | Cataract only |
| Simaroj et al. [59] | 2011 | Randomized Clinical Trial | Thailand | 60 | 60 | 66.1 (8.1) | 24 (40.0) | Cataract only |
| Sipos et al. [60] | 2011 | Randomized Clinical Trial | Austria | 30 | 60 | 75.2 (8.3) | 22 (36.7) | Cataract only |
| Solomon et al. [61] | 1998 | Randomized Clinical Trial | United States | 41 | 41 | 66.9 (11.5) | 26 (63.4) | Cataract only |
| Stifter et al. [62] | 2007 | Randomized Clinical Trial | Austria | 50 | 100 | 77.0 (8.4) | 38 (38.0) | Cataract only |
| Stifter et al. [63] | 2010 | Randomized Clinical Trial | Austria | 30 | 60 | 79.9 (6.2) | 26 (43.0) | Cataract only |
| Studeny et al. [64] | 2014 | Randomized Clinical Trial | Czech Republic | 96 | 192 | 70.2 (8.3) | 70 (36.5) | Cataract only |
| Waseem et al. [65] | 2007 | Randomized Clinical Trial | Pakistan | 91 | 91 | - | 51 (56.0) | Cataract only |
| Wedrich et al. [66] | 1992 | Randomized Clinical Trial | Austria | 90 | 90 | 76.5 (7.2) | 11 (12.2) | Cataract only |
| Wirtitsch et al. [67] | 2007 | Randomized Clinical Trial | Austria | 44 | 88 | 76.0 (8.5) | 22 (25.0) | Cataract only |
| Wu et al. [68] | 2018 | Randomized Clinical Trial | China | 81 | 99 | 70.0 (10.0) | 21 (21.2) | Cataract only |
| Yaylali et al. [69] | 2004 | Randomized Clinical Trial | Turkey | 48 | 48 | 61.9 (12.2) | 26 (54.2) | Cataract only |
| Zebardast et al. [70] | 2020 | Randomized Clinical Trial | Multicentre (Canada, USA, Germany, Italy, Mexico, Philippines, Poland, Spain, UK) | 187 | 187 | 71.2 (7.6) | 82 (43.8) | Cataract with Glaucoma |
| Ziakas et al. [71] | 2009 | Randomized Clinical Trial | Greece | 15 | 30 | 72.6 (5.7) | 16 (53.3) | Cataract only |
| First Author | Year | 1. Was the Allocation Sequence Adequately Generated? | 2. Was the Allocation Adequately Concealed? | 3a. Were Patients Blinded? | 3b. Were Healthcare Providers Blinded? | 3c. Were Data Collectors Blinded? | 3d. Were Outcome Assessors Blinded? | 3e. Were Data Analysts Blinded? | 4. Was Loss to Follow-Up (Missing Outcome Data) Infrequent? | 5. Are Reports of the Study Free of Selective Outcome Reporting? | 6. Was the Study Apparently Free of Other Problems That Could Put It at a Risk of Bias? |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Akbari et al. [15] | 2021 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Akmaz et al. [16] | 2023 | Definitely yes (low risk of bias) | Probably no | Probably no | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Arshinoff et al. [17] | 2002 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Asano et al. [18] | 2008 | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Auffarth et al. [19] | 2017 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Balsak et al. [20] | 2018 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Borazan et al. [21] | 2007 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Probably yes |
| Camesaca et al. [22] | 2007 | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably yes | Definitely yes (low risk of bias) | Probably yes |
| Cekic et al. [23] | 1999 | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Probably yes | Probably yes |
| Cekic et al. [24] | 1999 | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Probably yes | Definitely yes (low risk of bias) | Probably yes |
| Chang et al. [25] | 2017 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) |
| Dieleman et al. [26] | 2011 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Dieleman et al. [27] | 2012 | Probably no | Probably no | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) |
| el-Harazi et al. [28] | 1998 | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Fernandez-Barrientos et al. [29] | 2010 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Gungor et al. [30] | 2014 | Probably no | Probably no | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Haripriya et al. [31] | 2019 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Holzer et al. [32] | 2001 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Holzer et al. [33] | 2002 | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Honda et al. [34] | 2004 | Probably no | Probably no | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Karalezli et al. [35] | 2008 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Probably yes | Probably yes |
| Karalezli et al. [36] | 2010 | Definitely yes (low risk of bias) | Probably no | Probably no | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Kim et al. [37] | 1996 | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Probably yes | Probably yes |
| Kohnen et al. [38] | 1996 | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably yes | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Kozera et al. [39] | 2020 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably no | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Levkovitch-Verbin et al. [40] | 2008 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Li et al. [41] | 2008 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Mahajan et al. [42] | 2021 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably no | Probably no | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Malecaze et al. [43] | 2000 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Mastropasqua et al. [44] | 1998 | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Paganelli et al. [45] | 2004 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Paganelli et al. [46] | 2009 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Probst et al. [47] | 1993 | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rabsilber et al. [48] | 2007 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably no | Probably no | Probably no | Probably no | Probably no | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rainer et al. [49] | 2000 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rainer et al. [50] | 2000 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rainer et al. [51] | 2001 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rainer et al. [52] | 2001 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rainer et al. [53] | 2001 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Rainer et al. [54] | 2003 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Saari et al. [55] | 2006 | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Sandoval et al. [56] | 2006 | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Schwenn et al. [57] | 2000 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Schwenn et al. [58] | 2001 | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Simaroj et al. [59] | 2011 | Probably no | Probably no | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Sipos et al. [60] | 2011 | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Solomon et al. [61] | 1998 | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) |
