Pseudomyopia: A Review
Abstract
:1. Introduction
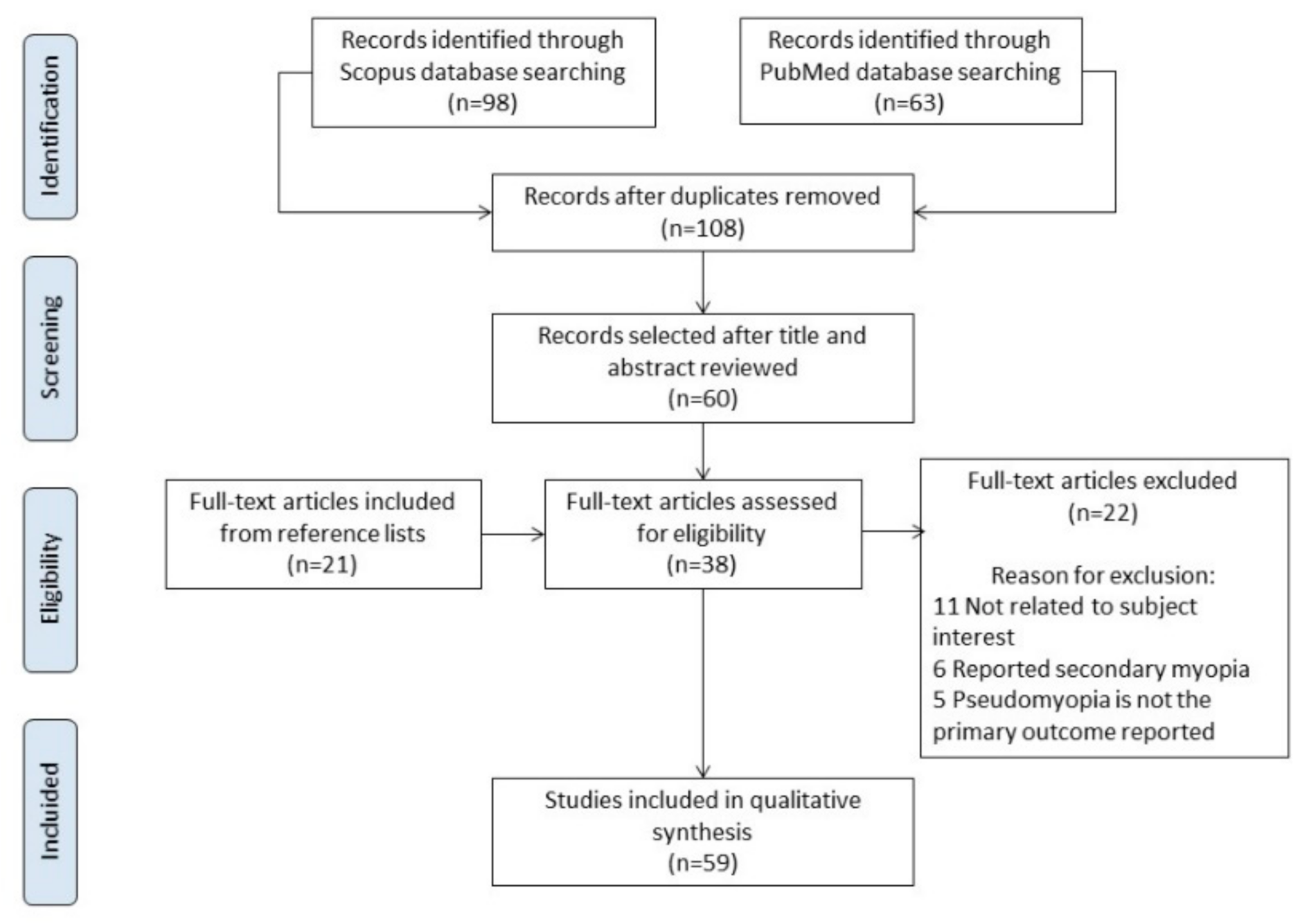
2. Methods: Literature Search
3. Results
3.1. Pathophysiology
3.2. Clinical Presentation
3.3. Assessment and Diagnosis
3.4. Treatment
| Author Year | Sex | Age | Symptoms/Signs | Diagnostic Test | Non-Cycloplegic Rx (D) | Cycloplegic Rx (D) | Gap Refraction (D) | Dx/Etiology | Treatment | After Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| Rutstein, Marsh-Tootle 2001 [12] | Female | 27 | Blurred distance vision in LE | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Accomodative response Funduscopy Slit-lamp exam | RE plano LE −5.00 | RE + 0.75 − 0.25 × 180 LE + 0.75 − 0.50 × 180 | RE 0.75 LE 5.75 | Pseudomyopia Unilateral LE accommodative spasm associated with excessive near work | Not treatment | Not reported |
| Ninomiya et al. 2003 [22] | Male | 12 | Blurred distance vision after a head/eye trauma soccer ball | VA Non-cycloplegic Rx Cycloplegic Rx Slit-lamp exam SA * | RE −2.00 LE −3.00 SA RE: −0.107 μm LE: −0.112 μm | RE plano LE plano | RE 2.00 LE 3.00 | Pseudomyopia Accommodative spasm associated with eye trauma | Cyclopentolate 0.1%, 2 drops/day | Resolved SA RE: 0.020 μm LE: 0.031 μm |
| Ninomiya et al. 2003 [22] | Female | 37 | Blurred distance vision | VA Non-cycloplegic Rx Cycloplegic Rx Slit-lamp exam SA * | RE −11.25 LE −5.00 SA RE: −0.075 μm LE: −0.048 μm | RE −3.50 LE −3.00 SA RE: 0.027 μm LE: 0.022 μm | RE 7.75 LE 2.00 | Pseudomyopia Accommodative spasm associated with excessive near work | Not reported | Not reported |
| Peinado et al. 2019 [14] | Female | 10 | Monocular decreased of vision | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Papillary and macular OCT Neurophysiological studies | RE −6.00 | RE +0.50 | RE 6.50 | Pseudomyopia Unilateral RE accommodative spasmIdiopathic | Atropine 1% daily (15 days) and +3D near-vision spectacles in RE | Resolved |
| Hughes et al. 2017 [25] | Female | 34 | Blurred distance vision in RE after a whiplash injury sustained | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Funduscopy Slit-lamp exam Neuro-ophtalmology exam MRI | RE −3.50 | Not reported | Pseudomyopia following a whiplash type injury | Far vision minus lens Atropine 1% | Not resolved | |
| Laria et al. 2014 [17] | Female | 8 | Headaches and blurred vision | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Funduscopy Slit-lamp exam Neuro-ophtalmology exam | RE −9.75 − 0.25 × 65°LE −7.75 − 0.75 × 65° | RE +0.75 LE +0.75 D | RE 10.50 LE 8.50 | Pseudomyopia Esotropia, spasm of the near reflex | Cyclopentolate 1.0%, 2 drops/day Atropine 1%, 1 drop/day and near-vision glasses. Botulinum toxin in the medial rectus Visual therapy | Resolved |
| Shetty et al. 2015 [38] | Female | 33 | Blurred distance vision and headache after one month PRK for myopia | VA Non-cycloplegic Rx Cycloplegic Rx Slit-lamp exam Aberrometry † | RE −0.75 − 0.50 × 165° LE −0.50 × 20° Internal defocus RE: 1.019 μm LE: 0.366 μm | RE −0.50 × 165 LE −0.50 × 20° Internal defocus RE:0.142 μm (86% decreassed) LE:0.230 μm(36% decreased) | RE −0.75 LE plano | Pseudomyopia Accommodative spasm | Cyclopentolate 1%, 3 drops/day | Resolved |
| Airiani S, Braunstein RE 2006 [39] | Female | 41 | Severe headache after undergoing LASIK surgery. | VA Non-cycloplegic Rx Cycloplegic Rx Slit-lamp exam Funduscopy | RE −2.25 − 0.50 × 170° LE plano | RE plano LE +0.75 | RE 2.25 LE 0.75 | Pseudomyopia | Cyclopentolate 1% | Patient lost to follow-up |
| Shanker et al. 2012 [26] | Male | 22 | Headaches and blurred vision | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic examMEM Funduscopy | RE −10.00 D LE −10.00 D | RE −2.25 LE −1.50 | RE 7.75 LE 8.50 | Pseudomyopia Accommodative spasm | Homatropine 2%, 2 drops/day for 10 days Accommodative training | AS resolved, but after exotropia intermittent |
| Jayakumar et al. 2012 [16] | Male | 29 | Squint and blurred vision | VA Cycloplegic Rx Orthoptic exam | Not reported | RE plano LE plano | Basic exotropia | Bilateral lateral rectus recession | Blurred vision after strabismus surgery | |
| Blurred vision after strabismus surgery | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam NRA | RE −2.00 − 0.50 × 90° LE −2.75 | RE plano LE plano | RE 2.25 LE 2.75 | Pseudomyopia | Cyclopentolate 1%, 3 drops/day Prisms | Not reported | |||
| Bohlmann BJ, France TD 1987 [40] | Female | 19 | Blurred distance vision after trauma | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Neuro-ophtalmology exam MRI | RE −1.50 LE −1.50 | RE 0.25 LE 0.25 | RE 1.75 LE 1.75 | Pseudomyopia after a closed head trauma | Atropine 1% and bifocals | Resolved after 9 years |
| London et al. 2003 [18] | Female | 15 | Blurred distance vision after closed head trauma | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam MEM Neurophysiological studies | RE −1.50 LE−1.50 − 0.50 × 175° | RE +0.50 LE + 0.25 − 0.25 × 180° | RE 2.00 LE 1.75 | Pseudomyopia Accommodative spasm associated with head trauma | Accommodative rock exercises | Resolved |
| London et al. 2003 [18] | Male | 25 | Blurred distance vision for a year. | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam MEM Neurophysiological studies | RE −2.75 LE −2.50 | RE −0.50 LE −0.25 | RE 2.25 LE 2.25 | Pseudomyopia Accommodative spasm associated with Parinaud’s syndrome Exotropia | Accommodative rock exercises Atropine and near-vision spectacles Far vision minus lenses Strabismus surgery | Partially resolved Eventually he required far vision minus lenses |