| Stifter et al. [62] | 2007 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Stifter et al. [63] | 2010 | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Studeny et al. [64] | 2014 | Definitely yes (low risk of bias) | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Waseem et al. [65] | 2007 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Wedrich et al. [66] | 1992 | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably no | Probably yes | Definitely yes (low risk of bias) | Probably yes |
| Wirtitsch et al. [67] | 2007 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) |
| Wu et al. [68] | 2018 | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Probably no | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Yaylali et al. [69] | 2004 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Probably yes |
| Zebardast et al. [70] | 2020 | Probably no | Probably no | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Definitely no (high risk of bias) | Probably yes | Definitely yes (low risk of bias) | Probably yes |
| Ziakas et al. [71] | 2009 | Probably no | Probably no | Probably no | Definitely no (high risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely yes (low risk of bias) | Definitely no (high risk of bias) | Definitely yes (low risk of bias) |
| Author | Year | Baseline IOP (mmHg), Mean (SD; Range), n Eyes | Post-op IOP (mmHg), Mean (SD); Min:25th: 50th:75th:Max Percentile | OVD Used (n Eyes) | Surgical Technique Performed | Method of IOP Measurement | Clear Corneal Thickness Measured (Yes/No) |
|---|---|---|---|---|---|---|---|
| Akbari et al. [15] | 2021 | 16.2 (2.9) n = 88 | 1-day: 22.5 (5.6) n = 88 3-days: 17.5 (2.2) n = 88 | - | 2.8 mm temporal incision and 5–6 mm capsulorrhexis | Goldmann Applanation Tonometry | No |
| Akmaz et al. [16] | 2023 | 13.9 (1.5) n = 32 14.2 (2.1) n = 33 | 1-day: 18.1 (1.4) n = 32 15.4 (3.2) n = 33 7-days: 14.5 (1.4) n = 32 14.1 (2.8) n = 33 | 1.4% Sodium Hyaluronate (32); None (33) | 2.8 mm incision and 5.0–5.5 mm capsulorhexis | Goldmann Applanation Tonometry | Yes |
| Arshinoff et al. [17] | 2002 | 15.0 (2.4) n = 49 15.2 (2.3) n = 99 15.6 (2.4) n = 50 | 6 h: 17.6 (4.0) n = 49 18.1 (5.4) n = 99 18.2 (5.2) n = 50 1-day: 17.9 (4.7) n = 49 18.6 (5.3) n = 99 20.2 (6.2) n = 50 7-days: 14.4 (3.2) n = 49 14.3 (3.3) n = 99 14.1 (3.5) n = 50 | 1.0% Sodium Hyaluronate (49); 1.4% Sodium Hyaluronate (99); 2.3% Sodium Hyaluronate (50) | 2.8 mm incision | Goldmann Applanation Tonometry | Yes |
| Asano et al. [18] | 2008 | 13.9 (3.0) n = 142 | 1-day: 14.3 (4.1) n = 142 11.6 (3.2) n = 142 | - | Small-incision | - | No |
| Auffarth et al. [19] | 2017 | 15.3 (2.4) n = 111 15.2 (2.7) n = 109 | 6 h: 20.2 (6.6) n = 111 19.0 (6.7) n = 109 1-day: 16.0 (4.6) n = 111 15.2 (4.6) n = 109 7-days: 14.3 (2.8) n = 111 14.6 (4.4) n = 109 | 4.0% Chondroitin sulphate- 1.65% sodium hyaluronate (111); 2.2% Sodium hyaluronate—1.0% Sodium hyaluronate (109) | Self-sealing clear corneal incisions | Goldmann Applanation Tonometry | Yes |
| Balsak et al. [20] | 2018 | 13.9 (3.2) n = 277 | 6 h: 24.0 (7.4) n = 277 1-day: 15.7 (5.0) n = 277 3-days:13.7 (4.0) n = 277 | 1.8% Sodium hyaluronate (277) | 2.75 mm clear corneal incision | Non-Contact Tonomtery | No |
| Borazan et al. [21] | 2007 | 14.7 (2.3) n = 185 | 6 h: 19.1 (5.4) n = 185 1-day: 13.9 (3.9) n = 185 7-days: 14.3 (1.6) n = 185 | 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (185) | 3.2 mm clear corneal temporal incision, 5.0 mm capsulorhexis | Goldmann Applanation Tonometry | No |
| Camesaca et al. [22] | 2007 | 15.6 (2.7) n = 286 | 1-day: 15.3 (4.5) n = 286 14.6 (5.2) n = 286 | Sodium hyaluronate 3.0%, 1.0% sodium hyaluronate, 4.0% chondroitin sulfate-3.0% sodium hyaluronate, 1.4% sodium hyaluronate, 2.3% sodium hyaluronate, or 1.8% sodium hyaluronate (286) | Temporal incision | Goldmann Applanation Tonometry | No |
| Cekic et al. [23] | 1999 | 15.8 (3.0) n = 51 | 8 h: 15.7 (6.1) n = 51 1-day: 15.0 (4.8) n = 51 7-days: 14.4 (3.9) n = 51 | Sodium hyaluronate (51) | A clear corneal, curvilinear two-plane two-level incision | Goldmann Applanation Tonometry | No |
| Cekic et al. [24] | 1999 | 15.1 (3.0) n = 58 | 1-day: 11.2 (2.4) n = 58 7-days: 11.5 (2.4) n = 58 | Chondroitin sulfate-sodium hyaluronate (58) | A clear corneal, curvilinear two-plane two-level incision, with either a 4.0 mm or 6.0 mm capsulorhexis | Goldmann Applanation Tonometry | No |
| Chang et al. [25] | 2017 | 15.5 (14–19) n = 43 | 1-day: 18.8 (14–24) n = 43 21-days: 15.0 (13–17) n = 43 | 1.5% Sodium hyaluronate (43) | 2.2 mm clear corneal incision with either Standard or Low fluid settings | Goldmann Applanation Tonometry | Yes |
| Dieleman et al. [26] | 2011 | 16.1 (3.2) n = 400 | 1-day: 15.5 (4.6) n = 400 30-days: 14.0 (2.9) n = 400 | 2.0% Hydroxypropyl methylcellulose (400) | 2.8 mm corneal or corneoscleral incision | Goldmann Applanation Tonometry | No |
| Dieleman et al. [27] | 2012 | 16.0 (3.2) n = 400 | 1-day: 15.5 (4.6) n = 400 30-days: 14.0 (2.9) n = 400 | - | - | Goldmann Applanation Tonometry | No |
| el-Harazi et al. [28] | 1998 | 17.2 (1.7) n = 58 | 1-day: 12.4 (2.6) n = 58 7-days: 15.3 (2.3) n = 58 | - | 5 mm incision | Goldmann Applanation Tonometry | No |
| Fernandez-Barrientos et al. [29] | 2010 | 23.6 (1.5) n = 16 | 1-day: 26.4 (8.1) n = 16 14-days: 18.2 (4.2) n = 16 | 1.0% Sodium hyaluronate (16) | 2.8-mm temporal corneal incision | Goldmann Applanation Tonometry | No |
| Gungor et al. [30] | 2014 | 14.9 (10–17) n = 60 | 1-day: 17.7 (12–24) n = 60 7-days: 14.3 (11–18) n = 60 | 4.0% Chondroitin sulphate-3.0% sodium hyaluronate and Sodium hyaluronate 1.0% (60) | 2.8 mm clear corneal incision and 5.0 mm capsulorhexis | Goldmann Applanation Tonometry | Yes |
| Haripriya et al. [31] | 2019 | 14.3 (3.2) n = 1406 | 1-day: 13.6 (4.8) n = 1406 30-days: 13.6 (3.4) n = 1406 | - | 2.8 mm clear corneal temporal incision and 5 to 5.5 mm capsulorhexis | Goldmann Applanation Tonometry | No |
| Holzer et al. [32] | 2001 | 16.0 (3.3) n = 19 16.6 (3.1) n = 30 14.5 (2.7) n = 12 15.4 (3.0) n = 20 | 6 h: 21.6 (4.5) n = 19 21.8 (7.1) n = 30 24.9 (7.1) n = 12 23.6 (7.5) n = 20 1-day: 17.1 (7.8) n = 19 19.3 (3.8) n = 30 15.7 (4.1) n = 12 17.1 (7.8) n = 20 7-days: 13.3 (2.6) n = 19 13.4 (3.4) n = 30 13.5 (2.6) n = 12 15.5 (3.5) n = 20 | 1.4% Sodium hyaluronate (19); 2.0% Hydroxypropyl methylcellulose (30); 2.3% Sodium hyaluronate (12); 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (20) | 2.5 mm corneoscleral superior incision | Goldmann Applanation Tonometry | No |
| Holzer et al. [33] | 2002 | 15.6 (3.3) n = 60 | 1-day: 14.5 (5.4) n = 60 3-days: 13.1 (3.7) n = 60 | - | Clear corneal temporal incision | - | No |