| London et al. 2003 [18] | Female | 36 | Blurred and variable distance vision after closed head trauma.Pupillary asymmetry | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Neuro-ophtalmology exam Funduscopy Slit-lamp exam | RE −1.50 − 1.00 × 175° LE −1.75 − 1.25 × 157° | RE −0.25 LE −0.25 | RE 1.25 LE 1.50 | Pseudomyopia Accommodative spasm associated with head trauma | Homatropine 5% Scopolamine 0.25% Bifocal glasses +2.00 D | Partially resolved She required pharmacologic drops and bifocal glasses |
| London et al. 2003 [18] | Male | 17 | Blurred distance vision without correction and blurred near vision with correction unilateral for a year after head trauma | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Accommodative response (MEM) and amplitudes | LE −2.25 | LE −0.25 | LE 2.00 | Pseudomyopia Unilateral LE accommodative spasm associated with head trauma | Bifocal glasses RE −0.50 Ad +0.75 LE −2.00 Ad +1.75 | Partially resolved He required bifocal glasses |
| Chan RV, Trobe JD 2002 [36] | Male | 30 | Blurred distance vision after trauma | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Neuro-ophtalmology exam MRI | RE −1.50 LE −1.50 | RE plano LE plano | RE 1.50 LE 1.50 | Pseudomyopia after a closed head trauma | Manifest Rx | Not resolved |
| Male | 20 | RE −5.00 LE −5.00 | RE −3.25 LE −3.25 | RE 1.75 LE 1.75 | Manifest Rx | Not resolved | ||||
| Male | 18 | RE −1.50 − 0.75 × 93° LE −2.50 − 0.50 × 96° | RE +0.75 − 1.50 × 90° LE +0.25 − 1.25 × 70° | RE 1.50 LE 2.75 | Cycloplegic Rx Manifest Rx | Not resolved | ||||
| Male | 17 | RE −2.50 − 0.50 × 10° LE −2.50 | RE −1.00 − 0.25 × 10° LE−0.75 − 0.25 × 150° | RE 1.50 LE 1.75 | Homatropine and bifocals | Not resolved | ||||
| Male | 16 | RE −2.00 LE −1.25 − 0.75 × 55° | RE −1.25 LE −0.50 − 0.75 × 55° | RE 0.75 LE 0.75 | Manifest Rx | Not resolved | ||||
| Mc Murray et al. 2004 [45] | Male | 28 | Decreased VA after closed head trauma sustained in a motor vehicle accident 16 weeks earlier | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Axial length Computerized tomography | NR | NR | RE 4.00 LE 5.25 | Pseudomyopia Accommodative spasm associated with head trauma | Unsatisfactory despite a variety of cycloplegic and refractive corrections Finally, sequential clear lens extraction was selected. | Resolved VA was N5 with +2.50 D reading glasses |
| Park et al. 2021 [55] | Female | 33 | Blurred distance vision after | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Accomodative response Funduscopy Slit-lamp exam Biometry | RE −2.34 (SE) LE −2.50 (SE) | RE −0.26 (SE) LE 0.13 (SE) | RE 2.08 LE 2.63 | Pseudomyopia with paradoxical accommodation | Glasses −1.00 D | She is in monitorization |