| Honda et al. [34] | 2004 | 13.8 (2.7) n = 44 | 1-day: 16.5 (5.5) n = 44 13.2 (3.7) n = 44 | - | Corneoscleral incision and continuous curvilinear capsulorhexis | - | No |
| Karalezli et al. [35] | 2008 | 14.8 (2.4) n = 60 | 1-day: 15.6 (2.4) n = 60 7-days: 14.3 (1.4) n = 60 | 4.0% Chondroitin sulphate-3.0% sodium hyaluronate and 1.2% sodium hyaluronate (60) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Karalezli et al. [36] | 2010 | 14.0 (2.0) n = 120 | 6 h: 17.9 (3.0) n = 120 1-day: 16.3 (2.7) n = 120 7-days: 14.0 (1.9) n = 120 | 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (120) | 3.2 mm clear corneal temporal incision and 5.0 mm capsulorhexis | Goldmann Applanation Tonometry | No |
| Kim et al. [37] | 1996 | 14.5 (2.6) n = 24 | 1-day: 14.4 (3.4) n = 24 3-days: 14.0 (2.5) n = 24 | 1.4% Sodium hyaluronate (24) | Traditional Phacoemulsification | Pneumo-tonometry | No |
| Kohnen et al. [38] | 1996 | 14.8 (2.3) n = 30 14.2 (2.2) n = 30 | 6 h: 16.8 (3.3) n = 30 16.2 (5.4) n = 30 1-day: 17.7 (3.7) n = 30 17.5 (6.8) n = 30 1.5-days: 15.6 (3.0) n = 30 14.3 (2.3) n = 30 2-days: 15.5 (3.4) n = 30 14.3 (2.5) n = 30 30-days: 14.6 (2.6) n = 30 14.1 (2.8) n = 30 | 1.0% sodium hyaluronate (30); 1.4% sodium hyaluronate (30) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Kozera et al. [39] | 2020 | 21.9 (2.3) n = 36 | 1-day: 17.8 (4.3) n = 36 7-days: 16.8 (3.6) n = 36 | - | Traditional Phacoemulsification | Goldmann Applanation Tonometry | Yes |
| Levkovitch-Verbin et al. [40] | 2008 | 15.7 (1.4) n = 122 | 4 h: 18.0 (4.3) n = 122 8 h: 17.0 (2.7) n = 122 1-day: 15.0 (2.1) n = 122 7-days: 13.9 (1.3) n = 122 | 1.2% Sodium hyaluronate (122) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Li et al. [41] | 2008 | 16.7 (1.4) n = 70 16.5 (1.4) n = 70 | 1-day: 18.8 (1.0) n = 70 19.4 (1.2) n = 70 7-days: 12.4 (0.7) n = 70 13.0 (1.0) n = 70 | 0.1% chitosan (70); 1.4% Sodium hyaluronate (70) | - | Goldmann Applanation Tonometry | Yes |
| Mahajan et al. [42] | 2021 | 15.9 (2.6) n = 150 | 1-day: 17.3 (5.8) n = 150 7-days: 15.8 (4.2) n = 150 | - | - | Non-Contact Tonometry | No |
| Malecaze et al. [43] | 2000 | 14.9 (1.0) n = 50 | 1-day: 14.9 (1.2) n = 50 7-days: 14.7 (1.1) n = 50 | 1.4% Sodium hyaluronate (50) | 3.2 mm clear corneal incision | Goldmann Applanation Tonometry | No |
| Mastropasqua et al. [44] | 1998 | 16.0 (2.0) n = 100 | 6 h: 19.9 (4.5) n = 100 1-day: 19.2 (4.7) n = 100 7-days: 16.4 (2.4) n = 100 | 1.4% Sodium hyaluronate (100) | 3.2 mm clear corneal superior incision and 5 mm capsulorhexis | Goldmann Applanation Tonometry | No |
| Paganelli et al. [45] | 2004 | 14.2 (10–19) n = 100 | 1-day: 17.3 (12–24) n = 100 3-days: 15.4 (10–22) n = 100 | - | 2.75-mm clear corneal incision | Goldmann Applanation Tonometry | No |
| Paganelli et al. [46] | 2009 | 14.0 (3.1) n = 135 | 1-day: 14.0 (3.9) n = 135 3-days: 13.2 (3.0) n = 132 | - | 2.75 mm clear corneal incision | Goldmann Applanation Tonometry | No |
| Probst et al. [47] | 1993 | 14.7 (2.0) n = 25 17.1 (0.6) n = 25 | 1-day: 20.9 (2.0) n = 25 18.6 (2.0) n = 25 7-days: 15.4 (0.9) n = 25 13.4 (0.8) n = 25 | 1.6% Sodium hyaluronate (25); 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (25) | Superior limbal incision | - | Yes |
| Rabsilber et al. [48] | 2007 | 14.8 (2.8) n = 34 | 1-day: 11.5 (2.7) n = 34 30-days: 11.9 (2.7) n = 34 | 1.4% Sodium hyaluronate (34) | Sealed capsule irrigation or Traditional | - | Yes |
| Rainer et al. [49] | 2000 | 14.8 (2.4) n = 50 | 6 h: 16.8 (4.1) n = 50 1-day: 14.4 (4.2) n = 50 7-days: 13.7 (2.2) n = 50 | 1.0% Sodium hyaluronate (50) | 6.0 mm superior sutureless frown incision | Goldmann Applanation Tonometry | No |
| Rainer et al. [50] | 2000 | 14.9 (2.5) n = 35 15.2 (2.9) n = 35 | 6 h: 20.1 (6.2) n = 35 25.2 (9.0) n = 35 1-day: 15.3 (3.9) n = 35 15.0 (3.4) n = 35 7-days: 13.5 (2.3) n = 35 13.5 (2.5) n = 35 | 2.3% Sodium hyaluronate (35); 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (35) | 3.5 mm temporal incision | Goldmann Applanation Tonometry | No |
| Rainer et al. [51] | 2001 | 14.3 (2.6) n = 80 | 6 h: 20.6 (7.7) n = 80 1-day: 14.4 (3.8) n = 80 7-days: 13.7 (2.8) n = 80 | 1.0% Sodium hyaluronate (80) | 3.2 mm temporal incision | Goldmann Applanation Tonometry | No |
| Rainer et al. [52] | 2001 | 13.9 (3.0) n = 60 | 6 h: 15.3 (4.4) n = 60 1-day: 12.8 (4.0) n = 60 7-days: 13.1 (3.0) n = 60 | 1.0% Sodium hyaluronate (60) | 3.5 mm temporal incision | Goldmann Applanation Tonometry | No |
| Rainer et al. [53] | 2001 | 14.0 (2.8) n = 40 14.1 (2.8) n = 40 | 6 h: 19.0 (5.8) n = 40 18.8 (6.0) n = 40 1-day: 15.9 (3.9) n = 40 15.7 (4.7) n = 40 7-days: 13.8 (3.0) n = 40 13.6 (2.6) n = 40 | 2.0% Hydroxypropyl methylcellulose (40); 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (40) | 3.5 mm temporal incision | Goldmann Applanation Tonometry | No |
| Rainer et al. [54] | 2003 | 15.4 (2.5) n = 76 | 6 h: 21.8 (6.5) n = 76 1-day: 14.8 (4.2) n = 76 7-days: 14.5 (3.2) n = 76 | 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (76) | 3.5 mm temporal incision | Goldmann Applanation Tonometry | No |
| Saari et al. [55] | 2006 | 17.9 (3.0) n = 20 | 1-day: 15.7 (5.5) n = 20 3-days: 14.6 (4.5) n = 20 | 1.0% Sodium hyaluronate (20) | 3.5 mm sclerotunnel superior incision and 5.0 mm capsulorhexis | Goldmann Applanation Tonometry | No |
| Sandoval et al. [56] | 2006 | 15.1 (3.5) n = 40 | 1-day: 16.6 (5.2) n = 40 3-days: 12.7 (1.9) n = 40 | - | Traditional Phacoemulsification | - | No |
| Schwenn et al. [57] | 2000 | 13.5 (2.0) n = 20 14.6 (3.0) n = 28 | 4 h: 18.1 (6.7) n = 20 27.5 (10.1) n = 28 6 h: 16.4 (5.1) n = 20 23.1 (8.5) n = 28 1-day: 12.3 (3.0) n = 20 14.5 (5.5) n = 28 2-days: 9.6 (2.2) n = 20 12.3 (3.5) n = 28 3-days: 9.8 (2.2) n = 20 12.2 (3.8) n = 28 | 2.3% Sodium hyaluronate (20); 4.0% Chondroitin sulphate-3.0% sodium hyaluronate (28) | 3.2 mm inverse curved superior incision | - | Yes |
| Schwenn et al. [58] | 2001 | 14.4 (2.6) n = 100 | 6 h: 20.9 (7.6) n = 100 1-day: 15.7 (4.9) n = 100 2-days: 13.5 (3.1) n = 100 3-days: 13.4 (3.0) n = 100 | 2.0% Hydroxypropyl methylcellulose (100) | Temporal incision being either clear corneal or sclerocorneal incision | Goldmann Applanation Tonometry | No |
| Simaroj et al. [59] | 2011 | 13.9 (2.2) n = 60 | 1-day: 13.1 (2.4) n = 60 7-days: 12.6 (2.0) n = 60 | - | 3-mm clear corneal incision | Goldmann Applanation Tonometry | No |
| Sipos et al. [60] | 2011 | 16.4 (2.4) n = 60 | 1-day: 17.0 (1.6) n = 60 7-days: 15.2 (1.6) n = 60 | - | - | - | No |
| Solomon et al. [61] | 1998 | 15.3 (2.6) n = 41 | 6 h: 18.1 (7.1) n = 41 1-day: 16.3 (3.9) n = 41 7-days: 13.9 (2.6) n = 41 | 1.4% Sodium hyaluronate (41) | Clear corneal incision | Goldmann Applanation Tonometry | Yes |
| Stifter et al. [62] | 2007 | 13.4 (2.5) n = 100 | 1 h: 19.0 (3.3) n = 100 2 h: 18.4 (2.8) n = 100 4 h:16.8 (2.4) n = 100 6 h: 15.8 (2.7) n = 100 8 h: 14.9 (2.8) n = 100 1-day: 14.2 (2.6) n = 100 7-days: 14.4 (2.1) n = 100 | 1.0% Sodium hyaluronate (100) | Combined Primary posterior continuous curvilinear capsulorhexis and posterior optic buttonholing or Conventional in-the-bag IOL implantation | Goldmann Applanation Tonometry | No |
| Stifter et al. [63] | 2010 | 13.8 (1.9) n = 60 | 1 h: 20.8 (6.7) n = 60 2 h: 19.4 (5.9) n = 60 4 h: 18.5 (5.2) n = 60 6 h: 17.6 (4.5) n = 60 8 h: 16.5 (3.1) n = 60 1-day: 15.5 (2.4) n = 60 7-days: 14.1 (2.2) n = 60 | 1.0% Sodium hyaluronate and 2.0% Hydroxypropyl methylcellulose (60) | Combined Primary posterior capsulorhexis and posterior optic buttonholing or Conventional in-the-bag IOL implantation | Goldmann Applanation Tonometry | No |
| Studeny et al. [64] | 2014 | 16.8 (3.9) n = 96 16.4 (3.9) n = 96 | 2 h: 10.2 (6.8) n = 96 9.9 (7.0) n = 96 1-day: 14.5 (5.6) n = 96 15.5 (5.8) n = 96 30-days: 13.2 (3.5) n = 96 13.1 (3.4) n = 96 | 2.0% Hydroxypropyl methylcellulose (96); 1.0% Sodium hyaluronate and 2.0% Hydroxypropyl methylcellulose (96) | Either hydroimplantation of IOL or OVD use in IOL implantation | Non-Contact Tonometry | No |
| Waseem et al. [65] | 2007 | 14.3 (2) n = 46 14.1 (1.9) n = 45 | 1-day: 18.8 (2.9) n = 46 16.9 (2.6) n = 45 7-days: 14.7 (1.6) n = 46 14.4 (1.7) n = 45 | 1.0% Sodium hyaluronate (46); 2.0% Hydroxypropyl methylcellulose (45) | 3.2 mm temporal limbal incision | Goldmann Applanation Tonometry | No |
| Wedrich et al. [66] | 1992 | 14.2 (3.2) n = 90 | 6 h: 15.1 (8.2) n = 90 18 h: 14.3 (6.5) n = 90 7-days: 13.8 (2.5) n = 90 | 1.0% Sodium hyaluronate (90) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Wirtitsch et al. [67] | 2007 | 16.6 (2.6) n = 88 | 6 h: 18.7 (5.4) n = 88 1-day: 15.2 (3.5) n = 88 7-days: 16.0 (2.9) n = 88 | 1.0% Sodium hyaluronate (88) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Wu et al. [68] | 2018 | 14.5 (2.6) n = 99 | 1-day: 15.2 (5.0) n = 99 7-days: 14.6 (3.3) n = 99 | 1.0% Sodium hyaluronate (99) | Standard 3.0 mm small incision phacoemulsification or Coaxial 2.2 mm micro-incision Fusion Phaco complex phacoemulsification | Non-Contact Tonometry | Yes |
| Yaylali et al. [69] | 2004 | 13.3 (2.5) n = 48 | 1-day: 14.7 (5.6) n = 48 3-days: 11.3 (1.7) n = 48 | 4.0% Chondroitin sulphate-3.0% sodium hyaluronate and 1.2% Sodium hyaluronate (48) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Zebardast et al. [70] | 2020 | 25.4 (2.9) n = 187 | 1-day: 27.6 (10.2) n = 187 7-days: 20.8 (6.3) n = 187 | - | Traditional Phacoemulsification | Goldmann Applanation Tonometry | Yes |
| Ziakas et al. [71] | 2009 | 14.5 (3.0) n = 30 | 1-day: 12.7 (4.5) n = 30 7-days: 13.2 (2.3) n = 30 | Sodium hyaluronate (30) | Traditional Phacoemulsification | Goldmann Applanation Tonometry | No |
| Author | Year | Pre-Operative Medications (n Eyes) | Intra-Operative Medications (n Eyes) | Post-Operative Medications (n Eyes) |
|---|---|---|---|---|
| Akbari et al. [15] | 2021 | None | None | Chloramphenicol 5%, betamethasone 0.1%, and ketorolac tomethamine 0.5%(46) Or Chloramphenicol 5%, and betamethasone 0.1% (42) |
| Akmaz et al. [16] | 2023 | None | 0.1 cc moxifloxacin (65) | None |
| Arshinoff et al. [17] | 2002 | Ofloxacin 0.3%, and diclofenac 0.1% eyedrops (198) | None | Tobramycin and dexamethasone eyedrops (198) |
| Asano et al. [18] | 2008 | Diclofenac sodium 0.1% (71) or Betamethasone sodium 0.1% (71) | None | Diclofenac sodium 0.1% (71) Or Betamethasone sodium 0.1% (71) |
| Auffarth et al. [19] | 2017 | - | - | - |
| Balsak et al. [20] | 2018 | None | Cefurozime axetil 0.1% (277) | Brimonidine-timolol, tobramycin and dexamethasone (231) Or Tobramycin and dexamethasone (46) |
| Borazan et al. [21] | 2007 | Diclofenac (185) | None (153) or Carbachol (32) | Acetazolamide 250 mg, ofloxacin 0.3% and prednisolone acetate 1% eyedrops (185) With either Topical brinzolamide 1% (30), Brimonidine 0.2% (32), Oral acetazolamide 250 mg (30), Timolol maleate 0.5% (30), Or nothing else (63) |
| Camesaca et al. [22] | 2007 | Fluoroquinolone (286) | None | Chloramphenicol 0.25% and betamethasone 0.13% gel (143) Or Tobramycin 0.3% and dexamethasone 0.1% (143) |
| Cekic et al. [23] | 1999 | None | None | 0.5 mL balanced salt solution (24) Or 0.5 mL carbachol 0.01% (27) |
| Cekic et al. [24] | 1999 | None | Carbachol (58) | 20 mg gentamicin and 2 mg betamethasone (58) |
| Chang et al. [25] | 2017 | None | 0.2 mg moxifloxacin (43) | Dexamethasone (43) |
| Dieleman et al. [26] | 2011 | None | None | Betamethasone acetate 5.7 mg/mL (200) Or Dexamethasone 0.1% (200) |
| Dieleman et al. [27] | 2012 | None | None | Physostigmine, and dexamethasone (199) Or Dexamethasone (201) |
| el-Harazi et al. [28] | 1998 | None | None | Diclofenac sodium 0.1% (19) Or Ketorolac tromethamine 0.5% (19) Or Prednisolone acetate 1% (20) |
| Fernandez-Barrientos et al. [29] | 2010 | 1 mg/mL tetracaine chloride and 4mg/mL oxybuprocainechloride (16) | None | None |
| Gungor et al. [30] | 2014 | None | None | Triamcinolone acetonide 2 mg/0.05 mL (30) Or Dexamethasone (0.4 mg/0.1 mL (30) |
| Haripriya et al. [31] | 2019 | Topical ofloxacin 0.3% (1406) | None | Topical ofloxacin 0.3% and prednisolone acetate 1% (1406) |
| Holzer et al. [32] | 2001 | - | - | - |
| Holzer et al. [33] | 2002 | Ofloxacin 0.3% (60) | Epinephrine and carbachol (60) | Loteprednol etabonate 0.5% and ofloxacin 0.3% (30) Or Ketorolac tromethamine 0.5% and ofloxacin 0.3% (30) |
| Honda et al. [34] | 2004 | - | - | Topical mixture of unspecified antibiotics and steroids (44) |
| Karalezli et al. [35] | 2008 | None | None (30) Or 1 mg intracameral triamcinolone acetonide (30) | Topical prednisolone acetate 1% and topical ofloxacin 0.3% (30) Or Topical ofloxacin 0.3% (30) |
| Karalezli et al. [36] | 2010 | None | None | None (60) Or 1mg triamcinolone acetonide (60) |
| Kim et al. [37] | 1996 | Tobramycin (24) | None | Topical 0.1% fluorometholone (24) |
| Kohnen et al. [38] | 1996 | Unspecified antibiotics eye drops and oral 250 mg acetazolamide (60) | None | Dexamethasone, polymyxin, neomycin, and unspecified steroid/antibiotic drops (60) |
| Kozera et al. [39] | 2020 | None | None | Loteprednol and Moxifloksacinum (36) |
| Levkovitch-Verbin et al. [40] | 2008 | Unspecified anti-glaucoma medications (33) Or None (89) | None | Dexamethasone 0.1% eye drops and chloramphenicol ointment (122) With either Timolol maleate (60), unspecified anti-glaucoma medications (33), and/or nothing else (44) |
| Li et al. [41] | 2008 | - | - | - |
| Mahajan et al. [42] | 2021 | - | - | Topical difluprednate 0.05% (50) Or Topical dexamethasone 0.1% (50) Or Topical prednisolone 1% (50) |
| Malecaze et al. [43] | 2000 | None | None | Gentamicin eye drops (50) |
| Mastropasqua et al. [44] | 1998 | - | None | - |