| Nguyen et al. 2020 [43] | Female | 10 | Painless vision loss in both eyes | VA Non-cycloplegic Rx Cycloplegic Rx Orthoptic exam Accomodative response Funduscopy Slit-lamp exam Biometry | RE −8.50 − 0.50 × 57° LE −9.25 − 0.50 × 153° | RE +0.75 − 0.50 × 7° LE + 0.75 − 0.50 × 47° | RE 9.25 LE 10.00 | Accommodative spasm associated with conversion disorder | Atropine 0.5%–0.1%–0.01% in both eyes once daily-10 weeks | Atropine drops discontinued |
| Author | Year | Cycloplegic Agents | Plus Lenses | Manifest Rx | Prism Base in | Orthoptics |
|---|---|---|---|---|---|---|
| Shaffer [20] | 1928 | x | x | |||
| Padman [56] | 1930 | x | ||||
| Hathaway [54] | 1930 | x | ||||
| Willians [11] | 1956 | x | ||||
| Bohlmann BJ, France TD [40] | 1987 | x | x | |||
| Ciufreda [23] | 1999 | |||||
| Chan RV, Trobe JD [36] | 2002 | x | x | x | ||
| Ninomiya et al. [22] | 2003 | x | ||||
| London et al. [18] | 2003 | x | x | x | x | |
| Airiani S, Braunstein RE [39] | 2006 | x | ||||
| Shanker et al. [26] | 2012 | x | x | |||
| Jayakumar et al. [16] | 2012 | x | x | |||
| Laria et al. [17] | 2014 | x | x | x | ||
| Shetty et al. [38] | 2015 | x | ||||
| Hughes et al. [25] | 2017 | x | x | |||
| Peinado et al. [14] | 2019 | x | x | |||
| Nguyen et al. [43] | 2020 | x | ||||
| Park et al. [55] | 2021 | x |
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Flitcroft, D.I.; He, M.; Jonas, J.B.; Jong, M.; Naidoo, K.; Ohno-Matsui, K.; Rahi, J.; Resnikoff, S.; Vitale, S.; Yannuzzi, L. IMI–Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Investig. Opthalmol. Vis. Sci. 2019, 60, M20–M30. [Google Scholar] [CrossRef] [Green Version]
- Pesudovs, K.; Elliott, D.B. Refractive error changes in cortical, nuclear, and posterior subcapsular cataracts. Br. J. Ophthalmol. 2003, 87, 964–967. [Google Scholar] [CrossRef]
- Cho, Y.K.; Huang, W.; Nishimura, E. Myopic refractive shift represents dense nuclear sclerosis and thin lens in lenticular myopia. Clin. Exp. Optom. 2013, 96, 479–485. [Google Scholar] [CrossRef] [PubMed]
- Padhy, D.; Rao, A. Bimatoprost (0.03%)-induced accommodative spasm and pseudomyopia. BMJ Case Rep. 2015, 2015, 211820. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaštelan, S.; Gverović-Antunica, A.; Pelcic, G.; Gotovac, M.; Marković, I.; Kasun, B. Refractive Changes Associated with Diabetes Mellitus. Semin. Ophthalmol. 2018, 33, 838–845. [Google Scholar] [CrossRef]
- Riedl, P.; Dragana, S.; Arnell, P.; Wannholt, R.; Zetterberg, M.; Gronlund, M.A. Myopic shift and lens turbidity following hyperbaric oxygen therapy-a prospective, longitudinal, observational cohort study. Acta Ophthalmol. 2019, 97, 596–602. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Ikeda, T.; Nagata, M.; Mimura, O. Pathogenesis of transient high myopia after blunt eye trauma. Ophthalmology 2002, 109, 501–507. [Google Scholar] [CrossRef]
- De Jong, P.T.V.M. Myopia: Its historical contexts. Br. J. Ophthalmol. 2018, 102, 1021–1027. [Google Scholar] [CrossRef] [PubMed]
- Stenson, M.S.; Raskind, R.H. Pseudomyopia: Etiology, mechanisms and therapy. J. Pediatr. Ophthalmol. 1970, 7, 110–115. [Google Scholar] [CrossRef]
- Walker, J.P. Myopia and pseudo-myopia. Br. J. Ophthalmol. 1946, 30, 735–742. [Google Scholar] [CrossRef] [Green Version]
- Williams, O.A. Base in prisms and pseudo myopia. Australas. J. Optom. 1956, 39, 260. [Google Scholar] [CrossRef]
- Rutstein, R.P.; Marsh-Tootle, W. Acquired Unilateral Visual Loss Attributed to an Accommodative Spasm. Optom. Vis. Sci. 2001, 78, 492–495. [Google Scholar] [CrossRef] [PubMed]
- Jones, R. Physiological Pseudomyopia. Optom. Vis. Sci. 1990, 67, 610–616. [Google Scholar] [CrossRef]
- Peinado, G.; Sanz, P.M.; Pérez, I.D.C.; Sánchez, P.G.D.L. Unilateral accommodation spasm: Case report and literature review. Arch. Soc. Española Oftalmol. 2019, 94, 285–287. [Google Scholar] [CrossRef]
- Seaber, J.H. Pseudomyopia in Exodeviations. Am. Orthopt. J. 1966, 16, 67–72. [Google Scholar] [CrossRef]
- Jayakumar, M.; Kaul, S.; Jayakumar, N. Pseudomyopia in intermittent exodeviation. Indian J. Ophthalmol. 2012, 60, 578–579. [Google Scholar] [CrossRef] [PubMed]
- Laria, C.; Merino-Suárez, M.L.; Piñero, D.P.; Gómez-Hurtado, A.; Pérez-Cambrodí, R.J. Botulinum Toxin as an Alternative to Treat the Spasm of the Near Reflex. Semin. Ophthalmol. 2014, 30, 393–396. [Google Scholar] [CrossRef]
- London, R.; Wick, B.; Kirschen, D. Post-traumatic pseudomyopia. Optometry 2003, 74, 111–120. [Google Scholar]
- Rutstein, R.P. Accommodative spasm in siblings: A unique finding. Indian J. Ophthalmol. 2010, 58, 326–327. [Google Scholar] [CrossRef]
- Shaffer, S. A Method for reducing Pseudo-myopia. Optom. Vis. Sci. 1928, 5, 396–397. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Ninomiya, S.; Fujikado, T.; Kuroda, T.; Maeda, N.; Tano, Y.; Hirohara, Y.; Mihashi, T. Wavefront analysis in eyes with accommodative spasm. Am. J. Ophthalmol. 2003, 136, 1161–1163. [Google Scholar] [CrossRef]
- Ciuffreda, K.J.; Rosenfield, M.; Gillard, M.A. Near-vision lens effects on nearwork-induced transient myopia. Clin. Eye Vis. Care 1999, 10, 205–207. [Google Scholar] [CrossRef]
- Ciuffreda, K.J.; Wallis, D.M. Myopes show increased susceptibility to nearwork aftereffects. Investig. Ophthalmol. Vis. Sci. 1998, 39, 1797–1803. [Google Scholar]
- Hughes, F.E.; Treacy, M.P.; Duignan, E.S.; Mullaney, P.B. Persistent pseudomyopia following a whiplash injury in a previously emmetropic woman. Am. J. Ophthalmol. Case Rep. 2017, 8, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Shanker, V.; Ganesh, S.; Sethi, S. Accommodative spasm with bilateral vision loss due to untreated intermittent exotropia in an adult. Nepal. J. Ophthalmol. 2012, 4, 319–322. [Google Scholar] [CrossRef]