| Paganelli et al. [45] | 2004 | None | None (50) Or 40-mg triamcinolone acetonide (50) | Prednisolone acetate 1% (50) Or None |
| Paganelli et al. [46] | 2009 | None | None (67) Or 25 mg triamcinolone and 2 mg ciprofloxacin (68) | Prednisolone acetate 1% and ciprofloxacin hydrochloride 0.3% (67) Or None (68) |
| Probst et al. [47] | 1993 | None | None | None (42) Or Topical Beta blocker (8) |
| Rabsilber et al. [48] | 2007 | None | None | None |
| Rainer et al. [49] | 2000 | Diclofenac (50) | None | Betamethasone-neomycin ointment, diclofenac and prednisolone acetate (50) With either Apraclonidine 0.5% (25) Or dorzolamide 2% (25) |
| Rainer et al. [50] | 2000 | Diclofenac (70) | None | Gentamicin-prednisolone ointment, and diclofenac and prednisolone acetate 0.5% eyedrops (70) |
| Rainer et al. [51] | 2001 | Diclofenac (80) | None | Prednisolone acetate 0.5% ointment and diclofenac and prednisolone acetate 0.5% eyedrops (80) With either brimonidine 0.2% eye drops (40) Or prednisolone acetate 0.5% ointment (40) |
| Rainer et al. [52] | 2001 | Diclofenac eye drops (80) | None | Prednisolone ointment and diclofenac and prednisolone acetate 0.5% eyedrops (80) |
| Rainer et al. [53] | 2001 | Diclofenac eyedrops (60) | None | Acetate 0.5% ointment, and diclofenac and prednisolone acetate 0.5% eyedrops (60) With either Prednisolone fixed dorzolamide–timolol combination eye drops (30), Or latanoprost eye drops (30) |
| Rainer et al. [54] | 2003 | None | None | None (38) Or Fixed dorzolamide–timolol combination (38) |
| Saari et al. [55] | 2006 | 250 mg Oral acetazolamide (20) | None | 0.7% or 0.1% dexamethasone with chloramphenicol eye drops, and dexamethasone alcohol and neomycin sulphate ointment (20) |
| Sandoval et al. [56] | 2006 | Ketorolac 0.4% or 0.5%, eye drops (40) | None | Ketorolac 0.4% or 0.5% and ofloxacin 0.3% (40) |
| Schwenn et al. [57] | 2000 | Topical diclofenac (48) | None | Prednisolone acetate eye drops and ointment, and gentamicin eye drops (48) |
| Schwenn et al. [58] | 2001 | None | None | Prednisolone acetate eyedrops, gentamicin sulfate, and 5 mg/g prednisolone pivalate ointment (100) |
| Simaroj et al. [59] | 2011 | None | None (30) Or Intracameral triamcinolone acetonide and gentamicin (30) | Topical 0.1% dexamethasone-0.3% tobramycin combination (30) Or Topical tobramycin (30) |
| Sipos et al. [60] | 2011 | Diclofenac eye drops (60) | None | Diclofenac sodium and gentamicin eyedrops (60) With either Low-viscosity tear replacement eye drops (11), high-viscosity tear replacement eye drops (9), 0.3 mg dexamethasone and 3 mg gentamicin sulfate ointment (10), or nothing else (30) |
| Solomon et al. [61] | 1998 | None | None (20) Or Intracameral carbachol 0.01% (21) | Unspecified topical antibiotic-corticosteroid combination (41) |
| Stifter et al. [62] | 2007 | None | None | Dexamethasone-gentamicin ointment, diclofenac sodium and prednisolone acetate 0.5% eyedrops (100) With either Dorzolamide hydrochloride 2.0%–timolol maleate 0.5% eye drops (50) Or Nothing else (50) |
| Stifter et al. [63] | 2010 | Diclofenac eye drops (60) | None | None |
| Studeny et al. [64] | 2014 | None | None | None |
| Waseem et al. [65] | 2007 | None | None | Norfloxacin 0.3%, dexamethasone eye 0.1% drops, and Fusidic acid eye ointment (91) |
| Wedrich et al. [66] | 1992 | None | None (30) Or Intracameral carbachol (30) Or Intracameral acetylcholine 1% | Topical steroids and indomethacin (90) |
| Wirtitsch et al. [67] | 2007 | None | Fixed dorzolamide–timolol combination eye drop (88) | Prednisolone acetate 1% and diclofenac eye drops (88) |
| Wu et al. [68] | 2018 | None | None | Levofloxacin and prednisolone eye drops (99) |
| Yaylali et al. [69] | 2004 | None | None | Ofloxacin 0.3% (48) With either prednisolone acetate 1% eyedrops (21) Or topical rimexolone 1% (27) |
| Zebardast et al. [70] | 2020 | None | None | Unspecified topical antibiotics and corticosteroids (187) |
| Ziakas et al. [71] | 2009 | None | None (15) Or Trypan Blue (15) | 1 tablet of acetazolamide 250 mg, and dexamethasone 1mg/mL and chloramphenicol 5 mg/mL eye drops (30) |
References
- Liu, Y.C.; Wilkins, M.; Kim, T.; Malyugin, B.; Mehta, J.S. Cataracts. Lancet 2017, 390, 600–612. [Google Scholar] [CrossRef] [PubMed]
- Canadian National Institute for the Blind (CNIB). Blindness in Canada. 2023. Available online: https://www.cnib.ca/en/sight-loss-info/blindness/blindness-canada?region=on (accessed on 21 August 2024).
- Hatch, W.V.; Campbell, E.D.L.; Bell, C.M.; El-Defrawy, S.R.; Campbell, R.J. Projecting the growth of cataract surgery during the next 25 years. Arch. Ophthalmol. 2012, 130, 1479–1481. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Andreev, K.; Dupre, M.E. Major Trends in Population Growth Around the World. China CDC Wkly. 2021, 3, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Wang, W.; Yan, W.; Fotis, K.; Prasad, N.M.; Lansingh, V.C.; Taylor, H.R.; Finger, R.P.; Facciolo, D.; He, M. Cataract Surgical Rate and Socioeconomics: A Global Study. Investig. Ophthalmol. Vis. Sci. 2016, 57, 5872–5881. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Ophthalmology. Cataract in the Adult Eye PPP. 2021. Available online: https://www.aao.org/education/preferred-practice-pattern/cataract-in-adult-eye-ppp-2021-in-press (accessed on 21 August 2024).
- Thompson, J.; Lakhani, N. Cataracts. Prim. Care Clin. Off. Pract. 2015, 42, 409–423. [Google Scholar] [CrossRef]
- Malvankar-Mehta, M.S.; Fu, A.; Subramanian, Y.; Hutnik, C. Impact of Ophthalmic Viscosurgical Devices in Cataract Surgery. J. Ophthalmol. 2020, 780, 1093. [Google Scholar] [CrossRef]
- Chan, E.; Mahroo, O.A.R.; Spalton, D.J. Complications of cataract surgery. Clin. Exp. Optom. 2010, 93, 379–389. [Google Scholar] [CrossRef]
- Ahmed, I.I.; Kranenmann, C.; Chipman, M.; Malam, F. Revisiting early postoperative follow-up after phacoemulsification. J. Cataract. Refract. Surg. 2002, 28, 100–108. [Google Scholar] [CrossRef]
- Todorović, M.; Šarenac Vulović, T.; Petrović, N.; Todorović, D.; Srećković, S. Intraocular pressure changes after uneventful phacoemulsification in early postoperative period in healthy eyes. Acta Clin. Croat. 2019, 58, 467–472. [Google Scholar] [CrossRef]
- Grzybowski, A.; Kanclerz, P. Do we need day-1 postoperative follow-up after cataract surgery? Graefes Arch. Clin. Exp. Ophthalmol. 2019, 257, 855–861. [Google Scholar] [CrossRef]
- CLARITY Group at McMaster University. Tools to Assess Risk of Bias in Cohort and Case Control Studies; Randomized Controlled Trials; and Longitudinal Symptom Research Studies Aimed at the General Population. 2024. Available online: https://www.distillersr.com/resources/methodological-resources/tool-to-assess-risk-of-bias-in-randomized-controlled-trials-distillersr (accessed on 21 August 2024).