- Goss, D.A.; Grosvenor, T.P.; Keller, J.P.; Marsh-Tootle, W.; Thomas, M.S.; Zadnik, K. Optometric clinical practice guideline care of the patient with myopia. In Clinical Guideline of the American Optometric Association; American Optometric Association: St. Louis, MO, USA, 2006. [Google Scholar]
- Wagner, S.; Schaeffel, F.; Zrenner, E.; Straber, T. Prolonged nearwork affects the ciliary muscle morphology. Exp. Eye Res. 2019, 186, 107741. [Google Scholar] [CrossRef]
- French, A.N.; Morgan, I.G.; Mitchell, P.; Rose, K.A. Risk factors for incident myopia in Australian schoolchildren: The Sydney adolescent vascular and eye study. Ophthalmology 2013, 120, 2100–2108. [Google Scholar] [CrossRef]
- Huang, H.-M.; Chang, D.S.-T.; Wu, P.-C. The Association between Near Work Activities and Myopia in Children—A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0140419. [Google Scholar] [CrossRef] [Green Version]
- Lin, Z.; Vasudevan, B.; Mao, G.Y.; Ciuffreda, K.J.; Jhanji, V.; Li, X.X.; Zhou, H.J.; Wang, N.L.; Liang, Y.B. The influence of near work on myopic refractive change in urban students in Beijing: A three-year follow-up report. Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 2247–2255. [Google Scholar] [CrossRef]
- Vera-Díaz, F.A.; Strang, N.C.; Winn, B. Nearwork induced transient myopia during myopia progression. Curr. Eye Res. 2002, 24, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Vasudevan, B.; Ciuffreda, K.J. Additivity of Near Work–Induced Transient Myopia and Its Decay Characteristics in Different Refractive Groups. Investig. Opthalmol. Vis. Sci. 2008, 49, 836–841. [Google Scholar] [CrossRef] [PubMed]
- Rhatigan, M.; Byrne, C.; Logan, P. Spasm of the near reflex: A case report. Am. J. Ophthalmol. Case Rep. 2017, 6, 35–37. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, J.H.; Schneekloth, B.B. Spasm of the near reflex: A spectrum of anomalies. Surv. Ophthalmol. 1996, 40, 269–278. [Google Scholar] [CrossRef]
- Chan, R.V.P.; Trobe, J. Spasm of Accommodation Associated with Closed Head Trauma. J. Neuro-Ophthalmol. 2002, 22, 15–17. [Google Scholar] [CrossRef] [PubMed]
- Artal, P.; Schwarz, C.; Cánovas, C.; Mira-Agudelo, A. Night Myopia Studied with an Adaptive Optics Visual Analyzer. PLoS ONE 2012, 7, e40239. [Google Scholar] [CrossRef]
- Shetty, R.; Deshpande, K.; Kemmanu, V.; Kaweri, L. The Role of Aberrometry in Accommodative Spasm After Myopic Photorefractive Keratectomy. J. Refract. Surg. 2015, 31, 851–853. [Google Scholar] [CrossRef]
- Airiani, S.; Braunstein, R.E. Accommodative Spasm after Laser-Assisted In Situ Keratomileusis (LASIK). Am. J. Ophthalmol. 2006, 141, 1163–1164. [Google Scholar] [CrossRef]
- Bohlmann, B.J.; France, T.D. Persistent accommodative spasm nine years after head trauma. J. Clin. Neuro-ophthalmol. 1987, 7, 129–134. [Google Scholar]
- Kara, H.; Yasar, E.; Gurlevik, U. Is pseudomyopia associated with anxiety and related disorders? Pak. J. Med. Sci. 2021, 37, 1514–1518. [Google Scholar] [CrossRef]
- Khalid, K.; Padda, J.; Pokhriyal, S.; Hitawala, G.; Khan, M.S.; Upadhyay, P.; Cooper, A.C.; Jean-Charles, G. Pseudomyopia and Its Association with Anxiety. Cureus 2021, 13, 17411. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, H.T.T.; Hoang, T.T.; Tran, A.P.; Tran, H.D.M. Combined Interventions for Nonorganic Visual Loss in a Case with Pseudo-Myopia: A Perspective from Vietnam. Case Rep. Ophthalmol. 2020, 11, 229–233. [Google Scholar] [CrossRef] [PubMed]
- Kowal, L. Ophthalmic manifestations of head injury. Aust. N. Z. J. Ophthalmol. 1992, 20, 35–40. [Google Scholar] [CrossRef] [PubMed]
- McMurray, C.J.; Burley, C.D.; Elder, M.J. Clear lens extraction for the treatment of persistent accommodative spasm after head trauma. J. Cataract Refract. Surg. 2004, 30, 2629–2631. [Google Scholar] [CrossRef]
- Cooper, J.S.B.C.; Cotter, S.A.; Daum, K.M.; Griffin, J.R.; Scheiman, M.M. Care of the Patient with Accommodative and Vergence Dysfunction; American Optometric Association: St. Louis, MI, USA, 2006. [Google Scholar]
- Demir, M.S.; Muhafiz, E. Performance of a photoscreener in detecting accommodation spasm. Clin. Exp. Optom. 2021, 1–5. [Google Scholar] [CrossRef]
- Gifford, K.L.; Richdale, K.; Kang, P.; Aller, T.A.; Lam, C.S.; Liu, Y.M.; Michaud, L.; Mulder, J.; Orr, J.B.; Rose, K.A.; et al. IMI–Clinical Management Guidelines Report. Investig. Ophthalmol. Vis. Sci. 2019, 60, M184–M203. [Google Scholar] [CrossRef] [Green Version]
- Morgan, I.G.; Iribarren, R.; Fotouhi, A.; Grzybowski, A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015, 93, 581–585. [Google Scholar] [CrossRef]
- Mimouni, M.; Zoller, L.; Horowitz, J.; Wygnaski-Jaffe, T.; Morad, Y.; Mezer, E. Cycloplegic autorefraction in young adults: Is it mandatory? Graefes Arch. Clin. Exp. Ophthalmol. 2016, 254, 395–398. [Google Scholar] [CrossRef]
- Sankaridurg, P.; He, X.; Naduvilath, T.; Lv, M.; Ho, A.; Smith, E.; Erickson, P.; Zhu, J.; Zou, H.; Xu, X. Comparison of noncycloplegic and cycloplegic autorefraction in categorizing refractive error data in children. Acta Ophthalmol. 2017, 95, e633–e640. [Google Scholar] [CrossRef] [Green Version]
- Kang, M.-T.; Jan, C.; Li, S.; Yusufu, M.; Liang, X.; Cao, K.; Liu, L.-R.; Li, H.; Wang, N.; Congdon, N. Prevalence and risk factors of pseudomyopia in a Chinese children population: The Anyang Childhood Eye Study. Br. J. Ophthalmol. 2020, 105, 1216–1221. [Google Scholar] [CrossRef]