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Moghadam, R.S.; Mohamadpour, A. The Effect of Ketorolac Eye Drop on Inflammation and Anterior Segment Complications after Cataract Surgery in Pseudoexfoliation Syndrome; a Randomized Clinical Trial. Pak. J. Med. Health Sci. 2021, 15, 1098–1104. [Google Scholar]
- Akmaz, B.; Kilic, D.; Duru, N. The Safety and Efficacy of Phacoemulsification Surgery in Uncomplicated Cataracts with and without an Ophthalmic-Viscosurgical-Device. Eur. J. Ophthalmol. 2023, 33, 269–277. [Google Scholar] [CrossRef] [PubMed]
- Arshinoff, S.A.; Albiani, D.A.; Taylor-Laporte, J. Intraocular Pressure after Bilateral Cataract Surgery Using Healon, Healon5, and Healon GV. J. Cataract. Refract. Surg. 2002, 28, 617–625. [Google Scholar] [CrossRef]
- Asano, S.; Miyake, K.; Ota, I.; Sugita, G.; Kimura, W.; Sakka, Y.; Yabe, N. Reducing Angiographic Cystoid Macular Edema and Blood-Aqueous Barrier Disruption after Small-Incision Phacoemulsification and Foldable Intraocular Lens Implantation: Multicenter Prospective Randomized Comparison of Topical Diclofenac 0.1% and Betamethason. J. Cataract. Refract. Surg. 2008, 34, 57–63. [Google Scholar] [CrossRef]
- Auffarth, G.U.; Auerbach, F.N.; Rabsilber, T.; Gegundez, J.A.; Cuina, R.; Renard, Y.; Vinciguerra, P.; Camesasca, F.; Van Cauwenberge, F.; Amzallag, T.; et al. Comparison of the Performance and Safety of 2 Ophthalmic Viscosurgical Devices in Cataract Surgery. J. Cataract. Refract. Surg. 2017, 43, 87–94. [Google Scholar] [CrossRef]
- Balsak, S.; Kaydu, A.; Erdem, S.; Fuat Alakus, M.; Ozkurt, Z.G. Brimonidine-Timolol versus Brinzolamide-Timolol for Treatment of Elevated Intraocular Pressure after Phacoemulsification Surgery. Int. Ophthalmol. 2018, 38, 1583–1589. [Google Scholar] [CrossRef] [PubMed]
- Borazan, M.; Karalezli, A.; Akman, A.; Akova, Y.A. Effect of Antiglaucoma Agents on Postoperative Intraocular Pressure after Cataract Surgery with Viscoat. J. Cataract. Refract. Surg. 2007, 33, 1941–1945. [Google Scholar] [CrossRef]
- Camesasca, F.I.; Bianchi, C.; Beltrame, G.; Caporossi, A.; Piovella, M.; Rapisarda, A.; Tassinari, G.; Zeppa, L. Italian Betamethasone-Chloramphenicol vs. Dexamethasone-Tobramycin Combination Study Group Control of Inflammation and Prophylaxis of Endophthalmitis after Cataract Surgery: A Multicenter Study. Eur. J. Ophthalmol. 2007, 17, 733–742. [Google Scholar] [CrossRef]
- Cekic, O.; Batman, C. Effect of Capsulorhexis Size on Postoperative Intraocular Pressure. J. Cataract. Refract. Surg. 1999, 25, 416–419. [Google Scholar] [CrossRef]
- Cekic, O.; Batman, C. Effect of Intracameral Carbachol on Intraocular Pressure Following Clear Corneal Phacoemulsification. Eye 1999, 13 Pt 2, 209–211. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Fridberg, A.; Kugelberg, M. Comparison of Phacoemulsification Cataract Surgery with Low versus Standard Fluidic Settings and the Impact on Postoperative Parameters. Eur. J. Ophthalmol. 2017, 27, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Dieleman, M.; Wubbels, R.J.; van Kooten-Noordzij, M.; de Waard, P.W.T. Single Perioperative Subconjunctival Steroid Depot versus Postoperative Steroid Eyedrops to Prevent Intraocular Inflammation and Macular Edema after Cataract Surgery. J. Cataract. Refract. Surg. 2011, 37, 1589–1597. [Google Scholar] [CrossRef] [PubMed]
- Dieleman, M.; Wubbels, R.J.; De Waard, P.W.T. Miotics after Modern Cataract Surgery Are History. J. Ocul. Pharmacol. Ther. 2012, 28, 98–101. [Google Scholar] [CrossRef] [PubMed]
- el-Harazi, S.M.; Ruiz, R.S.; Feldman, R.M.; Villanueva, G.; Chuang, A.Z. A Randomized Double-Masked Trial Comparing Ketorolac Tromethamine 0.5%, Diclofenac Sodium 0.1%, and Prednisolone Acetate 1% in Reducing Post-Phacoemulsification Flare and Cells. Ophthalmic Surg. Lasers 1998, 29, 539–544. [Google Scholar] [CrossRef]
- Fernandez-Barrientos, Y.; Garcia-Feijoo, J.; Martinez-de-la-Casa, J.M.; Pablo, L.E.; Fernandez-Perez, C.; Garcia Sanchez, J. Fluorophotometric Study of the Effect of the Glaukos Trabecular Microbypass Stent on Aqueous Humor Dynamics. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3327–3332. [Google Scholar] [CrossRef]
- Gungor, S.G.; Bulam, B.; Akman, A.; Colak, M. Comparison of Intracameral Dexamethasone and Intracameral Triamcinolone Acetonide Injection at the End of Phacoemulsification Surgery. Indian J. Ophthalmol. 2014, 62, 861–864. [Google Scholar] [CrossRef]
- Haripriya, A.; Ramulu, P.Y.; Chandrashekharan, S.; Venkatesh, R.; Narendran, K.; Shekhar, M.; Ramakrishnan, R.; Ravindran, R.D.; Robin, A.L. The Aravind Pseudoexfoliation Study: Surgical and First-Year Postoperative Results in Eyes without Phacodonesis and Nonmiotic Pupils. Ophthalmology 2019, 126, 362–371. [Google Scholar] [CrossRef]
- Holzer, M.P.; Tetz, M.R.; Auffarth, G.U.; Welt, R.; Volcker, H.E. Effect of Healon5 and 4 Other Viscoelastic Substances on Intraocular Pressure and Endothelium after Cataract Surgery. J. Cataract. Refract. Surg. 2001, 27, 213–218. [Google Scholar] [CrossRef]
- Holzer, M.P.; Solomon, K.D.; Sandoval, H.P.; Vroman, D.T. Comparison of Ketorolac Tromethamine 0.5% and Loteprednol Etabonate 0.5% for Inflammation after Phacoemulsification: Prospective Randomized Double-Masked Study. J. Cataract. Refract. Surg. 2002, 28, 93–99. [Google Scholar] [CrossRef]
- Honda, S.; Matsuo, A.; Toda, H.; Saito, I. Effect of Eye Patching on Postoperative Inflammation after Cataract Surgery. J. Cataract. Refract. Surg. 2004, 30, 273–274. [Google Scholar] [CrossRef] [PubMed]
- Karalezli, A.; Borazan, M.; Akova, Y.A. Intracameral Triamcinolone Acetonide to Control Postoperative Inflammation Following Cataract Surgery with Phacoemulsification. Acta Ophthalmol. 2008, 86, 183–187. [Google Scholar] [CrossRef] [PubMed]
- Karalezli, A.; Borazan, M.; Kucukerdonmez, C.; Akman, A.; Akova, Y.A. Effect of Intracameral Triamcinolone Acetonide on Postoperative Intraocular Pressure after Cataract Surgery. Eye 2010, 24, 619–623. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W. Comparative Study of Intraocular Pressure Change after Cataract Surgery: Phacoemulsification and Extracapsular Cataract Extraction. Korean J. Ophthalmol. KJO 1996, 10, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Kohnen, T.; von Ehr, M.; Schutte, E.; Koch, D.D. Evaluation of Intraocular Pressure with Healon and Healon GV in Sutureless Cataract Surgery with Foldable Lens Implantation. J. Cataract. Refract. Surg. 1996, 22, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Kozera, M.; Konopinska, J.; Mariak, Z.; Rekas, M. Effectiveness of iStent Trabecular Micro-Bypass System Combined with Phacoemulsification vs. Phacoemulsification Alone in Patients with Glaucoma and Cataract Depending on the Initial Intraocular Pressure. Ophthalmic Res. 2020, 64, 327–336. [Google Scholar] [CrossRef]