- Kanda, H.; Kobayashi, M.; Mihashi, T.; Morimoto, T.; Nishida, K.; Fujikado, T. Serial measurements of accommodation by open-field Hartmann–Shack wavefront aberrometer in eyes with accommodative spasm. Jpn. J. Ophthalmol. 2012, 56, 617–623. [Google Scholar] [CrossRef] [PubMed]
- Hathaway, C.J. A case of Esophoria and Pseudo-Myopia corrected with base-in Kratometer treatments, base-in corrections and bifocals. Optom. Vis. Sci. 1930, 7, 541–546. [Google Scholar] [CrossRef]
- Park, I.K.; Park, Y.K.; Shin, J.-H.; Chun, Y.S. Pseudomyopia with paradoxical accommodation: A case report. BMC Ophthalmol. 2021, 21, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Padman, R.S. The modern treatment of true and pseudo myopia. Australas. J. Optom. 1930, 13, 3–6. [Google Scholar] [CrossRef]
- Takada, M.; Sugiura, A.; Matsuura, Y.; Miyao, M.; Takada, H. A Study of Accommodation Training by Stereoscopic Film Presentation. In Design Methods, Tools, and Interaction Techniques for eInclusion. UAHCI 2013; Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2013; Volume 8009. [Google Scholar] [CrossRef]
- Takada, M.; Miyao, M.; Satoh, M.; Yoshikawa, K.; Matsuura, Y. Effect of Accommodation Training on Visual Function of Visual Inspection Workers and Middle-Aged People. J. Sports Med. Doping Stud. 2012, 2, 112. [Google Scholar] [CrossRef] [Green Version]
- Li, L.-P.; Jin, C.-Z. Tuina combined with needling distal points for pseudo-myopia in adolescents. J. Acupunct. Tuina Sci. 2015, 13, 160–164. [Google Scholar] [CrossRef]
| Inclusion Criteria |
|---|
| Pseudomyopia caused by an increase in ocular refractive power due to overstimulation of the eye’s accommodative mechanism. |
| Explicit mention of pseudomyopia as the primary outcome reported. |
| Exclusion Criteria |
| Not related to subject interest. |
| Reported secondary myopia. |
| Reported pseudomyopia, but it is not the primary outcome. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Montero, M.; Felipe-Márquez, G.; Arriola-Villalobos, P.; Garzón, N. Pseudomyopia: A Review. Vision 2022, 6, 17. https://doi.org/10.3390/vision6010017
García-Montero M, Felipe-Márquez G, Arriola-Villalobos P, Garzón N. Pseudomyopia: A Review. Vision. 2022; 6(1):17. https://doi.org/10.3390/vision6010017
Chicago/Turabian StyleGarcía-Montero, María, Gema Felipe-Márquez, Pedro Arriola-Villalobos, and Nuria Garzón. 2022. "Pseudomyopia: A Review" Vision 6, no. 1: 17. https://doi.org/10.3390/vision6010017
APA StyleGarcía-Montero, M., Felipe-Márquez, G., Arriola-Villalobos, P., & Garzón, N. (2022). Pseudomyopia: A Review. Vision, 6(1), 17. https://doi.org/10.3390/vision6010017