- Levkovitch-Verbin, H.; Habot-Wilner, Z.; Burla, N.; Melamed, S.; Goldenfeld, M.; Bar-Sela, S.M.; Sachs, D. Intraocular Pressure Elevation within the First 24 Hours after Cataract Surgery in Patients with Glaucoma or Exfoliation Syndrome. Ophthalmology 2008, 115, 104–108. [Google Scholar] [CrossRef]
- Li, Y.; Cheng, J.-W.; Wei, R.-L.; Hou, C.-L.; Wang, W.-B.; Gu, Q.-S.; Cai, J.-P. Intraocular Pressure and Endothelium Cell Counts after Cataract Surgery with Chitosan and Sodium Hyaluronate (Healon GV): 3-Year Follow-up Results of a Randomised Clinical Trial. Adv. Ther. 2008, 25, 422–429. [Google Scholar] [CrossRef]
- Mahajan, S.; Kai, S.; Choudhary, S.; Bala, K.; Sahni, B. Evaluation of Intraocular Pressure Changes with Topical Dexamethasone 0.1%, Prednisolone 1% and Difluprednate 0.05% Postcataract Surgery-A Randomised Clinical Trial. J. Clin. Diagn. Res. 2021, 15, 15071. [Google Scholar] [CrossRef]
- Malecaze, F.A.; Deneuville, S.F.; Julia, B.J.; Daurin, J.G.; Chapotot, E.M.; Grandjean, H.M.; Arne, J.L.; Rascol, O. Pain Relief with Intracameral Mepivacaine during Phacoemulsification. Br. J. Ophthalmol. 2000, 84, 171–174. [Google Scholar] [CrossRef][Green Version]
- Mastropasqua, L.; Carpineto, P.; Ciancaglini, M.; Falconio, G. Intraocular Pressure Changes after Phacoemulsification and Foldable Silicone Lens Implantation Using Healon GV. Ophthalmologica 1998, 212, 318–321. [Google Scholar] [CrossRef]
- Paganelli, F.; Cardillo, J.A.; Melo, L.A.S.J.; Oliveira, A.G.; Skaf, M.; Costa, R.A. Brazilian Ocular Pharmacology and Pharmaceutical Technology Research Group A Single Intraoperative Sub-Tenon’s Capsule Triamcinolone Acetonide Injection for the Treatment of Post-Cataract Surgery Inflammation. Ophthalmology 2004, 111, 2102–2108. [Google Scholar] [CrossRef] [PubMed]
- Paganelli, F.; Cardillo, J.A.; Melo, L.A.S.J.; Lucena, D.R.; Silva, A.A.J.; Oliveira, A.G.; Hofling-Lima, A.L.; Nguyen, Q.D.; Kuppermann, B.D.; Belfort, R.J.; et al. A Single Intraoperative Sub-Tenon’s Capsule Injection of Triamcinolone and Ciprofloxacin in a Controlled-Release System for Cataract Surgery. Investig. Ophthalmol. Vis. Sci. 2009, 50, 3041–3047. [Google Scholar] [CrossRef] [PubMed]
- Probst, L.E.; Nichols, B.D. Corneal Endothelial and Intraocular Pressure Changes after Phacoemulsification with Amvisc Plus and Viscoat. J. Cataract. Refract. Surg. 1993, 19, 725–730. [Google Scholar] [CrossRef] [PubMed]
- Rabsilber, T.M.; Limberger, I.-J.; Reuland, A.J.; Holzer, M.P.; Auffarth, G.U. Long-Term Results of Sealed Capsule Irrigation Using Distilled Water to Prevent Posterior Capsule Opacification: A Prospective Clinical Randomised Trial. Br. J. Ophthalmol. 2007, 91, 912–915. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rainer, G.; Menapace, R.; Findl, O.; Georgopoulos, M.; Kiss, B.; Heinze, G. Randomised Fellow Eye Comparison of the Effectiveness of Dorzolamide and Apraclonidine on Intraocular Pressure Following Phacoemulsification Cataract Surgery. Eye 2000, 14, 757–760. [Google Scholar] [CrossRef][Green Version]
- Rainer, G.; Menapace, R.; Findl, O.; Georgopoulos, M.; Kiss, B.; Petternel, V. Intraocular Pressure after Small Incision Cataract Surgery with Healon5 and Viscoat. J. Cataract. Refract. Surg. 2000, 26, 271–276. [Google Scholar] [CrossRef]
- Rainer, G.; Menapace, R.; Findl, O.; Petternel, V.; Kiss, B.; Georgopoulos, M. Effect of Topical Brimonidine on Intraocular Pressure after Small Incision Cataract Surgery. J. Cataract. Refract. Surg. 2001, 27, 1227–1231. [Google Scholar] [CrossRef]
- Rainer, G.; Menapace, R.; Findl, O.; Petternel, V.; Kiss, B.; Georgopoulos, M. Intraindividual Comparison of the Effects of a Fixed Dorzolamide-Timolol Combination and Latanoprost on Intraocular Pressure after Small Incision Cataract Surgery. J. Cataract. Refract. Surg. 2001, 27, 706–710. [Google Scholar] [CrossRef]
- Rainer, G.; Menapace, R.; Findl, O.; Kiss, B.; Petternel, V.; Georgopoulos, M.; Schneider, B. Intraocular Pressure Rise after Small Incision Cataract Surgery: A Randomised Intraindividual Comparison of Two Dispersive Viscoelastic Agents. Br. J. Ophthalmol. 2001, 85, 139–142. [Google Scholar] [CrossRef]
- Rainer, G.; Menapace, R.; Findl, O.; Sacu, S.; Schmid, K.; Petternel, V.; Kiss, B.; Georgopoulos, M. Effect of a Fixed Dorzolamide-Timolol Combination on Intraocular Pressure after Small-Incision Cataract Surgery with Viscoat. J. Cataract. Refract. Surg. 2003, 29, 1748–1752. [Google Scholar] [CrossRef] [PubMed]
- Saari, K.M.; Nelimarkka, L.; Ahola, V.; Loftsson, T.; Stefansson, E. Comparison of Topical 0.7% Dexamethasone-Cyclodextrin with 0.1% Dexamethasone Sodium Phosphate for Postcataract Inflammation. Graefe’s Arch. Clin. Exp. Ophthalmol. = Albrecht Von Graefes Arch. Klin. Exp. Ophthalmol. 2006, 244, 620–626. [Google Scholar] [CrossRef]
- Sandoval, H.P.; De Castro, L.E.F.; Vroman, D.T.; Solomon, K.D. Evaluation of 0.4% Ketorolac Tromethamine Ophthalmic Solution versus 0.5% Ketorolac Tromethamine Ophthalmic Solution after Phacoemulsification and Intraocular Lens Implantation. J. Ocul. Pharmacol. Ther. 2006, 22, 251–257. [Google Scholar] [CrossRef]
- Schwenn, O.; Dick, H.B.; Krummenauer, F.; Christmann, S.; Vogel, A.; Pfeiffer, N. Healon5 versus Viscoat during Cataract Surgery: Intraocular Pressure, Laser Flare and Corneal Changes. Graefe’s Arch. Clin. Exp. Ophthalmol. = Albrecht Von Graefes Arch. Klin. Exp. Ophthalmol. 2000, 238, 861–867. [Google Scholar] [CrossRef] [PubMed]
- Schwenn, O.; Dick, H.B.; Krummenauer, F.; Krist, R.; Pfeiffer, N. Intraocular Pressure after Small Incision Cataract Surgery: Temporal Sclerocorneal versus Clear Corneal Incision. J. Cataract. Refract. Surg. 2001, 27, 421–425. [Google Scholar] [CrossRef] [PubMed]
- Simaroj, P.; Sinsawad, P.; Lekhanont, K. Effects of Intracameral Triamcinolone and Gentamicin Injections Following Cataract Surgery. J. Med. Assoc. Thail. = Chotmaihet Thangphaet 2011, 94, 819–825. [Google Scholar]
- Sipos, E.; Stifter, E.; Menapace, R. Patient Satisfaction and Postoperative Pain with Different Postoperative Therapy Regimens after Standardized Cataract Surgery: A Randomized Intraindividual Comparison. Int. Ophthalmol. 2011, 31, 453–460. [Google Scholar] [CrossRef]
- Solomon, K.D.; Stewart, W.C.; Hunt, H.H.; Stewart, J.A.; Cate, E.A. Intraoperative Intracameral Carbachol in Phacoemulsification and Posterior Chamber Lens Implantation. Am. J. Ophthalmol. 1998, 125, 36–43. [Google Scholar] [CrossRef]
- Stifter, E.; Luksch, A.; Menapace, R. Postoperative Course of Intraocular Pressure after Cataract Surgery with Combined Primary Posterior Capsulorhexis and Posterior Optic Buttonholing. J. Cataract. Refract. Surg. 2007, 33, 1585–1590. [Google Scholar] [CrossRef]
- Stifter, E.; Menapace, R.; Kriechbaum, K.; Luksch, A. Posterior Optic Buttonholing Prevents Intraocular Pressure Peaks after Cataract Surgery with Primary Posterior Capsulorhexis. Graefe’s Arch. Clin. Exp. Ophthalmol. = Albrecht Von Graefes Arch. Klin. Exp. Ophthalmol. 2010, 248, 1595–1600. [Google Scholar] [CrossRef]
- Studeny, P.; Hyndrak, M.; Kacerovsky, M.; Mojzis, P.; Sivekova, D.; Kuchynka, P. Safety of Hydroimplantation: A Foldable Intraocular Lens Implantation without the Use of an Ophthalmic Viscosurgical Device. Eur. J. Ophthalmol. 2014, 24, 850–856. [Google Scholar] [CrossRef]
- Waseem, M.; Rustam, N. Qamar ul Islam Intraocular Pressure after Phacoemulsification Using Hydroxypropyl Methylcellulose and Sodium Hyaluronate as Viscoelastics. J. Ayub Med. Coll. Abbottabad JAMC 2007, 19, 42–45. [Google Scholar] [PubMed]
- Wedrich, A.; Menapace, R. Intraocular Pressure Following Small-Incision Cataract Surgery and polyHEMA Posterior Chamber Lens Implantation. A Comparison between Acetylcholine and Carbachol. J. Cataract. Refract. Surg. 1992, 18, 500–505. [Google Scholar] [CrossRef] [PubMed]
- Wirtitsch, M.G.; Menapace, R.; Georgopoulos, M.; Rainer, G.; Buehl, W.; Heinzl, H. Intraocular Pressure Rise after Primary Posterior Continuous Curvilinear Capsulorhexis with a Fixed Dorzolamide-Timolol Combination: Randomized Safety Study with Intraindividual Comparison Using an Angulated and a Nonangulated Intraocular Lens. J. Cataract. Refract. Surg. 2007, 33, 1754–1759. [Google Scholar] [CrossRef]
- Wu, J.; Liang, G.; Zheng, Q.; He, F.; Liu, J.; Xu, W. Fusion Phaco Complex Phacoemulsification through a Coaxial 2.2 Mm Micro-Incision: A Clinical Study. Int. J. Clin. Exp. Med. 2018, 11, 9921–9930. [Google Scholar]
- Yaylali, V.; Ozbay, D.; Tatlipinar, S.; Yildirim, C.; Ozden, S. Efficacy and Safety of Rimexolone 1% versus Prednisolone Acetate 1% in the Control of Postoperative Inflammation Following Phacoemulsification Cataract Surgery. Int. Ophthalmol. 2004, 25, 65–68. [Google Scholar]
- Zebardast, N.; Zheng, C.; Jampel, H.D. Effect of a Schlemm’s Canal Microstent on Early Postoperative Intraocular Pressure after Cataract Surgery: An Analysis of the HORIZON Randomized Controlled Trial. Ophthalmology 2020, 127, 1303–1310. [Google Scholar] [CrossRef] [PubMed]
- Ziakas, N.G.; Boboridis, K.; Nakos, E.; Mikropoulos, D.; Margaritis, V.; Konstas, A.G.P. Does the Use of Trypan Blue during Phacoemulsification Affect the Intraocular Pressure? Can. J. Ophthalmol. 2009, 44, 293–296. [Google Scholar] [CrossRef]
- Messenio, D.; Ferroni, M.; Boschetti, F. Goldmann Tonometry and Corneal Biomechanics. Appl. Sci. 2021, 11, 4025. [Google Scholar] [CrossRef]
- Phulke, S.; Kaushik, S.; Kaur, S.; Pandav, S.S. Steroid-induced Glaucoma: An Avoidable Irreversible Blindness. J. Curr. Glaucoma Pract. 2017, 11, 67–72. [Google Scholar]
- Erichsen, J.H.; Forman, J.L.; Holm, L.M.; Kessel, L. Effect of anti-inflammatory regimen on early postoperative inflammation after cataract surgery. J. Cataract. Refract. Surg. 2021, 47, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Kanjee, R.; Popovic, M.M.; Salimi, A.; Hutnik, C.M.L.; Ahmed, I.I.K.; Saheb, H. Prophylaxis against intraocular pressure spikes following uncomplicated phacoemulsification: A systematic-review and meta-analysis. Eye 2024, 38, 1518–1528. [Google Scholar] [CrossRef] [PubMed]
- Li, H.G.; Chen, Y.H.; Lin, F.; Li, S.Y.; Liu, Q.H.; Yin, C.G.; Chen, X.Y.; Zhang, X.J.; Qu, Y.; Hui, Y.N. Agreement of intraocular pressure measurement with Corvis ST, non-contact tonometer, and Goldmann applanation tonometer in children with ocular hypertension and related factors. Int. J. Ophthalmol. 2023, 16, 1601–1607. [Google Scholar] [CrossRef] [PubMed]
- De Bernardo, M.; Cione, F.; De Pascale, I.; Pagliarulo, S.; Rosa, N. Intraocular Pressure Measurements in Standing, Sitting, Prone, and Supine Positions. J. Pers. Med. 2024, 14, 826. [Google Scholar] [CrossRef]
- Birkeland, S.; Bismark, M.; Barry, M.J.; Möller, S. Is greater patient involvement associated with higher satisfaction? Experimental evidence from a vignette survey. BMJ Qual. Saf. 2022, 31, 86–93. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herspiegel, W.J.; Yu, B.E.; Algodi, H.S.; Malvankar-Mehta, M.S.; Hutnik, C.M.L. Optimal Timing for Intraocular Pressure Measurement Following Phacoemulsification Cataract Surgery: A Systematic Review and a Meta-Analysis. Vision 2024, 8, 65. https://doi.org/10.3390/vision8040065
Herspiegel WJ, Yu BE, Algodi HS, Malvankar-Mehta MS, Hutnik CML. Optimal Timing for Intraocular Pressure Measurement Following Phacoemulsification Cataract Surgery: A Systematic Review and a Meta-Analysis. Vision. 2024; 8(4):65. https://doi.org/10.3390/vision8040065
Chicago/Turabian StyleHerspiegel, William J., Brian E. Yu, Hamzah S. Algodi, Monali S. Malvankar-Mehta, and Cindy M. L. Hutnik. 2024. "Optimal Timing for Intraocular Pressure Measurement Following Phacoemulsification Cataract Surgery: A Systematic Review and a Meta-Analysis" Vision 8, no. 4: 65. https://doi.org/10.3390/vision8040065
APA StyleHerspiegel, W. J., Yu, B. E., Algodi, H. S., Malvankar-Mehta, M. S., & Hutnik, C. M. L. (2024). Optimal Timing for Intraocular Pressure Measurement Following Phacoemulsification Cataract Surgery: A Systematic Review and a Meta-Analysis. Vision, 8(4), 65. https://doi.org/10.3390/vision8040065







